Influence of Receptor Polymorphisms on the Response to α-Adrenergic Receptor Blockers in Pheochromocytoma Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Design
2.2. Data Recording and Analysis
2.3. DNA Collection and Genetic Analyses
2.4. Statistical Analyses
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Loyd, R.V.; Osamura, R.Y.; Kloppel, G.; Rosai, J. WHO Classification of Tumours: Pathology and Genetics of Tumours of Endocrine Organ, 4th ed; IARC: Lyon, France, 2017. [Google Scholar]
- Stolk, R.F.; Bakx, C.; Mulder, J.; Timmers, H.J.; Lenders, J.W. Is the excess cardiovascular morbidity in pheochromocytoma related to blood pressure or to catecholamines? J. Clin. Endocrinol. Metab. 2013, 98, 1100–1106. [Google Scholar] [CrossRef] [PubMed]
- Giavarini, A.; Chedid, A.; Bobrie, G.; Plouin, P.F.; Hagege, A.; Amar, L. Acute catecholamine cardiomyopathy in patients with pheaochromocytoma or functinal paraganglioma. Heart 2013, 99, 1438–1444. [Google Scholar] [CrossRef]
- Reister, A.; Weismann, D.; Quinkler, M.; Lichtenauer, U.D.; Sommerey, S.; Halbritter, R.; Penning, R.; Spitzweg, C.; Schopohl, J.; Beuschlein, F.; et al. Life-threatening events in patients with pheochromcytoma. Eur. J. Endocrinol. 2015, 173, 757–764. [Google Scholar] [CrossRef] [PubMed]
- Gu, Y.W.; Poste, J.; Kunal, M.; Schwarcz, M.; Weiss, I. Cardiovascular manifestations of pheochromocytoma. Cardiol. Rev. 2017, 25, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Berends, A.M.A.; Kerstens, M.N.; Lenders, J.W.M.; Timmers, H.J.L.M. Approach to the Patient: Perioperative Management of the Patient with Pheochromocytoma or Sympathetic Paraganglioma. J. Clin. Endocrinol. Metab. 2020, 105, dgaa441. [Google Scholar] [CrossRef] [PubMed]
- Lenders, J.W.M.; Duh, Q.Y.; Eisenhofer, G.; Gimenez-Roqueplo, A.P.; Grebe, S.K.; Murad, M.H.; Naruse, M.; Pacak, K.; Young, W.F.; Endocrine Society. Pheochromocytoma and paraganglioma; an endocrine society clincal practice guideline. J. Clin. Endocrinol. Metab. 2014, 99, 1915–1942. [Google Scholar] [CrossRef]
- Buitenwerf, E.; Osinga, T.E.; Timmers, H.J.L.M.; Lenders, J.W.M.; Feelders, R.A.; Eekhoff, E.M.W.; Haak, H.R.; Corssmit, E.P.M.; Bisschop, P.H.L.T.; Valk, G.D.; et al. Efficacy of α-blockers on hemodynamic control during pheochromocytoma resection: A randomized controlled trial. J. Clin. Endocrinol. Metab. 2020, 105, 2381–2391. [Google Scholar] [CrossRef]
- Price, D.T.; Lefkowitz, R.J.; Caron, M.G.; Berkowitz, D.; Schwinn, D.A. Localization of mRNA for three distinct alpha 1-adrenergic receptor subtypes in human tissues: Implications for human alpha-adrenergic physiology. Mol. Pharmacol. 1994, 45, 171–175. [Google Scholar]
- Rudner, X.L.; Berkowitz, D.E.; Booth, J.V.; Funk, B.L.; Cozart, K.L.; D’Amico, E.B.; El-Moalem, H.; Page, S.O.; Richardson, C.D.; Winters, B.; et al. Subtype specific regulation of human vascular alpha(1)-adrenergic receptors by vessel bed and age. Circulation 1999, 100, 2336–2343. [Google Scholar] [CrossRef]
- Guimarães, S.; Moura, D. Vascular adrenoceptors: An update. Pharmacol. Rev. 2001, 53, 319–356. [Google Scholar]
- Flordellis, C.; Paris, H.; Karabinis, A.; Lymperopoulos, A. Pharmacogenomics of adrenoceptors. Pharmacogenomics 2004, 5, 803–817. [Google Scholar] [CrossRef] [PubMed]
- Docherty, J.R. Subtypes of functional alpha1-adrenoceptor. Cell Mol. Life Sci. 2010, 67, 405–417. [Google Scholar] [CrossRef] [PubMed]
