Use of Urinary Cytokine and Chemokine Levels for Identifying Bladder Conditions and Predicting Treatment Outcomes in Patients with Interstitial Cystitis/Bladder Pain Syndrome
Abstract
:1. Introduction
2. Materials and Methods
2.1. Treatment and Outcome Assessment
2.2. Urinary Biomarker Investigation
2.3. Cytokine and Chemokine Assay
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HIC | Hunner’s interstitial cystitis |
| Non-HIC | Non-Hunner’s interstitial cystitis |
| MBC | Maximal bladder capacity |
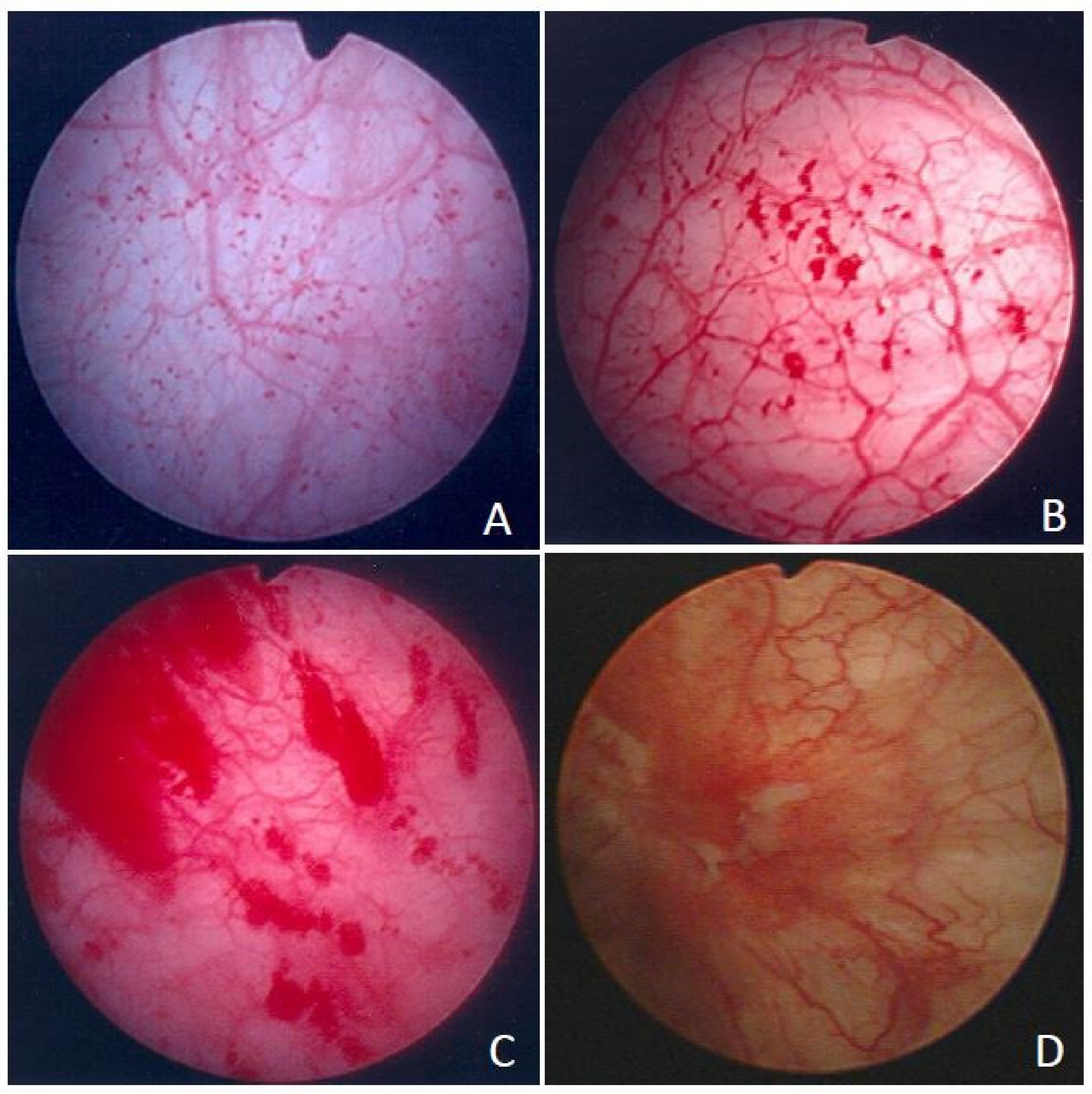
| GR | Glomerulation |
| IC/BPS | Interstitial cystitis/bladder pain syndrome |
| ESSIC | European Society for the Study of Interstitial Cystitis |
| IL | Interleukin |
| CXCL 10 | C-X-C motif chemokine ligand 10 |
| MCP-1 | Monocyte chemoattractant protein-1 |
| BDNF | Brain-derived neurotrophic factor |
| MIP-1β | Macrophage inflammatory protein-1β |
| RANTES | Regulated on activation, normal T-cell expressed and secreted protein |
| TNF-α | Tumor necrosis factor-α |
| PGE2 | Prostaglandin E2 |
| PPV | Positive predictive value |
| NPV | Negative predictive value |
References
- Hanno, P.M.; Sant, G.R. Clinical highlights of the National Institute of Diabetes and Digestive and Kidney Diseases/Interstitial Cystitis Association scientific conference on interstitial cystitis. Urology 2001, 57 (Suppl. 1), 2–6. [Google Scholar] [CrossRef]
- Hanno, P.M.; Erickson, D.; Moldwin, R.; Faraday, M.M.; American Urological Association. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J. Urol. 2015, 193, 1545–1553. [Google Scholar] [CrossRef] [PubMed]
- Hanno, P.M.; Erickson, D.; Moldwin, R.; Faraday, M.M.; American Urological Association. Clinical guidelines for interstitial cystitis/bladder pain syndrome. Int. J. Urol. 2020, 27, 578–589. [Google Scholar]
- Akiyama, Y.; Homma, Y.; Maeda, D. Pathology and terminology of interstitial cystitis/bladder pain syndrome: A review. Histol. Histopathol. 2019, 34, 25–32. [Google Scholar]
- Fall, M.; Baranowski, A.P.; Elneil, S.; Engeler, D.; Hughes, J.; Messelink, E.J.; Oberpenning, F.; de Williams, A.; European Association of Urology. EAU guidelines on chronic pelvic pain. Eur. Urol. 2010, 57, 35–48. [Google Scholar] [CrossRef]
- Malde, S.; Palmisani, S.; Al-Kaisy, A.; Sahai, A. Guideline of guidelines: Bladder pain syndrome. BJU Int. 2018, 122, 729–743. [Google Scholar] [CrossRef] [Green Version]
