C-Reactive Protein to Albumin Ratio as Prognostic Marker in Locally Advanced Non-Small Cell Lung Cancer Treated with Chemoradiotherapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Treatment Protocol
2.2. Response Assessment and Follow-Up
2.3. Clinicopathologic Features and Serum Chemistry
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
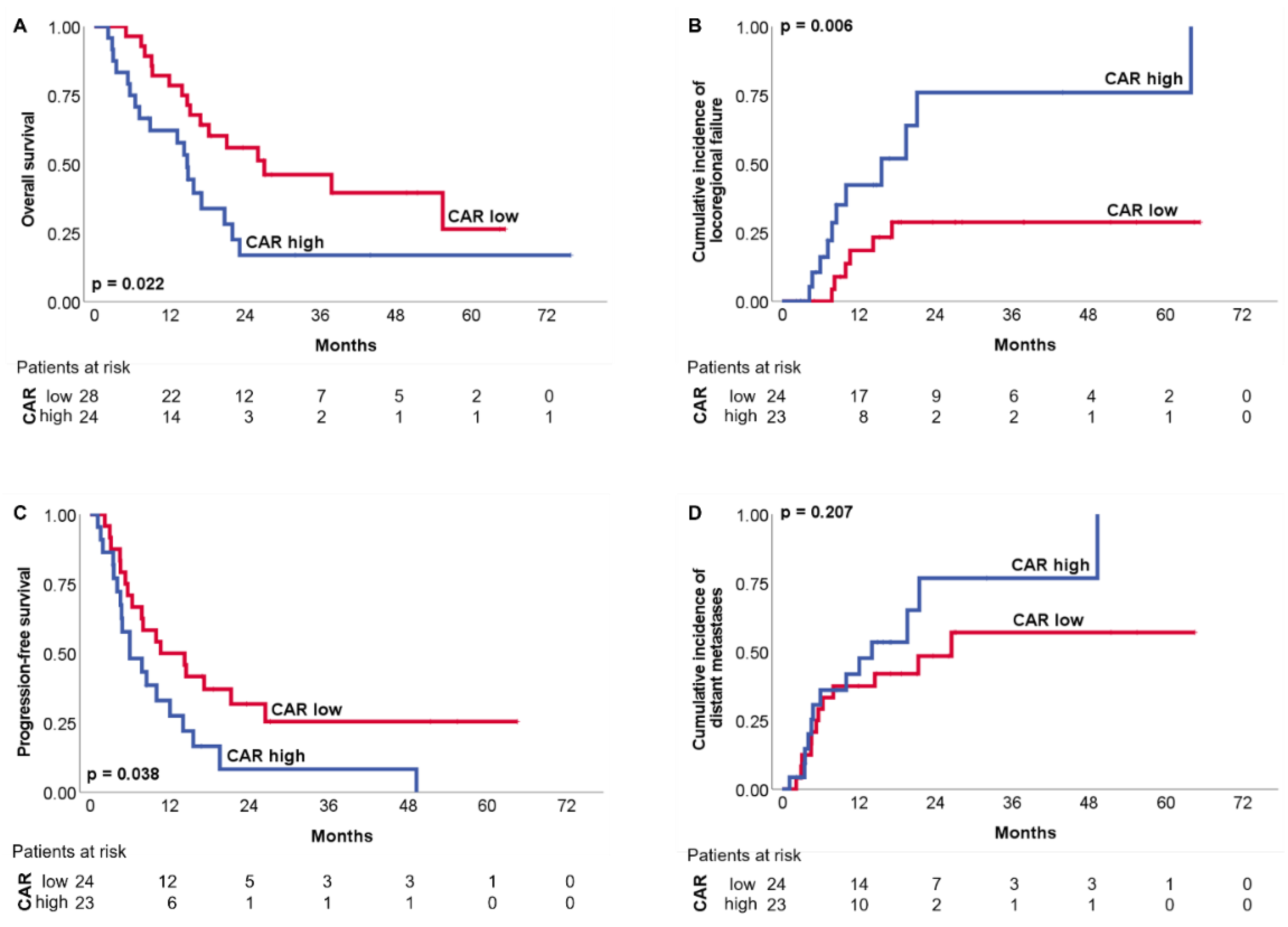
3.2. Clinical Outcomes: Disease Control and Survival
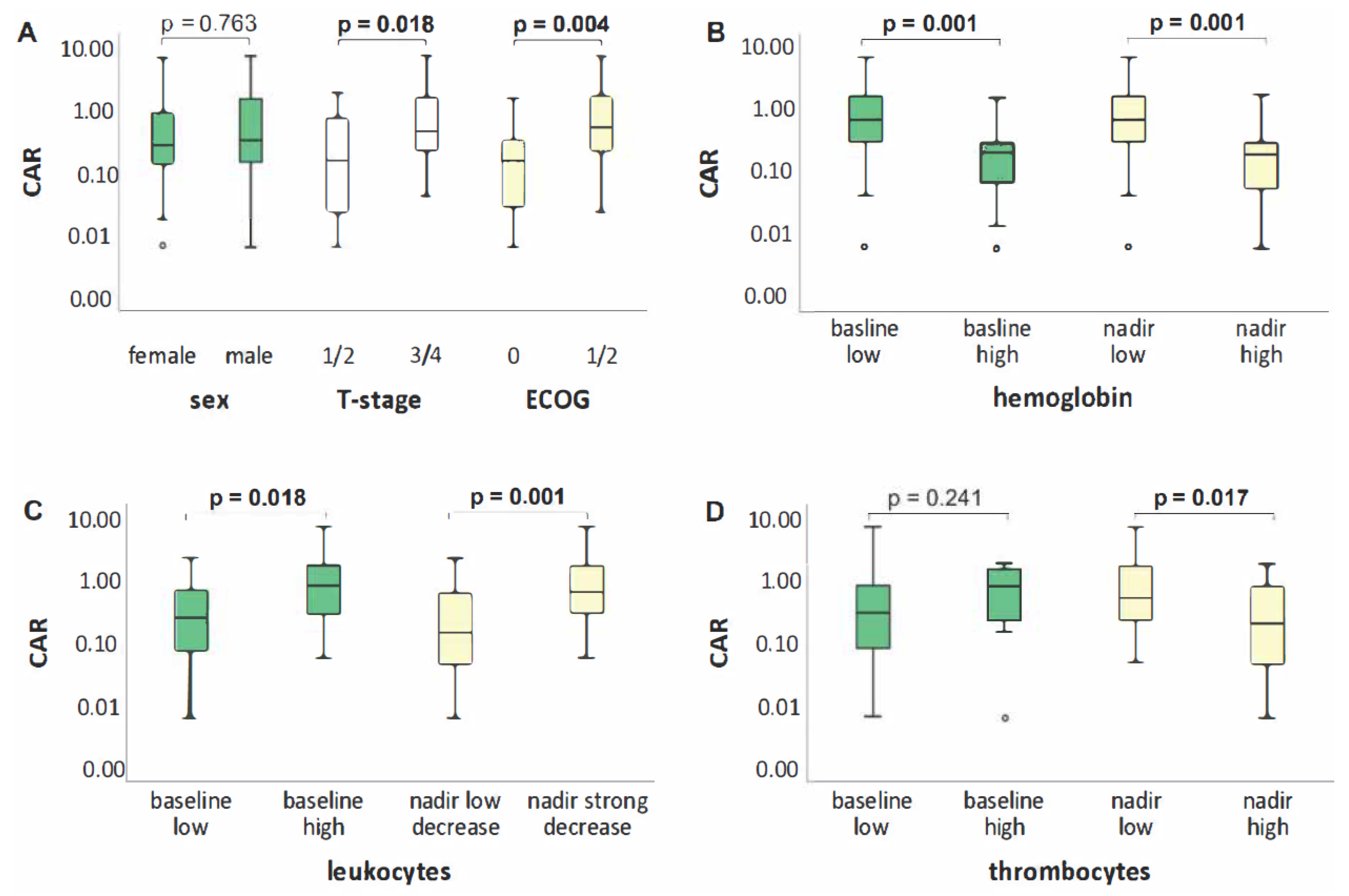
3.2.1. Univariate Analysis
3.2.2. Multivariate Analysis
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- National Cancer Institute. SEER*Explorer: An Interactive Website for SEER Cancer Statistics. Surveillance Research Program. 2022. Available online: https://seer.cancer.gov/explorer/application.html?site=47&data_type=1&graph_type=4&compareBy=sex&chk_sex_1=1&chk_sex_3=3&chk_sex_2=2&race=1&age_range=1&advopt_precision=1&advopt_display=2 (accessed on 10 January 2022).