- Giovannitti, J.A., Jr.; Thoms, S.M.; Crawford, J.J. Alpha-2 adrenergic receptor agonists: A review of current clinical applications. Anesth. Prog. 2015, 62, 31–39. [Google Scholar] [CrossRef]
- Docherty, J.R. Subtypes of functional alpha1- and alpha2-adrenoceptors. Eur. J. Pharmacol. 1998, 361, 1–15. [Google Scholar] [CrossRef]
- Flordellis, C.; Manolis, A.; Scheinin, M.; Paris, H. Clinical and pharmacological significance of alpha2-adrenoceptor polymorphisms in cardiovascular diseases. Int. J. Cardiol. 2004, 97, 367–372. [Google Scholar] [CrossRef] [PubMed]
- Small, K.M.; Liggett, S.B. Identification and functional characterization of alpha(2)-adrenoceptor polymorphisms. Trends Pharmacol. Sci. 2001, 22, 471–477. [Google Scholar] [CrossRef]
- Shastry, B.S. SNPs: Impact on gene function and phenotype. Methods Mol. Biol. 2009, 578, 3–22. [Google Scholar]
- Lockette, W.; Ghosh, S.; Farrow, S.; MacKenzie, S.; Baker, S.; Miles, P.; Schork, A.; Cadaret, L. Alpha 2-adrenergic receptor gene polymorphism and hypertension in blacks. Am. J. Hypertens. 1995, 8, 390–394. [Google Scholar] [CrossRef]
- Svetkey, L.P.; Timmons, P.Z.; Emovon, O.; Anderson, N.B.; Preis, L.; Chen, Y.T. Association of hypertension with beta2- and alpha2c10-adrenergic receptor genotype. Hypertension 1996, 27, 1210–1215. [Google Scholar] [CrossRef]
- Freitas, S.R.; Pereira, A.C.; Floriano, M.S.; Mill, J.G.; Krieger, J.E. Association of alpha1a-adrenergic receptor polymorphism and blood pressure phenotypes in the Brazilian population. BMC Cardiovasc. Disord. 2008, 8, 40. [Google Scholar] [CrossRef]
- Sõber, S.; Org, E.; Kepp, K.; Juhanson, P.; Eyheramendy, S.; Gieger, C.; Lichtner, P.; Klopp, N.; Veldre, G.; Viigimaa, M.; et al. Targeting 160 candidate genes for blood pressure regulation with a genome-wide genotyping array. PLoS ONE 2009, 4, e6034. [Google Scholar] [CrossRef] [PubMed]
- Lei, B.; Morris, D.P.; Smith, M.P.; Svetkey, L.P.; Newman, M.F.; Rotter, J.I.; Buchanan, T.A.; Beckstrom-Sternberg, S.M.; Green, E.D.; Schwinn, D.A. Novel human alpha1a-adrenoceptor single nucleotide polymorphisms alter receptor pharmacology and biological function. Naunyn Schmiedeberg’s Arch Pharmacol. 2005, 371, 229–239. [Google Scholar] [CrossRef]
- Buitenwerf, E.; Boekel, M.F.; van der Velde, M.I.; Voogd, M.F.; Kerstens, M.N.; Wietasch, G.J.K.G.; Scheeren, T.W.L. The hemodynamic instability score: Development and internal validation of a new rating method of intra-operative haemodynamic instability. Eur. J. Anaesthesiol. 2019, 36, 290–296. [Google Scholar] [CrossRef] [PubMed]
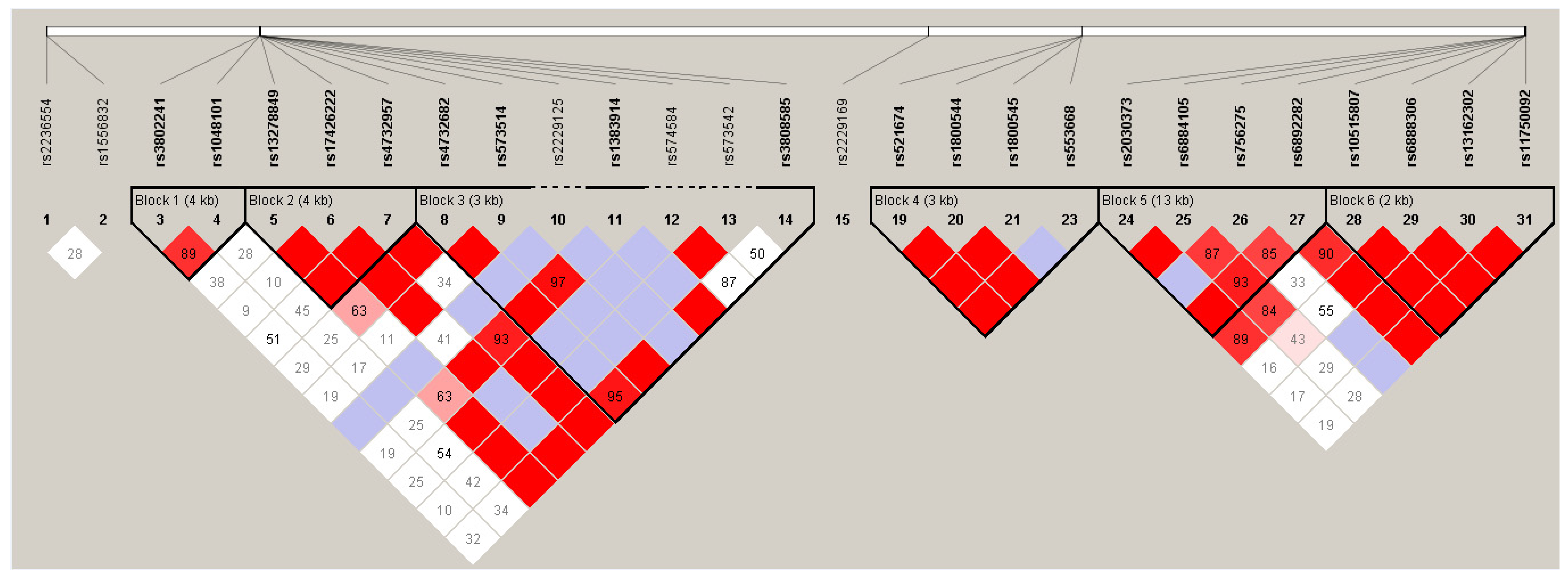
- Gabriel, S.B.; Schaffner, S.F.; Nguyen, H.; Moore, J.M.; Roy, J.; Blumenstiel, B.; Higgins, J.; DeFelice, M.; Lochner, A.; Faggart, M.; et al. The structure of haplotype blocks in the human genome. Science 2002, 296, 2225–2229. [Google Scholar] [CrossRef] [PubMed]
- Barrett, J.C.; Fry, B.; Maller, J.; Daly, M.J. Haploview: Analysis and visualization of LD and haplotype maps. Bioinformatics 2005, 21, 263–265. [Google Scholar] [CrossRef]
- Sinnwell, J.P.; Schaid, D.J. Haplo.Stats: Statistical Analysis of Haplotypes with Traits and Covariates when Linkage Phase is Ambiguous, R Package Version 1.8.6; R Foundation for Statistical Computing: Vienna, Austria, 2020. Available online: https://CRAN.R-project.org/package=haplo.stats (accessed on 3 March 2021).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2017; Available online: https://www.R-project.org (accessed on 3 March 2021).