- Jhang, J.F.; Hsu, Y.H.; Ho, H.C.; Jiang, Y.H.; Lee, C.L.; Yu, W.R.; Kuo, H.C. Possible association between bladder wall morphological changes on computed tomography and bladder-centered interstitial cystitis/bladder pain syndrome. Biomedicines 2021, 9, 1306. [Google Scholar] [CrossRef]
- Van de Merwe, J.P.; Nordling, J.; Bouchelouche, P.; Bouchelouche, K.; Vervigni, M.; Daha, L.K.; Elneil, S.; Fall, M.; Hohlbrugger, G.; Irwin, P.; et al. Diagnostic criteria, classification, and nomenclature for painful bladder syndrome/interstitial cystitis: An ESSIC proposal. Eur. Urol. 2008, 53, 60–67. [Google Scholar] [CrossRef]
- Jhang, J.F.; Hsu, Y.H.; Jiang, Y.H.; Ho, H.C.; Kuo, H.C. Clinical relevance of bladder histopathological findings and their impact on treatment outcomes among patients with interstitial cystitis/bladder pain syndrome: An investigation of the European Society for the Study of interstitial Cystitis histopathological classification. J. Urol. 2021, 205, 226–235. [Google Scholar]
- Yu, W.R.; Jhang, J.F.; Ho, H.C.; Jiang, Y.H.; Lee, C.L.; Hsu, Y.H.; Kuo, H.C. Cystoscopic hydrodistention characteristics provide clinical and long-term prognostic features of interstitial cystitis after treatment. Sci. Rep. 2021, 11, 455. [Google Scholar] [CrossRef]
- Akiyama, Y. Biomarkers in interstitial cystitis/bladder pain syndrome with and without Hunner Lesion: A review and future perspectives. Diagnostics 2021, 11, 2238. [Google Scholar] [CrossRef] [PubMed]
- Kuo, H.C. Potential urine and serum biomarkers for patients with bladder pain syndrome/interstitial cystitis. Int. J. Urol. 2014, 21 (Suppl. 1), 34–41. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; De Hoedt, A.; Wiggins, E.; Haywood, K.; Jin, P.; Greenwood, B.; Narain, N.R.; Tolstikov, V.; Bussberg, V.; Barbour, K.E.; et al. Diagnostic utility of serum and urinary metabolite analysis in patients with interstitial cystitis/painful bladder syndrome. Urology 2021, 157, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.H.; Jhang, J.F.; Hsu, Y.H.; Ho, H.C.; Wu, Y.H.; Kuo, H.C. Urine biomarkers in ESSIC type 2 interstitial cystitis/bladder pain syndrome and overactive bladder with developing a novel diagnostic algorithm. Sci. Rep. 2021, 11, 914. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.H.; Jhang, J.F.; Hsu, Y.H.; Ho, H.C.; Wu, Y.H.; Kuo, H.C. Urine cytokines as biomarkers for diagnosing interstitial cystitis/bladder pain syndrome and mapping its clinical characteristics. Am. J. Physiol. Ren. Physiol. 2020, 318, F1391–F1399. [Google Scholar] [CrossRef]
