PMMA Bone Cement: Antibiotic Elution and Mechanical Properties in the Context of Clinical Use
Abstract
1. Introduction
2. Indications for ALBCs in Arthroplasty
3. Mechanical Properties of Hardened PMMA Cement
3.1. Requirements
3.2. Type of Antibiotic
3.3. Proportion of Antibiotic in the Bone Cement
3.4. Loading Technique
3.5. Legal Implications
4. Antibiotic Elution from ALBCs
4.1. Choice of Cement
4.2. Geometry of the Cement Body
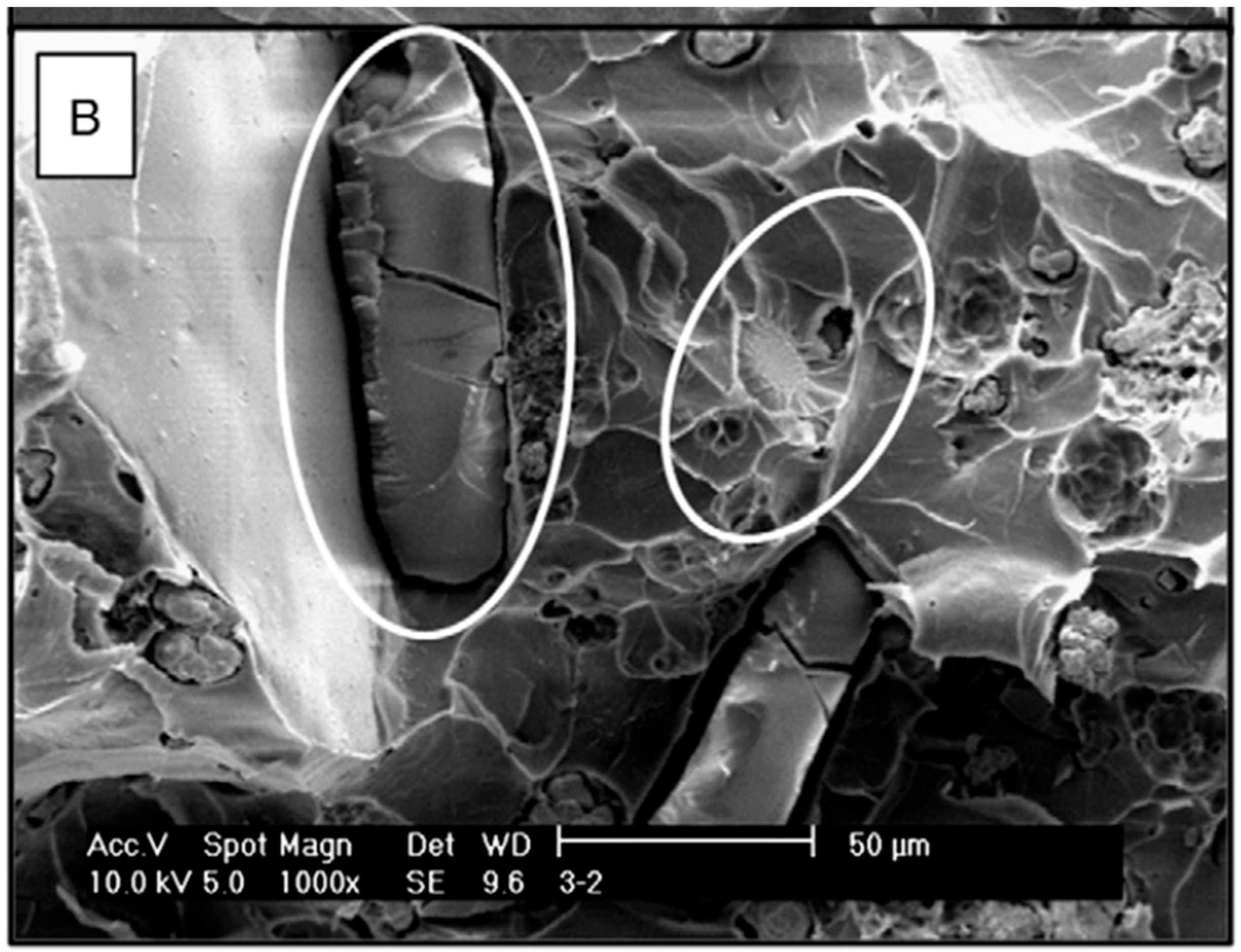
4.3. Porosity of the Cured Cement
4.4. Antibiotic and Antibiotic Combinations
5. Future Directions
6. Summary
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Antibiotic Group | Type of Antibiotic | Activity Against | Dose per 40 g Cement (in Grams) |
|---|---|---|---|
| Aminoglycoside | Tobramycin | Gram-negative bacteria such as Pseudomonas | 1 to 4.8 |
| Aminoglycoside | Gentamicin | Gram-negative bacteria—Eschericcia coli, Klebsiella and particularly Pseudomonas aeroginosa. Additionally, aerobic bacteria (not obligate/facultative anaerobes) | 0.25 to 4.8 |
| Cephalosporin, 1st gen | Cefazolin | Gram-positive infections, limited Gram negative coverage | 1 to 2 |
| Cephalosporin, 2nd gen | Cefuroxime | Reduced gram-positive coverage, improved gram-negative coverage | 1.5 to 2 |
| Cephalosporin, 3rd gen | Ceflazidime | Gram-negative bacteria, particularly Pseudomonas | 2 |
| Cephalosporin, 4th gen | Cefotaxime | Gram-negative bacteria, no activity against Pseudomonas | 2 |
| Cephalosporin, 5th gen | Ceftaroline | Gram-negative bacteria, no activity against Pseudomonas | 2 to 4 |
| Fluoroquinolone | Ciprofloxacin | Gram-negative organisms including activity against Enterobacteriaciae | 0.2 to 3 |
| Glycopeptide | Vancomycin | Gram-positive bacteria, including methicillin-resistant organisms | 0.5 to 4 |
| Lincosamide | Clindamycin | Gram-positive cocci, anaerobes | 1 to 2 |
| Macrolide | Erythromycin | Aerobic gram-positive cocci and bacilli | 0.5 to 1 |
