Pre- and Postnatal Vitamin D Status and Allergy Outcomes in Early Childhood
Abstract
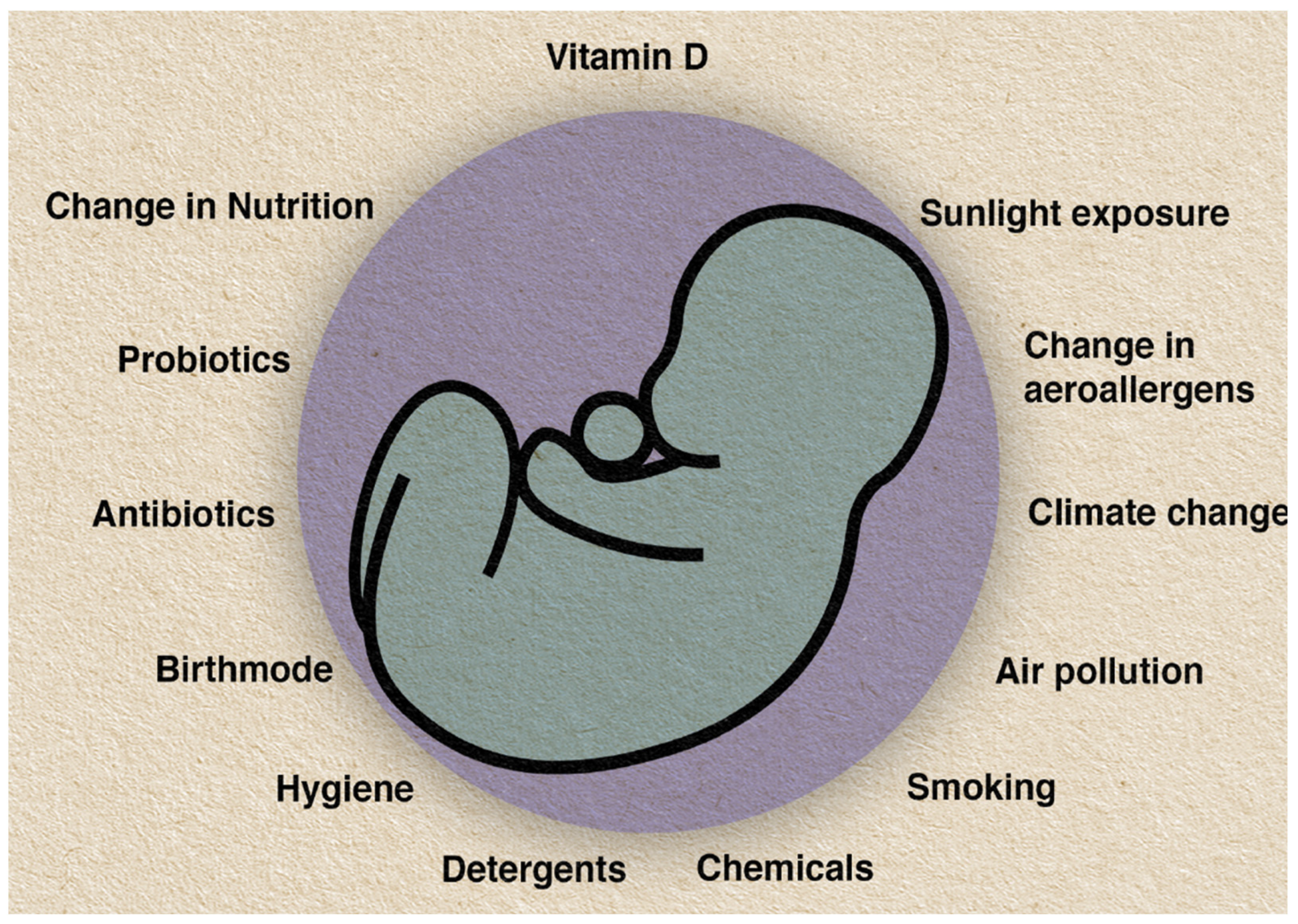
:1. Introduction
2. Environmental Factors as Causes for the Global Rise of Vitamin D Deficiency and Sources of Vitamin D
3. Vitamin D Metabolism and Physiology
4. Vitamin D Receptor and Vitamin D-Binding Protein Polymorphisms and Links to Allergic Diseases
5. Immunoregulatory Functions of Vitamin D and the Influence on Allergic Disease Development
5.1. The Role of Vitamin D in the Th1/Th2 Dichotomy
5.2. Immunomodulatory Function of Vitamin D on T Regulatory Cells and Allergic Disease Development
5.3. Antigen-Presenting Cells and Dendritic Cells
6. Studies of Geographical Variation and Allergy Outcome
7. In Utero Effects of Vitamin D Exposure and the Risk of Allergic Disease in Offspring
7.1. Observational Studies of Estimated Maternal Vitamin D Intake
7.2. Observational Studies of Maternal Vitamin D Status
7.3. Observational Studies of Cord Blood 25(OH)D Levels
7.4. Randomized Controlled Trials of Prenatal Vitamin D Supplementation
8. Vitamin D Intake and Status during Childhood and Allergy Outcomes
8.1. Observational Studies of Vitamin D Intake or Status in Relation to Allergy Outcomes
| Reference Study Location Latitude | Study Design | Study Population | Assay for 25(OH)D | Time Point When 25(OH)D Level Was Taken | Data Collection/ Outcome Variable | Main Results | Higher 25(OH) D Level |
|---|---|---|---|---|---|---|---|
| Sharief et al. (2011) USA 37.09 πN | National Health and Nutrition Examination Survey (NHANES) | n = 3136 (1 to 21 years) Non-Hispanic White 61.9% General population | CIA | Any stage between 1 and 21 years of age (mean age 12.5 years) | NHANES 2005/2006 questionnaire [189] sIgE levels for aeroallergens and foods | 25(OH)D levels of <37.5 nmol/L associated with peanut (OR 2.39; CI1.29–4.45), ragweed (OR 1.83; CI1.20–2.80) and oak (OR 4.75; CI 1.53–4.94) sensitization, (sIgE) (p < 0.01) 25(OH)D < 50 nmol/L and sIgE associated with dog, cockroach, Alternaria species, shrimp, ryegrass, Bermuda grass, birch, thistle (p < 0.05) No association with eczema and AR | S↓ E←→ AR←→ |
| Heimbeck et al. (2013) Germany 51.2 πN | Survey | n = 9838 (0 to 17 years) Residence in Germany (including 1411 migrants) General population | CIA | Any stage between 1 and 17 years of age (no mean age given) | Parental questionnaire: “Did a physician ever diagnose eczema?” | 25(OH)D level for eczema (n = 1364; mean = 50.6 nmol/L) higher than for control group (n = 8474; mean = 47.1 nmol/L) (p < 0.001) Inverse association between low 25 (OH)D levels and eczema (multivariant OR for 1st quartile vs. 2nd quartile): 0.76 (95% CI 0.61–0.94)) | E↑ |
| Wang et al. (2014) Hong Kong 22 πN | Case control study | n = 826 (0–18 years) Eczema: n = 498; No eczema: n = 328 (no eczema: general population) Chinese population Ethnicity not further specified | Enzyme Imuno-assay | Any stage between 0 and 18 years of age Mean age in eczema group 10.5 (SD 3.9) vs. no eczema 12.3 years (SD 4.1) | Medical assessment for eczema; Hanifin and Rajka criteria applied [161] Total IgE and sIgE for aeroallergens | Eczema cases (n = 498, mean age 10.5 years) more frequently 25(OH)D levels < 25 nmol/L than controls (n = 328, mean age 12.3 years) (mean 25(OH)D level (SD); 28.9 (15.3) vs. 34.2 nmol/L (14.5); p < 0.001) Total IgE and sensitization to aeroallergens (sIgE and SPT): not significant between groups | E↓ S←→ |
| Berents et al.(2016) Oslo, Norway 59.9 πN | Cross-sectional study | n = 623, <12 months of age n = 388 general population (mean age 6.5 months) n = 235 recruited from trial on acute bronchiolitis (mean age 4.3 months) 93% European ancestry | LC–MS/MS | Between 1 and 13 months (mean age 5.1 months) and at 24 months | Caregivers interviewed by a structured questionnaire: Hanifin and Rajka criteria applied [161] | Appointment at 1 to 13 months of age: (n = 67 eczema, n = 529 no eczema; mean age 5.1 months): 25(OH)D level (mean 58.2 nmol/L) no association with eczema At 2 year appointment (n = 103 eczema, n = 346 no eczema; mean age 24.7 months): 25(OH)D level (mean 66.9 nmol/L) no association with eczema | E←→ |
| Allen et al. (2013) Melbourne, Australia 37.81 πS | Cohort study | n = 577, 11 to 15 months General population 62.5% both parents born in Australia Ethnicity not provided | LC–MS/MS | 11 to 15 months | Challenge-proven food allergy at 14 to 18 months (n = 344), sensitized but tolerant (n = 74) SPT (wheal size >2 mm) or sIgE to egg, sesame, peanut, cow’s milk, shrimp | Infants of Australian-born parents only: if 25(OH)D ≤ 50 nmol/L at 12 months of age: More likely to have challenge-proven allergy to egg (aOR, 3.79; 95% CI, 1.19–12.08, p = 0.025) and peanut (aOR, 11.51; 95% CI, 2.01–65.79; p = 0.006) More likely to have multiple food allergies (>2) rather than a single food allergy (aOR, 10.48; 95% CI, 1.60–68.61 vs. aOR,1.82; 95% CI, 0.38–8.77, respectively) No parent-reported eczema | FA↓ E←→ |
| Molloy et al. (2017) Barwon, Australia 38.14 πS | Birth cohort study | 274 mother–infant pairs (mean age = 41 months (24; 60)) 75.2% European ancestry General population | LC–MS/MS | At birth and at 6 months | Challenge-proven food allergy at 1 year of age Questionnaire: Eczema UK working party criteria applied [198] | No association between 25(OH)D < 50 nmol/L at birth (n = 105; aRR 1.25, 95% CI 0.7–2.22) or at 6 months of age (n = 55; aRR 0.93, 95% CI 0.41–2.14) and food allergy at 1 year of age No association between 25(OH)D < 50 nmol/L at birth (n = 105; aRR 0.88, 95% CI 0.54–1.43) or at 6 months of age (n = 55; aRR 0.84, 95% CI 0.33–2.14) and eczema within first 12 months of age | FA←→ E←→ |
| Cairncross et al. (2016) New Zealand 35–46 πS | Cross-sectional study | n = 1329 (2 to 3 years, mean age 41 months) General population 70% European ancestry | LC–MS/MS | Any stage from 24 to 60 months | ISAAC questionnaire | Food allergy associated with higher mean 25(OH)D levels (56 vs. 52 nmol/L, p = 0.007) 25(OH)D ≥ 75 nmol/L compared to 50–74.9 nmol/L (n = 29): increased risk of parent-reported food allergy (OR = 2.21, 1.33–3.68, p = 0.002) No associations between eczema (mean 25 (OH)D level 53 vs. 52 nmol/L, p = 0.50) AR (52 vs. 52 nmol/L, p = 0.94) Asthma (52 vs. 52 nmol/L, p = 0.98) | FA↑ E←→ AR←→ A←→ |
| Bener et al. (2014} Doha, Qatar 25.28 πN | Cross-sectional study | n = 1833 (5 to 16 years) General population Population from Qatar Ethnicity not further specified | RIA | Any time from 5 to 16 years | Questionnaire: Parent-reported physician diagnosed | 25(OH)D < 50 nmol/L associated with risk for: wheezing (OR = 1.29; p = 0.05) asthma (OR = 2.31: p = 0.001) AR (OR1.59; p < 0.001) | W↓ A↓ AR↓ |
| Freishtat et al. (2010) Washington, USA 47.75 πN | Cross-sectional case control study | n = 113 African American Asthma n = 92 (6 to 20 years of age, mean age 11.1 (SE 0.4)) No asthma n = 21 (6 to 9 years, mean age 7 years (SE 0.3)) Controls younger than cases (p < 0.001) | Enzyme-linked immuno- absorbant assay | For cases: Any stage from 6 to 20 years For controls: Any stage from 6 to 9 years | Cases: Physician-diagnosed asthma Controls: General population | 25(OH)D < 75 nmol/L associated with more asthma cases than controls (73/85 vs. 4/21, aOR = 42 (95% CI: 4.4 to 399) 25(OH)D < 50 nmol/L associated with more asthma cases compared to controls (46/84 vs. 1/21, aOR = 20 (95% CI:1.4 to 272) | A↓ |
| Kutlug et al. (2017) Samsun, Turkey 41.27 πN | Case control study | n = 200, 6–18 years of age 100 cases with AR with seasonal symptoms for at least 2 years and positive SPT to pollen 100 controls General population | LC–MS/MS | For cases: median age 12.35 years (6; 17.8) For controls median age 11.5 years (6; 17.8) | AR diagnosis by “Allergic Rhinitis and its impact on asthma (ARIA) criteria 2008” | 25(OH)D level in AR group (mean 51.95, SD 16,2) significantly higher than in control group (mean 44.8, SD 16.2), (p = 0.002) | AR↑ |
| Baeck et al. (2014) Seongnam-Si, Korea 37.44 πN | Cross-sectional study | n = 226, age 3 to 24 months High-risk population n = 168 diagnosed with eczema n = 58 suspected food allergy, no eczema | CIA | Any time from 3 to 24 months | Physician diagnosed, parent-reported questionnaire sIgE to food (milk, egg, wheat, soy) | Polysensitization group significantly lower levels of 25(OH)D than the non-sensitization (p = 0.001) and monosensitization (p = 0.023) group 25(OH)D ≤ 50 nmol/L increased the risk of sensitization to food allergens (OR 5.0; 95% CI 1.8–14.1), milk (OR10.4; 95% CI 3.3–32.7) wheat (OR 4.2; 95% CI 1.1–15.8) | S↓ |
| Guo et al. (2020) Guangdong, China 23.38 πN | Cross-sectional study | n = 2642 (at 12 or 24 months of age) General population Chinese population, not further specified | CIA | At 12 months or 24 months of age | Total IgE Food and aeroallergen sensitization by sIgE | Positive association between 25(OH)D ≥ 75 nmol/L and sIgE to cow’s milk (<0.001), cat (p < 0.001), dog (p = 0.028) Inverse association between 25(OH)D < 75 nmol/L and sIgE to Der f (p = 0.012) No difference in total IgE | S milk↑ S cat↑ S dog↑ S Der.farinae↓ Total IgE←→ |
| Hollams et al. (2016) Perth, Australia 31.95 πS | Cross-sectional analysis | n = 263 High-risk population | LC–MS/MS | At birth and at 0.5, 1, 2, 3, 4, 5, 10 years of age | Up to 5 years symptom diary: Clinical phenotyping Total and sIgE levels | Inverse association between 25(OH)D levels and sensitization at age 0.5, 2 and 3 years. No association for all other age groups Number of 25(OH)D-deficient levels on follow ups positively associated with risk for asthma/wheeze, eczema and sensitization at 10 years of age | S↓ at 0.5, 2, 3 years S←→ at 1, 4, 5, 10 years Number of f/u: A/W↓ E↓ S↓ |
