Abstract
Sensorineural hearing loss is one of the most common inherited sensory disorders. Functional classifications of deafness genes have shed light on genotype- and mechanism-based pharmacological approaches and on gene therapy strategies. In this study, we characterized the clinical phenotypes and genotypes of non-syndromic deafness caused by transcription factor (TF) gene variants, one of the functional classifications of genetic hearing loss. Of 1280 probands whose genomic DNA was subjected to molecular genetic testing, TF genes were responsible for hearing loss in 2.6%. Thirty-three pathogenic variants, including nine novel variants, accounting for non-syndromic deafness were clustered in only four TF genes (POU3F4, POU4F3, LMX1A, and EYA4), which is indicative of a narrow molecular etiologic spectrum of TF genes, and the functional redundancy of many other TF genes, in the context of non-syndromic deafness. The audiological and radiological characteristics associated with the four TF genes differed significantly, with a wide phenotypic spectrum. The results of this study reveal the genetic load of TF gene alterations among a cohort with non-syndromic hearing loss. Additionally, we have further refined the clinical profiles associated with TF gene variants as a basis for a personalized, genetically tailored approach to audiological rehabilitation.
1. Introduction
Congenital hearing loss affects 1–2 out of every 1000 newborns and is one of the most common inherited sensory disorders in humans [1]. Genetic causes account for approximately 50% of sensorineural hearing loss (SNHL) cases, with recent advances in genomics contributing to the identification of more than 150 genes implicated in its etiology (https://hereditaryhearingloss.org/, accessed on 1 February 2022) [2]. Genetically engineered in vivo and in vitro models were used to establish functional classifications of deafness-related genes, including (1) hair bundle development and functioning; (2) synaptic transmission; (3) cellular adhesion and maintenance; (4) cochlear ion homeostasis; (5) extracellular matrix; (6) oxidative stress, metabolism, and mitochondrial defects; and (7) transcriptional regulation [3]. The application of these functional assignments provides a better understanding of genetic hearing loss, including mechanism- and genotype-based pharmacological and gene therapy approaches.
The “central dogma” refers to the transfer of sequence information between RNA, DNA, and proteins within a biological system. It describes how the information embedded in DNA is transferred to mRNA (transcription) and how amino-acid chains are synthesized from mRNA (translation) [4]. Transcription factors (TFs) recognize specific DNA sequences to control transcription by forming a complex that guides genome expression [5]. TFs generally contain several domains (effector, DNA-binding, and regulatory domains) that regulate their localization, chromatin accessibility, and transcriptional activity. More than 1600 human TFs have been documented in the literature [5], and their variants have been implicated in diverse diseases and syndromes, including cardiovascular diseases, cancer, neurological disorders, autoimmune diseases, and diabetes [6]. However, only a handful of TF variants are known to cause hearing impairment, and their clinical phenotypes and genotypes in the context of hearing loss remain poorly understood. The delineation of audiological phenotypes related to TF genes may be clinically valuable, shedding light on the mechanism of SNHL and the potential for timely intervention.
In this study, we characterized the audiological phenotypes and genotypes of disease-causing TF variants, as one of the functional classifications of genetic hearing loss (transcriptional regulation), with the aim of revealing genotype-phenotype correlations. Our results expand the genetic spectrum of TF variants associated with non-syndromic deafness and further refine the associated clinical profiles.
2. Materials and Methods
2.1. Subjects
All procedures in this study were approved by the Institutional Review Boards of Seoul National University Hospital (IRB-H-0905-041-281) and Seoul National University Bundang Hospital (IRB-B-1007-105-402). Written informed consent was obtained from all participants or the legal guardians of the pediatric participants. The study consisted of a retrospective review using the in-house databases of genetic hearing loss from the two participating hospitals. The DNA of 1280 probands was subjected to molecular genetic testing regardless of any specific audiologic phenotypes or modes of inheritance. Families with genetically confirmed disease-causing TF variants were included (n = 55, 4.3%). Families harboring genetic variants implicated in syndromic deafness (n = 22, 1.7%), primarily Waardenburg syndrome and branchio-oto-renal syndrome, were excluded. Ultimately, 33 families (2.6%) with TF-associated non-syndromic deafness were included.
2.2. Clinical Phenotyping
Comprehensive phenotypic evaluations, including audiological imaging, were performed in all patients and the postoperative outcome of cochlear implantation (CI) was documented. Audiological evaluations consisted of pure tone audiometry (PTA) in adults, and the auditory brainstem response threshold (ABRT) in prelingual infants. Hearing levels (HLs) were determined by averaging the hearing thresholds at 0.5, 1, 2, and 4 kHz of the PTA and were categorized as mild (25–40 dB HL), moderate (41–55 dB HL), moderately severe (56–70 dB HL), severe (71–90 dB HL), or profound (>91 dB HL) [7,8]. The audiograms were classified into four categories according to their configuration: flat, down-sloping, rising, or U-shaped [9,10]. Audiograms were defined as flat if the thresholds across frequencies did not differ from each other by >20 dB. Down-sloping audiograms were those with thresholds that occurred at equal or successively higher levels from 0.25 kHz to 8 kHz, with the difference between thresholds at 0.25 kHz and 8 kHz being >20 dB. Rising audiograms were defined as having thresholds that occurred at equal or successively lower levels from 0.25 kHz to 8 kHz, with the difference between thresholds at 0.25 kHz and 8 kHz being >20 dB. Audiograms were defined as U-shaped if one or more adjacent thresholds between 0.5 kHz and 4 kHz was >20 dB compared to the poorer threshold of 0.25 kHz or 8 kHz. Asymmetric hearing loss was defined as an interaural difference >10 dB in the threshold average of 0.5, 1, 2, and 4 kHz, with the HL of the better-hearing ear being worse than 25 dB HL [9,11]. Radiological evaluation of the middle ear, inner ear, and internal acoustic canal (IAC) included temporal bone computed tomography (CT) and internal acoustic canal magnetic resonance imaging (IAC MRI). Anatomical abnormalities of the middle ear, inner ear, and IAC were evaluated and classified using Sennaroglu’s revised classifications of cochleovestibular malformations [12]. The audiologic performance outcome of each cochlear implantee was evaluated by comparing the Categories of Auditory Perception (CAP), the Korean version of the Central Institute for the Deaf Everyday Speech Sentence Test (K-CID), Phonetically Balanced Word (PB), and spondee scores based on the speech evaluations conducted before and after CI. The postoperative speech evaluations were performed 3, 6, 12, 18, and 24 months after CI [13].