- Propert, K.J.; Mayer, R.D.; Wang, Y.; Sant, G.R.; Hanno, P.M.; Peters, K.M.; Kusek, J.W.; Interstitial Cystitis Clinical Trials Group. Responsiveness of symptom scales for interstitial cystitis. Urology 2006, 67, 55–59. [Google Scholar] [CrossRef]
- Yoshimura, N.; Oguchi, T.; Yokoyama, H.; Funahashi, Y.; Yoshikawa, S.; Sugino, Y.; Kawamorita, N.; Kashyap, M.P.; Chancellor, M.B.; Tyagi, P.; et al. Bladder afferent hyperexcitability in bladder pain syndrome/interstitial cystitis. Int. J. Urol. 2014, 21 (Suppl. 1), 18–25. [Google Scholar] [CrossRef]
- Cervigni, M.; Natale, F. Gynecological disorders in bladder pain syndrome/interstitial cystitis patients. Int. J. Urol. 2014, 21 (Suppl. 1), 85–88. [Google Scholar] [CrossRef]
- Bouchelouche, K.; Alvarez, S.; Andersen, L.; Nordling, J.; Horn, T.; Bouchelouche, P. Monocyte chemoattractant protein-1 production by human detrusor smooth muscle cells. J. Urol. 2004, 171, 462–466. [Google Scholar] [CrossRef]
- Tyagi, P.; Killinger, K.; Tyagi, V.; Nirmal, J.; Chancellor, M.; Peters, K.M. Urinary chemokines as noninvasive predictors of ulcerative interstitial cystitis. J. Urol. 2012, 187, 2243–2248. [Google Scholar] [CrossRef] [Green Version]
- Blalock, E.M.; Korrect, G.S.; Stromberg, A.J.; Erickson, D.R. Gene expression analysis of urine sediment: Evaluation for potential noninvasive markers of interstitial cystitis/bladder pain syndrome. J. Urol. 2012, 187, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Spoettl, T.; Hausmann, M.; Herlyn, M.; Gunckel, M.; Dirmeier, A.; Falk, W.; Herfarth, H.; Schoelmerich, J.; Rogler, G. Monocyte chemoattractant protein-1 (MCP-1) inhibits the intestinal-like differentiation of monocytes. Clin. Exp. Immunol. 2006, 145, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Ip, W.K.; Wong, C.K.; Lam, C.W. Interleukin (IL)-4 and IL-13 up-regulate monocyte chemoattractant protein-1 expression in human bronchial epithelial cells: Involvement of p38 mitogen-activated protein kinase, extracellular signal-regulated kinase 1/2 and Janus kinase-2 but not c-Jun NH2-terminal kinase 1/2 signalling pathways. Clin. Exp. Immunol. 2006, 145, 162–172. [Google Scholar] [PubMed]
