Association of Oral Anticoagulation Prescription with Clinical Events in Patients with an Asymptomatic Unrepaired Abdominal Aortic Aneurysm
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. Follow-Up and Outcome Assessment
2.3. Statistical Analyses
2.4. Data Sharing
3. Results
3.1. Characteristics of Participants at Recruitment in Relation to Anticoagulant Drug Prescription
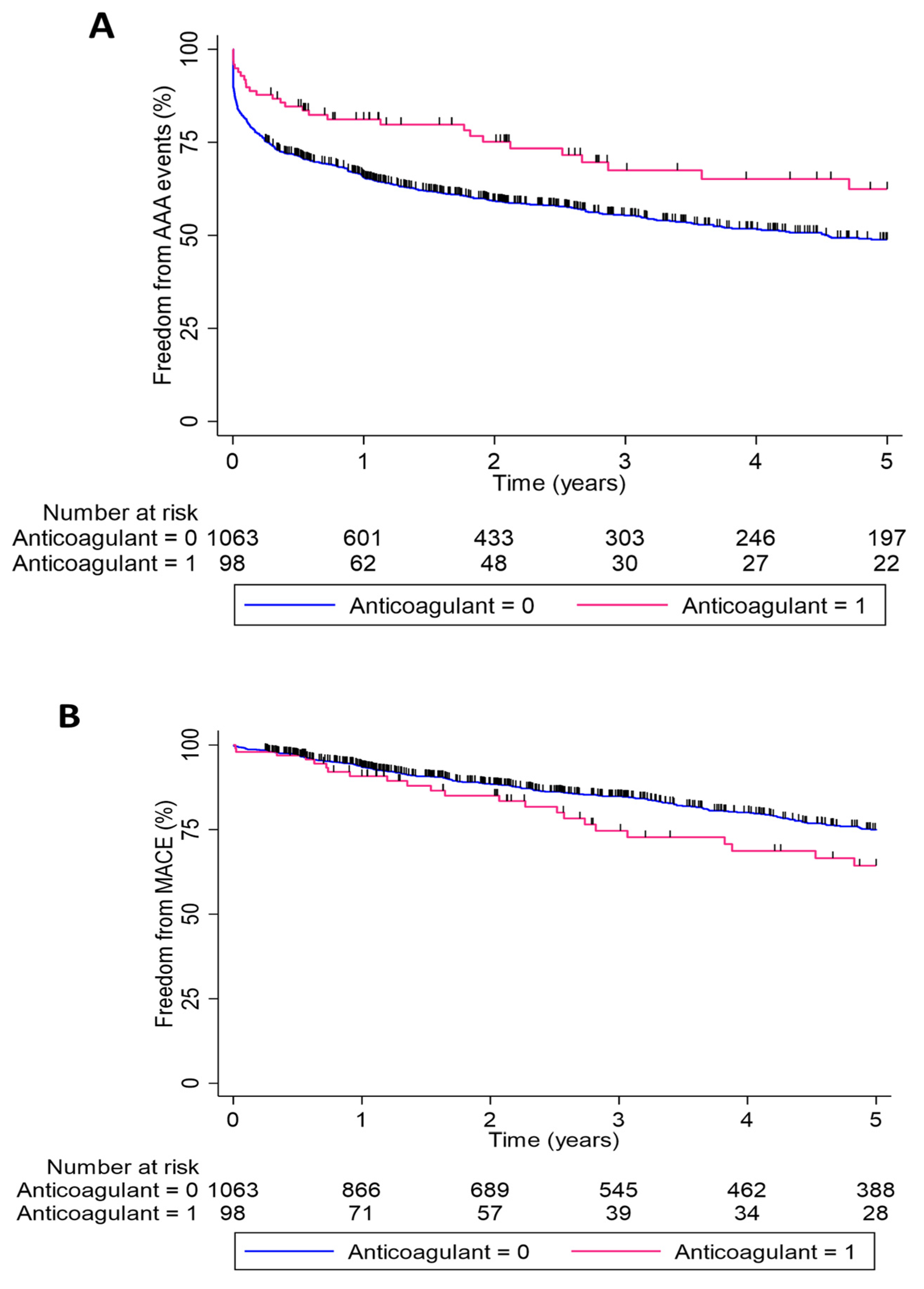
3.2. Outcome Events
3.3. Association of Outcome Events with Anticoagulant Drug Prescription
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mortality, G.B.D. Causes of Death C. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 385, 117–171. [Google Scholar]
- Nastasi, D.R.; Norman, R.; Moxon, J.V.; Quigley, F.; Velu, R.; Jenkins, J.; Golledge, J. The Potential Benefits and Costs of an Intensified Approach to Low Density Lipoprotein Cholesterol Lowering in People with Abdominal Aortic Aneurysm. Eur. J. Vasc. Endovasc. Surg. 2021, 62, 643–650. [Google Scholar] [CrossRef] [PubMed]
- Golledge, J. Abdominal aortic aneurysm: Update on pathogenesis and medical treatments. Nat. Rev. Cardiol. 2019, 16, 225–242. [Google Scholar] [CrossRef] [PubMed]
- Parr, A.M.M.; Bradshaw, B.; Shahzad, A.; Buttner, P.; Golledge, J. Thrombus volume is associated with cardiovascular events and aneurysm growth in patients who have abdominal aortic aneurysms. J. Vasc. Surg. 2011, 53, 28–35. [Google Scholar] [CrossRef]
- Golledge, J.; Wolanski, P.; Parr, A.; Buttner, P. Measurement and determinants of infrarenal aortic thrombus volume. Eur. Radiol. 2008, 18, 1987–1994. [Google Scholar] [CrossRef]
- Michel, J.-B.; Martin-Ventura, J.-L.; Egido, J.; Sakalihasan, N.; Treska, V.; Lindholt, J.; Allaire, E.; Thorsteinsdottir, U.; Cockerill, G.; Swedenborg, J.; et al. Novel aspects of the pathogenesis of aneurysms of the abdominal aorta in humans. Cardiovasc. Res. 2011, 90, 18–27. [Google Scholar] [CrossRef]
- Golledge, J.; Muller, R.; Clancy, P.; McCann, M.; Norman, P.E. Evaluation of the diagnostic and prognostic value of plasma D-dimer for abdominal aortic aneurysm. Eur. Heart J. 2011, 32, 354–364. [Google Scholar] [CrossRef]
- Zagrapan, B.; Eilenberg, W.; Prausmueller, S.; Nawrozi, P.; Muench, K.; Hetzer, S.; Elleder, V.; Rajic, R.; Juster, F.; Martelanz, L.; et al. A Novel Diagnostic and Prognostic Score for Abdominal Aortic Aneurysms Based on D-Dimer and a Comprehensive Analysis of Myeloid Cell Parameters. Thromb. Haemost. 2019, 119, 807–820. [Google Scholar] [CrossRef]
- Zhu, C.; Leach, J.R.; Wang, Y.; Gasper, W.; Saloner, D.; Hope, M.D. Intraluminal Thrombus Predicts Rapid Growth of Abdominal Aortic Aneurysms. Radiology 2020, 294, 707–713. [Google Scholar] [CrossRef]