8.2. Randomized Controlled Trials of Vitamin D Supplementation in Infancy and Allergy Outcomes
9. Conclusions and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Christie, G.L.; Helms, P.J.; Godden, D.J.; Ross, S.J.; Friend, J.A.; Legge, J.S.; Haites, N.E.; Douglas, J.G. Asthma, wheezy bronchitis, and atopy across two generations. Am. J. Respir. Crit. Care Med. 1999, 159, 125–129. [Google Scholar] [CrossRef]
- Pearce, N.; Ait-Khaled, N.; Beasley, R.; Mallol, J.; Keil, U.; Mitchell, E.; Robertson, C.; Group, I.P.T.S. Worldwide trends in the prevalence of asthma symptoms: Phase III of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax 2007, 62, 758–766. [Google Scholar] [CrossRef] [Green Version]
- Koet, L.B.M.; Brand, P.L.P. Increase in atopic sensitization rate among Dutch children with symptoms of allergic disease between 1994 and 2014. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2018, 29, 78–83. [Google Scholar] [CrossRef] [Green Version]
- Rappaport, S.M. Genetic Factors Are Not the Major Causes of Chronic Diseases. PLoS ONE 2016, 11, e0154387. [Google Scholar] [CrossRef]
- von Hertzen, L.; Beutler, B.; Bienenstock, J.; Blaser, M.; Cani, P.D.; Eriksson, J.; Farkkila, M.; Haahtela, T.; Hanski, I.; Jenmalm, M.C.; et al. Helsinki alert of biodiversity and health. Ann. Med. 2015, 47, 218–225. [Google Scholar] [CrossRef] [Green Version]
- D’Amato, G.; Akdis, C.A. Global warming, climate change, air pollution and allergies. Allergy 2020, 75, 2158–2160. [Google Scholar] [CrossRef]
- D’Amato, G.; Chong-Neto, H.J.; Monge Ortega, O.P.; Vitale, C.; Ansotegui, I.; Rosario, N.; Haathela, T.; Galan, C.; Pawankar, R.; Murrieta, M.; et al. The effects of climate change on respiratory allergy and asthma induced by pollen and mold allergens. Allergy 2020, 75, 2219–2228. [Google Scholar] [CrossRef]
- McFadden, J.P.; Thyssen, J.P.; Basketter, D.A.; Puangpet, P.; Kimber, I. T helper cell 2 immune skewing in pregnancy/early life: Chemical exposure and the development of atopic disease and allergy. Br. J. Dermatol. 2015, 172, 584–591. [Google Scholar] [CrossRef]
- Prescott, S.L. Early-life environmental determinants of allergic diseases and the wider pandemic of inflammatory noncommunicable diseases. J. Allergy Clin. Immunol. 2013, 131, 23–30. [Google Scholar] [CrossRef]
- Hanson, M.; Gluckman, P. Developmental origins of noncommunicable disease: Population and public health implications. Am. J. Clin. Nutr. 2011, 94, 1754S–1758S. [Google Scholar] [CrossRef] [Green Version]
- Hanson, M.A.; Gluckman, P.D. Developmental origins of health and disease: Moving from biological concepts to interventions and policy. Int. J. Gynaecol. Obstet. 2011, 115, S3–S5. [Google Scholar] [CrossRef]
- Holick, M.F. Vitamin D deficiency. N. Engl. J. Med. 2007, 357, 266–281. [Google Scholar] [CrossRef]
- Holick, M.F. Biological Effects of Sunlight, Ultraviolet Radiation, Visible Light, Infrared Radiation and Vitamin D for Health. Anticancer. Res. 2016, 36, 1345–1356. [Google Scholar]
- Wacker, M.; Holick, M.F. Sunlight and Vitamin D: A global perspective for health. Derm. Endocrinol. 2013, 5, 51–108. [Google Scholar] [CrossRef] [Green Version]
- Holick, M.F.; Chen, T.C.; Lu, Z.; Sauter, E. Vitamin D and skin physiology: A D-lightful story. J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 2007, 22, V28–V33. [Google Scholar] [CrossRef]
- Faurschou, A.; Beyer, D.M.; Schmedes, A.; Bogh, M.K.; Philipsen, P.A.; Wulf, H.C. The relation between sunscreen layer thickness and vitamin D production after ultraviolet B exposure: A randomized clinical trial. Br. J. Dermatol. 2012, 167, 391–395. [Google Scholar] [CrossRef]
- Wortsman, J.; Matsuoka, L.Y.; Chen, T.C.; Lu, Z.; Holick, M.F. Decreased bioavailability of vitamin D in obesity. Am. J. Clin. Nutr. 2000, 72, 690–693. [Google Scholar] [CrossRef]
- Matsuoka, L.Y.; Ide, L.; Wortsman, J.; MacLaughlin, J.A.; Holick, M.F. Sunscreens suppress cutaneous vitamin D3 synthesis. J. Clin. Endocrinol. Metab. 1987, 64, 1165–1168. [Google Scholar] [CrossRef] [Green Version]
- Holick, M.F. The vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention. Rev. Endocr. Metab. Disord. 2017, 18, 153–165. [Google Scholar] [CrossRef]
- Hintzpeter, B.; Scheidt-Nave, C.; Muller, M.J.; Schenk, L.; Mensink, G.B. Higher prevalence of vitamin D deficiency is associated with immigrant background among children and adolescents in Germany. J. Nutr. 2008, 138, 1482–1490. [Google Scholar] [CrossRef] [Green Version]
- Clemens, T.L.; Adams, J.S.; Henderson, S.L.; Holick, M.F. Increased skin pigment reduces the capacity of skin to synthesise vitamin D3. Lancet 1982, 1, 74–76. [Google Scholar] [CrossRef]
- Piotrowska, A.; Wierzbicka, J.; Zmijewski, M.A. Vitamin D in the skin physiology and pathology. Acta Biochim. Pol. 2016, 63, 17–29. [Google Scholar] [CrossRef] [Green Version]
- Holick, M.F. Vitamin D: A D-Lightful health perspective. Nutr. Rev. 2008, 66, S182–S194. [Google Scholar] [CrossRef]
- Holick, M.F.; Chen, T.C. Vitamin D deficiency: A worldwide problem with health consequences. Am. J. Clin. Nutr. 2008, 87, 1080S–1086S. [Google Scholar] [CrossRef] [Green Version]
- Chun, R.F.; Peercy, B.E.; Orwoll, E.S.; Nielson, C.M.; Adams, J.S.; Hewison, M. Vitamin D and DBP: The free hormone hypothesis revisited. J. Steroid Biochem. Mol. Biol. 2014, 144, 132–137. [Google Scholar] [CrossRef] [Green Version]
- Christakos, S.; Ajibade, D.V.; Dhawan, P.; Fechner, A.J.; Mady, L.J. Vitamin D: Metabolism. Endocrinol. Metab. Clin. N. Am. 2010, 39, 243–253. [Google Scholar] [CrossRef]
- DeLuca, H.F. Vitamin D: Historical Overview. Vitam. Horm. 2016, 100, 1–20. [Google Scholar] [CrossRef]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M.; Endocrine, S. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef] [Green Version]
- Chun, R.F.; Liu, P.T.; Modlin, R.L.; Adams, J.S.; Hewison, M. Impact of vitamin D on immune function: Lessons learned from genome-wide analysis. Front. Physiol. 2014, 5, 151. [Google Scholar] [CrossRef] [Green Version]
- Cantorna, M.T. Mechanisms underlying the effect of vitamin D on the immune system. Proc. Nutr. Soc. 2010, 69, 286–289. [Google Scholar] [CrossRef] [Green Version]
- Brennan, A.; Katz, D.R.; Nunn, J.D.; Barker, S.; Hewison, M.; Fraher, L.J.; O’Riordan, J.L. Dendritic cells from human tissues express receptors for the immunoregulatory vitamin D3 metabolite, dihydroxycholecalciferol. Immunology 1987, 61, 457–461. [Google Scholar]
- Morgan, J.W.; Kouttab, N.; Ford, D.; Maizel, A.L. Vitamin D-mediated gene regulation in phenotypically defined human B cell subpopulations. Endocrinology 2000, 141, 3225–3234. [Google Scholar] [CrossRef]
- Provvedini, D.M.; Tsoukas, C.D.; Deftos, L.J.; Manolagas, S.C. 1,25-dihydroxyvitamin D3 receptors in human leukocytes. Science 1983, 221, 1181–1183. [Google Scholar] [CrossRef]
- Umar, M.; Sastry, K.S.; Al Ali, F.; Al-Khulaifi, M.; Wang, E.; Chouchane, A.I. Vitamin D and the Pathophysiology of Inflammatory Skin Diseases. Ski. Pharmacol. Physiol. 2018, 31, 74–86. [Google Scholar] [CrossRef]
- Duplancic, D.; Cesarik, M.; Poljak, N.K.; Radman, M.; Kovacic, V.; Radic, J.; Rogosic, V. The influence of selective vitamin D receptor activator paricalcitol on cardiovascular system and cardiorenal protection. Clin. Interv. Aging 2013, 8, 149–156. [Google Scholar] [CrossRef] [Green Version]
- Egshatyan, L.V.; Dudinskaya, E.N.; Tkacheva, O.N.; Kashtanova, D.A. The role of vitamin D in the pathogenesis of chronic non-communicable diseases. Osteoporoz I Osteopat. 2014, 17, 27–30. [Google Scholar] [CrossRef] [Green Version]
- Bikle, D.D. Vitamin D and the skin: Physiology and pathophysiology. Rev. Endocr. Metab. Disord. 2012, 13, 3–19. [Google Scholar] [CrossRef] [Green Version]
- Poon, A.H.; Laprise, C.; Lemire, M.; Montpetit, A.; Sinnett, D.; Schurr, E.; Hudson, T.J. Association of vitamin D receptor genetic variants with susceptibility to asthma and atopy. Am. J. Respir. Crit. Care Med. 2004, 170, 967–973. [Google Scholar] [CrossRef] [Green Version]
- Valdivielso, J.M.; Fernandez, E. Vitamin D receptor polymorphisms and diseases. Clin. Chim. Acta Int. J. Clin. Chem. 2006, 371, 1–12. [Google Scholar] [CrossRef]
- Tizaoui, K.; Berraies, A.; Hamdi, B.; Kaabachi, W.; Hamzaoui, K.; Hamzaoui, A. Association of vitamin D receptor gene polymorphisms with asthma risk: Systematic review and updated meta-analysis of case-control studies. Lung 2014, 192, 955–965. [Google Scholar] [CrossRef]
- Wjst, M. Variants in the vitamin D receptor gene and asthma. BMC Genet. 2005, 6, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vollmert, C.; Illig, T.; Altmuller, J.; Klugbauer, S.; Loesgen, S.; Dumitrescu, L.; Wjst, M. Single nucleotide polymorphism screening and association analysis--exclusion of integrin beta 7 and vitamin D receptor (chromosome 12q) as candidate genes for asthma. Clin. Exp. Allergy J. Br. Soc. Allergy Clin. Immunol. 2004, 34, 1841–1850. [Google Scholar] [CrossRef] [PubMed]
- Tamasauskiene, L.; Golubickaite, I.; Ugenskiene, R.; Sjakste, N.; Paramonova, N.; Wu, L.S.; Wang, L.S.; Sitkauskiene, B. Vitamin D receptor gene polymorphisms in atopy. Immun. Inflamm. Dis. 2021, 9, 1153–1159. [Google Scholar] [CrossRef] [PubMed]