- Rosskopf, D.; Michel, M.C. Pharmacogenomics of G protein-coupled receptor ligands in cardiovascular medicine. Pharmacol. Rev. 2008, 60, 513–535. [Google Scholar] [CrossRef]
- Kurnik, D.; Muszkat, M.; Li, C.; Sofowora, G.G.; Friedman, E.A.; Scheinin, M.; Wood, A.J.; Stein, C.M. Genetic variations in the α(2A)-adrenoreceptor are associated with blood pressure response to the agonist dexmedetomidine. Circ. Cardiovasc. Genet. 2011, 4, 179–187. [Google Scholar] [CrossRef]
- Büscher, R.; Herrmann, V.; Ring, K.M.; Kailasam, M.T.; O’Connor, D.T.; Parmer, R.J.; Insel, P.A. Variability in phenylephrine response and essential hypertension: A search for human alpha(1B)-adrenergic receptor polymorphisms. J. Pharmacol. Exp. Ther. 1999, 291, 793–798. [Google Scholar]
- Morrow, A.L.; Creese, I. Characterization of alpha 1-adrenergic receptor subtypes in rat brain: A reevaluation of [3H]WB4104 and [3H]prazosin binding. Mol. Pharmacol. 1986, 29, 321–330. [Google Scholar]
- Adefurin, A.; Ghimire, L.V.; Kohli, U.; Muszkat, M.; Sofowora, G.G.; Li, C.; Levinson, R.T.; Paranjape, S.Y.; Stein, C.M.; Kurnik, D. Genetic variation in the alpha1B-adrenergic receptor and vascular response. Pharm. J. 2017, 17, 366–371. [Google Scholar] [CrossRef]
- Kobilka, B.K.; Matsui, H.; Kobilka, T.S.; Yang-Feng, T.L.; Francke, U.; Caron, M.G.; Lefkowitz, R.J.; Regan, J.W. Cloning, sequencing, and expression of the gene coding for the human platelet alpha 2-adrenergic receptor. Science 1987, 238, 650–656. [Google Scholar] [CrossRef] [PubMed]
- Altman, J.D.; Trendelenburg, A.U.; MacMillan, L.; Bernstein, D.; Limbird, L.; Starke, K.; Kobilka, B.K.; Hein, L. Abnormal regulation of the sympathetic nervous system in alpha2A-adrenergic receptor knockout mice. Mol. Pharmacol. 1999, 56, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Nunes, R.A.; Barroso, L.P.; Pereira Ada, C.; Krieger, J.E.; Mansur, A.J. Gender-related associations of genetic polymorphisms of α-adrenergic receptors, endothelial nitric oxide synthase and bradykinin B2 receptor with treadmill exercise test responses. Open Heart 2014, 1, e000132. [Google Scholar] [CrossRef]
- Small, K.M.; Brown, K.M.; Seman, C.A.; Theiss, C.T.; Liggett, S.B. Complex haplotypes derived from noncoding polymorphisms of the intronless alpha2A-adrenergic gene diversify receptor expression. Proc. Natl. Acad. Sci. USA 2006, 103, 5472–5477. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, M.I.; Abecasis, G.R.; Cardon, L.R.; Goldstein, D.B.; Little, J.; Ioannidis, J.P.; Hirschhorn, J.N. Genome-wide association studies for complex traits: Consensus, uncertainty and challenges. Nat. Rev. Genet. 2008, 9, 356–369. [Google Scholar] [CrossRef] [PubMed]
- Burton, P.; Clayton, D.; Cardon, L.; Craddock, N.; Duncanson, A.; Kwiatkowski, D.; McCarthy, M.; Ouwehand, W.; Samani, N.; Todd, J.; et al. Association scan of 14,500 nonsynonymous SNPs in four diseases identifies autoimmunity variants. Nat. Genet. 2007, 39, 1329–1337. [Google Scholar]
- Herlyn, P.; Müller-Hilke, B.; Wendt, M.; Hecker, M.; Mittlmeier, T.; Gradl, G. Frequencies of polymorphisms in cytokines, neurotransmitters and adrenergic receptors in patients with complex regional pain syndrome type I after distal radial fracture. Clin J Pain. 2010, 26, 175–181. [Google Scholar] [CrossRef]
- Kelsey, R.M.; Alpert, B.S.; Dahmer, M.K.; Krushkal, J.; Quasney, M.W. Alpha-adrenergic receptor gene polymorphisms and cardiovascular reactivity to stress in Black adolescents and young adults. Psychophysiology 2012, 49, 401–412. [Google Scholar] [CrossRef]
- Shorter, D.; Nielsen, D.A.; Huang, W.; Harding, M.J.; Hamon, S.C.; Kosten, T.R. Pharmacogenetic randomized trial for cocaine abuse: Disulfiram and α1A-adrenoceptor gene variation. Eur. Neuropsychopharmacol. 2013, 23, 1401–1407. [Google Scholar] [CrossRef]
- Wei, W.Q.; Feng, Q.; Weeke, P.; Bush, W.; Waitara, M.S.; Iwuchukwu, O.F.; Roden, D.M.; Wilke, R.A.; Stein, C.M.; Denny, J.C. Creation and Validation of an EMR-based Algorithm for Identifying Major Adverse Cardiac Events while on Statins. AMIA Jt Summits Transl. Sci. Proc. 2014, 2014, 112–119. [Google Scholar] [PubMed]
- Adefurin, A.; Ghimire, L.V.; Kohli, U.; Muszkat, M.; Sofowora, G.G.; Li, C.; Paranjape, S.Y.; Stein, C.M.; Kurnik, D. Genetic variation in the α1A-adrenergic receptor and phenylephrine-mediated venoconstriction. Pharm. J. 2015, 15, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Shorter, D.; Nielsen, D.A.; Hamon, S.C.; Nielsen, E.M.; Kosten, T.R.; Newton, T.F.; De La Garza, R., 2nd. The α-1 adrenoceptor (ADRA1A) genotype moderates the magnitude of acute cocaine-induced subjective effects in cocaine-dependent individuals. Pharm. Genom. 2016, 26, 428–435. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Amorim Belo Nunes, R.; Pereira Barroso, L.; da Costa Pereira, A.; Pinto Brandão Rondon, M.U.; Negrão, C.E.; Krieger, J.E.; Mansur, A.J. Alpha2A-adrenergic receptor and eNOS genetic polymorphisms are associated with exercise muscle vasodilatation in apparently healthy individuals. Int. J. Cardiol. Heart. Vasc. 2016, 13, 14–18. [Google Scholar] [CrossRef]