- Fan, Y.-N.; Ke, X.; Yi, Z.-L.; Lin, Y.-Q.; Deng, B.-Q.; Shu, X.-R.; Yang, D.-H.; Liao, Z.-Y.; Nie, R.-Q. Plasma D-dimer as a predictor of intraluminal thrombus burden and progression of abdominal aortic aneurysm. Life Sci. 2020, 240, 117069. [Google Scholar] [CrossRef]
- Ding, Y.; Li, X.; Zhou, M.; Cai, L.; Tang, H.; Xie, T.; Shi, Z.; Fu, W. Factor Xa inhibitor rivaroxaban suppresses experimental abdominal aortic aneurysm progression via attenuating aortic inflammation. Vascul. Pharmacol. 2021, 136, 106818. [Google Scholar] [CrossRef]
- Cameron, S.J.; Russell, H.M.; Owens, A.P., 3rd. Antithrombotic therapy in abdominal aortic aneurysm: Beneficial or detrimental? Blood 2018, 132, 2619–2628. [Google Scholar] [CrossRef]
- Moran, C.S.; Seto, S.-W.; Krishna, S.; Sharma, S.; Jose, R.J.; Biros, E.; Wang, Y.; Morton, S.K.; Golledge, J. Parenteral administration of factor Xa/IIa inhibitors limits experimental aortic aneurysm and atherosclerosis. Sci. Rep. 2017, 7, 43079. [Google Scholar] [CrossRef]
- Wanhainen, A.; Verzini, F.; van Herzeele, I.; Allaire, E.; Bown, M.; Cohnert, T.; Dick, F.; van Herwaarden, J.; Karkos, C.; Koelemay, M.; et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms. Eur. J. Vasc. Endovasc. Surg. 2019, 57, 8–93. [Google Scholar] [CrossRef]
- Chaikof, E.L.; Dalman, R.L.; Eskandari, M.K.; Jackson, B.M.; Lee, W.A.; Mansour, M.A.; Mastracci, T.M.; Mell, M.; Murad, M.H.; Nguyen, L.L.; et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J. Vasc. Surg. 2018, 67, 2–77. [Google Scholar] [CrossRef]
- Golledge, J.; Velu, R.; Quigley, F.; Jenkins, J.; Singh, T.P. Editor’s Choice—Cohort Study Examining the Association Between Abdominal Aortic Size and Major Adverse Cardiovascular Events in Patients with Aortic and Peripheral Occlusive and Aneurysmal Disease. Eur. J. Vasc. Endovasc. Surg. 2021, 62, 960–968. [Google Scholar] [CrossRef]
- Golledge, J.M.D.; Pinchbeck, J.; Rowbotham, S.; Jenkins, J.; Bourke, M.; Bourke, B.; Norman, P.E.; Jones, R.; Moxon, J.V. Editor’s Choice—Metformin Prescription is Associated with a Reduction in the Combined Incidence of Surgical Repair and Rupture Related Mortality in Patients with Abdominal Aortic Aneurysm. Eur. J. Vasc. Endovasc. Surg. 2019, 57, 94–101. [Google Scholar] [CrossRef]
- Biccire, F.G.; Farcomeni, A.; Gaudio, C.; Pignatelli, P.; Tanzilli, G.; Pastori, D. D-dimer for risk stratification and antithrombotic treatment management in acute coronary syndrome patients: Asystematic review and metanalysis. Thromb. J. 2021, 19, 102. [Google Scholar] [CrossRef]
- Zamorano-Leon, J.J.; de la Serna-Soto, M.; Moñux, G.; Freixer, G.; Zekri-Nechar, K.; Cabrero-Fernandez, M.; Segura, A.; Gonzalez-Cantalapiedra, A.; Serrano, J.; Farré, A.L. Factor Xa Inhibition by Rivaroxaban Modified Mitochondrial-Associated Proteins in Human Abdominal Aortic Aneurysms. Ann. Vasc. Surg. 2020, 67, 482–489. [Google Scholar] [CrossRef]