- Pillai, D.K.; Iqbal, S.F.; Benton, A.S.; Lerner, J.; Wiles, A.; Foerster, M.; Ozedirne, T.; Holbrook, H.P.; Payne, P.W., Jr.; Gordish-Dressman, H.; et al. Associations between genetic variants in vitamin D metabolism and asthma characteristics in young African Americans: A pilot study. J. Investig. Med. 2011, 59, 938–946. [Google Scholar] [CrossRef] [PubMed]
- Wjst, M. The vitamin D slant on allergy. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2006, 17, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Chun, R.F.; Peercy, B.E.; Adams, J.S.; Hewison, M. Vitamin D binding protein and monocyte response to 25-hydroxyvitamin D and 1, 25-dihydroxyvitamin D: Analysis by mathematical modeling. PLoS ONE 2012, 7, e30773. [Google Scholar] [CrossRef] [Green Version]
- Malik, S.; Fu, L.; Juras, D.J.; Karmali, M.; Wong, B.Y.; Gozdzik, A.; Cole, D.E. Common variants of the vitamin D binding protein gene and adverse health outcomes. Crit. Rev. Clin. Lab. Sci. 2013, 50, 1–22. [Google Scholar] [CrossRef] [Green Version]
- Carpenter, T.O.; Zhang, J.H.; Parra, E.; Ellis, B.K.; Simpson, C.; Lee, W.M.; Balko, J.; Fu, L.; Wong, B.Y.; Cole, D.E. Vitamin D binding protein is a key determinant of 25-hydroxyvitamin D levels in infants and toddlers. J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 2013, 28, 213–221. [Google Scholar] [CrossRef]
- Navas-Nazario, A.; Li, F.Y.; Shabanova, V.; Weiss, P.; Cole, D.E.; Carpenter, T.O.; Bazzy-Asaad, A. Effect of vitamin D-binding protein genotype on the development of asthma in children. Ann. Allergy Asthma Immunol. Off. Publ. Am. Coll. Allergy Asthma Immunol. 2014, 112, 519–524. [Google Scholar] [CrossRef] [Green Version]
- Tsoukas, C.D.; Provvedini, D.M.; Manolagas, S.C. 1,25-dihydroxyvitamin D3: A novel immunoregulatory hormone. Science 1984, 224, 1438–1440. [Google Scholar] [CrossRef]
- Lemire, J.M.; Adams, J.S.; Kermani-Arab, V.; Bakke, A.C.; Sakai, R.; Jordan, S.C. 1,25-Dihydroxyvitamin D3 suppresses human T helper/inducer lymphocyte activity in vitro. J. Immunol. 1985, 134, 3032–3035. [Google Scholar] [PubMed]
- Lemire, J.M.; Archer, D.C.; Beck, L.; Spiegelberg, H.L. Immunosuppressive actions of 1,25-dihydroxyvitamin D3: Preferential inhibition of Th1 functions. J. Nutr. 1995, 125, 1704S–1708S. [Google Scholar] [CrossRef] [PubMed]
- Jirapongsananuruk, O.; Melamed, I.; Leung, D.Y. Additive immunosuppressive effects of 1,25-dihydroxyvitamin D3 and corticosteroids on TH1, but not TH2, responses. J. Allergy Clin. Immunol. 2000, 106, 981–985. [Google Scholar] [CrossRef] [PubMed]
- Rausch-Fan, X.; Leutmezer, F.; Willheim, M.; Spittler, A.; Bohle, B.; Ebner, C.; Jensen-Jarolim, E.; Boltz-Nitulescu, G. Regulation of cytokine production in human peripheral blood mononuclear cells and allergen-specific th cell clones by 1alpha,25-dihydroxyvitamin D3. Int. Arch. Allergy Immunol. 2002, 128, 33–41. [Google Scholar] [CrossRef]
- Pichler, J.; Gerstmayr, M.; Szepfalusi, Z.; Urbanek, R.; Peterlik, M.; Willheim, M. 1 alpha,25(OH)2D3 inhibits not only Th1 but also Th2 differentiation in human cord blood T cells. Pediatr. Res. 2002, 52, 12–18. [Google Scholar] [CrossRef] [Green Version]
- Fisher, S.A.; Rahimzadeh, M.; Brierley, C.; Gration, B.; Doree, C.; Kimber, C.E.; Plaza Cajide, A.; Lamikanra, A.A.; Roberts, D.J. The role of vitamin D in increasing circulating T regulatory cell numbers and modulating T regulatory cell phenotypes in patients with inflammatory disease or in healthy volunteers: A systematic review. PLoS ONE 2019, 14, e0222313. [Google Scholar] [CrossRef] [Green Version]
- Lio, C.W.; Hsieh, C.S. Becoming self-aware: The thymic education of regulatory T cells. Curr. Opin. Immunol. 2011, 23, 213–219. [Google Scholar] [CrossRef] [Green Version]
- Mucida, D.; Kutchukhidze, N.; Erazo, A.; Russo, M.; Lafaille, J.J.; Curotto de Lafaille, M.A. Oral tolerance in the absence of naturally occurring Tregs. J. Clin. Investig. 2005, 115, 1923–1933. [Google Scholar] [CrossRef] [Green Version]
- Kretschmer, K.; Apostolou, I.; Hawiger, D.; Khazaie, K.; Nussenzweig, M.C.; von Boehmer, H. Inducing and expanding regulatory T cell populations by foreign antigen. Nat. Immunol. 2005, 6, 1219–1227. [Google Scholar] [CrossRef]
- Curotto de Lafaille, M.A.; Kutchukhidze, N.; Shen, S.; Ding, Y.; Yee, H.; Lafaille, J.J. Adaptive Foxp3+ regulatory T cell-dependent and -independent control of allergic inflammation. Immunity 2008, 29, 114–126. [Google Scholar] [CrossRef] [Green Version]
- Noval Rivas, M.; Chatila, T.A. Regulatory T cells in allergic diseases. J. Allergy Clin. Immunol. 2016, 138, 639–652. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noval Rivas, M.; Burton, O.T.; Wise, P.; Charbonnier, L.M.; Georgiev, P.; Oettgen, H.C.; Rachid, R.; Chatila, T.A. Regulatory T cell reprogramming toward a Th2-cell-like lineage impairs oral tolerance and promotes food allergy. Immunity 2015, 42, 512–523. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Syed, A.; Garcia, M.A.; Lyu, S.C.; Bucayu, R.; Kohli, A.; Ishida, S.; Berglund, J.P.; Tsai, M.; Maecker, H.; O’Riordan, G.; et al. Peanut oral immunotherapy results in increased antigen-induced regulatory T-cell function and hypomethylation of forkhead box protein 3 (FOXP3). J. Allergy Clin. Immunol. 2014, 133, 500–510. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shreffler, W.G.; Wanich, N.; Moloney, M.; Nowak-Wegrzyn, A.; Sampson, H.A. Association of allergen-specific regulatory T cells with the onset of clinical tolerance to milk protein. J. Allergy Clin. Immunol. 2009, 123, 43–52.e7. [Google Scholar] [CrossRef]
- Lloyd, C.M.; Hawrylowicz, C.M. Regulatory T cells in asthma. Immunity 2009, 31, 438–449. [Google Scholar] [CrossRef] [Green Version]
- Dimeloe, S.; Nanzer, A.; Ryanna, K.; Hawrylowicz, C. Regulatory T cells, inflammation and the allergic response—The role of glucocorticoids and Vitamin D. J. Steroid Biochem. Mol. Biol. 2010, 120, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, B.; Riedel, R.; Jorss, K.; Loddenkemper, C.; Steinmeyer, A.; Zugel, U.; Babina, M.; Radbruch, A.; Worm, M. Vitamin D receptor activation improves allergen-triggered eczema in mice. J. Investig. Dermatol. 2012, 132, 330–336. [Google Scholar] [CrossRef] [Green Version]
- Gorman, S.; Judge, M.A.; Hart, P.H. Topical 1,25-dihydroxyvitamin D3 subverts the priming ability of draining lymph node dendritic cells. Immunology 2010, 131, 415–425. [Google Scholar] [CrossRef]
- Joshi, S.; Pantalena, L.C.; Liu, X.K.; Gaffen, S.L.; Liu, H.; Rohowsky-Kochan, C.; Ichiyama, K.; Yoshimura, A.; Steinman, L.; Christakos, S.; et al. 1,25-dihydroxyvitamin D3 ameliorates Th17 autoimmunity via transcriptional modulation of interleukin-17A. Mol. Cell. Biol. 2011, 31, 3653–3669. [Google Scholar] [CrossRef] [Green Version]
- Jeffery, L.E.; Burke, F.; Mura, M.; Zheng, Y.; Qureshi, O.S.; Hewison, M.; Walker, L.S.; Lammas, D.A.; Raza, K.; Sansom, D.M. 1,25-Dihydroxyvitamin D3 and IL-2 combine to inhibit T cell production of inflammatory cytokines and promote development of regulatory T cells expressing CTLA-4 and FoxP3. J. Immunol. 2009, 183, 5458–5467. [Google Scholar] [CrossRef] [Green Version]
- Christakos, S.; Dhawan, P.; Verstuyf, A.; Verlinden, L.; Carmeliet, G. Vitamin D: Metabolism, Molecular Mechanism of Action, and Pleiotropic Effects. Physiol. Rev. 2016, 96, 365–408. [Google Scholar] [CrossRef] [PubMed]
- van Halteren, A.G.; Tysma, O.M.; van Etten, E.; Mathieu, C.; Roep, B.O. 1alpha,25-dihydroxyvitamin D3 or analogue treated dendritic cells modulate human autoreactive T cells via the selective induction of apoptosis. J. Autoimmun. 2004, 23, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Van Belle, T.L.; Vanherwegen, A.S.; Feyaerts, D.; De Clercq, P.; Verstuyf, A.; Korf, H.; Gysemans, C.; Mathieu, C. 1,25-Dihydroxyvitamin D3 and its analog TX527 promote a stable regulatory T cell phenotype in T cells from type 1 diabetes patients. PLoS ONE 2014, 9, e109194. [Google Scholar] [CrossRef] [PubMed]
- Gorman, S.; Geldenhuys, S.; Weeden, C.E.; Grimbaldeston, M.A.; Hart, P.H. Investigating the roles of regulatory T cells, mast cells and interleukin-9 in the control of skin inflammation by vitamin D. Arch. Dermatol. Res. 2018, 310, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Khoo, A.L.; Koenen, H.J.; Chai, L.Y.; Sweep, F.C.; Netea, M.G.; van der Ven, A.J.; Joosten, I. Seasonal variation in vitamin D3 levels is paralleled by changes in the peripheral blood human T cell compartment. PLoS ONE 2012, 7, e29250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prietl, B.; Treiber, G.; Mader, J.K.; Hoeller, E.; Wolf, M.; Pilz, S.; Graninger, W.B.; Obermayer-Pietsch, B.M.; Pieber, T.R. High-dose cholecalciferol supplementation significantly increases peripheral CD4(+) Tregs in healthy adults without negatively affecting the frequency of other immune cells. Eur. J. Nutr. 2014, 53, 751–759. [Google Scholar] [CrossRef]
- Maalmi, H.; Sassi, F.H.; Berraies, A.; Ammar, J.; Hamzaoui, K.; Hamzaoui, A. Association of vitamin D receptor gene polymorphisms with susceptibility to asthma in Tunisian children: A case control study. Hum. Immunol. 2013, 74, 234–240. [Google Scholar] [CrossRef]
- Treiber, G.; Prietl, B.; Frohlich-Reiterer, E.; Lechner, E.; Ribitsch, A.; Fritsch, M.; Rami-Merhar, B.; Steigleder-Schweiger, C.; Graninger, W.; Borkenstein, M.; et al. Cholecalciferol supplementation improves suppressive capacity of regulatory T-cells in young patients with new-onset type 1 diabetes mellitus—A randomized clinical trial. Clin. Immunol. 2015, 161, 217–224. [Google Scholar] [CrossRef]