- Han, J.; Zuo, J.; Zhu, D.; Gao, C. The correlation between SNPs within the gene of adrenergic receptor and neuropeptide Y and risk of cervical vertigo. J. Clin. Lab. Anal. 2018, 32, e22366. [Google Scholar] [CrossRef] [PubMed]
- Márquez, M.F.; Fragoso, J.M.; Pérez-Pérez, D.; Cázares-Campos, I.; Totomoch-Serra, A.; Gómez-Flores, J.R.; Vargas-Alarcón, G. Polymorphisms in β-adrenergic receptors are associated with increased risk to have a positive head-up tilt table test in patients with vasovagal syncope. Rev. Invest. Clin. 2019, 71, 124–132. [Google Scholar] [CrossRef]
- Elia, J.; Capasso, M.; Zaheer, Z.; Lantieri, F.; Ambrosini, P.; Berrettini, W.; Devoto, M.; Hakonarson, H. Candidate gene analysis in an on-going genome-wide association study of attention-deficit hyperactivity disorder: Suggestive association signals in ADRA1A. Psychiatr. Genet. 2009, 19, 134–141. [Google Scholar] [CrossRef]
- Zhang, X.; Norton, J.; Carrière, I.; Ritchie, K.; Chaudieu, I.; Ryan, J.; Ancelin, M.L. Preliminary evidence for a role of the adrenergic nervous system in generalized anxiety disorder. Sci. Rep. 2017, 7, 42676. [Google Scholar] [CrossRef]
- Sun, Y.X.; Liao, Y.H.; Zhu, F.; Wang, M.; Chen, X.; Chen, F.; Cao, A.L.; Wang, J. Association between ADRA1A gene polymorphism and autoantibodies against the alpha1-adrenergic receptor in hypertensive patients. Zhonghua Xin Xue Guan Bing Za Zhi 2008, 36, 883–887. (In Chinese) [Google Scholar]
- Mathias, R.A.; Grant, A.V.; Rafaels, N.; Hand, T.; Gao, L.; Vergara, C.; Tsai, Y.J.; Yang, M.; Campbell, M.; Foster, C.; et al. A genome-wide association study on African-ancestry populations for asthma. J. Allergy. Clin. Immunol. 2010, 125, 336–346.e4. [Google Scholar] [CrossRef]
- Hawi, Z.; Matthews, N.; Barry, E. Kirley A, Wagner J, Wallace RH, Heussler HS, Vance A, Gill M, Bellgrove MA; l. A high density linkage disequilibrium mapping in 14 noradrenergic genes: Evidence of association between SLC6A2, ADRA1B and ADHD. Psychopharmacol. 2013, 225, 895–902. [Google Scholar] [CrossRef] [PubMed]
- Orand, A.; Gupta, A.; Shih, W.; Presson, A.P.; Hammer, C.; Niesler, B.; Heendeniya, N.; Mayer, E.A.; Chang, L. Catecholaminergic Gene Polymorphisms Are Associated with GI Symptoms and Morphological Brain Changes in Irritable Bowel Syndrome. PLoS ONE 2015, 10, e0135910. [Google Scholar] [CrossRef] [PubMed]
- Parkman, H.P.; Mishra, A.; Jacobs, M.; Pathikonda, M.; Sachdeva, P.; Gaughan, J.; Krynetskiy, E. Clinical response and side effects of metoclopramide: Associations with clinical, demographic, and pharmacogenetic parameters. J. Clin. Gastroenterol. 2012, 46, 494–503. [Google Scholar] [CrossRef] [PubMed]
- Shorter, D.I.; Zhang, X.; Domingo, C.B.; Nielsen, E.M.; Kosten, T.R.; Nielsen, D.A. Doxazosin treatment in cocaine use disorder: Pharmacogenetic response based on an alpha-1 adrenoreceptor subtype D genetic variant. Am. J. Drug Alcohol Abuse 2020, 46, 184–193. [Google Scholar] [CrossRef]
- Lima, J.J.; Feng, H.; Duckworth, L.; Wang, J.; Sylvester, J.E.; Kissoon, N.; Garg, H. Association analyses of adrenergic receptor polymorphisms with obesity and metabolic alterations. Metabolism 2007, 56, 757–765. [Google Scholar] [CrossRef][Green Version]
- Sickert, L.; Müller, D.J.; Tiwari, A.K.; Shaikh, S.; Zai, C.; De Souza, R.; De Luca, V.; Meltzer, H.Y.; Lieberman, J.A.; Kennedy, J.L. Association of the alpha 2A adrenergic receptor -1291C/G polymorphism and antipsychotic-induced weight gain in European-Americans. Pharmacogenomics 2009, 10, 1169–1176. [Google Scholar] [CrossRef]
- de Cerqueira, C.C.; Polina, E.R.; Contini, V.; Marques, F.Z.; Grevet, E.H.; Salgado, C.A.; da Silva, P.O.; Picon, F.A.; Belmonte-de-Abreu, P.; Bau, C.H. ADRA2A polymorphisms and ADHD in adults: Possible mediating effect of personality. Psychiatry Res. 2011, 186, 345–350. [Google Scholar] [CrossRef]
- Yang, L.; Qian, Q.; Liu, L.; Li, H.; Faraone, S.V.; Wang, Y. Adrenergic neurotransmitter system transporter and receptor genes associated with atomoxetine response in attention-deficit hyperactivity disorder children. J. Neural Transm. 2013, 120, 1127–1133. [Google Scholar] [CrossRef]
- Lochman, J.; Balcar, V.J.; Sťastný, F.; Serý, O. Preliminary evidence for association between schizophrenia and polymorphisms in the regulatory Regions of the ADRA2A, DRD3 and SNAP-25 Genes. Psychiatry Res. 2013, 205, 7–12. [Google Scholar] [CrossRef]