2.3. Molecular Genetic Testing
Genomic DNA was extracted from peripheral blood using a standard procedure. Initial screening was usually conducted with real-time PCR mutational hotspot screening kits, which targeted 22 variants of 10 hearing loss genes (GJB2, SLC26A4, CDH23, TMPRSS3, MT-RNR1, OTOF, MPZL2, TMC1, COCH, and ATP1A3), based on the prevalence of the genetic diagnostic yield in Korea and genotype–phenotype correlation (e.g., auditory neuropathy) [14,15]. Specifically, for a particular phenotype, direct sequencing was performed preferentially, followed by targeted panel sequencing (Otogenetics, Norcross, GA, USA) or whole-exome sequencing. The resulting reads were compared with the UCSC hg19 reference genome, and non-synonymous single-nucleotide polymorphisms (SNPs) were filtered at a depth of 40; dbSNP138 was filtered out, except for the flagged SNP. Disease-causing variants were detected in this study using a comprehensive filtering process and bioinformatics analyses, as described previously [16,17,18]. The pathogenic potential of the novel variants identified herein was evaluated according to the ACMG/AMP guidelines developed for hearing loss [19].
2.4. Statistical Analysis
Descriptive statistical analyses of the postoperative speech evaluation scores were performed using SPSS for Windows, version 18.0 (IBM Corp., Armonk, NY, USA). The schematic illustrations were created using GraphPad Prism version 9.0.3 for Windows (GraphPad Software LLC, San Diego, CA, USA; www.graphpad.com, accessed on 1 February 2022). The Mann–Whitney U test was used to compare postoperative CI outcomes between groups. Statistical significance was defined as a p-value < 0.05.
3. Results
3.1. Distribution of TF Genes
Among 720 probands in whom causative deafness variants were identified, 33 were from families with TF-associated non-syndromic deafness. The causative TF genes of these families were POU3F4 (n = 16, 48.5%), POU4F3 (n = 6, 18.2%), LMX1A (n = 6, 18.2%), and EYA4 (n = 5, 15.2%) (Table 1). The clustering of the deafness-causing TF variants in only four genes highlighted their role in non-syndromic deafness in Korea. Among the 33 variants detected in total, nine were novel: POU3F4 (c.458delC:p.Pro153Leufs*88, c.989G>A:p.Arg330Lys, c.958G>T:p.Glu320*, and c.626A>G:p.Gln229Arg), LMX1A (c.331del:p.Gln111Argfs*7), and EYA4 (c.697C>T:p.Gln233*, c.208+1del, c.578dup:p.Tyr193*, and c.1468G>T:p.Glu490*) (Table 2). All nine novel TF gene variants satisfied the criteria of the ACMG/AMP guidelines defining pathogenic or likely pathogenic genes (Table 2).

Table 1.
Phenotypes and genotypes associated with non-syndromic deafness caused by transcription factor variants.

Table 2.
Novel variants of transcription factor genes associated with non-syndromic deafness.
3.2. POU3F4
3.2.1. POU3F4: Genotype Profile
POU3F4 variants, segregating as an X-linked or de novo trait, were detected in 18 patients from 16 families. Most variants resided within the coding region of POU3F4, but four were copy number variants consisting of a large genomic deletion in the DFNX2 locus (Figure 1a). Large genomic deletions located upstream of POU3F4 were previously reported and presumably affect gene expression by disturbing the promotor or enhancer. Moreover, four of the 16 families harbored novel hemizygous POU3F4 variants (c.458delC:p.Pro153Leufs*88, c.989G>A:p.Arg330Lys, c.958G>T:p.Glu320*, and c.626A>G:p.Gln229Arg).
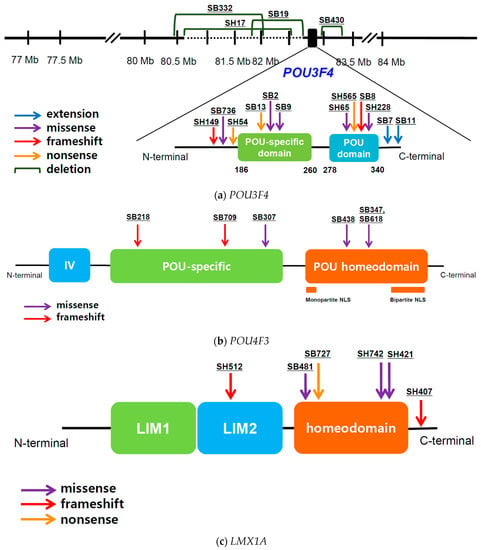
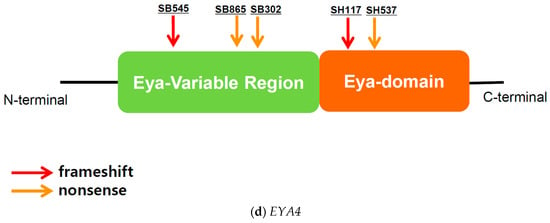
Figure 1.