- Piantoni, S.; Andreoli, L.; Scarsi, M.; Zanola, A.; Dall’Ara, F.; Pizzorni, C.; Cutolo, M.; Airo, P.; Tincani, A. Phenotype modifications of T-cells and their shift toward a Th2 response in patients with systemic lupus erythematosus supplemented with different monthly regimens of vitamin D. Lupus 2015, 24, 490–498. [Google Scholar] [CrossRef]
- Gutcher, I.; Becher, B. APC-derived cytokines and T cell polarization in autoimmune inflammation. J. Clin. Investig. 2007, 117, 1119–1127. [Google Scholar] [CrossRef] [Green Version]
- Upham, J.W.; Zhang, G.; Rate, A.; Yerkovich, S.T.; Kusel, M.; Sly, P.D.; Holt, P.G. Plasmacytoid dendritic cells during infancy are inversely associated with childhood respiratory tract infections and wheezing. J. Allergy Clin. Immunol. 2009, 124, 707–713.e2. [Google Scholar] [CrossRef] [PubMed]
- Silver, E.; Yin-DeClue, H.; Schechtman, K.B.; Grayson, M.H.; Bacharier, L.B.; Castro, M. Lower levels of plasmacytoid dendritic cells in peripheral blood are associated with a diagnosis of asthma 6 yr after severe respiratory syncytial virus bronchiolitis. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2009, 20, 471–476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hewison, M.; Freeman, L.; Hughes, S.V.; Evans, K.N.; Bland, R.; Eliopoulos, A.G.; Kilby, M.D.; Moss, P.A.; Chakraverty, R. Differential regulation of vitamin D receptor and its ligand in human monocyte-derived dendritic cells. J. Immunol. 2003, 170, 5382–5390. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koeffler, H.P.; Reichel, H.; Bishop, J.E.; Norman, A.W. gamma-Interferon stimulates production of 1,25-dihydroxyvitamin D3 by normal human macrophages. Biochem. Biophys. Res. Commun. 1985, 127, 596–603. [Google Scholar] [CrossRef]
- Bscheider, M.; Butcher, E.C. Vitamin D immunoregulation through dendritic cells. Immunology 2016, 148, 227–236. [Google Scholar] [CrossRef]
- Colotta, F.; Jansson, B.; Bonelli, F. Modulation of inflammatory and immune responses by vitamin D. J. Autoimmun. 2017, 85, 78–97. [Google Scholar] [CrossRef]
- Weiland, S.K.; Husing, A.; Strachan, D.P.; Rzehak, P.; Pearce, N.; ISAAC Phase One Study Group. Climate and the prevalence of symptoms of asthma, allergic rhinitis, and atopic eczema in children. Occup. Environ. Med. 2004, 61, 609–615. [Google Scholar] [CrossRef]
- Krstic, G. Asthma prevalence associated with geographical latitude and regional insolation in the United States of America and Australia. PLoS ONE 2011, 6, e18492. [Google Scholar] [CrossRef] [Green Version]
- Hoyos-Bachiloglu, R.; Morales, P.S.; Cerda, J.; Talesnik, E.; Gonzalez, G.; Camargo, C.A., Jr.; Borzutzky, A. Higher latitude and lower solar radiation influence on anaphylaxis in Chilean children. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2014, 25, 338–343. [Google Scholar] [CrossRef] [Green Version]
- Camargo, J.C.A.; Clark, S.; Kaplan, M.S.; Lieberman, P.; Wood, R.A. Regional differences in EpiPen prescriptions in the United States: The potential role of vitamin D. J. Allergy Clin. Immunol. 2007, 120, 131–136. [Google Scholar] [CrossRef]
- Fioletov, V.E.; McArthur, L.J.; Mathews, T.W.; Marrett, L. Estimated ultraviolet exposure levels for a sufficient vitamin D status in North America. J. Photochem. Photobiol. B Biol. 2010, 100, 57–66. [Google Scholar] [CrossRef]
- Mullins, R.J.; Clark, S.; Camargo, C.A., Jr. Regional variation in epinephrine autoinjector prescriptions in Australia: More evidence for the vitamin D-anaphylaxis hypothesis. Ann. Allergy Asthma Immunol. Off. Publ. Am. Coll. Allergy Asthma Immunol. 2009, 103, 488–495. [Google Scholar] [CrossRef]
- Rueter, K.; Ta, B.; Bear, N.; Lucas, M.; Borland, M.L.; Prescott, S.L. Increased Use of Adrenaline in the Management of Childhood Anaphylaxis Over the Last Decade. J. Allergy Clin. Immunol. Pract. 2018, 6, 1545–1552. [Google Scholar] [CrossRef]
- Sheehan, W.J.; Graham, D.; Ma, L.; Baxi, S.; Phipatanakul, W. Higher incidence of pediatric anaphylaxis in northern areas of the United States. J. Allergy Clin. Immunol. 2009, 124, 180–182. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.H.; Ban, G.Y.; Park, H.S.; Kim, S.C.; Ye, Y.M. Regional differences in vitamin D levels and incidence of food-induced anaphylaxis in South Korea. Ann. Allergy Asthma Immunol. Off. Publ. Am. Coll. Allergy Asthma Immunol. 2016, 116, 237–243. [Google Scholar] [CrossRef]
- Osborne, N.J.; Ukoumunne, O.C.; Wake, M.; Allen, K.J. Prevalence of eczema and food allergy is associated with latitude in Australia. J. Allergy Clin. Immunol. 2012, 129, 865–867. [Google Scholar] [CrossRef]
- Franco, J.M.G.R.; Sole, D.; Lucia Franca, V.; Brabin, B.; Brazilian, I.G. Socio-environmental conditions and geographical variability of asthma prevalence in northeast Brazil. Allergol. Immunopathol. 2009, 37, 116–121. [Google Scholar] [CrossRef]
- Hamilton, S.A.; McNeil, R.; Hollis, B.W.; Davis, D.J.; Winkler, J.; Cook, C.; Warner, G.; Bivens, B.; McShane, P.; Wagner, C.L. Profound Vitamin D Deficiency in a Diverse Group of Women during Pregnancy Living in a Sun-Rich Environment at Latitude 32 degrees N. Int. J. Endocrinol. 2010, 2010, 917428. [Google Scholar] [CrossRef] [Green Version]
- Kimlin, M.; Harrison, S.; Nowak, M.; Moore, M.; Brodie, A.; Lang, C. Does a high UV environment ensure adequate vitamin D status? J. Photochem. Photobiol. B Biol. 2007, 89, 139–147. [Google Scholar] [CrossRef]
- Chakhtoura, M.; Rahme, M.; Chamoun, N.; El-Hajj Fuleihan, G. Vitamin D in the Middle East and North Africa. Bone Rep. 2018, 8, 135–146. [Google Scholar] [CrossRef]
- Miyake, Y.; Tanaka, K.; Okubo, H.; Sasaki, S.; Arakawa, M. Maternal consumption of dairy products, calcium, and vitamin D during pregnancy and infantile allergic disorders. Ann. Allergy Asthma Immunol. Off. Publ. Am. Coll. Allergy Asthma Immunol. 2014, 113, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Camargo, C.A., Jr.; Rifas-Shiman, S.L.; Litonjua, A.A.; Rich-Edwards, J.W.; Weiss, S.T.; Gold, D.R.; Kleinman, K.; Gillman, M.W. Maternal intake of vitamin D during pregnancy and risk of recurrent wheeze in children at 3 y of age. Am. J. Clin. Nutr. 2007, 85, 788–795. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Erkkola, M.; Kaila, M.; Nwaru, B.I.; Kronberg-Kippila, C.; Ahonen, S.; Nevalainen, J.; Veijola, R.; Pekkanen, J.; Ilonen, J.; Simell, O.; et al. Maternal vitamin D intake during pregnancy is inversely associated with asthma and allergic rhinitis in 5-year-old children. Clin. Exp. Allergy J. Br. Soc. Allergy Clin. Immunol. 2009, 39, 875–882. [Google Scholar] [CrossRef] [PubMed]
- Miyake, Y.; Sasaki, S.; Tanaka, K.; Hirota, Y. Dairy food, calcium and vitamin D intake in pregnancy, and wheeze and eczema in infants. Eur. Respir. J. 2010, 35, 1228–1234. [Google Scholar] [CrossRef] [Green Version]
- Maslova, E.; Hansen, S.; Jensen, C.B.; Thorne-Lyman, A.L.; Strom, M.; Olsen, S.F. Vitamin D intake in mid-pregnancy and child allergic disease—A prospective study in 44,825 Danish mother-child pairs. BMC Pregnancy Childbirth 2013, 13, 199. [Google Scholar] [CrossRef] [Green Version]
- Devereux, G.; Litonjua, A.A.; Turner, S.W.; Craig, L.C.; McNeill, G.; Martindale, S.; Helms, P.J.; Seaton, A.; Weiss, S.T. Maternal vitamin D intake during pregnancy and early childhood wheezing. Am. J. Clin. Nutr. 2007, 85, 853–859. [Google Scholar] [CrossRef] [Green Version]
- Anderson, L.N.; Chen, Y.; Omand, J.A.; Birken, C.S.; Parkin, P.C.; To, T.; Maguire, J.L.; Collaboration, T.A.K. Vitamin D exposure during pregnancy, but not early childhood, is associated with risk of childhood wheezing. J. Dev. Orig. Health Dis. 2015, 6, 308–316. [Google Scholar] [CrossRef] [Green Version]
- Rueter, K.; Siafarikas, A.; Prescott, S.L.; Palmer, D.J. In utero and postnatal vitamin D exposure and allergy risk. Expert Opin. Drug Saf. 2014, 13, 1601–1611. [Google Scholar] [CrossRef]
- Pike, K.C.; Inskip, H.M.; Robinson, S.; Lucas, J.S.; Cooper, C.; Harvey, N.C.; Godfrey, K.M.; Roberts, G.; Southampton Women’s Survey Study, G. Maternal late-pregnancy serum 25-hydroxyvitamin D in relation to childhood wheeze and atopic outcomes. Thorax 2012, 67, 950–956. [Google Scholar] [CrossRef] [Green Version]
- Allan, K.M.; Prabhu, N.; Craig, L.C.; McNeill, G.; Kirby, B.; McLay, J.; Helms, P.J.; Ayres, J.G.; Seaton, A.; Turner, S.W.; et al. Maternal vitamin D and E intakes during pregnancy are associated with asthma in children. Eur. Respir. J. 2015, 45, 1027–1036. [Google Scholar] [CrossRef] [Green Version]
- Devereux, G.; Craig, L.; Seaton, A.; Turner, S. Maternal vitamin D and E intakes in pregnancy and asthma to age 15 years: A cohort study. Pediatr. Pulmonol. 2019, 54, 11–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shen, S.Y.; Xiao, W.Q.; Lu, J.H.; Yuan, M.Y.; He, J.R.; Xia, H.M.; Qiu, X.; Cheng, K.K.; Lam, K.B.H. Early life vitamin D status and asthma and wheeze: A systematic review and meta-analysis. BMC Pulm. Med. 2018, 18, 120. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.M.; Smith, J.R.; Philipp, B.L.; Chen, T.C.; Mathieu, J.; Holick, M.F. Vitamin D deficiency in a healthy group of mothers and newborn infants. Clin. Pediatr. 2007, 46, 42–44. [Google Scholar] [CrossRef] [PubMed]