| Polymyxin | Colistin | Gram-negative | 0.24 |
| ß-lactam | Piperacillin—not available Piptzobactam | Gram-negative bacteria (particularly Pseudomonas), Enterobacteria and anaerobes | 4 to 8 |
| ß-lactam | Aztreonam | Only gram-negative bacteria | 4 |
| ß-lactamase inhibitor | Tazobactam | Gram-negative bacteria (particularly Pseudomonas), Enterobacteria and anaerobes in combination with Piperacillin | 0.5 |
| Oxazolidinones | Linezolid | Multidrug-resistant gram-positive cocci such as MRSA | 1.2 |
| Carbapenem | Meropenem | Gram-positive and gram-negative bacteria, anaerobes, Pseudomonas | 0.5 to 4 |
| Lipopeptide | Daptomycin | Only gram-positive organisms | 2 |
| Antifungals | Amphotericin | Most Fungi | 200 |
| Antifungal | Voricanazole | Most Fungi | 300–600 mg |
| Antibiotic Groups | Antibiotics | Activity against | Cement Example |
|---|---|---|---|
| Aminoglycoside and Lincosamide | Gentamicin and Clindamycin | Many gram-positive and—negative bacteria (Staphylococcus species, Enterococcus species, Pseudomonas, Escherichia coli, Klebsiella, Proteus | Copal® G+C |
| Aminoglycoside and Glycopeptide | Gentamicin and Vancomycin | Many gram-positive bacteria (Staphylococcus species, MRSA, MRSE, Enterococcus species | Copal® G+V |
| Macrolide and Polymyxin | Erythromycin and Colistin | Gram-positive bacteria (Streptococcus species, Staphylococcus species), anaerobic bacteria (Corynebacteria) | Simplex® with Erythromycin/Colistin |
References
- Zahar, A.; Hannah, P. Addition of antibiotics to bone cement for septic prosthesis exchange. Oper. Orthop. Traumatol. 2016, 28, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Ensing, G.T.; van Horn, J.R.; van der Mei, H.C.; Busscher, H.J.; Neut, D. Copal bone cement is more effective in preventing biofilm formation than Palacos R-G. Clin. Orthop. Relat. Res. 2008, 466, 1492–1498. [Google Scholar] [CrossRef] [PubMed]