- Yang, W.; Searl, T.J.; Yaggie, R.; Schaeffer, A.J.; Klumpp, D.J. A MAPP Network study: Overexpression of tumor necrosis factor-alpha in mouse urothelium mimics interstitial cystitis. Am. J. Physiol. Ren. Physiol. 2018, 315, F36–F44. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.Y.; Lu, J.H.; Chuang, S.M.; Chueh, K.S.; Juan, T.J.; Liu, Y.C.; Juan, Y.S. Urinary biomarkers in interstitial cystitis/bladder pain syndrome and its impact on therapeutic outcome. Diagnostics 2021, 12, 75. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.T.; Tyagi, P.; Chancellor, M.B.; Kuo, H.C. Urinary nerve growth factor but not prostaglandin E2 increases in patients with interstitial cystitis/bladder pain syndrome and detrusor overactivity. BJU Int. 2010, 106, 1681–1685. [Google Scholar] [CrossRef]
- Nickel, J.C.; Tripp, D.A.; International Interstitial Cystitis Study Group. Clinical and psychological parameters associated with pain pattern phenotypes in women with interstitial cystitis/bladder pain syndrome. J. Urol. 2015, 193, 138–144. [Google Scholar] [CrossRef]
- Martínez-Martínez, L.A.; Mora, T.; Vargas, A.; Fuentes-Iniestra, M.; Martínez-Lavín, M. Sympathetic nervous system dysfunction in fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, and interstitial cystitis: A review of case-control studies. J. Clin. Rheumatol. 2014, 20, 146–150. [Google Scholar] [CrossRef]
- Warren, J.W.; Morozov, V.; Howard, F.M.; Wesselmann, U.; Gallicchio, L.; Langenberg, P.; Clauw, D.J. Before the onset of interstitial cystitis/bladder pain syndrome, the presence of multiple non-bladder syndromes is strongly associated with a history of multiple surgeries. J. Psychosom. Res. 2014, 76, 75–79. [Google Scholar] [CrossRef]
- Walker, S.J.; Zambon, J.; Andersson, K.E.; Langefeld, C.D.; Matthews, C.A.; Badlani, G.; Bowman, H.; Evans, R.J. Bladder capacity is a biomarker for a bladder centric versus systemic manifestation in interstitial cystitis/bladder pain syndrome. J. Urol. 2017, 198, 369–375. [Google Scholar] [CrossRef]
- Akiyama, Y.; Hanno, P. Phenotyping of interstitial cystitis/bladder pain syndrome. Int. J. Urol. 2019, 26 (Suppl. 1), 17–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Denson, M.A.; Griebling, T.L.; Cohen, M.B.; Kreder, K.J. Comparison of cystoscopic and histological findings in patients with suspected interstitial cystitis. J. Urol. 2000, 164, 1908–1911. [Google Scholar] [CrossRef]