Physical map of variants caused by four transcription factor genes associated with non-syndromic deafness: (a) POU3F4; (b) POU4F3; (c) LMX1A; (d) EYA4.
3.2.2. POU3F4: Audiological Profile and Cochlear Implantation Results
Of the 18 patients, 10 (55.6%) had MHL and 8 (44.4%) severe-to-profound SNHL. Hearing loss progression was documented in 40% of MHL patients, whereas hearing loss in all SNHL patients was non-progressive, due to a severe-to-profound loss already at baseline. As expected, temporal bone CT revealed incomplete partition (IP) type III in all patients. Eleven (61.1%) of these patients had undergone unilateral or bilateral CI, with a mean age at implantation of 6.9 (SD: 26.6) years. In the 11 patients (13 ears), the average CAP score was 1.3 (SD: 1.9) at baseline, 2.6 (SD: 1.6) at 3 months postoperatively, 3.0 (SD: 1.6) at 6 months postoperatively, 3.4 (SD: 1.2) at 12 months postoperatively, 3.7 (SD: 1.5) at 18 months postoperatively, and 3.8 (SD: 1.3) at 24 months postoperatively. Among the 13 ears, only one (SH65) had a score > 6 after 2 years: in the other ears it remained at or below 5 (i.e., understanding common phrases but not sentences without lip-reading). The postoperative CI outcomes were also compared with an age-, sex-, and laterality-matched cohort of GJB2-associated cochlear implantees (control group) (Table 3). Although the CAP scores at baseline, 3 months, and 6 months post-CI were not significantly different, the postoperative CAP scores of POU3F4 patients were significantly and progressively poorer than those of the controls at 12, 18, and 24 months after implantation (p < 0.05). The determination of postoperative CI outcomes depending on the genotype (missense or C-terminal extension variants versus truncated or copy number variants) did not reveal a definite genotype–phenotype correlation (Figure 2a).

Table 3.
Postoperative auditory perception score (CAP score) of cochlear implantees with POU3F4 variants.
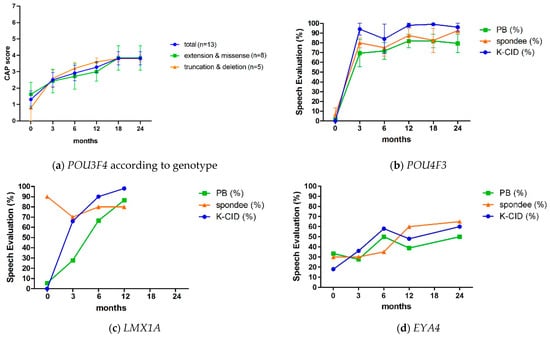
Figure 2.
Postoperative cochlear implant outcomes in patients with mutations in transcription factor genes: (a) POU3F4 according to genotype; (b) POU4F3; (c) LMX1A; (d) EYA4.
3.3. POU4F3
3.3.1. POU4F3: Genotype Profile
Ten patients from six POU4F3-associated families were identified, and in all of them an autosomal dominant inheritance pattern was determined. All familial variants were missense or frameshift variants within the two functional domains, including the POU-specific and POU homeodomain (Figure 1b). Notably, the variant in SB218 was a truncated variant residing in the POU-specific domain, thus affecting the two nuclear localization signal (NLS) domains within the POU homeodomain.
3.3.2. POU4F3: Audiological Profile and Cochlear Implantation Results
Nine of the ten patients (90%) in the POU4F3 group had SNHL, except one patient who had mixed hearing loss. The audiograms had a U-shaped configuration, characterized by a mid-frequency notch at 1–2 kHz in five patients (50.0%). Down-sloping (n = 3, 30.0%), mixed hearing loss (n = 1, 10.0%), and flat (n = 1, 10.0%) configurations characterized the audiograms of the remaining patients. The severity of hearing loss tended to be moderate to moderately severe initially but progressed thereafter. In three patients, their hearing loss eventually deteriorated to severe-to-profound, and they underwent CI at a mean age of 41.3 years (SD: 13.1). One patient was implanted bilaterally in a single procedure, and the other two patients were implanted unilaterally. The CI outcomes were favorable, with K-CID, PB, and spondee scores above 96%, 70%, and 70% at the 1 year postoperative exam, respectively (Figure 2b). One patient (SB216) displayed bilateral moderate SNHL in her early 30s and opted for bilateral middle ear implantation (MEI) surgery rather than a hearing aid due to unsatisfactory experience with conventional hearing aids. She has been a satisfied user of MEI for 6 years.
3.4. LMX1A
3.4.1. LMX1A: Genotype Profile
Nine patients from six LMX1A-associated families were identified. In most cases, the pedigrees indicated an autosomal dominant inheritance pattern. In one family, a de novo heterozygous missense variant (c.595A>G:p.Arg199Gly) was previously reported [18]. Four of the six variants were in the homeodomain, and the remaining two were truncated variants in LIM2 and the C-terminus, respectively (Figure 1c). Of these, a novel heterozygous LMX1A variant (c.331del:p.Gln111Argfs*7) was identified.
3.4.2. LMX1A: Audiological Profile and Cochlear Implantation Results
Asymmetric hearing loss (interaural difference > 15dB) was identified in five of the nine patients. The average asymmetry between the two ears was 35.75 dB (range 15–65). Three of the four LMX1A patients who were eligible for follow-up audiometry reported progressive hearing loss. In one patient (SB727), hearing deteriorated to profound hearing loss in her left ear and the asymmetric hearing loss remained. The patient eventually underwent unilateral CI, with significant improvement in her speech perception scores 3 and 6 months postoperatively (Figure 2c). One patient (SH407) reported hearing fluctuations in the left ear, with intermittent episodes of vertigo and headache, likely indicating Meniere’s disease.