- Spigel, D.R.; Faivre-Finn, C.; Gray, J.E.; Vicente, D.; Planchard, D.; Paz-Ares, L.G.; Vansteenkiste, J.F.; Garassino, M.C.; Hui, R.; Quantin, X.; et al. Five-year survival outcomes with durvalumab after chemoradiotherapy in unresectable stage III NSCLC: An update from the PACIFIC trial. J. Clin. Oncol. 2021, 39, 8511. [Google Scholar] [CrossRef]
- Greten, F.R.; Grivennikov, S.I. Inflammation and Cancer: Triggers, Mechanisms, and Consequences. Immunity 2019, 51, 27–41. [Google Scholar] [CrossRef]
- Lippitz, B.E.; Harris, R.A. Cytokine patterns in cancer patients: A review of the correlation between interleukin 6 and prognosis. OncoImmunology 2016, 5, e1093722. [Google Scholar] [CrossRef]
- Pikarsky, E.; Porat, R.M.; Stein, I.; Abramovitch, R.; Amit, S.; Kasem, S.; Gutkovich-Pyest, E.; Urieli-Shoval, S.; Galun, E.; Ben-Neriah, Y. NF-κB functions as a tumour promoter in inflammation-associated cancer. Nature 2004, 431, 461–466. [Google Scholar] [CrossRef]
- Castell, J.V.; Gómez-Lechón, M.J.; David, M.; Hirano, T.; Kishimoto, T.; Heinrich, P.C. Recombinant human interleukin-6 (IL-6/BSF-2/HSF) regulates the synthesis of acute phase proteins in human hepatocytes. FEBS Lett. 1988, 232, 347–350. [Google Scholar] [CrossRef]
- Sproston, N.R.; Ashworth, J.J. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front. Immunol. 2018, 9, 754. [Google Scholar] [CrossRef]
- Alsaffar, H.; Martino, N.; Garrett, J.P.; Adam, A.P. Interleukin-6 promotes a sustained loss of endothelial barrier function via Janus kinase-mediated STAT3 phosphorylation and de novo protein synthesis. Am. J. Physiol. Physiol. 2018, 314, C589–C602. [Google Scholar] [CrossRef]
- Keller, U. Nutritional Laboratory Markers in Malnutrition. J. Clin. Med. 2019, 8, 775. [Google Scholar] [CrossRef]
- Liao, W.S.; Jefferson, L.S.; Taylor, J.M. Changes in plasma albumin concentration, synthesis rate, and mRNA level during acute inflammation. Am. J. Physiol. Physiol. 1986, 251, C928–C934. [Google Scholar] [CrossRef]
- Eckart, A.; Struja, T.; Kutz, A.; Baumgartner, A.; Baumgartner, T.; Zurfluh, S.; Neeser, O.; Huber, A.; Stanga, Z.; Mueller, B.; et al. Relationship of Nutritional Status, Inflammation, and Serum Albumin Levels During Acute Illness: A Prospective Study. Am. J. Med. 2020, 133, 713–722. [Google Scholar] [CrossRef]
- Sheinenzon, A.; Shehadeh, M.; Regina, M.; Shaoul, E.; Ronen, O. Serum albumin levels and inflammation. Int. J. Biol. Macromol. 2021, 184, 857–862. [Google Scholar] [CrossRef]
- Kuboki, A.; Kanaya, H.; Nakayama, T.; Konno, W.; Goto, K.; Nakajima, I.; Kashiwagi, T.; Hirabayashi, H.; Haruna, S. Prognostic value of C-reactive protein/albumin ratio for patients with hypopharyngeal and laryngeal cancer undergoing invasive surgery involving laryngectomy. Head Neck 2019, 41, 1342–1350. [Google Scholar] [CrossRef]
- Shibutani, M.; Maeda, K.; Nagahara, H.; Iseki, Y.; Ikeya, T.; Hirakawa, K. Prognostic Significance of the Preoperative Ratio of C-Reactive Protein to Albumin in Patients with Colorectal Cancer. Anticancer Res. 2016, 36, 995–1001. [Google Scholar]
- Martin, D.; Rödel, F.; Balermpas, P.; Winkelmann, R.; Fokas, E.; Rödel, C. C-Reactive Protein-to-Albumin Ratio as Prognostic Marker for Anal Squamous Cell Carcinoma Treated with Chemoradiotherapy. Front. Oncol. 2019, 9, 1200. [Google Scholar] [CrossRef]