- Schachar, J.S.; Evans, R.J.; Parks, G.E.; Zambon, J.; Badlani, G.; Walker, S.J. Histological evidence supports low anesthetic bladder capacity as a marker of a bladder-centric disease subtype in interstitial cystitis/bladder pain syndrome. Int. Urogynecol. J. 2019, 30, 1863–1870. [Google Scholar] [CrossRef] [PubMed]
- Tyagi, P.; Chen, X.; Hayashi, Y.; Yoshimura, N.; Chancellor, M.B.; de Miguel, F. Proteomic investigation on chronic bladder irritation in the rat. Urology 2008, 71, 536–540. [Google Scholar] [CrossRef] [Green Version]
- Jiang, Y.H.; Peng, C.H.; Liu, H.T.; Kuo, H.C. Increased pro-inflammatory cytokines, C-reactive protein and nerve growth factor expressions in serum of patients with interstitial cystitis/bladder pain syndrome. PLoS ONE 2013, 8, e76779. [Google Scholar] [CrossRef]
- Clemens, J.Q.; Elliott, M.N.; Suttorp, M.; Berry, S.H. Temporal ordering of interstitial cystitis/bladder pain syndrome and non-bladder conditions. Urology 2012, 80, 1227–1231. [Google Scholar] [CrossRef] [Green Version]
| Urine Biomarker | (A) Non-HIC (n = 285) | (B) HIC (n = 24) | (C) Control (n = 30) | p-Value | Post Hoc |
|---|---|---|---|---|---|
| IL-8 | 15.9 ± 23.6 | 34.4 ± 39.7 * | 12.5 ± 21.0 | 0.030 | B vs. A,C |
| CXCL 10 | 10.1 ± 17.4 | 35.1 ± 38.2 * | 13.8 ± 18.4 | 0.005 | B vs. A,C |
| MCP-1 | 299 ± 306 * | 289 ± 239 * | 147 ± 110 | 0.001 | A,B vs. C |
| BDNF | 0.57 ± 0.14 | 0.71 ± 0.30 * | 0.55 ± 0.12 | 0.018 | B vs. A,C |
| Eotaxin | 7.29 ± 7.05 * | 12.0 ± 11.5 * | 4.98 ± 3.7 | 0.017 | A,B vs. C |
| IL-6 | 2.92 ± 6.96 * | 10.8 ± 8.35 | 1.29 ± 1.35 | 0.019 | A vs. C |
| MIP-1β | 1.18 ± 1.60 * | 1.96 ± 2.80 | 2.52 ± 1.82 | 0.009 | A vs. C |
| RANTES | 5.30 ± 7.90 | 10.2 ± 10.1 * | 6.04 ± 5.15 | 0.021 | B vs. AC |
| TNF-α | 1.65 ± 0.35 * | 1.85 ± 0.64 * | 0.82 ± 0.33 | <0.001 | A,B vs. C |
| PGE2 | 291 ± 232 * | 302 ± 335 | 161 ± 105 | 0.037 | A vs. C |
| Non-HIC Biomarkers | (A) Male (n = 45) | (B) Female (n = 240) | (C) Total (n = 285) | (D) Control (n = 30) | p-Value A vs. B | p-Value A vs. B vs. D | Post Hoc |
|---|---|---|---|---|---|---|---|
| IL-8 | 3.87 ± 5.5 | 18.2 ± 25.0 | 15.9 ± 23.6 | 12.5 ± 21.0 | <0.001 | <0.001 | A vs. B |
| CXCL 10 | 6.4 ± 7.49 | 10.8 ± 18.6 | 10.1 ± 17.4 | 13.8± 18.4 | 0.008 | 0.092 | |
| MCP-1 | 303 ± 323 | 298 ± 303 | 299 ± 36.1 | 147 ± 110 | 0.923 | 0.009 | AB vs. D |
| BDNF | 0.58 ± 0.16 | 0.57 ± 0.13 | 0.57 ± 0.14 | 0.55 ± 0.12 | 0.574 | 0.638 | |