3.5. EYA4
3.5.1. EYA4: Genotype Profile
In the eight patients from five EYA4-associated families, an autosomal dominant pattern was determined. Of the five identified variants, two nonsense and one deletion variant were localized within the variable region (eya-VR), and two loss-of-function variants, one frameshift variant, and one nonsense variant in the homologous domain (eya-HR) (Figure 1d). Of these, four novel heterozygous EYA4 variants (c.697C>T:p.Gln233*, c.208+1del, c.578dup:p.Tyr193*, and c.1468G>T:p.Glu490*) were identified.
3.5.2. EYA4: Audiological Profile and Cochlear Implantation Results
Among the eight patients, six (75.0%) had SNHL and two (25.0%) MHL, with postlingual onset (average age of onset: 32.5 ± 14.9 years). The severity of hearing loss ranged from moderate to severe. A down-sloping audiogram was the most prevalent configuration (five patients, 62.5%). The audiometric configuration deteriorated gradually in seven out of eight patients (87.5%). None of the patients reported symptoms of vestibulopathy or cardiac phenotypes (e.g., dilated cardiomyopathy or Mobitz type II AV block) indicating DFNA10. One patient underwent unilateral CI at the age of 80, due to gradual hearing deterioration. Following CI, her sentence recognition score (K-CID) improved significantly, from 18% at baseline to 60% at 2 years postoperatively (Figure 2d).
4. Discussion
This study is the first to provide detailed genotype and audiological phenotypes associated with TF variants inducing non-syndromic deafness. In the clinical exome sequencing era, many questions regarding the pathogenic mechanisms of SNHL have been answered, allowing a functional classification of the etiology of genetic hearing loss. Based on our in-house databases of genetic hearing loss, TF genes were implicated in ~3% of the study patients. Notably, 33 potentially pathogenic variants were observed, including nine novel variants, accounting for non-syndromic deafness clustered in only four TF genes (POU3F4, POU4F3, LMX1A, and EYA4), indicating a narrow molecular etiologica; spectrum within the enormous number of TF genes reported thus far in humans (up to 1600 genes). The limited genetic spectrum of TF genes accounting for non-syndromic deafness suggests the functional redundancy of many other TF genes in inner ear development or the maintenance of function. Alternatively, fetuses with variants in developmentally lethal, deafness-related TF genes may be spontaneously aborted.
POU3F4 encodes a POU-domain TF expressed in mesenchymal cells of the otic capsule, responsible for normal inner ear development [21,22]. POU3F4 mutant mice have reduced endocochlear potential and alterations in cochlear spiral ligament fibrocytes [23], leading to hearing impairment. POU3F4 is associated with IP type III, segregating as an X-linked recessive trait. In our cohort, POU3F4 was the TF gene most commonly associated with non-syndromic deafness. Although in most patients, single-nucleotide variants at the POU3F4 locus were identified, structural variants such as a large deletion upstream of the POU3F4 locus [24,25,26], have been reported. The current study also expands the genotypic spectrum of disease-causing variants of POU3F4 causing DFNX2, including the detection of four novel variants.
Despite numerous reports on CI in patients with POU3F4 variants, detailed information is lacking and the postoperative outcomes have been highly variable. Choi et al. [25] and Smeds et al. [22] reported that patients with POU3F4 variants had improved speech scores after implantation but the scores were still lower than those of age-matched cohorts without apparent cochlear anomalies. These results differ from those reported by Tian et al. [27] and Kang et al. [28]. To our knowledge, the present study was based on the largest cohort of patients and families with genetically confirmed IP type III, with 11 patients (13 ears) undergoing CI. The postoperative speech performance of POU3F4 patients was notably poorer than that of the GJB2-control group, precluding a potential correlation between postoperative CI outcomes and genotype. None of the 13 implanted ears of our POU3F4 cohort exhibited either a change or deterioration in speech or aided hearing upon follow-up beyond 3 years. Either intraoperative CSF gushers during electrode insertion or an unexpected localization of the spiral ganglion neurons might hinder the CI outcome, even in a patient with a genotype allowing residual transcriptional performance. Chao et al. [29] also reported an inconsistent distribution and responsiveness of the residual spiral ganglion neuron in IP type III, with CI outcomes varying accordingly. Furthermore, a recent study showed that POU3F4 variants were associated with neurodevelopmental disorders, such as hyperactivity, concentration difficulties, poor phonological working memory, and slow language development [22], all of which may contribute to a negative CI outcome.
POU4F3, a member of the POU family of TFs, is encoded by a gene located on chromosome 5q32 [30] and comprises two highly conserved POU domains: a POU-specific domain and a POU homeodomain [31]. POU4F3 is expressed in cochlear hair cells and plays a pivotal role in their differentiation, maturation, and maintenance by regulating downstream transcripts [32]. In humans, POU4F3 defects commonly cause autosomal dominant deafness, with variants associated with progressive non-syndromic deafness of postlingual onset [33,34,35,36,37,38,39]. The results of this study suggest that POU4F3 is the most common TF gene to cause non-syndromic deafness, excluding POU3F4 associated with X-linked inherited deafness in IP type III. In terms of related audiological characteristics, Kitano et al. [38] reported that POU4F3-associated DFNA15 is primarily characterized by mid-frequency hearing loss, followed by high-frequency hearing loss. This is consistent with our findings, as 45.5% of our cohort had U-shaped audiograms (mid-frequency hearing loss), followed by 36.4% with down-sloping audiograms (high-frequency hearing loss). Unfortunately, few studies have examined CI outcomes in patients with the POU4F3 variant. Kitano et al. [38] reported on two individuals with POU4F3 deafness who underwent CI, with good postoperative auditory performance. Miyake et al. [40] also reported a favorable CI outcome in a patient with a POU4F3 mutation. Three of our CI recipients with POU4F3 variants had a favorable outcome even at 1 year postoperatively. Our study thus doubles the number of reported CIs in patients with POU4F3 variants. In line with the spiral ganglion neuron hypothesis [41], these results suggest that POU4F3 patients are promising candidates for CI, as favorable postoperative outcomes can be expected.