- Wills, A.K.; Shaheen, S.O.; Granell, R.; Henderson, A.J.; Fraser, W.D.; Lawlor, D.A. Maternal 25-hydroxyvitamin D and its association with childhood atopic outcomes and lung function. Clin. Exp. Allergy J. Br. Soc. Allergy Clin. Immunol. 2013, 43, 1180–1188. [Google Scholar] [CrossRef] [Green Version]
- Wegienka, G.; Havstad, S.; Zoratti, E.M.; Kim, H.; Ownby, D.R.; Johnson, C.C. Association between vitamin D levels and allergy-related outcomes vary by race and other factors. J. Allergy Clin. Immunol. 2015, 136, 1309–1314.e4. [Google Scholar] [CrossRef] [Green Version]
- Blomberg, M.; Rifas-Shiman, S.L.; Camargo, C.A., Jr.; Gold, D.R.; Asgari, M.M.; Thyssen, J.P.; Litonjua, A.A.; Gillman, M.W.; Oken, E. Low Maternal Prenatal 25-Hydroxyvitamin D Blood Levels Are Associated with Childhood Atopic Dermatitis. J. Investig. Dermatol. 2017, 137, 1380–1384. [Google Scholar] [CrossRef] [Green Version]
- Hennessy, A.; Hourihane, J.O.; Malvisi, L.; Irvine, A.D.; Kenny, L.C.; Murray, D.M.; Kiely, M.E. Antenatal vitamin D exposure and childhood eczema, food allergy, asthma and allergic rhinitis at 2 and 5 years of age in the atopic disease-specific Cork BASELINE Birth Cohort Study. Allergy 2018, 73, 2182–2191. [Google Scholar] [CrossRef]
- Gazibara, T.; Elbert, N.J.; den Dekker, H.T.; de Jongste, J.C.; Reiss, I.; McGrath, J.J.; Eyles, D.W.; Burne, T.H.; Tiemeier, H.; Jaddoe, V.W.; et al. Associations of maternal and fetal 25-hydroxyvitamin D levels with childhood eczema: The Generation R Study. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2016, 27, 283–289. [Google Scholar] [CrossRef]
- Morales, E.; Romieu, I.; Guerra, S.; Ballester, F.; Rebagliato, M.; Vioque, J.; Tardon, A.; Rodriguez Delhi, C.; Arranz, L.; Torrent, M.; et al. Maternal vitamin D status in pregnancy and risk of lower respiratory tract infections, wheezing, and asthma in offspring. Epidemiology 2012, 23, 64–71. [Google Scholar] [CrossRef]
- Magnus, M.C.; Stene, L.C.; Haberg, S.E.; Nafstad, P.; Stigum, H.; London, S.J.; Nystad, W. Prospective study of maternal mid-pregnancy 25-hydroxyvitamin D level and early childhood respiratory disorders. Paediatr. Perinat. Epidemiol. 2013, 27, 532–541. [Google Scholar] [CrossRef] [Green Version]
- Maslova, E.; Hansen, S.; Thorne-Lyman, A.L.; Jensen, C.B.; Strom, M.; Cohen, A.; Nielsen, N.O.; Olsen, S.F. Predicted vitamin D status in mid-pregnancy and child allergic disease. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2014, 25, 706–713. [Google Scholar] [CrossRef] [PubMed]
- Zosky, G.R.; Hart, P.H.; Whitehouse, A.J.; Kusel, M.M.; Ang, W.; Foong, R.E.; Chen, L.; Holt, P.G.; Sly, P.D.; Hall, G.L. Vitamin D deficiency at 16 to 20 weeks’ gestation is associated with impaired lung function and asthma at 6 years of age. Ann. Am. Thorac. Soc. 2014, 11, 571–577. [Google Scholar] [CrossRef] [PubMed]
- Weisse, K.; Winkler, S.; Hirche, F.; Herberth, G.; Hinz, D.; Bauer, M.; Roder, S.; Rolle-Kampczyk, U.; von Bergen, M.; Olek, S.; et al. Maternal and newborn vitamin D status and its impact on food allergy development in the German LINA cohort study. Allergy 2013, 68, 220–228. [Google Scholar] [CrossRef] [PubMed]
- Gale, C.R.; Robinson, S.M.; Harvey, N.C.; Javaid, M.K.; Jiang, B.; Martyn, C.N.; Godfrey, K.M.; Cooper, C.; Princess Anne Hospital Study, G. Maternal vitamin D status during pregnancy and child outcomes. Eur. J. Clin. Nutr. 2008, 62, 68–77. [Google Scholar] [CrossRef] [Green Version]
- Hansen, S.; Maslova, E.; Strom, M.; Linneberg, A.; Halldorsson, T.I.; Granstrom, C.; Dahl, R.; Hoffmann, H.J.; Olsen, S.F. The long-term programming effect of maternal 25-hydroxyvitamin D in pregnancy on allergic airway disease and lung function in offspring after 20 to 25 years of follow-up. J. Allergy Clin. Immunol. 2015, 136, 169–176.e2. [Google Scholar] [CrossRef]
- Woon, F.C.; Chin, Y.S.; Ismail, I.H.; Abdul Latiff, A.H.; Batterham, M.; Chan, Y.M.; On Behalf Of The Micos Research, G. Maternal Vitamin D Levels during Late Pregnancy and Risk of Allergic Diseases and Sensitization during the First Year of Life-A Birth Cohort Study. Nutrients 2020, 12, 2418. [Google Scholar] [CrossRef]
- Loo, E.X.L.; Tham, E.H.; Phang, K.W.; Goh, A.; Teoh, O.H.; Chong, Y.S.; Gluckman, P.D.; Godfrey, K.M.; Van Bever, H.; Lee, B.W.; et al. Associations between maternal vitamin D levels during pregnancy and allergic outcomes in the offspring in the first 5 years of life. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2019, 30, 117–122. [Google Scholar] [CrossRef]
- de Jongh, R.T.; Crozier, S.R.; D’Angelo, S.; Pike, K.C.; Roberts, G.; Lucas, J.S.; Inskip, H.; Godfrey, K.M.; Cooper, C.; Harvey, N.C.; et al. Maternal 25-hydroxyvitamin D levels in relation to offspring respiratory symptoms and infections. Eur. Respir. J. 2014, 43, 1181–1183. [Google Scholar] [CrossRef] [Green Version]
- Chiu, C.Y.; Huang, S.Y.; Peng, Y.C.; Tsai, M.H.; Hua, M.C.; Yao, T.C.; Yeh, K.W.; Huang, J.L. Maternal vitamin D levels are inversely related to allergic sensitization and atopic diseases in early childhood. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2015, 26, 337–343. [Google Scholar] [CrossRef]
- Pike, J.W.; Meyer, M.B. The vitamin D receptor: New paradigms for the regulation of gene expression by 1, 25-dihydroxyvitamin D3. Endocrinol. Metab. Clin. N. Am. 2010, 39, 255–269. [Google Scholar] [CrossRef] [Green Version]
- Rueter, K.; Black, L.J.; Jones, A.; Bulsara, M.; Clarke, M.W.; Gamez, C.; Lim, E.M.; Palmer, D.J.; Prescott, S.L.; Siafarikas, A. Analytical Bias in the Measurement of Plasma 25-Hydroxyvitamin D Concentrations in Infants. Int. J. Environ. Res. Public Health 2020, 17, 412. [Google Scholar] [CrossRef] [Green Version]
- Asher, M.I.; Keil, U.; Anderson, H.R.; Beasley, R.; Crane, J.; Martinez, F.; Mitchell, E.A.; Pearce, N.; Sibbald, B.; Stewart, A.W.; et al. International Study of Asthma and Allergies in Childhood (ISAAC): Rationale and methods. Eur. Respir. J. 1995, 8, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Heckmatt, J.Z.; Peacock, M.; Davies, A.E.; McMurray, J.; Isherwood, D.M. Plasma 25-hydroxyvitamin D in pregnant Asian women and their babies. Lancet 1979, 2, 546–548. [Google Scholar] [CrossRef]
- Cadario, F.; Savastio, S.; Pozzi, E.; Capelli, A.; Dondi, E.; Gatto, M.; Zaffaroni, M.; Bona, G. Vitamin D status in cord blood and newborns: Ethnic differences. Ital. J. Pediatr. 2013, 39, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grant, C.C.; Stewart, A.W.; Scragg, R.; Milne, T.; Rowden, J.; Ekeroma, A.; Wall, C.; Mitchell, E.A.; Crengle, S.; Trenholme, A.; et al. Vitamin D during pregnancy and infancy and infant serum 25-hydroxyvitamin D concentration. Pediatrics 2014, 133, e143–e153. [Google Scholar] [CrossRef] [Green Version]
- Wagner, C.L.; McNeil, R.B.; Johnson, D.D.; Hulsey, T.C.; Ebeling, M.; Robinson, C.; Hamilton, S.A.; Hollis, B.W. Health characteristics and outcomes of two randomized vitamin D supplementation trials during pregnancy: A combined analysis. J. Steroid Biochem. Mol. Biol. 2013, 136, 313–320. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Jiao, X.; Tian, Y.; Zhang, J.; Zhang, Y.; Li, J.; Yang, F.; Xu, M.; Yu, X.; Shanghai Birth Cohort, S. Associations between maternal vitamin D status during three trimesters and cord blood 25(OH)D concentrations in newborns: A prospective Shanghai birth cohort study. Eur. J. Nutr. 2021, 60, 3473–3483. [Google Scholar] [CrossRef]
- Chawes, B.L.; Bonnelykke, K.; Jensen, P.F.; Schoos, A.M.; Heickendorff, L.; Bisgaard, H. Cord Blood 25(OH)-Vitamin D Deficiency and Childhood Asthma, Allergy and Eczema: The COPSAC2000 Birth Cohort Study. PLoS ONE 2014, 9, e99856. [Google Scholar] [CrossRef] [Green Version]
- Stelmach, I.; Majak, P.; Jerzynska, J.; Podlecka, D.; Stelmach, W.; Polanska, K.; Gromadzinska, J.; Wasowicz, W.; Hanke, W. Cord serum 25-hydroxyvitamin D correlates with early childhood viral-induced wheezing. Respir. Med. 2015, 109, 38–43. [Google Scholar] [CrossRef] [Green Version]
- Jones, A.P.; Palmer, D.; Zhang, G.; Prescott, S.L. Cord blood 25-hydroxyvitamin D3 and allergic disease during infancy. Pediatrics 2012, 130, e1128–e1135. [Google Scholar] [CrossRef] [Green Version]
- Baiz, N.; Dargent-Molina, P.; Wark, J.D.; Souberbielle, J.C.; Annesi-Maesano, I.; Group, E.M.-C.C.S. Cord serum 25-hydroxyvitamin D and risk of early childhood transient wheezing and atopic dermatitis. J. Allergy Clin. Immunol. 2014, 133, 147–153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palmer, D.J.; Sullivan, T.R.; Skeaff, C.M.; Smithers, L.G.; Makrides, M.; DOMInO Allergy Follow-Up Team. Higher cord blood 25-hydroxyvitamin D concentrations reduce the risk of early childhood eczema: In children with a family history of allergic disease. World Allergy Organ. J. 2015, 8, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mustapa Kamal Basha, M.A.; Majid, H.A.; Razali, N.; Yahya, A. Risk of eczema, wheezing and respiratory tract infections in the first year of life: A systematic review of vitamin D concentrations during pregnancy and at birth. PLoS ONE 2020, 15, e0233890. [Google Scholar] [CrossRef] [PubMed]
- Visness, C.M.; Sandel, M.T.; O’Connor, G.; Gern, J.E.; Jaffee, K.F.; Wood, R.A.; Kattan, M.; Bloomberg, G.R.; Dresen, A.; Gergen, P.J.; et al. Cord blood vitamin D concentrations are unrelated to atopy and wheeze in 2 diverse birth cohort studies. J. Allergy Clin. Immunol. 2015, 136, 1108–1110.e2. [Google Scholar] [CrossRef] [Green Version]