- Boelch, S.P.; Rueckl, K.; Fuchs, C.; Jordan, M.; Knauer, M.; Steinert, A.; Rudert, M.; Luedemann, M. Comparison of Elution Characteristics and Compressive Strength of Biantibiotic-Loaded PMMA Bone Cement for Spacers: Copal(R) Spacem with Gentamicin and Vancomycin versus Palacos(R) R+G with Vancomycin. Biomed. Res. Int. 2018, 2018, 4323518. [Google Scholar] [CrossRef] [PubMed]
- Paz, E.P.; Abenojar, J.; Vaquero-Martín, J.; Forriol, F.; Del Real, J.C. Evaluation of Elution and Mechanical Properties of High-Dose Antibiotic-Loaded Bone Cement: Comparative "In Vitro" Study of the Influence of Vancomycin and Cefazolin. J. Arthroplast. 2015, 30, 1423–1429. [Google Scholar] [CrossRef] [PubMed]
- Anagnostakos, K.; Meyer, C. Antibiotic Elution from Hip and Knee Acrylic Bone Cement Spacers: A Systematic Review. Biomed. Res. Int. 2017, 2017, 4657874. [Google Scholar] [CrossRef]
- Kuhn, K.D.; Renz, N.; Trampuz, A. Local antibiotic therapy. Unfallchirurgy 2017, 120, 561–572. [Google Scholar] [CrossRef]
- Wahlig, H.; Buchholz, H.W. Experimental and clinical studies on the release of gentamicin from bone cement. Chirurgy 1972, 43, 441–445. [Google Scholar]
- Wahlig, H.; Buchholz, D.E.B.H.; Bachmann, M. Pharmacokinetic study of gentamicin-loaded cement in total hip replacements: Comparative effects of varying dosage. J. Bone Jt. Surgery. Br. Vol. 1984, 66, 175–179. [Google Scholar] [CrossRef]
- Ben-Shlomo, Y.; Blom, A.; Boulton, C.; Brittain, R.; Clark, E.; Craig, R.; Dawson-Bowling, S.; Deere, K.; Esler, C.; Espinoza, O.; et al. The National Joint Registry 17th Annual Report 2020; National Joint Registry: London, UK, 2020. [Google Scholar]
- Grimberg, A.; Jansson, V.; Lutzner, J.; Melsheimer, O.; Morlock, M.; Steinbrück, A. EPRD Jahresbericht 2020. Available online: https://www.eprd.de/de/ueber-uns/aktuelles/artikel/eprd-veroeffentlicht-jahresbericht-2020 (accessed on 2 January 2022).