LMX1A, a LIM homeobox TF, has been recently implicated in non-syndromic deafness. LMX1A plays a vital role in ear patterning, regulating the morphogenesis of inner ear structures [18]. To date, only nine LMX1A variants have been reported in the literature. Wesdorp et al. [42] first reported two Dutch families with LMX1A dominant variants (c.290G>C;p.Cys97Ser and c.721G>C;p.Val241Leu) and variable onset, severity, progression, and asymmetry. Schrauwen et al. [43] described a Pakistani family with an LMX1A recessive C-terminus missense variant (c.1106T>C;p.Ile369Thr) associated with profound SNHL. In recent studies, we reported five LMX1A heterozygous variants (c.595A>G:p.Arg199Gly, c.622C>T;p.Arg208*, c.719A>G;p.Gln240Arg, c.721G>A;p.Val241Met, and c.887dup;p.Gln297Thrfs*41) in five Korean families and one LMX1A heterozygous variant (c.686C>A; p.Ala229Asp) in a Polish family [18,44]. Together, these results suggest that alterations in LMX1A are associated with dominantly inherited asymmetric deafness. In these variants, audiological severity correlated with the extent of transcriptional activation, measured in a luciferase-reporter assay, implying a genotype–phenotype correlation [18]. Our study expands the genotypic spectrum of LMX1A in DFNA7 by identifying a novel variant (c.331del:p.Gln111Argfs*7), in addition to demonstrating audiologic asymmetry (SH421). Indeed, most LMX1A-related DFNA7 patients display audiologic asymmetry to varying degrees and a gradual progression of hearing loss. Our results provide evidence for favorable CI outcomes in patients with LMX1A-related DFNA7.
EYA4 encodes both an EYA domain (eya-HR) and a transactivation domain (eya-VR) and is responsible for the function of the mature organ of Corti [45]. EYA4 mutations generally cause autosomal dominant non-syndromic deafness (DFNA10). However, in some cases, EYA4 variants result in cardiac phenotypes, including dilated cardiomyopathy and a Mobitz type II AV block with deafness [46,47]. Makishima et al. [46] and Schonberger et al. [48] proposed that the variant location of EYA4 determines the occurrence of cardiac abnormalities, and thus a genotype–phenotype correlation. Truncating variants residing in the eya-HR domain seem to be associated with non-syndromic deafness, whereas those residing in the eya-VR region lead to dilated cardiomyopathy with deafness. However, recent studies have reported additional cases implicating truncations in the eya-VR region with non-syndromic deafness [49,50]. Three of our five EYA4 variants were predicted to encode truncated proteins affecting the eya-VR domain, but cardiac evaluations in these patients showed no signs of dilated cardiomyopathy. Our study also expands the genotypic spectrum of EYA4 in DFNA10, by adding four novel variants (c.697C>T:p.Gln233Ter, c.208+1del, c.578dup:p.Tyr193Ter, and c.1468G>T:p.Glu490Ter), all of which were associated with moderate to severe non-syndromic deafness characterized by gradual hearing loss. To our knowledge, this is the first study to describe a successful CI outcome in a patient with an EYA4 variant, but this result must be confirmed in a larger cohort.
Although in this study we examined the clinical characteristics of disease-causing TF variants associated with non-syndromic deafness, the study’s limitations should be addressed in future studies. A larger cohort with longitudinal audiologic follow-up is needed to strengthen our findings. Furthermore, functional studies of different genotypes associated with TF genes, such as transcriptional activity, nuclear localization, and mutant protein stability, will reveal the clinical and molecular relationships of TF genes. Nevertheless, our results provide further insights into the genetic landscape of TF-related non-syndromic deafness and thus a basis for the implementation of a personalized, genetically tailored approach for audiological treatment and rehabilitation in these patients.
Author Contributions
Conceptualization, S.-Y.L. and B.Y.C.; methodology, S.-Y.L. and B.Y.C.; formal analysis, H.D.J.; investigation, S.-Y.L., B.Y.C., J.H.H., S.M.L. and D.H.C.; resources, J.H.H., S.M.L. and D.H.C.; writing—original draft preparation, H.D.J. and S.-Y.L.; writing—review and editing, H.D.J., S.-Y.L. and B.Y.C.; visualization, H.D.J.; supervision, S.-Y.L. and B.Y.C.; project administration, S.-Y.L. and B.Y.C.; funding acquisition, S.-Y.L. and B.Y.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI20C0285 to S.Y. Lee). This work was supported by the grant (No. 0420210670-2021 to S.Y. Lee) from the SNUH Research Fund. This study was also supported by the Basic Science Research Program through the NRF, funded by the Ministry of Education (Grant 2021R1A2C2092038 to Choi. B.Y.) and also by SNUBH intramural research funds (14-2021-0003 to Choi. B.Y. and 13-2022-0010 to Choi. B.Y.)
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Boards of Seoul National University Hospital (IRB-H-0905-041-281) and Seoul National University Bundang Hospital (IRB-B-1007-105-402).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Berninger, E.; Westling, B. Outcome of a universal newborn hearing-screening programme based on multiple transient-evoked otoacoustic emissions and clinical brainstem response audiometry. Acta Otolaryngol. 2011, 131, 728–739. [Google Scholar] [CrossRef] [PubMed]
- Van Camp, G.; Smith, R.J.H. Hereditary Hearing Loss Homepage. Available online: https://hereditaryhearingloss.org (accessed on 1 February 2022).