- Jartti, T.; Kuusipalo, H.; Vuorinen, T.; Soderlund-Venermo, M.; Allander, T.; Waris, M.; Hartiala, J.; Ruuskanen, O. Allergic sensitization is associated with rhinovirus-, but not other virus-, induced wheezing in children. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2010, 21, 1008–1014. [Google Scholar] [CrossRef]
- Camargo, C.A., Jr.; Ingham, T.; Wickens, K.; Thadhani, R.; Silvers, K.M.; Epton, M.J.; Town, G.I.; Pattemore, P.K.; Espinola, J.A.; Crane, J.; et al. Cord-blood 25-hydroxyvitamin D levels and risk of respiratory infection, wheezing, and asthma. Pediatrics 2011, 127, e180–e187. [Google Scholar] [CrossRef] [Green Version]
- Song, H.; Yang, L.; Jia, C. Maternal vitamin D status during pregnancy and risk of childhood asthma: A meta-analysis of prospective studies. Mol. Nutr. Food Res. 2017, 61, 1600657. [Google Scholar] [CrossRef]
- Rothers, J.; Wright, A.L.; Stern, D.A.; Halonen, M.; Camargo, J.C.A. Cord blood 25-hydroxyvitamin D levels are associated with aeroallergen sensitization in children from Tucson, Arizona. J. Allergy Clin. Immunol. 2011, 128, 1093–1099.e5. [Google Scholar] [CrossRef] [Green Version]
- Hypponen, E.; Berry, D.J.; Wjst, M.; Power, C. Serum 25-hydroxyvitamin D and IgE—A significant but nonlinear relationship. Allergy 2009, 64, 613–620. [Google Scholar] [CrossRef]
- Pacheco-Gonzalez, R.M.; Garcia-Marcos, L.; Morales, E. Prenatal vitamin D status and respiratory and allergic outcomes in childhood: A meta-analysis of observational studies. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2018, 29, 243–253. [Google Scholar] [CrossRef]
- Chawes, B.L.; Bonnelykke, K.; Stokholm, J.; Vissing, N.H.; Bjarnadottir, E.; Schoos, A.M.; Wolsk, H.M.; Pedersen, T.M.; Vinding, R.K.; Thorsteinsdottir, S.; et al. Effect of Vitamin D3 Supplementation During Pregnancy on Risk of Persistent Wheeze in the Offspring: A Randomized Clinical Trial. JAMA J. Am. Med. Assoc. 2016, 315, 353–361. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldring, S.T.; Griffiths, C.J.; Martineau, A.R.; Robinson, S.; Yu, C.; Poulton, S.; Kirkby, J.C.; Stocks, J.; Hooper, R.; Shaheen, S.O.; et al. Prenatal vitamin d supplementation and child respiratory health: A randomised controlled trial. PLoS ONE 2013, 8, e66627. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Litonjua, A.A.; Carey, V.J.; Laranjo, N.; Harshfield, B.J.; McElrath, T.F.; O’Connor, G.T.; Sandel, M.; Iverson, R.E., Jr.; Lee-Paritz, A.; Strunk, R.C.; et al. Effect of Prenatal Supplementation With Vitamin D on Asthma or Recurrent Wheezing in Offspring by Age 3 Years: The VDAART Randomized Clinical Trial. JAMA J. Am. Med. Assoc. 2016, 315, 362–370. [Google Scholar] [CrossRef] [PubMed]
- Ng, K.; Scott, J.B.; Drake, B.F.; Chan, A.T.; Hollis, B.W.; Chandler, P.D.; Bennett, G.G.; Giovannucci, E.L.; Gonzalez-Suarez, E.; Meyerhardt, J.A.; et al. Dose response to vitamin D supplementation in African Americans: Results of a 4-arm, randomized, placebo-controlled trial. Am. J. Clin. Nutr. 2014, 99, 587–598. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhagatwala, J.; Zhu, H.; Parikh, S.J.; Guo, D.H.; Kotak, I.; Huang, Y.; Havens, R.; Pham, M.; Afari, E.; Kim, S.; et al. Dose and time responses of vitamin D biomarkers to monthly vitamin D3 supplementation in overweight/obese African Americans with suboptimal vitamin d status: A placebo controlled randomized clinical trial. BMC Obes. 2015, 2, 27. [Google Scholar] [CrossRef] [Green Version]
- Wegienka, G.; Havstad, S.; Joseph, C.L.; Zoratti, E.; Ownby, D.; Woodcroft, K.; Johnson, C.C. Racial disparities in allergic outcomes in African Americans emerge as early as age 2 years. Clin. Exp. Allergy J. Br. Soc. Allergy Clin. Immunol. 2012, 42, 909–917. [Google Scholar] [CrossRef] [Green Version]
- Allen, K.J.; Koplin, J.J.; Ponsonby, A.L.; Gurrin, L.C.; Wake, M.; Vuillermin, P.; Martin, P.; Matheson, M.; Lowe, A.; Robinson, M.; et al. Vitamin D insufficiency is associated with challenge-proven food allergy in infants. J. Allergy Clin. Immunol. 2013, 131, 1109–1116.e6. [Google Scholar] [CrossRef]
- Sitarik, A.; Havstad, S.; Kim, H.; Zoratti, E.M.; Ownby, D.; Johnson, C.C.; Wegienka, G. Racial disparities in allergic outcomes persist to age 10 years in black and white children. Ann. Allergy Asthma Immunol. Off. Publ. Am. Coll. Allergy Asthma Immunol. 2020, 124, 342–349. [Google Scholar] [CrossRef] [Green Version]
- Wolsk, H.M.; Harshfield, B.J.; Laranjo, N.; Carey, V.J.; O’Connor, G.; Sandel, M.; Strunk, R.C.; Bacharier, L.B.; Zeiger, R.S.; Schatz, M.; et al. Vitamin D supplementation in pregnancy, prenatal 25(OH)D levels, race, and subsequent asthma or recurrent wheeze in offspring: Secondary analyses from the Vitamin D Antenatal Asthma Reduction Trial. J. Allergy Clin. Immunol. 2017, 140, 1423–1429.e5. [Google Scholar] [CrossRef] [Green Version]
- Litonjua, A.A.; Lange, N.E.; Carey, V.J.; Brown, S.; Laranjo, N.; Harshfield, B.J.; O’Connor, G.T.; Sandel, M.; Strunk, R.C.; Bacharier, L.B.; et al. The Vitamin D Antenatal Asthma Reduction Trial (VDAART): Rationale, design, and methods of a randomized, controlled trial of vitamin D supplementation in pregnancy for the primary prevention of asthma and allergies in children. Contemp. Clin. Trials 2014, 38, 37–50. [Google Scholar] [CrossRef] [Green Version]
- Hanifin, J.; Rajka, G. Diagnostic features of atopic dermatitis. Acta Derm. Venereol. 1980, 92, 44–47. [Google Scholar]
- Bahnson, H.T.; du Toit, G.; Lack, G. Statistical Considerations of Food Allergy Prevention Studies. J. Allergy Clin. Immunol. Pract. 2017, 5, 274–282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolsk, H.M.; Chawes, B.L.; Litonjua, A.A.; Hollis, B.W.; Waage, J.; Stokholm, J.; Bonnelykke, K.; Bisgaard, H.; Weiss, S.T. Prenatal vitamin D supplementation reduces risk of asthma/recurrent wheeze in early childhood: A combined analysis of two randomized controlled trials. PLoS ONE 2017, 12, e0186657. [Google Scholar] [CrossRef] [PubMed]
- Kimlin, M.G.; Olds, W.J.; Moore, M.R. Location and vitamin D synthesis: Is the hypothesis validated by geophysical data? J. Photochem. Photobiol. B Biol. 2007, 86, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Larsen, V.; Ierodiakonou, D.; Jarrold, K.; Cunha, S.; Chivinge, J.; Robinson, Z.; Geoghegan, N.; Ruparelia, A.; Devani, P.; Trivella, M.; et al. Diet during pregnancy and infancy and risk of allergic or autoimmune disease: A systematic review and meta-analysis. PLoS Med. 2018, 15, e1002507. [Google Scholar] [CrossRef] [PubMed]
- Grant, C.C.; Crane, J.; Mitchell, E.A.; Sinclair, J.; Stewart, A.; Milne, T.; Knight, J.; Gilchrist, C.; Camargo, J.C.A. Vitamin D supplementation during pregnancy and infancy reduces aeroallergen sensitization: A randomized controlled trial. Allergy 2016, 71, 1325–1334. [Google Scholar] [CrossRef]
- Brustad, N.; Eliasen, A.U.; Stokholm, J.; Bonnelykke, K.; Bisgaard, H.; Chawes, B.L. High-Dose Vitamin D Supplementation During Pregnancy and Asthma in Offspring at the Age of 6 Years. JAMA J. Am. Med. Assoc. 2019, 321, 1003–1005. [Google Scholar] [CrossRef] [Green Version]
- Litonjua, A.A.; Carey, V.J.; Laranjo, N.; Stubbs, B.J.; Mirzakhani, H.; O’Connor, G.T.; Sandel, M.; Beigelman, A.; Bacharier, L.B.; Zeiger, R.S.; et al. Six-Year Follow-up of a Trial of Antenatal Vitamin D for Asthma Reduction. N. Engl. J. Med. 2020, 382, 525–533. [Google Scholar] [CrossRef]
- Hornsby, E.; Pfeffer, P.E.; Laranjo, N.; Cruikshank, W.; Tuzova, M.; Litonjua, A.A.; Weiss, S.T.; Carey, V.J.; O’Connor, G.; Hawrylowicz, C. Vitamin D supplementation during pregnancy: Effect on the neonatal immune system in a randomized controlled trial. J. Allergy Clin. Immunol. 2018, 141, 269–278.e1. [Google Scholar] [CrossRef] [Green Version]
- Gluckman, P.D.; Hanson, M.A.; Cooper, C.; Thornburg, K.L. Effect of in utero and early-life conditions on adult health and disease. N. Engl. J. Med. 2008, 359, 61–73. [Google Scholar] [CrossRef] [Green Version]
- McDade, T.W. Early environments and the ecology of inflammation. Proc. Natl. Acad. Sci. USA 2012, 109, 17281–17288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strachan, D.P. Hay fever, hygiene, and household size. Br. Med. J. 1989, 299, 1259–1260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaub, B.; Lauener, R.; von Mutius, E. The many faces of the hygiene hypothesis. J. Allergy Clin. Immunol. 2006, 117, 969–977. [Google Scholar] [CrossRef] [PubMed]
- Prescott, S.L.; Smith, P.; Tang, M.; Palmer, D.J.; Sinn, J.; Huntley, S.J.; Cormack, B.; Heine, R.G.; Gibson, R.A.; Makrides, M. The importance of early complementary feeding in the development of oral tolerance: Concerns and controversies. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2008, 19, 375–380. [Google Scholar] [CrossRef]
- Joshi, S.; Kotecha, S. Lung growth and development. Early Hum. Dev. 2007, 83, 789–794. [Google Scholar] [CrossRef]
- Henderson, A.J.; Warner, J.O. Fetal origins of asthma. Semin. Fetal Neonatal Med. 2012, 17, 82–91. [Google Scholar] [CrossRef]
- Rueter, K.; Haynes, A.; Prescott, S.L. Developing Primary Intervention Strategies to Prevent Allergic Disease. Curr. Allergy Asthma Rep. 2015, 15, 40. [Google Scholar] [CrossRef]
- Hollis, B.W.; Roos, B.A.; Draper, H.H.; Lambert, P.W. Vitamin D and its metabolites in human and bovine milk. J. Nutr. 1981, 111, 1240–1248. [Google Scholar] [CrossRef]
- Greer, F.R.; Hollis, B.W.; Cripps, D.J.; Tsang, R.C. Effects of maternal ultraviolet B irradiation on vitamin D content of human milk. J. Pediatr. 1984, 105, 431–433. [Google Scholar] [CrossRef]