- Kuhn, K.D. PMMA Cements; Kraplow, D., Ed.; Springer: Berlin, Germany, 2014. [Google Scholar]
- Namba, R.S.; Prentice, H.A.; Paxton, E.W.; Hinman, A.D.; Kelly, M.P. Commercially Prepared Antibiotic-Loaded Bone Cement and Infection Risk Following Cemented Primary Total Knee Arthroplasty. J. Bone Jt. Surg. Am. 2020, 102, 1930–1938. [Google Scholar] [CrossRef]
- Tan, T.L. When to Use Commercially Available Antibiotic Cement: An Ongoing Debate: Commentary on an article by Namba, R.S. Commercially Prepared Antibiotic-Loaded Bone Cement and Infection Risk Following Cemented Primary Total Knee Arthroplasty. J. Bone Jt. Surg Am. 2020, 102, e127. [Google Scholar] [CrossRef]
- Parvizi, J.; Gehrke, T.; Chen, A.F. Proceedings of the International Consensus on Periprosthetic Joint Infection. Bone Jt. J. 2013, 95, 1450–1452. [Google Scholar] [CrossRef]
- Jameson, S.S.; Asaad, A.; Diament, M.; Kasim, A.; Bigirumurame, T.; Baker, P.; Mason, J.; Partington, P.; Reed, M. Antibiotic-loaded bone cement is associated with a lower risk of revision following primary cemented total knee arthroplasty: An analysis of 731,214 cases using National Joint Registry data. Bone Jt. J. 2019, 101, 1331–1347. [Google Scholar] [CrossRef]
- Anagnostakos, K. Therapeutic Use of Antibiotic-loaded Bone Cement in the Treatment of Hip and Knee Joint Infections. J. Bone Jt. Infect. 2017, 2, 29–37. [Google Scholar] [CrossRef]
- Kelm, J.; Schmitt, E.; Jung, W.; Anagnostakos, K. In vivo and in vitro studies of antibiotic release from and bacterial growth inhibition by antibiotic-impregnated polymethylmethacrylate hip spacers. Antimicrob. Agents Chemother. 2006, 50, 332–335. [Google Scholar] [CrossRef]
- Kunutsor, S.K.; Whitehouse, M.R.; Lenguerrand, E.; Blom, A.W.; Beswick, A.D.; Team, I. Re-Infection Outcomes Following One- And Two-Stage Surgical Revision of Infected Knee Prosthesis: A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0151537. [Google Scholar] [CrossRef]
- ISO 5833; Implants for Surgery–Acrylic Resins Cements. International Organization for Standardization: Geneva, Switzerland, 2002.
- Hsieh, P.H.; Tai, C.L.; Lee, P.C.; Chang, Y.H. Liquid gentamicin and vancomycin in bone cement: A potentially more cost-effective regimen. J. Arthroplast. 2009, 24, 125–130. [Google Scholar] [CrossRef]
- Galvez-Lopez, R.; Pena-Monje, A.; Antelo-Lorenzo, R.; Guardia-Olmedo, J.; Moliz, J.; Hernandez-Quero, J.; Parra-Ruiz, J. Elution kinetics, antimicrobial activity, and mechanical properties of 11 different antibiotic loaded acrylic bone cement. Diagn. Microbiol. Infect. Dis. 2014, 78, 70–74. [Google Scholar] [CrossRef]
- Lilikakis, A. The effect of vancomycin addition to the compression strength of antibiotic-loaded bone cements. Int. Orthop. 2009, 33, 815–819. [Google Scholar] [CrossRef]
- Boelch, S.P.; Jordan, M.C.; Arnholdt, J.; Rudert, M.; Luedemann, M.; Steinert, A.F. Loading with vancomycin does not decrease gentamicin elution in gentamicin premixed bone cement. J. Mater. Sci. Mater. Med. 2017, 28, 104. [Google Scholar] [CrossRef]
- Lachiewicz, P.F.; Wellman, S.S.; Peterson, J.R. Antibiotic Cement Spacers for Infected Total Knee Arthroplasties. J. Am. Acad. Orthop. Surg. 2020, 28, 180–188. [Google Scholar] [CrossRef]