- Delmaghani, S.; El-Amraoui, A. Inner Ear Gene Therapies Take Off: Current Promises and Future Challenges. J. Clin. Med. 2020, 9, 2309. [Google Scholar] [CrossRef]
- Crick, F.H. On protein synthesis. Symp. Soc. Exp. Biol. 1958, 12, 138–163. [Google Scholar] [PubMed]
- Lambert, S.A.; Jolma, A.; Campitelli, L.F.; Das, P.K.; Yin, Y.; Albu, M.; Chen, X.; Taipale, J.; Hughes, T.R.; Weirauch, M.T. The Human Transcription Factors. Cell 2018, 172, 650–665. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.I.; Young, R.A. Transcriptional regulation and its misregulation in disease. Cell 2013, 152, 1237–1251. [Google Scholar] [CrossRef]
- Clark, J.G. Uses and abuses of hearing loss classification. ASHA 1981, 23, 493–500. [Google Scholar]
- Bahmad, F. Update on Hearing Loss; Bahmad, F., Ed.; IntechOpen Book Series; IntechOpen Limited: London, UK, 2015; p. 206. [Google Scholar]
- Liu, H.; Zhang, H.; Bentler, R.A.; Mo, L.; Han, D.; Zhang, L. Audiometric records analysis in a clinical population in China. ORL J. Otorhinolaryngol. Relat. Spec. 2011, 73, 237–245. [Google Scholar] [CrossRef]
- Pittman, A.L.; Stelmachowicz, P.G. Hearing loss in children and adults: Audiometric configuration, asymmetry, and progression. Ear Hear. 2003, 24, 198–205. [Google Scholar] [CrossRef]
- Lee, S.Y.; Han, S.C.; Han, J.H.; Kim, M.Y.; Oh, D.Y.; Kim, N.J.; Song, J.J.; Koo, J.W.; Lee, J.H.; Oh, S.H.; et al. Natural Course of Residual Hearing with Reference to GJB2 and SLC26A4 Genotypes: Clinical Implications for Hearing Rehabilitation. Ear Hear. 2021, 42, 644–653. [Google Scholar] [CrossRef]
- Sennaroglu, L.; Saatci, I. A new classification for cochleovestibular malformations. Laryngoscope 2002, 112, 2230–2241. [Google Scholar] [CrossRef]
- Lee, S.Y.; Choi, B.Y. Potential Implications of Slim Modiolar Electrodes for Severely Malformed Cochleae: A Comparison With the Straight Array With Circumferential Electrodes. Clin. Exp. Otorhinolaryngol. 2021, 14, 287–294. [Google Scholar] [CrossRef]
- Han, K.H.; Kim, A.R.; Kim, M.Y.; Ahn, S.; Oh, S.H.; Song, J.H.; Choi, B.Y. Establishment of a Flexible Real-Time Polymerase Chain Reaction-Based Platform for Detecting Prevalent Deafness Mutations Associated with Variable Degree of Sensorineural Hearing Loss in Koreans. PLoS ONE 2016, 11, e0161756. [Google Scholar] [CrossRef]
- Lee, S.Y.; Oh, D.Y.; Han, J.H.; Kim, M.Y.; Kim, B.; Kim, B.J.; Song, J.J.; Koo, J.W.; Lee, J.H.; Oh, S.H.; et al. Flexible Real-Time Polymerase Chain Reaction-Based Platforms for Detecting Deafness Mutations in Koreans: A Proposed Guideline for the Etiologic Diagnosis of Auditory Neuropathy Spectrum Disorder. Diagnostics 2020, 10, 672. [Google Scholar] [CrossRef]
- Lee, S.Y.; Joo, K.; Oh, J.; Han, J.H.; Park, H.R.; Lee, S.; Oh, D.Y.; Woo, S.J.; Choi, B.Y. Severe or Profound Sensorineural Hearing Loss Caused by Novel USH2A Variants in Korea: Potential Genotype-Phenotype Correlation. Clin. Exp. Otorhinolaryngol. 2020, 13, 113–122. [Google Scholar] [CrossRef]
- Lee, S.Y.; Choi, H.B.; Park, M.; Choi, I.S.; An, J.; Kim, A.; Kim, E.; Kim, N.; Han, J.H.; Kim, M.Y.; et al. Novel KCNQ4 variants in different functional domains confer genotype- and mechanism-based therapeutics in patients with nonsyndromic hearing loss. Exp. Mol. Med. 2021, 53, 1192–1204. [Google Scholar] [CrossRef]
- Lee, S.Y.; Han, J.H.; Carandang, M.; Kim, M.Y.; Kim, B.; Yi, N.; Kim, J.; Kim, B.J.; Oh, D.Y.; Koo, J.W.; et al. Novel genotype-phenotype correlation of functionally characterized LMX1A variants linked to sensorineural hearing loss. Hum. Mutat. 2020, 41, 1877–1883. [Google Scholar] [CrossRef]
- Oza, A.M.; DiStefano, M.T.; Hemphill, S.E.; Cushman, B.J.; Grant, A.R.; Siegert, R.K.; Shen, J.; Chapin, A.; Boczek, N.J.; Schimmenti, L.A.; et al. Expert specification of the ACMG/AMP variant interpretation guidelines for genetic hearing loss. Hum. Mutat. 2018, 39, 1593–1613. [Google Scholar] [CrossRef]
- Korean Reference Genome Database. Available online: http://152.99.75.168:9090/KRGDB (accessed on 17 August 2022).