- Moñux, G.; Zamorano-León, J.J.; Marqués, P.; Sopeña, B.; García-García, J.M.; De Koller, G.L.; Calvo-Rico, B.; García-Fernandez, M.A.; Serrano, J.; López-Farré, A. FXa inhibition by rivaroxaban modifies mechanisms associated with the pathogenesis of human abdominal aortic aneurysms. Br. J. Clin. Pharmacol. 2017, 83, 2661–2670. [Google Scholar] [CrossRef]
- Wemmelund, H.; Jorgensen, T.M.; Hogh, A.; Behr-Rasmussen, C.; Johnsen, S.P.; Lindholt, J.S. Low-dose aspirin and rupture of abdominal aortic aneurysm. J. Vasc. Surg. 2017, 65, 616–625. [Google Scholar] [CrossRef] [Green Version]
- Lindholt, J.S.; Sorensen, H.T.; Michel, J.B.; Thomsen, H.F.; Henneberg, E.W. Low-dose aspirin may prevent growth and later surgical repair of medium-sized abdominal aortic aneurysms. Vasc. Endovascular. Surg. 2008, 42, 329–334. [Google Scholar] [CrossRef]
- Wanhainen, A.; Mani, K.; Kullberg, J.; Svensjö, S.; Bersztel, A.; Karlsson, L.; Holst, J.; Gottsäter, A.; Linné, A.; Gillgren, P.; et al. The effect of ticagrelor on growth of small abdominal aortic aneurysms—A randomized controlled trial. Cardiovasc. Res. 2020, 116, 450–456. [Google Scholar] [CrossRef]
- Morisaki, K.; Matsubara, Y.; Furuyama, T.; Kurose, S.; Yoshino, S.; Yamashita, S.; Mori, M. Effects of antithrombotic therapy on abdominal aortic aneurysm sac size after endovascular repair in patients with favorable neck anatomy. J. Vasc. Interv. Radiol. 2021, 33, 113–119. [Google Scholar] [CrossRef]
- Seike, Y.; Tanaka, H.; Fukuda, T.; Itonaga, T.; Morita, Y.; Oda, T.; Inoue, Y.; Sasaki, H.; Minatoya, K.; Kobayashi, J. Influence of warfarin therapy on the occurrence of postoperative endoleaks and aneurysm sac enlargement after endovascular abdominal aortic aneurysm repair. Interact. Cardiovasc. Thorac. Surg. 2017, 24, 615–618. [Google Scholar] [CrossRef]
- Flohr, T.R.; Snow, R.; Aziz, F. The fate of endoleaks after endovascular aneurysm repair and the impact of oral anticoagulation on their persistence. J. Vasc. Surg. 2021, 74, 1183–1192. [Google Scholar] [CrossRef]
- Elbadawi, A.; Omer, M.; Ogunbayo, G.; Owens, A.P., III; Mix, D.; Lyden, S.P.; Cameron, S.J. Antiplatelet medications protect against aortic dissection and rupture in patients with abdominal aortic aneurysms. J. Am. Coll. Cardiol. 2020, 75, 1609–1610. [Google Scholar] [CrossRef]
| Factor | Prescribed Anticoagulant | p Value | |
|---|---|---|---|
| Yes | No | ||
| Number | 98 | 1063 | |
| Age (years) | 73.9 ± 7.6 | 73.0 ± 7.7 | 0.247 |
| Female | 17 (17.4%) | 188 (17.7%) | 0.933 |
| Smoking | 0.258 | ||
| Current | 22 (22.5%) | 282 (26.5%) | |
| Former | 67 (68.4%) | 640 (60.2%) | |
| Never | 9 (9.2%) | 141 (13.3%) | |
| Diabetes | 26 (26.5%) | 219 (20.6%) | 0.169 |
| Hypertension | 81 (82.7%) | 801 (75.4%) | 0.106 |