| Eotaxin | 8.53 ± 8.32 | 7.06 ± 6.78 | 7.29 ± 7.05 | 4.98 ± 3.70 | 0.200 | 0.070 | |
| IL-6 | 2.32 ± 4.96 | 3.03 ± 7.28 | 2.92 ± 6.96 | 1.29 ± 1.35 | 0.526 | 0.367 | |
| MIP-1β | 0.89 ± 0.96 | 1.23 ± 1.70 | 1.18 ± 1.60 | 2.52 ± 1.82 | 0.189 | <0.001 | AB vs. D |
| RANTES | 5.18 ± 5.72 | 5.33 ± 8.26 | 5.30 ± 7.90 | 6.04 ± 5.15 | 0.909 | 0.880 | |
| TNF-α | 1.58 ± 0.23 | 1.66 ± 0.36 | 1.65 ± 0.35 | 0.82 ± 0.33 | 0.154 | <0.001 | AB vs. D |
| PGE2 | 371 ± 284 | 276 ± 218 | 291 ± 232 | 161 ± 105 | 0.012 | <0.001 | AB vs. D |
| HIC Biomarkers | (A) Male ( n = 3) | (B) Female ( n = 21) | (C) Total ( n = 24) | (D) Control (n = 30) | p-Value A vs. B | p-Value A vs. B vs. D | Post Hoc |
| IL-8 | 16.0 ± 11.0 | 37.3 ± 42.0 | 34.4 ± 39.7 | 12.5 ± 21.0 | 0.523 | 0.007 | B vs. D |
| CXCL 10 | 48.9 ± 59.6 | 33.4 ± 37.3 | 35.1 ± 38.2 | 13.8 ± 18.4 | 0.573 | 0.198 | |
| MCP-1 | 236 ± 244 | 297 ± 243 | 289 ± 239 | 147 ± 110 | 0.742 | 0.132 | |
| BDNF | 0.57 ± 0.05 | 0.73 ± 0.32 | 0.71 ± 0.30 | 0.55 ± 0.12 | 0.145 | 0.003 | B vs. D |
| Eotaxin | 8.64 ± 5.02 | 12.5 ± 12.2 | 12.0 ± 11.5 | 4.98 ± 3.70 | 0.830 | 0.119 | |
| IL-6 | 3.83 ± 2.68 | 11.9 ± 18.5 | 10.8 ± 17.4 | 1.29 ± 1.35 | 1.000 | 0.056 | |
| MIP-1β | 1.08 ± 1.55 | 2.09 ± 2.95 | 1.96 ± 2.80 | 2.52 ± 1.82 | 0.830 | 0.058 | |
| RANTES | 13.5 ± 17.7 | 9.78 ± 9.13 | 10.2 ± 10.1 | 6.04 ± 5.15 | 1.000 | 0.822 | |
| TNF-α | 1.63 ± 0.38 | 1.88 ± 0.67 | 1.85 ± 0.64 | 0.82 ± 0.33 | 0.830 | <0.001 | AB vs. D |
| PGE2 | 465 ± 522 | 277 ± 311 | 302 ± 335 | 162 ± 105 | 0.268 | 0.392 |
| ICSI | ICPI | VAS | MBC | Glomerulation | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pearson | p = | Pearson | p = | Pearson | p = | Pearson | p = | Pearson | p = | |
| IL-8 | 0.045 | 0.505 | 0.004 | 0.948 | −0.042 | 0.542 | −0.092 | 0.111 | 0.031 | 0.586 |
| CXCL 10 | 0.254 | 0.000 | 0.173 | 0.011 | 0.092 | 0.188 | −0.238 | 0.000 | 0.125 | 0.032 |
| MCP-1 | 0.091 | 0.180 | 0.037 | 0.583 | −0.063 | 0.364 | −0.253 | 0.000 | 0.173 | 0.003 |
| BDNF | 0.189 | 0.005 | 0.172 | 0.011 | 0.164 | 0.017 | −0.041 | 0.479 | −0.042 | 0.462 |
| Eotaxin | 0.237 | 0.000 | 0.144 | 0.034 | 0.052 | 0.456 | −0.255 | 0.000 | 0.097 | 0.093 |
| IL-6 | 0.213 | 0.002 | 0.148 | 0.029 | 0.207 | 0.003 | −0.231 | 0.000 | 0.134 | 0.020 |
| MIP-1β | 0.134 | 0.048 | 0.117 | 0.084 | 0.003 | 0.996 | −0.187 | 0.001 | 0.031 | 0.598 |