- Rubin, D.H.; Althoff, R.R.; Ehli, E.A.; Davies, G.E.; Rettew, D.C.; Crehan, E.T.; Walkup, J.T.; Hudziak, J.J. Candidate gene associations with withdrawn behavior. J. Child Psychol Psychiatry 2013, 54, 1337–1345. [Google Scholar] [CrossRef]
- McCracken, J.T.; Badashova, K.K.; Posey, D.J.; Aman, M.G.; Scahill, L.; Tierney, E.; Arnold, L.E.; Vitiello, B.; Whelan, F.; Chuang, S.Z.; et al. Positive effects of methylphenidate on hyperactivity are moderated by monoaminergic gene variants in children with autism spectrum disorders. Pharm. J. 2014, 14, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Cummins, T.D.; Jacoby, O.; Hawi, Z.; Nandam, L.S.; Byrne, M.A.; Kim, B.N.; Wagner, J.; Chambers, C.D.; Bellgrove, M.A. Alpha-2A adrenergic receptor gene variants are associated with increased intra-individual variability in response time. Mol. Psychiatry 2014, 19, 1031–1036. [Google Scholar] [CrossRef]
- Kochetova, O.V.; Viktorova, T.V.; Mustafina, O.E.; Karpov, A.A.; Khusnutdinova, E.K. Genetic Association of ADRA2A and ADRB3 Genes with Metabolic Syndrome among the Tatars. Genetika 2015, 51, 830–834. [Google Scholar] [CrossRef] [PubMed]
- Kaabi, B.; Belaaloui, G.; Benbrahim, W.; Hamizi, K.; Sadelaoud, M.; Toumi, W.; Bounecer, H. ADRA2A Germline Gene Polymorphism is Associated to the Severity, but not to the Risk, of Breast Cancer. Pathol. Oncol. Res. 2016, 22, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Sanchez, C.I.; Riveiro-Alvarez, R.; Soto-Insuga, V.; Rodrigo, M.; Tirado-Requero, P.; Mahillo-Fernandez, I.; Abad-Santos, F.; Carballo, J.J.; Dal-Ré, R.; Ayuso, C. Attention deficit hyperactivity disorder: Genetic association study in a cohort of Spanish children. Behav. Brain Funct. 2016, 12, 2. [Google Scholar] [CrossRef]
- Hegvik, T.A.; Jacobsen, K.K.; Fredriksen, M.; Zayats, T.; Haavik, J. A candidate gene investigation of methylphenidate response in adult attention-deficit/hyperactivity disorder patients: Results from a naturalistic study. J. Neural Transm. 2016, 123, 859–865. [Google Scholar] [CrossRef]
- Adefurin, A.; Darghosian, L.; Okafor, C.; Kawai, V.; Li, C.; Shah, A.; Wei, W.Q.; Kurnik, D.; Stein, C.M. Alpha2A adrenergic receptor genetic variation contributes to hyperglycemia after myocardial infarction. Int. J. Cardiol. 2016, 215, 482–486. [Google Scholar] [CrossRef]
- Havranek, M.M.; Hulka, L.M.; Tasiudi, E.; Eisenegger, C.; Vonmoos, M.; Preller, K.H.; Mössner, R.; Baumgartner, M.R.; Seifritz, E.; Grünblatt, E.; et al. α2A-Adrenergic receptor polymorphisms and mRNA expression levels are associated with delay discounting in cocaine users. Addict. Biol. 2017, 22, 561–569. [Google Scholar] [CrossRef]
- Myer, N.M.; Boland, J.R.; Faraone, S.V. Pharmacogenetics predictors of methylphenidate efficacy in childhood ADHD. Mol. Psychiatry 2018, 23, 1929–1936. [Google Scholar] [CrossRef]
- Sokol, J.; Skerenova, M.; Ivankova, J.; Simurda, T.; Stasko, J. Association of Genetic Variability in Selected Genes in Patients With Deep Vein Thrombosis and Platelet Hyperaggregability. Clin. Appl. Thromb. Hemost. 2018, 24, 1027–1032. [Google Scholar] [CrossRef]
- Papathanasopoulos, A.; Camilleri, M.; Carlson, P.J.; Vella, A.; Nord, S.J.; Burton, D.D.; Odunsi, S.T.; Zinsmeister, A.R. A preliminary candidate genotype-intermediate phenotype study of satiation and gastric motor function in obesity. Obesity 2010, 18, 1201–1211. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.C.; Kim, J.W.; Kim, H.W.; Kim, B.N.; Shin, M.S.; Cho, D.Y.; Jung, S.W.; Chung, U.S.; Son, J.W. Effect of ADRA2A and BDNF gene-gene interaction on the continuous performance test phenotype. Psychiatr Genet. 2011, 21, 132–135. [Google Scholar] [CrossRef] [PubMed]
- Talmud, P.J.; Cooper, J.A.; Gaunt, T.; Holmes, M.V.; Shah, S.; Palmen, J.; Drenos, F.; Shah, T.; Kumari, M.; Kivimaki, M.; et al. Variants of ADRA2A are associated with fasting glucose, blood pressure, body mass index and type 2 diabetes risk: Meta-analysis of four prospective studies. Diabetologia 2011, 54, 1710–1719. [Google Scholar] [CrossRef] [PubMed]
- Bo, S.; Cassader, M.; Cavallo-Perin, P.; Durazzo, M.; Rosato, R.; Gambino, R. The rs553668 polymorphism of the ADRA2A gene predicts the worsening of fasting glucose values in a cohort of subjects without diabetes. A population-based study. Diabet. Med. 2012, 29, 549–552. [Google Scholar] [CrossRef]
- Li, T.; Zhu, X.; Wu, X.; Li, J.; Pan, L.; Li, P.; Xin, Z.; Gu, H.F.; Liu, Y. Evaluation of the association between the ADRA2A genetic polymorphisms and type 2 diabetes in a Chinese Han population. Genet. Test. Mol. Biomark. 2012, 16, 1424–1427. [Google Scholar] [CrossRef]
- Mlakar, V.; Jurkovic Mlakar, S.; Zupan, J.; Komadina, R.; Prezelj, J.; Marc, J. ADRA2A is involved in neuro-endocrine regulation of bone resorption. J. Cell. Mol. Med. 2015, 19, 1520–1529. [Google Scholar] [CrossRef]