- Stankovic, K.M.; Hennessey, A.M.; Herrmann, B.; Mankarious, L.A. Cochlear implantation in children with congenital X-linked deafness due to novel mutations in POU3F4 gene. Ann. Otol. Rhinol. Laryngol. 2010, 119, 815–822. [Google Scholar] [CrossRef]
- Smeds, H.; Wales, J.; Karltorp, E.; Anderlid, B.M.; Henricson, C.; Asp, F.; Anmyr, L.; Lagerstedt-Robinson, K.; Lofkvist, U. X-linked Malformation Deafness: Neurodevelopmental Symptoms Are Common in Children With IP3 Malformation and Mutation in POU3F4. Ear Hear. 2021, 43, 53–69. [Google Scholar] [CrossRef]
- Minowa, O.; Ikeda, K.; Sugitani, Y.; Oshima, T.; Nakai, S.; Katori, Y.; Suzuki, M.; Furukawa, M.; Kawase, T.; Zheng, Y.; et al. Altered cochlear fibrocytes in a mouse model of DFN3 nonsyndromic deafness. Science 1999, 285, 1408–1411. [Google Scholar] [CrossRef]
- de Kok, Y.J.; van der Maarel, S.M.; Bitner-Glindzicz, M.; Huber, I.; Monaco, A.P.; Malcolm, S.; Pembrey, M.E.; Ropers, H.H.; Cremers, F.P. Association between X-linked mixed deafness and mutations in the POU domain gene POU3F4. Science 1995, 267, 685–688. [Google Scholar] [CrossRef] [Green Version]
- Choi, B.Y.; An, Y.H.; Song, J.J.; Koo, J.W.; Lee, J.H.; Oh, S.H.; Chang, S.O.; Kim, C.S.; Park, J.H. Clinical observations and molecular variables of patients with hearing loss and incomplete partition type III. Laryngoscope 2016, 126, E123–E128. [Google Scholar] [CrossRef]
- Jang, J.H.; Oh, J.; Han, J.H.; Park, H.R.; Kim, B.J.; Lee, S.; Kim, M.Y.; Lee, S.; Oh, D.Y.; Choung, Y.H.; et al. Identification of a Novel Frameshift Variant of POU3F4 and Genetic Counseling of Korean Incomplete Partition Type III Subjects Based on Detailed Genotypes. Genet. Test. Mol. Biomark. 2019, 23, 423–427. [Google Scholar] [CrossRef]
- Tian, H.; Wang, L.; Gao, F.; Liang, W.; Peng, K.A. Cochlear implantation using a custom guide catheter in 14 patients with incomplete partition type III. Clin. Otolaryngol. 2018, 43, 1379–1383. [Google Scholar] [CrossRef] [PubMed]
- Kang, W.S.; Shim, B.S.; Lee, K.S. Audiologic performance after cochlear implantation in children with X-linked deafness: Comparison with deaf children with a normal inner ear structure. Otol. Neurotol. 2013, 34, 544–548. [Google Scholar] [CrossRef]
- Chao, X.; Xiao, Y.; Zhang, F.; Luo, J.; Wang, R.; Liu, W.; Wang, H.; Xu, L. Cochlear Implantation in a Patient with a Novel POU3F4 Mutation and Incomplete Partition Type-III Malformation. Neural. Plast. 2020, 2020, 8829587. [Google Scholar] [CrossRef]
- Vahava, O.; Morell, R.; Lynch, E.D.; Weiss, S.; Kagan, M.E.; Ahituv, N.; Morrow, J.E.; Lee, M.K.; Skvorak, A.B.; Morton, C.C.; et al. Mutation in transcription factor POU4F3 associated with inherited progressive hearing loss in humans. Science 1998, 279, 1950–1954. [Google Scholar] [CrossRef]
- Weiss, S.; Gottfried, I.; Mayrose, I.; Khare, S.L.; Xiang, M.; Dawson, S.J.; Avraham, K.B. The DFNA15 deafness mutation affects POU4F3 protein stability, localization, and transcriptional activity. Mol. Cell. Biol. 2003, 23, 7957–7964. [Google Scholar] [CrossRef]
- Cui, T.Y.; Gao, X.; Huang, S.S.; Sun, Y.Y.; Zhang, S.Q.; Jiang, X.X.; Yang, Y.Z.; Kang, D.Y.; Zhu, Q.W.; Yuan, Y.Y. Four Novel Variants in POU4F3 Cause Autosomal Dominant Nonsyndromic Hearing Loss. Neural. Plast. 2020, 2020, 6137083. [Google Scholar] [CrossRef]
- Freitas, E.L.; Oiticica, J.; Silva, A.G.; Bittar, R.S.; Rosenberg, C.; Mingroni-Netto, R.C. Deletion of the entire POU4F3 gene in a familial case of autosomal dominant non-syndromic hearing loss. Eur. J. Med. Genet. 2014, 57, 125–128. [Google Scholar] [CrossRef]
- He, L.; Pang, X.; Chen, P.; Wu, H.; Yang, T. Mutation in the Hair Cell Specific Gene POU4F3 Is a Common Cause for Autosomal Dominant Nonsyndromic Hearing Loss in Chinese Hans. Neural. Plast. 2016, 2016, 9890827. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cai, X.Z.; Li, Y.; Xia, L.; Peng, Y.; He, C.F.; Jiang, L.; Feng, Y.; Xia, K.; Liu, X.Z.; Mei, L.Y.; et al. Exome sequencing identifies POU4F3 as the causative gene for a large Chinese family with non-syndromic hearing loss. J. Hum. Genet 2017, 62, 317–320. [Google Scholar] [CrossRef]