| RANTES | 0.207 | 0.002 | 0.130 | 0.054 | 0.032 | 0.639 | −0.246 | 0.000 | 0.132 | 0.021 |
| TNF-α | 0.083 | 0.220 | −0.035 | 0.600 | 0.009 | 0.898 | −0.116 | 0.042 | 0.082 | 0.154 |
| PGE2 | −0.029 | 0.668 | −0.004 | 0.955 | −0.169 | 0.015 | −0.154 | 0.007 | 0.148 | 0.010 |
| Urine Biomarker | (A) GR ≤ 1, MBC > 760 (n = 85) | (B) GR ≤ 1 MBC ≤ 760 (n = 70) | (C) GR > 1 MBC > 760 (n = 41) | (D) GR > 1 MBC ≤ 760 (n = 89) | (E) Hunner’s IC (n = 24) | (F) Control (n = 30) | p-Value # | p-Value $ |
|---|---|---|---|---|---|---|---|---|
| IL-8 | 18.7 ± 29.8 | 16.5 ± 23.6 | 7.84 ± 10.3 | 16.5 ± 20.7 | 34.4 ± 39.7 * | 12.5 ± 21.0 | 0.010 | 0.011 |
| CXCL 10 | 6.56 ± 11.6 | 11.3 ± 20.1 | 6.08 ± 12.3 | 14.4 ± 20.5 | 35.1 ± 38.2 * | 13.8 ± 18.4 | <0.001 | <0.001 |
| MCP-1 | 204 ± 173 | 281 ± 276 * | 274 ± 294 | 414 ± 389 * | 289 ± 239 | 147 ± 110 | <0.001 | <0.001 |
| BDNF | 0.57 ± 0.14 | 0.57 ± 0.14 | 0.58 ± 0.11 | 0.55 ± 0.15 | 0.71 ± 0.30 * | 0.55 ± 0.12 | 0.001 | 0.001 |
| Eotaxin | 6.11 ± 6.42 | 7.79 ± 7.14 | 5.48 ± 4.59 | 8.85 ± 8.12 * | 12.0 ± 11.5 * | 4.98 ± 3.7 | 0.002 | 0.008 |
| IL-6 | 1.5 ± 2.25 | 3.47 ± 8.02 | 2.99 ± 10.1 | 3.82 ± 7.2 * | 10.8 ± 8.35 | 1.29 ± 1.35 | 0.008 | 0.017 |
| MIP-1β | 0.9 ± 1.33 * | 1.44 ± 1.97 | 0.8 ± 1 * | 1.41 ± 1.69 | 1.96 ± 2.80 | 2.52 ± 1.82 | 0.001 | 0.058 |
| RANTES | 4.06 ± 9.55 | 5.32 ± 6.54 | 4.1 ± 5.25 | 7.05 ± 7.93 | 10.2 ± 10.1 * | 6.04 ± 5.15 | 0.005 | 0.005 |
| TNF-α | 1.66 ± 0.35 * | 1.62 ± 0.27 * | 1.6 ± 0.34 * | 1.68 ± 0.4 * | 1.85 ± 0.64 * | 0.82 ± 0.33 | <0.001 | 0.219 |
| PGE2 | 251 ± 226 | 284 ± 226 * | 265 ± 190 | 350 ± 252 * | 302 ± 335 * | 161 ± 105 | 0.007 | 0.087 |
| Urine Cytokines | AUC | Cutoff Value | IC/BPS Sensitivity | IC/BPS Specificity | IC/BPS PPV | IC/BPS NPV |
|---|---|---|---|---|---|---|
| IL-8 | 0.587 | 2.100 | 80.6% | 40.0% | 93.3% | 16.7% |
| CXCL 10 | 0.590 | 1.595 | 32.7% | 90.0% | 97.1% | 11.5% |
| MCP-1 | 0.639 | 283.1 | 35.9% | 93.3% | 98.2% | 12.4% |
| BDNF | 0.551 | 0.543 | 57.3% | 66.7% | 94.7% | 13.2% |
| Eotaxin | 0.587 | 12.50 | 21.0% | 96.7% | 98.5% | 10.6% |
| IL-6 | 0.534 | 0.515 | 38.2% | 83.3% | 95.9% | 11.6% |
| MIP-1β | 0.774 | 0.810 | 60.5% | 100% | 100% | 19.7% |
| RANTES | 0.636 | 1.495 | 36.9% | 100% | 100% | 13.3% |
| TNF-α | 0.920 | 1.050 | 99.0% | 92.6% | 98.4% | 89.3% |
| PGE2 | 0.679 | 175.4 | 63.6% | 80.0% | 97.0% | 17.6% |
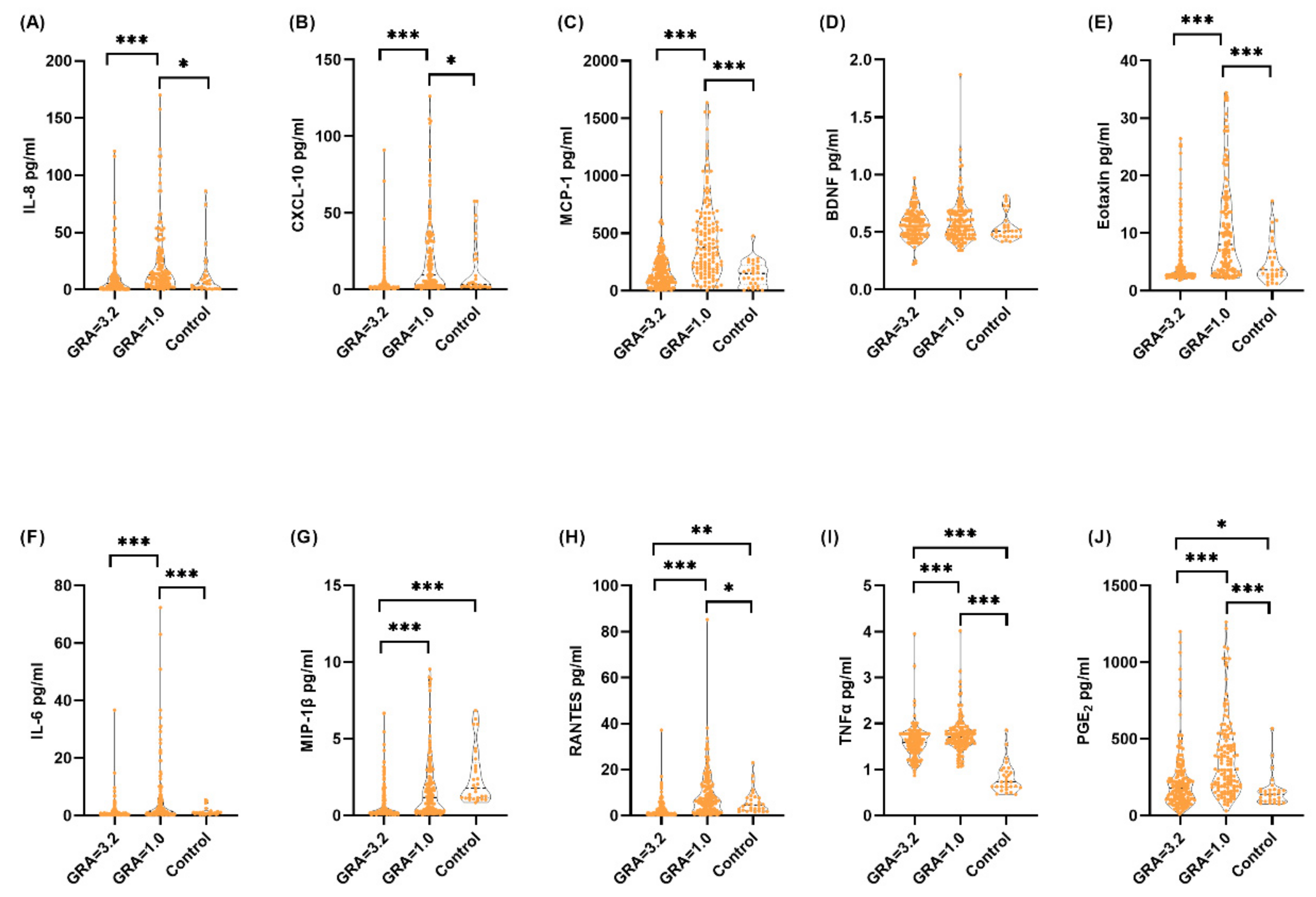
| IC/BPS | ||||||