- Nunes, R.A.; Lima, L.B.; Tanaka, N.I.; da Costa Pereira, A.; Krieger, J.E.; Mansur, A.J. Genetic associations of bradykinin type 2 receptor, alpha-adrenoceptors and endothelial nitric oxide synthase with blood pressure and left ventricular mass in outpatients without overt heart disease. Int. J. Cardiol. Heart Vasc. 2018, 21, 45–49. [Google Scholar] [CrossRef]
- Xu, D.; Liu, L.; Li, H.; Sun, L.; Yang, L.; Qian, Q.; Wang, Y. Potential Role of ADRA2A Genetic Variants in the Etiology of ADHD Comorbid With Tic Disorders. J. Atten. Disord. 2021, 25, 33–43. [Google Scholar] [CrossRef]
- Leońska-Duniec, A.; Jastrzębski, Z.; Jażdżewska, A.; Moska, W.; Lulińska-Kuklik, E.; Sawczuk, M.; Gubaydullina, S.I.; Shakirova, A.T.; Cięszczyk, P.; Maszczyk, A.; et al. Individual Responsiveness to Exercise-Induced Fat Loss and Improvement of Metabolic Profile in Young Women is Associated with Polymorphisms of Adrenergic Receptor Genes. J. Sports Sci. Med. 2018, 17, 134–144. [Google Scholar]
- Totomoch-Serra, A.; de Lourdes Muñoz, M.; Burgueño, J.; Revilla-Monsalve, M.C.; Perez-Muñoz, A.; Diaz-Badillo, Á. The ADRA2A rs553668 variant is associated with type 2 diabetes and five variants were associated at nominal significance levels in a population-based case-control study from Mexico City. Gene 2018, 669, 28–34. [Google Scholar] [CrossRef]
- Mărginean, C.O.; Mărginean, C.; Bănescu, C.; Meliţ, L.E.; Tripon, F.; Iancu, M. The relationship between MMP9 and ADRA2A gene polymorphisms and mothers-newborns’ nutritional status: An exploratory path model (STROBE compliant article). Pediatr. Res. 2019, 85, 822–829. [Google Scholar] [CrossRef] [PubMed]
- Perroud, N.; Aitchison, K.J.; Uher, R.; Smith, R.; Huezo-Diaz, P.; Marusic, A.; Maier, W.; Mors, O.; Placentino, A.; Henigsberg, N.; et al. Genetic predictors of increase in suicidal ideation during antidepressant treatment in the GENDEP project. Neuropsychopharmacol. 2009, 34, 2517–2528. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Tang, X.F.; Yao, Y.; He, C.; Xu, J.J.; Wang, H.H.; Gao, Z.; Wang, M.; Yuan, J.Q. Association of α2A-Adrenergic Receptor Genetic Variants with Platelet Reactivity in Chinese Patients on Dual Antiplatelet Therapy Undergoing Percutaneous Coronary Intervention. Biomed. Environ. Sci. 2017, 30, 898–906. [Google Scholar] [PubMed]
- Clarke, T.K.; Dempster, E.; Docherty, S.J. Desrivieres S, Lourdsamy A, Wodarz N, Ridinger M, Maier W, Rietschel M, Schumann G. Multiple polymorphisms in genes of the adrenergic stress system confer vulnerability to alcohol abuse. Addict. Biol. 2012, 17, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Hiltunen, T.P.; Donner, K.M.; Sarin, A.P.; Saarela, J.; Ripatti, S.; Chapman, A.B.; Gums, J.G.; Gong, Y.; Cooper-DeHoff, R.M.; Frau, F.; et al. Pharmacogenomics of hypertension: A genome-wide, placebo-controlled cross-over study, using four classes of antihypertensive drugs. J. Am. Heart Assoc. 2015, 4, e001521. [Google Scholar] [CrossRef] [PubMed]
- Muszkat, M.; Kurnik, D.; Sofowora, G.G.; Solus, J.; Xie, H.G.; Harris, P.A.; Williams, S.M.; Wood, A.J.; Stein, C.M. Desensitization of vascular response in vivo: Contribution of genetic variation in the [alpha]2B-adrenergic receptor subtype. J. Hypertens. 2010, 28, 278–284. [Google Scholar] [CrossRef]
- De Fusco, M.; Vago, R.; Striano, P.; Di Bonaventura, C.; Zara, F.; Mei, D.; Kim, M.S.; Muallem, S.; Chen, Y.; Wang, Q.; et al. The α2B-adrenergic receptor is mutant in cortical myoclonus and epilepsy. Ann. Neurol. 2014, 75, 77–87. [Google Scholar] [CrossRef]
| All Subjects (n = 116) | |
|---|---|
| Demographics | |
| Male sex—number (%) | 51 (44) |
| Ethnicity | |
| European (%) | 108 (93) |
| Asian (%) | 3 (3) |
| African (%) | 2 (1.5) |
| Latin American (%) | 2 (1.5) |
| Arab (%) | 1 (1) |
| Age (years) | 55 ± 15.1 |
| BMI (kg/m2) | 25.9 ± 4.8 |
| Serum creatinine (μmol/L) | 76.1 ± 21.7 |
| Tumor characteristics | |
| Pheochromocytoma—number (%) | 109 (94.0) |
| sPGL—number (%) | 7 (6.0) |
| Germline mutations—number (%) | 23 (19.8) |
| Tumor size (mm) | 53.63 (17.50–160.00) |
| Total plasma catecholamines (n < 5.28 nmol/L) | 6.01 (3.53–17.26) |
| Surgical approach | |
| Laparoscopy—number (%) | 82 (70.7) |
| Laparotomy—number (%) | 20 (17.2) |
| Posterior retroperitoneoscopic—number (%) | 14 (12.1) |
| Pretreatment | |
| Doxazosin/Phenoxybenzamine—number (%) | 59 (51)/57 (49) |
| 4/10 mg | 3 (2.6) |
| 8/20 mg | 5 (4.3) |
| 12/40 mg | 5 (4.3) |
| 16/60 mg | 9 (7.8) |
| 20/70 mg | 2 (1.7) |
| 24/80 mg | 6 (5.2) |
| 28/90 mg | 1 (0.9) |
| 32/100 mg | 19 (16.4) |
| 36/110 mg | 2 (1.7) |
| 40/120 mg | 14 (12.1) |
| 48/140 mg | 50 (43.1) |
| Total number of side effects | 2.0 (1.0–3.0) |
| Presurgical hemodynamics | |
| Supine SBP preoperative (mmHg) * | 127.7 ± 19.1 |