- Gao, X.; Xu, J.C.; Wang, W.Q.; Yuan, Y.Y.; Bai, D.; Huang, S.S.; Wang, G.J.; Su, Y.; Li, J.; Kang, D.Y.; et al. A Missense Mutation in POU4F3 Causes Midfrequency Hearing Loss in a Chinese ADNSHL Family. Biomed. Res. Int. 2018, 2018, 5370802. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.H.; Lin, Y.H.; Lu, Y.C.; Liu, T.C.; Chen, C.Y.; Hsu, C.J.; Chen, P.L.; Wu, C.C. A novel missense variant in the nuclear localization signal of POU4F3 causes autosomal dominant non-syndromic hearing loss. Sci. Rep. 2017, 7, 7551. [Google Scholar] [CrossRef] [PubMed]
- Kitano, T.; Miyagawa, M.; Nishio, S.Y.; Moteki, H.; Oda, K.; Ohyama, K.; Miyazaki, H.; Hidaka, H.; Nakamura, K.I.; Murata, T.; et al. POU4F3 mutation screening in Japanese hearing loss patients: Massively parallel DNA sequencing-based analysis identified novel variants associated with autosomal dominant hearing loss. PLoS ONE 2017, 12, e0177636. [Google Scholar] [CrossRef]
- Bai, X.; Zhang, F.; Xiao, Y.; Jin, Y.; Zheng, Q.; Wang, H.; Xu, L. Identification of two novel mutations in POU4F3 gene associated with autosomal dominant hearing loss in Chinese families. J. Cell. Mol. Med. 2020, 24, 6978–6987. [Google Scholar] [CrossRef]
- Miyake, K.; Shirai, K.; Nishiyama, N.; Kawaguchi, S.; Ohta, Y.; Kawano, A.; Usami, S.I.; Kitano, T.; Tsukahara, K. Cochlear implantation in a patient with a POU4F3 mutation. Clin. Case Rep. 2021, 9, 298–303. [Google Scholar] [CrossRef]
- Eppsteiner, R.W.; Shearer, A.E.; Hildebrand, M.S.; Deluca, A.P.; Ji, H.; Dunn, C.C.; Black-Ziegelbein, E.A.; Casavant, T.L.; Braun, T.A.; Scheetz, T.E.; et al. Prediction of cochlear implant performance by genetic mutation: The spiral ganglion hypothesis. Hear. Res. 2012, 292, 51–58. [Google Scholar] [CrossRef]
- Wesdorp, M.; de Koning Gans, P.A.M.; Schraders, M.; Oostrik, J.; Huynen, M.A.; Venselaar, H.; Beynon, A.J.; van Gaalen, J.; Piai, V.; Voermans, N.; et al. Heterozygous missense variants of LMX1A lead to nonsyndromic hearing impairment and vestibular dysfunction. Hum. Genet 2018, 137, 389–400. [Google Scholar] [CrossRef]
- Schrauwen, I.; Chakchouk, I.; Liaqat, K.; Jan, A.; Nasir, A.; Hussain, S.; Nickerson, D.A.; Bamshad, M.J.; Ullah, A.; Ahmad, W.; et al. A variant in LMX1A causes autosomal recessive severe-to-profound hearing impairment. Hum. Genet 2018, 137, 471–478. [Google Scholar] [CrossRef]
- Ozieblo, D.; Lee, S.Y.; Leja, M.L.; Sarosiak, A.; Baldyga, N.; Skarzynski, H.; Kim, Y.; Han, J.H.; Yoo, H.S.; Park, M.H.; et al. Update on CD164 and LMX1A genes to strengthen their causative role in autosomal dominant hearing loss. Hum. Genet 2022, 141, 445–453. [Google Scholar] [CrossRef] [PubMed]
- Huang, A.; Yuan, Y.; Liu, Y.; Zhu, Q.; Dai, P. A novel EYA4 mutation causing hearing loss in a Chinese DFNA family and genotype-phenotype review of EYA4 in deafness. J. Transl. Med. 2015, 13, 154. [Google Scholar] [CrossRef] [PubMed]
- Makishima, T.; Madeo, A.C.; Brewer, C.C.; Zalewski, C.K.; Butman, J.A.; Sachdev, V.; Arai, A.E.; Holbrook, B.M.; Rosing, D.R.; Griffith, A.J. Nonsyndromic hearing loss DFNA10 and a novel mutation of EYA4: Evidence for correlation of normal cardiac phenotype with truncating mutations of the Eya domain. Am. J. Med. Genet. A 2007, 143, 1592–1598. [Google Scholar] [CrossRef]
- Choi, H.S.; Kim, A.R.; Kim, S.H.; Choi, B.Y. Identification of a novel truncation mutation of EYA4 in moderate degree hearing loss by targeted exome sequencing. Eur. Arch. Otorhinolaryngol. 2016, 273, 1123–1129. [Google Scholar] [CrossRef]
- Schonberger, J.; Wang, L.; Shin, J.T.; Kim, S.D.; Depreux, F.F.; Zhu, H.; Zon, L.; Pizard, A.; Kim, J.B.; Macrae, C.A.; et al. Mutation in the transcriptional coactivator EYA4 causes dilated cardiomyopathy and sensorineural hearing loss. Nat. Genet. 2005, 37, 418–422. [Google Scholar] [CrossRef]
- Shinagawa, J.; Moteki, H.; Nishio, S.Y.; Ohyama, K.; Otsuki, K.; Iwasaki, S.; Masuda, S.; Oshikawa, C.; Ohta, Y.; Arai, Y.; et al. Prevalence and clinical features of hearing loss caused by EYA4 variants. Sci. Rep. 2020, 10, 3662. [Google Scholar] [CrossRef]
- Morin, M.; Borreguero, L.; Booth, K.T.; Lachgar, M.; Huygen, P.; Villamar, M.; Mayo, F.; Barrio, L.C.; Santos Serrao de Castro, L.; Morales, C.; et al. Insights into the pathophysiology of DFNA10 hearing loss associated with novel EYA4 variants. Sci. Rep. 2020, 10, 6213. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).