- Parvizi, J. Antibiotic Spacers in the Infected Hip: Optimizing Placement. Current Concepts in Joint Replacement. Orthop. Proc. 2017, 99, 126. [Google Scholar]
- Laine, J.C.; Nguyen, T.Q.; Buckley, J.M.; Kim, H.T. Effects of mixing techniques on vancomycin-impregnated polymethylmethacrylate. J. Arthroplast. 2011, 26, 1562–1566. [Google Scholar] [CrossRef]
- Lee, S.H.; Tai, C.L.; Chen, S.Y.; Chang, C.H.; Chang, Y.H.; Hsieh, P.H. Elution and Mechanical Strength of Vancomycin-Loaded Bone Cement: In Vitro Study of the Influence of Brand Combination. PLoS ONE 2016, 11, e0166545. [Google Scholar] [CrossRef]
- van de Belt, H.; Uges, D.R.; Schenk, W.; van Horn, J.R.; van der Mei, H.C.; Busscher, H.J. Surface roughness, porosity and wettability of gentamicin-loaded bone cements and their antibiotic release. Biomaterials 2000, 21, 1981–1987. [Google Scholar] [CrossRef]
- Duey, R.E.; Chong, A.C.; McQueen, D.A.; Womack, J.L.; Song, Z.; Steinberger, T.A.; Wooley, P.H. Mechanical properties and elution characteristics of polymethylmethacrylate bone cement impregnated with antibiotics for various surface area and volume constructs. Orthop. J. 2012, 32, 104–115. [Google Scholar]
- Masri, B.A.; Duncan, C.P.; Beauchamp, C.P.; Paris, N.J.; Arntorp, J. Effect of varying surface patterns on antibiotic elution from antibiotic-loaded bone cement. J. Arthroplast. 1995, 10, 453–459. [Google Scholar] [CrossRef]
- Schurman, D.J.; Trindade, C.; Hirshman, H.P.; Moser, K.; Kajiyama, G.; Stevens, P. Antibiotic-acrylic bone cement composites. Studies of gentamicin and Palacos. J. Bone Jt. Surg. Am. 1978, 60, 978–984. [Google Scholar] [CrossRef]
- Miller, R.; Leon, C.; McLemore, R. Mixing method affects elution and strength of high-dose ALBC: A pilot study. Clin. Orthop. Relat. Res. 2012, 470, 2677–2683. [Google Scholar] [CrossRef]
- Frommelt, L.; Kühn, K.D. Properties of Bone Cement–Antibiotic Loaded Bone Cement; Frommelt, L., Kühn, K.D., Eds.; Springer: Berlin, Germany, 2005. [Google Scholar]
- McLaren, A.C.; Nugent, M.; Economopoulos, K.; Kaul, H.; Vernon, B.L.; McLemore, R. Hand-mixed and premixed antibiotic-loaded bone cement have similar homogeneity. Clin. Orthop. Relat. Res. 2009, 467, 1693–1698. [Google Scholar] [CrossRef]
- Lewis, G.; Janna, S.; Bhattaram, A. Influence of the method of blending an antibiotic powder with an acrylic bone cement powder on physical, mechanical, and thermal properties of the cured cement. Biomaterials 2005, 26, 4317–4325. [Google Scholar] [CrossRef]
- Samelis, P.V.; Papagrigorakis, E.; Sameli, E.; Mavrogenis, A.; Savvidou, O.; Koulouvaris, P. Current Concepts on the Application, Pharmacokinetics and Complications of Antibiotic-Loaded Cement Spacers in the Treatment of Prosthetic Joint Infections. Cureus 2022, 14, e20968. [Google Scholar] [CrossRef] [PubMed]
- Meyer, J.; Spiegel, C.A.; Hetzel, S.; Squire, M. Vacuum-Mixing Significantly Changes Antibiotic Elution Characteristics of Commercially Available Antibiotic-Impregnated Bone Cements. J. Bone Jt. Surg. Am. Vol. 2011, 93, 2049–2056. [Google Scholar] [CrossRef] [PubMed]