|---|---|---|---|---|---|---|
| Urine Cytokines | (A) GRA = 3 (n = 58) | (B) GRA = 2 (n = 113) | (C) GRA = 1 (n = 109) | (D) GRA = 0 (n = 29) | p-Value | Post Hoc |
| IL-8 | 9.79 ± 18 | 12.2 ± 17.6 | 22.1 ± 29.5 | 32.2 ± 37.2 | <0.001 | A vs. CD; B vs. C |
| CXCL 10 | 2.68 ± 4.06 * | 6.02 ± 12.5 | 17.9 ± 24.4 | 31.4 ± 28.4 | <0.001 | AB vs. CD |
| MCP-1 | 130 ± 118 | 199 ± 208 | 423 ± 330 * | 589 ± 380 * | <0.001 | A vs. BCD; B vs. CD |
| BDNF | 0.56 ± 0.14 | 0.57 ± 0.12 | 0.59 ± 0.19 | 0.62 ± 0.2 | 0.301 | |
| Eotaxin | 4.09 ± 4.37 | 5.53 ± 5.17 | 10.3 ± 8.75 * | 13.8 ± 9.12 * | <0.001 | AB vs. CD |
| IL-6 | 0.78 ± 1.11 | 1.59 ± 3.93 | 5.08 ± 9.96 * | 10.5 ± 15.4 * | <0.001 | AB vs. CD |
| MIP-1β | 0.5 ± 0.88 * | 0.91 ± 1.27 * | 1.61 ± 2.04 | 2.69 ± 2.21 | <0.001 | AB vs. CD |
| RANTES | 1.89 ± 2.62 * | 3.17 ± 4.4 | 7.34 ± 6.52 | 17.2 ± 16.9 * | <0.001 | AB vs. CD; C vs. D |
| TNF-α | 1.51 ± 0.31 * | 1.63 ± 0.37 * | 1.72 ± 0.39 * | 1.9 ± 0.36 * | <0.001 | A vs. BCD; BC vs. D |
| PGE2 | 171 ± 131 | 252 ± 222 * | 360 ± 248 * | 453 ± 309 * | <0.001 | A vs. BCD; B vs. CD |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, W.-R.; Jiang, Y.-H.; Jhang, J.-F.; Kuo, H.-C. Use of Urinary Cytokine and Chemokine Levels for Identifying Bladder Conditions and Predicting Treatment Outcomes in Patients with Interstitial Cystitis/Bladder Pain Syndrome. Biomedicines 2022, 10, 1149. https://doi.org/10.3390/biomedicines10051149
Yu W-R, Jiang Y-H, Jhang J-F, Kuo H-C. Use of Urinary Cytokine and Chemokine Levels for Identifying Bladder Conditions and Predicting Treatment Outcomes in Patients with Interstitial Cystitis/Bladder Pain Syndrome. Biomedicines. 2022; 10(5):1149. https://doi.org/10.3390/biomedicines10051149
Chicago/Turabian StyleYu, Wan-Ru, Yuan-Hong Jiang, Jia-Fong Jhang, and Hann-Chorng Kuo. 2022. "Use of Urinary Cytokine and Chemokine Levels for Identifying Bladder Conditions and Predicting Treatment Outcomes in Patients with Interstitial Cystitis/Bladder Pain Syndrome" Biomedicines 10, no. 5: 1149. https://doi.org/10.3390/biomedicines10051149
APA StyleYu, W.-R., Jiang, Y.-H., Jhang, J.-F., & Kuo, H.-C. (2022). Use of Urinary Cytokine and Chemokine Levels for Identifying Bladder Conditions and Predicting Treatment Outcomes in Patients with Interstitial Cystitis/Bladder Pain Syndrome. Biomedicines, 10(5), 1149. https://doi.org/10.3390/biomedicines10051149