- Hollis, B.W.; Wagner, C.L. Clinical review: The role of the parent compound vitamin D with respect to metabolism and function: Why clinical dose intervals can affect clinical outcomes. J. Clin. Endocrinol. Metab. 2013, 98, 4619–4628. [Google Scholar] [CrossRef] [Green Version]
- Wagner, C.L.; Hulsey, T.C.; Fanning, D.; Ebeling, M.; Hollis, B.W. High-dose vitamin D3 supplementation in a cohort of breastfeeding mothers and their infants: A 6-month follow-up pilot study. Breastfeed. Med. Off. J. Acad. Breastfeed. Med. 2006, 1, 59–70. [Google Scholar] [CrossRef] [Green Version]
- Hollis, B.W.; Wagner, C.L. Vitamin D requirements during lactation: High-dose maternal supplementation as therapy to prevent hypovitaminosis D for both the mother and the nursing infant. Am. J. Clin. Nutr. 2004, 80, 1752S–1758S. [Google Scholar] [CrossRef]
- Gallo, S.; Comeau, K.; Vanstone, C.; Agellon, S.; Sharma, A.; Jones, G.; L’Abbe, M.; Khamessan, A.; Rodd, C.; Weiler, H. Effect of different dosages of oral vitamin D supplementation on vitamin D status in healthy, breastfed infants: A randomized trial. JAMA J. Am. Med. Assoc. 2013, 309, 1785–1792. [Google Scholar] [CrossRef] [Green Version]
- Barman, M.; Jonsson, K.; Hesselmar, B.; Sandin, A.; Sandberg, A.S.; Wold, A.E. No association between allergy and current 25-hydroxy vitamin D in serum or vitamin D intake. Acta Paediatr. 2015, 104, 405–413. [Google Scholar] [CrossRef]
- Kull, I.B.A.; Melén, E.; Lilja, G.; van Hage, M.; Pershagen, G.; Wickman, M. Earlylife supplementation of vitamins A and D, in water-soluble form or in peanut oil, and allergic diseases during childhood. J. Allergy Clin. Immunol. 2006, 118, 1299–1304. [Google Scholar] [CrossRef]
- Berents, T.L.; Lodrup Carlsen, K.C.; Mowinckel, P.; Sandvik, L.; Skjerven, H.O.; Rolfsjord, L.B.; Kvenshagen, B.; Hunderi, J.O.; Bradley, M.; Lieden, A.; et al. Vitamin D levels and atopic eczema in infancy and early childhood in Norway: A cohort study. Br. J. Dermatol. 2016, 175, 95–101. [Google Scholar] [CrossRef]
- Molloy, J.; Koplin, J.J.; Allen, K.J.; Tang, M.L.K.; Collier, F.; Carlin, J.B.; Saffery, R.; Burgner, D.; Ranganathan, S.; Dwyer, T.; et al. Vitamin D insufficiency in the first 6 months of infancy and challenge-proven IgE-mediated food allergy at 1 year of age: A case-cohort study. Allergy 2017, 72, 1222–1231. [Google Scholar] [CrossRef]
- Cairncross, C.; Grant, C.; Stonehouse, W.; Conlon, C.; McDonald, B.; Houghton, L.; Eyles, D.; Camargo, C.A.; Coad, J.; von Hurst, P. The Relationship between Vitamin D Status and Allergic Diseases in New Zealand Preschool Children. Nutrients 2016, 8, 326. [Google Scholar] [CrossRef]
- Sharief, S.; Jariwala, S.; Kumar, J.; Muntner, P.; Melamed, M.L. Vitamin D levels and food and environmental allergies in the United States: Results from the National Health and Nutrition Examination Survey 2005–2006. J. Allergy Clin. Immunol. 2011, 127, 1195–1202. [Google Scholar] [CrossRef] [Green Version]
- Wang, S.S.; Hon, K.L.; Kong, A.P.; Pong, H.N.; Wong, G.W.; Leung, T.F. Vitamin D deficiency is associated with diagnosis and severity of childhood atopic dermatitis. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2014, 25, 30–35. [Google Scholar] [CrossRef]
- Hollams, E.M.; Teo, S.M.; Kusel, M.; Holt, B.J.; Holt, K.E.; Inouye, M.; De Klerk, N.H.; Zhang, G.; Sly, P.D.; Hart, P.H.; et al. Vitamin D over the first decade and susceptibility to childhood allergy and asthma. J. Allergy Clin. Immunol. 2017, 139, 472–481.e9. [Google Scholar] [CrossRef] [Green Version]
- Heimbeck, I.; Wjst, M.; Apfelbacher, C.J. Low vitamin D serum level is inversely associated with eczema in children and adolescents in Germany. Allergy 2013, 68, 906–910. [Google Scholar] [CrossRef]
- Cairncross, C.T.; Stonehouse, W.; Conlon, C.A.; Grant, C.C.; McDonald, B.; Houghton, L.A.; Eyles, D.; Camargo, C.A., Jr.; Coad, J.; von Hurst, P.R. Predictors of vitamin D status in New Zealand preschool children. Matern. Child Nutr. 2017, 13, e12340. [Google Scholar] [CrossRef]
- Guo, Y.; Yu, L.; Deng, Y.H.; Ke, H.J.; Wu, J.L. Associations between serum 25-hydroxyvitamin D levels and allergic sensitization in early childhood. Allergol. Immunopathol. 2020, 48, 84–89. [Google Scholar] [CrossRef]
- Baek, J.H.; Shin, Y.H.; Chung, I.H.; Kim, H.J.; Yoo, E.G.; Yoon, J.W.; Jee, H.M.; Chang, Y.E.; Han, M.Y. The Link between Serum Vitamin D Level, Sensitization to Food Allergens, and the Severity of Atopic Dermatitis in Infancy. J. Pediatr. 2014, 165, 849–854.e1. [Google Scholar] [CrossRef]
- Kutlug, S.; Kilic, M.; Bilgici, B.; Paksu, S.; Yildiran, A.; Sancak, R. An evaluation of vitamin D levels in children with seasonal allergic rhinitis during pollen season. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2017, 28, 446–451. [Google Scholar] [CrossRef]
- Hollams, E.M.; Hart, P.H.; Holt, B.J.; Serralha, M.; Parsons, F.; de Klerk, N.H.; Zhang, G.; Sly, P.D.; Holt, P.G. Vitamin D and atopy and asthma phenotypes in children: A longitudinal cohort study. Eur. Respir. J. 2011, 38, 1320–1327. [Google Scholar] [CrossRef]
- Williams, H.C.; Burney, P.G.; Pembroke, A.C.; Hay, R.J. The U.K. Working Party’s Diagnostic Criteria for Atopic Dermatitis. III. Independent hospital validation. Br. J. Dermatol. 1994, 131, 406–416. [Google Scholar] [CrossRef]
- Rosendahl, J.; Valkama, S.; Holmlund-Suila, E.; Enlund-Cerullo, M.; Hauta-Alus, H.; Helve, O.; Hytinantti, T.; Levalahti, E.; Kajantie, E.; Viljakainen, H.; et al. Effect of Higher vs Standard Dosage of Vitamin D3 Supplementation on Bone Strength and Infection in Healthy Infants: A Randomized Clinical Trial. JAMA Pediatr. 2018, 172, 646–654. [Google Scholar] [CrossRef] [Green Version]
- Rosendahl, J.; Pelkonen, A.S.; Helve, O.; Hauta-Alus, H.; Holmlund-Suila, E.; Valkama, S.; Enlund-Cerullo, M.; Viljakainen, H.; Hytinantti, T.; Makitie, O.; et al. High-Dose Vitamin D Supplementation Does Not Prevent Allergic Sensitization of Infants. J. Pediatr. 2019, 209, 139–145.e1. [Google Scholar] [CrossRef] [Green Version]
- Hibbs, A.M.; Ross, K.; Kerns, L.A.; Wagner, C.; Fuloria, M.; Groh-Wargo, S.; Zimmerman, T.; Minich, N.; Tatsuoka, C. Effect of Vitamin D Supplementation on Recurrent Wheezing in Black Infants Who Were Born Preterm: The D-Wheeze Randomized Clinical Trial. JAMA J. Am. Med. Assoc. 2018, 319, 2086–2094. [Google Scholar] [CrossRef]
- Goedicke-Fritz, S.; Hartel, C.; Krasteva-Christ, G.; Kopp, M.V.; Meyer, S.; Zemlin, M. Preterm Birth Affects the Risk of Developing Immune-Mediated Diseases. Front. Immunol. 2017, 8, 1266. [Google Scholar] [CrossRef] [Green Version]
- Kotecha, S.; Clemm, H.; Halvorsen, T.; Kotecha, S.J. Bronchial hyper-responsiveness in preterm-born subjects: A systematic review and meta-analysis. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2018, 29, 715–725. [Google Scholar] [CrossRef]
- Rueter, K.; Jones, A.P.; Siafarikas, A.; Lim, E.M.; Bear, N.; Noakes, P.S.; Prescott, S.L.; Palmer, D.J. Direct infant UV light exposure is associated with eczema and immune development. J. Allergy Clin. Immunol. 2019, 143, 1012–1020.e2. [Google Scholar] [CrossRef] [Green Version]
- Rueter, K.; Jones, A.P.; Siafarikas, A.; Lim, E.M.; Prescott, S.L.; Palmer, D.J. In “High-Risk” Infants with Sufficient Vitamin D Status at Birth, Infant Vitamin D Supplementation Had No Effect on Allergy Outcomes: A Randomized Controlled Trial. Nutrients 2020, 12, 1747. [Google Scholar] [CrossRef]
- Maalmi, H.; Berraies, A.; Tangour, E.; Ammar, J.; Abid, H.; Hamzaoui, K.; Hamzaoui, A. The impact of vitamin D deficiency on immune T cells in asthmatic children: A case-control study. J. Asthma Allergy 2012, 5, 11–19. [Google Scholar] [CrossRef] [Green Version]
- Mullins, R.J.; Camargo, C.A. Latitude, sunlight, vitamin D, and childhood food allergy/anaphylaxis. Curr. Allergy Asthma Rep. 2012, 12, 64–71. [Google Scholar] [CrossRef]
- Thyssen, J.P.; Zirwas, M.J.; Elias, P.M. Potential role of reduced environmental UV exposure as a driver of the current epidemic of atopic dermatitis. J. Allergy Clin. Immunol. 2015, 136, 1163–1169. [Google Scholar] [CrossRef] [Green Version]
- Hwang, J.M.; Oh, S.H.; Shin, M.Y. The relationships among birth season, sunlight exposure during infancy, and allergic disease. Korean J. Pediatr. 2016, 59, 218–225. [Google Scholar] [CrossRef] [Green Version]
- Rueter, K.; Jones, A.P.; Siafarikas, A.; Chivers, P.; Prescott, S.L.; Palmer, D.J. The Influence of Sunlight Exposure and Sun Protecting Behaviours on Allergic Outcomes in Early Childhood. Int. J. Environ. Res. Public Health 2021, 18, 5429. [Google Scholar] [CrossRef]
- Chen, L.; Zosky, G.R. Lung development. Photochem. Photobiol. Sci. Off. J. Eur. Photochem. Assoc. Eur. Soc. Photobiol. 2017, 16, 339–346. [Google Scholar] [CrossRef]
- Bener, A.; Ehlayel, M.S.; Bener, H.Z.; Hamid, Q. The impact of Vitamin D deficiency on asthma, allergic rhinitis and wheezing in children: An emerging public health problem. J. Family Community Med. 2014, 21, 154–161. [Google Scholar] [CrossRef] [Green Version]
- Freishtat, R.J.; Iqbal, S.F.; Pillai, D.K.; Klein, C.J.; Ryan, L.M.; Benton, A.S.; Teach, S.J. High prevalence of vitamin D deficiency among inner-city African American youth with asthma in Washington, DC. J. Pediatr. 2010, 156, 948–952. [Google Scholar] [CrossRef] [Green Version]
- Upham, J.W.; Lee, P.T.; Holt, B.J.; Heaton, T.; Prescott, S.L.; Sharp, M.J.; Sly, P.D.; Holt, P.G. Development of interleukin-12-producing capacity throughout childhood. Infect. Immun. 2002, 70, 6583–6588. [Google Scholar] [CrossRef] [Green Version]