| Upright SBP preoperative (mmHg) * | 118.2 ± 19.3 |
| Heart rate baseline (bpm) | 73.0 ± 12.0 |
| Intraoperative hemodynamics | |
| Hemodynamic instability score | 43.5 (30.3–59.0) |
| Time outside BP range (%) | 10.0 (4.3–19.8) |
| Outcome | Covariate | Beta | SE | Univariate p-Value | Multivariate p-Value |
|---|---|---|---|---|---|
| Dose of α-adrenergic receptor blockers | Age | 0.046 | 0.013 | 0.00092 | 0.094 |
| Sex (female) | −0.77 | 0.38 | 0.044 | 0.025 | |
| BMI | 0.19 | 0.053 | 0.00059 | 0.011 | |
| SBP baseline (supine) | 0.047 | 0.0106 | 0.000029 | 0.0013 | |
| Number of antihypertensive comedication day -1 (baseline) | 0.92 | 0.28 | 0.0014 | 0.069 | |
| Serum creatinine | 0.0057 | 0.0086 | 0.50 | n.a. | |
| Tumor size | −0.00024 | 0.00063 | 0.70 | n.a. | |
| Catecholamines | 0.0087 | 0.0109 | 0.43 | n.a. | |
| Randomization | −0.089 | 0.36 | 0.80 | n.a. | |
| Number of side effects | Age | −0.003 | 0.011 | 0.78 | n.a. |
| Sex (female) | 0.33 | 0.33 | 0.32 | n.a. | |
| BMI | −0.066 | 0.034 | 0.06 | 0.045 | |
| SBP baseline (supine) | 0.004 | 0.007 | 0.55 | n.a. | |
| Number of antihypertensive comedication day -1 (baseline) | 0.39 | 0.22 | 0.07 | 0.16 | |
| Serum creatinine | −0.003 | 0.008 | 0.74 | n.a. | |
| Tumor size | −0.0003 | 0.0006 | 0.61 | n.a. | |
| Catecholamines | 0.012 | 0.009 | 0.17 | 0.38 | |
| Randomization | −0.43 | 0.33 | 0.20 | 0.29 | |
| Dose of α-adrenergic receptor blockers | 0.15 | 0.24 | 0.53 | n.a. | |
| Hemodynamic instability score | Age | 0.23 | 0.14 | 0.11 | 0.22 |
| Sex (female) | −1.39 | 4.32 | 0.75 | n.a. | |
| BMI | −0.69 | 0.45 | 0.13 | 0.15 | |
| SBP baseline (supine) | 0.21 | 0.09 | 0.018 | 0.11 | |
| Number of antihypertensive comedication day -1 (baseline) | 1.76 | 2.70 | 0.52 | n.a. | |
| Serum creatinine | −0.10 | 0.10 | 0.30 | n.a. | |
| Tumor size | 0.011 | 0.007 | 0.11 | 0.40 | |
| Catecholamines | 0.36 | 0.12 | 0.0032 | 0.15 | |
| Randomization | 9.63 | 4.20 | 0.024 | 0.026 | |
| Cumulative intraoperative time outside the blood pressure target range | Age | −0.013 | 0.62 | 0.25 | n.a. |
| Sex (female) | −0.28 | 0.33 | 0.40 | n.a. | |
| BMI | −0.038 | 0.035 | 0.28 | n.a. | |
| SBP baseline (supine) | 0.003 | 0.007 | 0.67 | n.a. | |
| Number of antihypertensive comedication day -1 (baseline) | 0.23 | 0.21 | 0.28 | n.a. | |
| Serum creatinine | −0.0027 | 0.0076 | 0.73 | n.a. | |
| Tumor size | 0.00054 | 0.00056 | 0.34 | n.a. | |
| Catecholamines | 0.02 | 0.0093 | 0.031 | 0.031 | |
| Randomization | 0.063 | 4.12 | 0.33 | n.a. |
| Dose of α-Adrenergic Receptor Blockers | Number of Side Effects | Hemodynamic Instability Score | Cumulative Intraoperative Time Outside the Blood Pressure Target Range | ||||||
|---|---|---|---|---|---|---|---|---|---|
| SNP-Allele | AF | OR (SE) | p-Value | OR (SE) | p-Value | Beta (SE) | p-Value | Beta (SE) | p-Value |
| rs2229169-T | 0.328 | 0.73 (0.37) | 0.39 | 0.98 (0.27) | 0.95 | 0.36 (3.31) | 0.91 | −0.04 (0.26) | 0.87 |
| rs2030373-C | 0.778 | 0.52 (0.46) | 0.17 | 0.58 (0.37) | 0.14 | 0.58 (4.17) | 0.89 | 0.02 (0.33) | 0.96 |
| rs6884105-G | 0.644 | 0.67 (0.40) | 0.31 | 0.95 (0.28) | 0.85 | 0.49 (3.29) | 0.88 | 0.06 (0.26) | 0.82 |
| rs756275-T | 0.073 | 0.70 (0.67) | 0.59 | 1.01 (0.54) | 0.98 | 3.18 (5.97) | 0.60 | −0.13 (0.46) | 0.78 |
| rs6892282-T | 0.440 | 1.35 (0.35) | 0.39 | 1.58 (0.27) | 0.10 | −3.53 (3.39) | 0.30 | −0.50 (0.25) | 0.05 |
| rs10515807-G | 0.862 | 0.31 (0.58) | 0.047 * | 0.27 (0.46) | 0.005 * | −2.18 (5.09) | 0.67 | 0.26 (0.38) | 0.50 |
| rs6888306-T | 0.248 | 0.89 (0.38) | 0.77 | 1.23 (0.32) | 0.52 | −4.67 (3.77) | 0.22 | −0.28 (0.28) | 0.32 |
| rs13162302-G | 0.196 | 1.03 (0.40) | 0.94 | 1.27 (0.33) | 0.47 | −6.79 (4.02) | 0.10 | −0.43 (0.30) | 0.15 |
| rs11750092-T | 0.192 | 1.20 (0.40) | 0.66 | 1.36 (0.33) | 0.36 | −7.56 (4.02) | 0.06 | −0.46 (0.30) | 0.15 |
| rs3802241-G | 0.545 | 1.28 (0.35) | 0.48 | 1.19 (0.26) | 0.51 | −0.33 (3.31) | 0.92 | 0.08 (0.23) | 0.72 |
| rs1048101-T | 0.539 | 1.43 (0.31) | 0.26 | 0.99 (0.24) | 0.96 | −2.16 (3.00) | 0.47 | −0.16 (0.23) | 0.48 |
| rs13278849-G | 0.263 | 0.92 (0.34) | 0.80 | 1.12 (0.28) | 0.68 | −0.08 (3.38) | 0.98 | −0.18 (0.27) | 0.51 |
| rs17426222-T | 0.286 | 2.04 (0.45) | 0.12 | 1.16 (0.32) | 0.64 | −1.72 (4.00) | 0.67 | 0.18 (0.30) | 0.56 |
| rs4732957-C | 0.784 | 1.50 (0.42) | 0.34 | 1.06 (0.34) | 0.87 | 1.17 (4.19) | 0.78 | 0.31 (0.32) | 0.35 |
| rs4732682-T | 0.458 | 0.78 (0.37) | 0.50 | 0.95 (0.27) | 0.86 | 1.27 (3.33) | 0.71 | 0.03 (0.26) | 0.91 |
| rs573514-G | 0.446 | 1.92 (0.37) | 0.09 | 1.04 (0.28) | 0.90 | −2.77 (3.30) | 0.40 | 0.16 (0.25) | 0.52 |
| rs1383914-T | 0.530 | 1.41 (0.32) | 0.29 | 1.21 (0.24) | 0.43 | −2.64 (3.00) | 0.38 | −0.02 (0.23) | 0.95 |
| rs3808585-T | 0.250 | 0.74 (0.40) | 0.46 | 1.31 (0.29) | 0.36 | 2.34 (3.59) | 0.52 | −0.04 (0.29) | 0.89 |