- Wu, K.; Chen, Y.C.; Hsu, Y.M.; Chang, C.H. Enhancing Drug Release from Antibiotic-loaded Bone Cement Using Porogens. J. Am. Acad. Orthop. Surg. 2016, 24, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Shi, M.; Kretlow, J.D.; Spicer, P.P.; Tabata, Y.; Demian, N.; Wong, M.E.; Kasper, F.K.; Mikos, A.G. Antibiotic-releasing porous polymethylmethacrylate/gelatin/antibiotic constructs for craniofacial tissue engineering. J. Control Release 2011, 152, 196–205. [Google Scholar] [CrossRef]
- Chen, L.; Tang, Y.; Zhao, K.; Zha, X.; Liu, J.; Bai, H.; Wu, Z. Fabrication of the antibiotic-releasing gelatin/PMMA bone cement. Colloids Surf. B Biointerfaces 2019, 183, 110448. [Google Scholar] [CrossRef]
- Fini, G.G.; Aldini, N.N.; Torricelli, P.; Botter, R.; Beruto, D.; Giardino, R. A bone substitute composed of polymethylmethacrylate and α-tricalcium phosphate: Results in terms of osteoblast function and bone tissue formation. Biomaterials 2002, 23, 196. [Google Scholar] [CrossRef]
- Bitsch, R.G.; Kretzer, J.P.; Vogt, S.; Buchner, H.; Thomsen, M.N.; Lehner, B. Increased antibiotic release and equivalent biomechanics of a spacer cement without hard radio contrast agents. Diagn. Microbiol. Infect. Dis. 2015, 83, 203–209. [Google Scholar] [CrossRef]
- Renner, L.; Perka, C.; Trampuz, A.; Renz, N. Treatment of periprosthetic infections. Chirurgy 2016, 87, 831–838. [Google Scholar] [CrossRef]
- Kaplan, L.; Kurdziel, M.; Baker, K.C.; Verner, J. Characterization of daptomycin-loaded antibiotic cement. Orthopedics 2012, 35, e503–e509. [Google Scholar] [CrossRef][Green Version]
- Gentile, P.; Chiono, V.; Carmagnola, I.; Hatton, P.V. An overview of poly(lactic-co-glycolic) acid (PLGA)-based biomaterials for bone tissue engineering. Int. J. Mol. Sci. 2014, 15, 3640–3659. [Google Scholar] [CrossRef]
- Wall, V.; Nguyen, T.H.; Nguyen, N.; Tran, P.A. Controlling Antibiotic Release from Polymethylmethacrylate Bone Cement. Biomedicines 2021, 9, 26. [Google Scholar] [CrossRef]
| Factors for Particular Consideration | Issue |
|---|---|
| (1) Choice of cement | Cement brand and type |
| (2) Geometry of the cement body | Volume and surface area of the cement |
| (3) Porosity of the cured cement | Use of a vacuum system, homogenization of antibiotic to the cement powder, porogens in the cement |
| (4) Antibiotic and antibiotic combinations | Choice of antibiotic, proportion in the cement, combinations |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
von Hertzberg-Boelch, S.P.; Luedemann, M.; Rudert, M.; Steinert, A.F. PMMA Bone Cement: Antibiotic Elution and Mechanical Properties in the Context of Clinical Use. Biomedicines 2022, 10, 1830. https://doi.org/10.3390/biomedicines10081830
von Hertzberg-Boelch SP, Luedemann M, Rudert M, Steinert AF. PMMA Bone Cement: Antibiotic Elution and Mechanical Properties in the Context of Clinical Use. Biomedicines. 2022; 10(8):1830. https://doi.org/10.3390/biomedicines10081830
Chicago/Turabian Stylevon Hertzberg-Boelch, Sebastian Philipp, Martin Luedemann, Maximilian Rudert, and Andre F. Steinert. 2022. "PMMA Bone Cement: Antibiotic Elution and Mechanical Properties in the Context of Clinical Use" Biomedicines 10, no. 8: 1830. https://doi.org/10.3390/biomedicines10081830
APA Stylevon Hertzberg-Boelch, S. P., Luedemann, M., Rudert, M., & Steinert, A. F. (2022). PMMA Bone Cement: Antibiotic Elution and Mechanical Properties in the Context of Clinical Use. Biomedicines, 10(8), 1830. https://doi.org/10.3390/biomedicines10081830