- Nelson, D.J.; Holt, P.G. Defective regional immunity in the respiratory tract of neonates is attributable to hyporesponsiveness of local dendritic cells to activation signals. J. Immunol. 1995, 155, 3517–3524. [Google Scholar]
- Lips, P.; van Schoor, N.M. The effect of vitamin D on bone and osteoporosis. Best Pract. Res. Clin. Endocrinol. Metab. 2011, 25, 585–591. [Google Scholar] [CrossRef]
| Reference and Year Latitude | Study Population | 25(OH)D Level | Main Results | Higher 25(OH)D Level |
|---|---|---|---|---|
| Camargo et al. (2011) Wellington and Christchurch, New Zealand Latitude 41–43 πS | 922 mother–child pairs General population | CB Median = 44 nmol/L (IQR 29–78) | Lower CB 25(OH)D (<10 ng/mL) levels were at higher risk for wheezing at 15 mo, 3 and 5 years than higher CB levels (>30 ng/mL) No association with asthma at 5 years of age | W↓ A←→ |
| Rothers et al. (2011) Tuscon, Arizona Latitude 32.22 πN | 219 mother–child pairs General population | CB Median = 64 nmol/L (IQR 49–81) | Lower (<50 ng/mL) and higher (≥100 ng/mL) levels of CB 25(OH)D were associated with increased total IgE and aeroallergen (sIgE) sensitization at 1, 2, 3, and 5 years of age No association with AR or asthma at 5 years | S U A←→ AR←→ |
| Jones et al. (2012) Perth, Australia Latitude 31.95 πS | 231 mother–child pairs High-risk population | CB Mean = 58 nmol/L (SD ± 24.1) | Lower CB level is associated with a higher risk for eczema at 12 months No association with wheeze, allergen sensitization or IgE-mediated food allergies | E↓ W←→ S←→ FA←→ |
| Weisse et al. (2013) Leipzig, Germany Latitude 51.4 πN | 378 mother–child pairs General population | CB median = 27 nmol/L (IQR: 17–43) | Positive association between CB 25(OH)D levels with food allergy within 2nd year of life No association with eczema and sensitization | FA↑ S←→ E←→ |
| Baiz et al. (2014) Poitiers and Nancy, France Latitude 46–48 πN | 239 mother–child pairs General population | CB Mean = 44 nmol/L (IQR: 38 nmol/L) | Inverse association between CB 25(OH)D levels with early transient wheezing and eczema by age 1, 3, and 5 years No association with asthma and AR at 5 years of age | W↓ E↓ A←→ AR←→ |
| Stelmach et al. (2015) Lodz, Poland Latitude 51.76 πN | 240 mother–child pairs General population | CB median 15.8 nmol/mL (IQR 10.4–21.3) | Inverse association between CB 25(OH)D levels wheezing in first 2 years of life No association with food allergy and eczema | W↓ E←→ FA←→ |
| Palmer et al. (2015) Adelaide, Australia Latitude 34.92 πS | 270 mother–child pairs High-risk population | CB mean 57.0 nmol/L (SD ± 24.1) | Inverse association between CB 25(OH)D and eczema to 3 years, stronger association at 1 year of age. IgE-mediated food allergies at 1 year of age in 4/260 (1.5%) children. The risk of IgE-mediated food allergies at 1 year of age (but not at 3 years of age) decreased as CB 25(OH)D concentration increased. No association with asthma, allergic rhinitis or sensitization | E↓ FA↓ A←→ AR←→ |
| Visness et al. (2015) Baltimore, Boston, New York and St Louis, USA Latitude 38–42 πN and Madison, Wisconsin Latitude 43.1 πN | 435 mother–child pairs and 258 mother–child pairs Both high-risk populations | CB median 50.3 nmol/mL (range 10.5–109.2) CB median 52.8 nmol/mL (range 10.0–194.3) | No association between CB 25(OH)D and any wheeze in first year or recurrent wheeze at 3 years No association with food allergy or food or aeroallergen sensitization to 5 years old No association with wheeze in the first 3 years, of life, food or aeroallergen sensitization to 5 years old and asthma at 6 years of age | W←→ FA←→ S←→ W←→ S←→ |
| Gazibara et al.(2015) Rotterdam, The Netherlands Latitude 51.91 πN | 2407 mother–child pairs General population | CB median 40.2 nmol/L (range 11–144.9) | No association between CB 25(OH)D levels divided into tertiles (lowest tertile (30.5 nmol/L), middle tertile (≥30.5–49), and highest tertile (≥49.0) and wheeze within the first 6 years of age | W←→ |
| Blomberg et al. (2017) Massachusetts, USA Latitude 42.41 πN | 1418 mother–child pairs General population | CB mean or median level not given | No association between CB 25(OH)D levels of sufficiency, deficiency and insufficiency (divided into 6 categories) and eczema outcome within the first 7 to 8 years of life | E←→ |
| Hennessy et al. (2018) Cork, Ireland Latitude 51.89 πN | 1050 mother–child pairs General population | CB mean 35.5 nmol/L (SD ± 18.2) | No association between CB 25(OH)D levels and: Persistent eczema in the first 2 years Food allergy and food and aeroallergen sensitization at 2 years of age Asthma at 5 years of age | E←→ FA←→ S←→ A←→ |
| Reference and Year Latitude | Study Population | Intervention Groups/Doses | Intervention Period | Duration of Intervention | Follow-Up Period/Age at Assessment | How the Outcome Was Assessed | Main Results |
|---|---|---|---|---|---|---|---|
| Goldring et al. (2013) London, UK 51.5 πN RCT, prospective | 180 mothers Mixed ethnic groups: 25% Asian, 26% Middle Eastern, 25% Black, 24% White General population | Maternal: Placebo, n = 50 800 IU/d vitD2 n = 56 Single oral bolus of 200.000 IU vitD3 n = 52 | 27 weeks to birth | 3 months | At 3 years of age | ISAAC questionnaire Except food allergy: physician diagnosed | 800 IU/day vitD2 vs. placebo No difference at age 3 in: -Wheeze ever (aOR 0.56; CI 0.20–1.57; p = 0.27) -Eczema ever (aOR 0.61; CI 0.23–1.67; p = 0.34) -AR (aOR 0.63; CI 0.17–2.36; p = 0.49) -Food allergy (aOR 4.53; CI 0.52–39.33; p = 0.17) Single oral bolus of 200.000 IU vitD3 vs. placebo No difference at age 3 in: -Wheeze ever (aOR 1.17; CI 0.44–3.10; p = 0.75) -Eczema ever (aOR 0.86; CI 0.32–2.28; p = 0.76) -AR (aOR 0.91; CI 0.20–4.11; p = 0.90) |
| Chawes et al. (2016) Brustad et al. (2019) Denmark 55 πN RCT, prospective | 623 mothers >90% European General population | Maternal: Placebo and 400 IU/d vit D3 n = 308 2400 IU/d and 400 IU/d vitD3 n = 315 | 24 weeks to 1 week postpartum | 3.5 to 4 months | Face-to-face medical follow-up visits at 1,3,6,12,18,24,30, 36 months Sensitization tested at 6 and 18 months | Persistent wheeze/asthma diagnosed by validated quanti- tative algorithm Eczema: criteria of Hanifin and Rajka [161] For sensitization: Skin Prick Test (SPT): ≥2 mm than negative control; or sIgE | 2800 IU/day vs. 400 IU/day vitD3 No difference in: -Persistent wheeze (HR 0.76, CI 0.52–1.12; p = 0.16) at 0–3 years -Asthma (OR 0.82; CI 0.50–1.36; p = 0.45) at 3 years -Eczema (HR 0.90; CI 0.65–1.26; p = 0.55) at 0–3 years -Sensitization at 6 or 18 mo by sIgE (OR 1.55; CI 0.89–2.73; p = 0.13) or SPT (OR 1.24; CI 0.66–2.31; p = 0.51) |
| Litonjua et al. (2016 and 2020) Boston, USA 42.3 πN Washington, USA 47.75 πN San Diego, USA 32.71 πN RCT, prospective | 876 mothers Mixed ethnic groups: 49% Black, 13% White Hispanic, 20% White non-Hispanic 18% other High risk for allergies | Maternal: 400 IU/d vitD3, n= 436 4400 IU/d vitD3 n = 440 | Between 10 and 18 weeks to delivery | 5 to 7.5 months | Every 3 months: phone call At 1, 2, and 3 years of age: face-to-face assessment by scientific staff | Parent report of physician diagnosis sIgE levels | 4400 IU/day vs. 400 IU/day vitD3 No difference within first 3 years in: -Recurrent wheeze/asthma (HR 0.8, CI 0.6–1.0; p = 0.51) -Eczema with rash (HR 0.9; CI 0.7–1.2; p = 0.56) Sensitization (IgE): lower in the 4400 IU/d group than in the 400 IU/d group: (10.7%; CI, 9.4–12.1% vs. 12.4%, CI, 11.45–13.5%, p = 0.02) |
| Grant et al. (2016) Auckland, New Zealand 36.84 πS RCT, post hoc | 260 mother–infant pairs Mixed ethnic groups: 16% European, 24% Mãori, 43% Pacific, 17% Other General population | Maternal/infant pairs Placebo/placebo n = 87 1000 IU/400 IU/d vitD3, n = 87 2000 IU/800 IU/d vitD3, n = 86 | Maternal: 27 weeks to birth Infant: birth to 6 months | Maternal: 3 months Infant: 6 months | Interviews at: 2, 4, 6 and 18 months | Primary care records for physician diagnosis For sensitization to aeroallergens: SPT (≥3 mm than negative control) or specific IgE levels | At 18 months of age: Sensitization Results presented for placebo, lower dose, and higher dose vitD3 - sIgE levels: Der-f1 (18% vs. 10% vs. 2%) Der-f2 (14% vs. 3% vs. 2%) Der-p1 (19% vs. 14% vs. 3%) Der-p2 (12% vs. 2% vs. 3%) For all p < 0.05 Grass pollen: p = 0.74 Cat: p = 0.99 -SPT: House Dust Mite (9% vs. 3% vs. 0%: p = 0.03) Cat: p = 0.74 Grass pollen: p = 0.99 -Asthma: (11% vs. 0% vs. 4%, p = 0.002) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rueter, K.; Siafarikas, A.; Palmer, D.J.; Prescott, S.L. Pre- and Postnatal Vitamin D Status and Allergy Outcomes in Early Childhood. Biomedicines 2022, 10, 933. https://doi.org/10.3390/biomedicines10050933
Rueter K, Siafarikas A, Palmer DJ, Prescott SL. Pre- and Postnatal Vitamin D Status and Allergy Outcomes in Early Childhood. Biomedicines. 2022; 10(5):933. https://doi.org/10.3390/biomedicines10050933
Chicago/Turabian StyleRueter, Kristina, Aris Siafarikas, Debra J. Palmer, and Susan L. Prescott. 2022. "Pre- and Postnatal Vitamin D Status and Allergy Outcomes in Early Childhood" Biomedicines 10, no. 5: 933. https://doi.org/10.3390/biomedicines10050933
APA StyleRueter, K., Siafarikas, A., Palmer, D. J., & Prescott, S. L. (2022). Pre- and Postnatal Vitamin D Status and Allergy Outcomes in Early Childhood. Biomedicines, 10(5), 933. https://doi.org/10.3390/biomedicines10050933