| rs521674-T | 0.260 | 3.30 (0.48) | 0.014 * | 1.04 (0.32) | 0.91 | 1.41 (4.04) | 0.73 | −0.08 (0.31) | 0.80 |
| rs1800544-G | 0.254 | 2.01 (0.38) | 0.07 | 1.23 (0.29) | 0.48 | −0.11 (3.57) | 0.98 | −0.02 (0.28) | 0.95 |
| rs1800545-A | 0.103 | 1.34 (0.56) | 0.60 | 0.87 (0.43) | 0.75 | 4.92 (5.43) | 0.37 | 0.40 (0.41) | 0.34 |
| rs553668-G | 0.859 | 0.26 (0.59) | 0.024 * | 0.72 (0.38) | 0.39 | 1.12 (4.66) | 0.81 | 0.27 (0.35) | 0.44 |
| rs2236554-T | 0.643 | 0.85 (0.40) | 0.69 | 1.11 (0.31) | 0.73 | −5.24 (4.06) | 0.20 | −0.34 (0.30) | 0.27 |
| rs1556832-T | 0.505 | 0.63 (0.36) | 0.20 | 0.87 (0.25) | 0.58 | −4.75 (3.15) | 0.14 | −0.18 (0.24) | 0.46 |
| Dose of α-Adrenergic Receptor Blockers | Number of Side Effects | Hemodynamic Instability Score | Cumulative Intraoperative Time Outside Blood Pressure Target Range | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Gene | Block # | Haplotype | OR (SE) | p-Value | OR (SE) | p-Value | Bèta (SE) | p-Value | Bèta (SE) | p-Value |
| ADRA1A | 1 | A-C | 0.70 (0.34) | 0.30 | 0.93 (0.27) | 0.78 | 0.79 (3.31) | 0.81 | −0.04 (0.25) | 0.87 |
| 1 | G-T | 1.58 (0.32) | 0.15 | 1.12 (0.24) | 0.63 | −1.19 (2.94) | 0.69 | 0.07 (0.23) | 0.76 | |
| ADRA1A | 2 | A-C-C | 0.62 (0.37) | 0.20 | 0.85 (0.27) | 0.56 | 1.49 (3.38) | 0.66 | −0.04 (0.26) | 0.88 |
| 2 | A-T-C | 1.95 (0.45) | 0.14 | 1.13 (0.32) | 0.71 | −1.55 (4.06) | 0.70 | 0.17 (0.30) | 0.56 | |
| 2 | G-C-A | 0.81 (0.43) | 0.63 | 1.31 (0.33) | 0.42 | −0.89 (3.91) | 0.83 | −0.22 (0.31) | 0.48 | |
| ADRA1A | 3 | C-A-T-C | 0.72 (0.58) | 0.57 | 1.42 (0.51) | 0.49 | 3.68 (5.64) | 0.52 | −0.54 (0.44) | 0.22 |
| 3 | C-G-T-C | 1.74 (0.36) | 0.13 | 1.06 (0.28) | 0.84 | −2.46 (3.28) | 0.46 | 0.18 (0.25) | 0.48 | |
| 3 | T-A-C-C | 0.78 (0.37) | 0.51 | 0.62 (0.31) | 0.13 | −1.95 (3.90) | 0.62 | −0.01 (0.29) | 0.97 | |
| 3 | T-A-C-T | 0.87 (0.41) | 0.74 | 1.18 (0.30) | 0.58 | 2.81 (3.63) | 0.44 | 0.00 (0.29) | 0.99 | |
| ADRA1B | 5 | A-A-C-T | 1.93 (0.46) | 0.16 | 1.86 (0.37) | 0.10 | −1.45 (4.12) | 0.73 | −0.08 (0.33) | 0.80 |
| 5 | C-A-T-T | 1.58 (0.86) | 0.60 | 0.58 (0.55) | 0.33 | 6.49 (6.50) | 0.32 | −0.19 (0.49) | 0.70 | |
| 5 | C-G-C-G | 0.71 (0.36) | 0.34 | 0.66 (0.28) | 0.15 | 3.65 (3.29) | 0.27 | 0.35 (0.26) | 0.19 | |
| 5 | C-G-C-T | 1.71 (0.71) | 0.45 | 1.85 (0.50) | 0.22 | −5.56 (6.22) | 0.37 | −0.69 (0.46) | 0.14 | |
| ADRA1B | 6 | A-C-A-C | 3.30 (0.58) | 0.044 * | 3.51 (0.46) | 0.007 * | 2.54 (5.06) | 0.62 | −0.30 (0.38) | 0.43 |
| 6 | G-C-A-C | 0.72 (0.38) | 0.38 | 0.55 (0.30) | 0.05 | 3.04 (3.76) | 0.42 | 0.38 (0.28) | 0.18 | |
| 6 | G-T-A-C | 0.49 (0.85) | 0.40 | 0.83 (0.67) | 0.78 | 4.66 (7.84) | 0.55 | 0.42 (0.56) | 0.46 | |
| 6 | G-T-G-T | 1.02 (0.42) | 0.96 | 1.16 (0.34) | 0.67 | −7.82 (4.17) | 0.07 | −0.38 (0.31) | 0.23 | |
| ADRA2A | 4 | A-C-G-G | 0.47 (0.39) | 0.056 | 0.94 (0.30) | 0.83 | −0.36 (3.65) | 0.92 | 0.11 (0.28) | 0.69 |
| 4 | T-G-G-A | 2.71 (0.51) | 0.055 | 1.33 (0.37) | 0.44 | −3.60 (4.53) | 0.43 | −0.34 (0.35) | 0.33 | |
| 4 | T-G-A-G | 1.55 (0.57) | 0.44 | 0.81 (0.44) | 0.62 | 5.79 (5.46) | 0.29 | 0.19 (0.41) | 0.65 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berends, A.M.A.; Bolhuis, M.S.; Nolte, I.M.; Buitenwerf, E.; Links, T.P.; Timmers, H.J.L.M.; Feelders, R.A.; Eekhoff, E.M.W.; Corssmit, E.P.M.; Bisschop, P.H.; et al. Influence of Receptor Polymorphisms on the Response to α-Adrenergic Receptor Blockers in Pheochromocytoma Patients. Biomedicines 2022, 10, 896. https://doi.org/10.3390/biomedicines10040896
Berends AMA, Bolhuis MS, Nolte IM, Buitenwerf E, Links TP, Timmers HJLM, Feelders RA, Eekhoff EMW, Corssmit EPM, Bisschop PH, et al. Influence of Receptor Polymorphisms on the Response to α-Adrenergic Receptor Blockers in Pheochromocytoma Patients. Biomedicines. 2022; 10(4):896. https://doi.org/10.3390/biomedicines10040896
Chicago/Turabian StyleBerends, Annika M. A., Mathieu S. Bolhuis, Ilja M. Nolte, Edward Buitenwerf, Thera P. Links, Henri J. L. M. Timmers, Richard A. Feelders, Elisabeth M. W. Eekhoff, Eleonora P. M. Corssmit, Peter H. Bisschop, and et al. 2022. "Influence of Receptor Polymorphisms on the Response to α-Adrenergic Receptor Blockers in Pheochromocytoma Patients" Biomedicines 10, no. 4: 896. https://doi.org/10.3390/biomedicines10040896
APA StyleBerends, A. M. A., Bolhuis, M. S., Nolte, I. M., Buitenwerf, E., Links, T. P., Timmers, H. J. L. M., Feelders, R. A., Eekhoff, E. M. W., Corssmit, E. P. M., Bisschop, P. H., Haak, H. R., van Schaik, R. H. N., el Bouazzaoui, S., Wilffert, B., & Kerstens, M. N. (2022). Influence of Receptor Polymorphisms on the Response to α-Adrenergic Receptor Blockers in Pheochromocytoma Patients. Biomedicines, 10(4), 896. https://doi.org/10.3390/biomedicines10040896