| Ischemic heart disease | 76 (77.6%) | 504 (47.4%) | <0.001 |
| Family history of aortic or peripheral aneurysm | 11 (11.2%) | 108 (10.2%) | 0.740 |
| Stroke | 15 (15.3%) | 101 (9.5%) | 0.067 |
| Aspirin | 32 (32.7%) | 649 (61.1%) | <0.001 |
| Other antiplatelet | 10 (10.2%) | 180 (16.9%) | 0.085 |
| Statin | 74 (75.5%) | 693 (65.2%) | 0.039 |
| Metformin | 12 (12.2%) | 127 (12.0%) | 0.931 |
| Frusemide prescribed for cardiac failure | 25 (25.5%) | 79 (7.4%) | <0.001 |
| Body mass index * | 28.2 ± 4.9 | 27.6 ± 5.0 | 0.251 |
| Initial AAA diameter | 44.2 ± 10.3 | 46.5 ± 11.4 | 0.053 |
| Follow-up (years) | 4.5 ± 4.3 | 4.9 ± 4.0 | 0.299 |
| AAA repair or AAA rupture related mortality | 32 (32.7%) | 504 (47.4%) | 0.005 |
| Major adverse cardiovascular events | 30 (30.6%) | 289 (27.2%) | 0.467 |
| Myocardial infarction | 10 (10.2%) | 109 (10.3%) | 0.988 |
| Stroke | 6 (6.1%) | 59 (5.6%) | 0.814 |
| Cardiovascular death | 22 (22.4%) | 202 (19.0%) | 0.408 |
| All-cause death | 42 (42.9%) | 394 (37.1%) | 0.257 |
| Model | Hazard Ratio | 95% Confidence Intervals | p Value |
|---|---|---|---|
| Unadjusted | 0.61 | 0.43, 0.87 | 0.007 |
| Adjusted * | 0.62 | 0.43, 0.89 | 0.010 |
| Adjusted † | 0.62 | 0.43, 0.89 | 0.010 |
| Adjusted ‡ | 0.61 | 0.42, 0.90 | 0.013 |
| Model | Hazard Ratio | 95% Confidence Intervals | p Value |
|---|---|---|---|
| Unadjusted | 1.25 | 0.86, 1.82 | 0.252 |
| Adjusted * | 1.27 | 0.87, 1.85 | 0.220 |
| Adjusted † | 1.09 | 0.74, 1.59 | 0.672 |
| Adjusted ‡ | 1.16 | 0.78, 1.72 | 0.476 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Golledge, J.; Jenkins, J.; Bourke, M.; Bourke, B.; Singh, T.P. Association of Oral Anticoagulation Prescription with Clinical Events in Patients with an Asymptomatic Unrepaired Abdominal Aortic Aneurysm. Biomedicines 2022, 10, 2112. https://doi.org/10.3390/biomedicines10092112
Golledge J, Jenkins J, Bourke M, Bourke B, Singh TP. Association of Oral Anticoagulation Prescription with Clinical Events in Patients with an Asymptomatic Unrepaired Abdominal Aortic Aneurysm. Biomedicines. 2022; 10(9):2112. https://doi.org/10.3390/biomedicines10092112
Chicago/Turabian StyleGolledge, Jonathan, Jason Jenkins, Michael Bourke, Bernard Bourke, and Tejas P. Singh. 2022. "Association of Oral Anticoagulation Prescription with Clinical Events in Patients with an Asymptomatic Unrepaired Abdominal Aortic Aneurysm" Biomedicines 10, no. 9: 2112. https://doi.org/10.3390/biomedicines10092112
APA StyleGolledge, J., Jenkins, J., Bourke, M., Bourke, B., & Singh, T. P. (2022). Association of Oral Anticoagulation Prescription with Clinical Events in Patients with an Asymptomatic Unrepaired Abdominal Aortic Aneurysm. Biomedicines, 10(9), 2112. https://doi.org/10.3390/biomedicines10092112