- Guo, Y.; Cai, K.; Mao, S.; Zhang, J.; Wang, L.; Zhang, Z.; Liu, M.; Zhang, W.; Wu, Y.; Yan, Y.; et al. Preoperative C-reactive protein/albumin ratio is a significant predictor of survival in bladder cancer patients after radical cystectomy: A retrospective study. Cancer Manag. Res. 2018, 10, 4789–4804. [Google Scholar] [CrossRef]
- Araki, T.; Tateishi, K.; Sonehara, K.; Hirota, S.; Komatsu, M.; Yamamoto, M.; Kanda, S.; Kuraishi, H.; Hanaoka, M.; Koizumi, T. Clinical utility of the C-reactive protein:albumin ratio in non-small cell lung cancer patients treated with nivolumab. Thorac. Cancer 2021, 12, 603–612. [Google Scholar] [CrossRef]
- Koh, Y.W.; Lee, H.W. Prognostic impact of C-reactive protein/albumin ratio on the overall survival of patients with advanced nonsmall cell lung cancers receiving palliative chemotherapy. Medicine 2017, 96, e6848. [Google Scholar] [CrossRef]
- Zhang, F.; Ying, L.; Jin, J.; Chen, K.; Zhang, N.; Wu, J.; Zhang, Y.; Su, D. The C-reactive protein/albumin ratio predicts long-term outcomes of patients with operable non-small cell lung cancer. Oncotarget 2016, 8, 8835–8842. [Google Scholar] [CrossRef]
- Yang, J.-R.; Xu, J.-Y.; Chen, G.-C.; Yu, N.; Yang, J.; Zeng, D.-X.; Gu, M.-J.; Li, D.-P.; Zhang, Y.-S.; Qin, L.-Q. Post-diagnostic C-reactive protein and albumin predict survival in Chinese patients with non-small cell lung cancer: A prospective cohort study. Sci. Rep. 2019, 9, 8143. [Google Scholar] [CrossRef]
- Yotsukura, M.; Ohtsuka, T.; Kaseda, K.; Kamiyama, I.; Hayashi, Y.; Asamura, H. Value of the Glasgow Prognostic Score as a Prognostic Factor in Resectable Non–Small Cell Lung Cancer. J. Thorac. Oncol. 2016, 11, 1311–1318. [Google Scholar] [CrossRef][Green Version]
- Kishi, T.; Matsuo, Y.; Ueki, N.; Iizuka, Y.; Nakamura, A.; Sakanaka, K.; Mizowaki, T.; Hiraoka, M. Pretreatment Modified Glasgow Prognostic Score Predicts Clinical Outcomes After Stereotactic Body Radiation Therapy for Early-Stage Non-Small Cell Lung Cancer. Int. J. Radiat. Oncol. 2015, 92, 619–626. [Google Scholar] [CrossRef]
- Leung, E.Y.; Scott, H.R.; McMillan, D.C. Clinical Utility of the Pretreatment Glasgow Prognostic Score in Patients with Advanced Inoperable Non-Small Cell Lung Cancer. J. Thorac. Oncol. 2012, 7, 655–662. [Google Scholar] [CrossRef]
- Forrest, L.M.; McMillan, D.C.; McArdle, C.S.; Angerson, W.J.; Dunlop, D.J. Evaluation of cumulative prognostic scores based on the systemic inflammatory response in patients with inoperable non-small-cell lung cancer. Br. J. Cancer 2003, 89, 1028–1030. [Google Scholar] [CrossRef]
- Peduzzi, P.; Concato, J.; Feinstein, A.R.; Holford, T.R. Importance of events per independent variable in proportional hazards regression analysis II. Accuracy and precision of regression estimates. J. Clin. Epidemiol. 1995, 48, 1503–1510. [Google Scholar] [CrossRef]
- Grivennikov, S.I.; Greten, F.R.; Karin, M. Immunity, inflammation, and cancer. Cell 2010, 140, 883–899. [Google Scholar] [CrossRef]
- Knittelfelder, O.; Delago, D.; Jakse, G.; Lukasiak, K.; Thurner, E.-M.; Thurnher, D.; Pichler, M.; Renner, W.; Stranzl-Lawatsch, H.; Langsenlehner, T. The Pre-Treatment C-Reactive Protein Represents a Prognostic Factor in Patients with Oral and Oropharyngeal Cancer Treated with Radiotherapy. Cancers 2020, 12, 626. [Google Scholar] [CrossRef]
- Woo, H.D.; Kim, K.; Kim, J. Association between preoperative C-reactive protein level and colorectal cancer survival: A meta-analysis. Cancer Causes Control 2015, 26, 1661–1670. [Google Scholar] [CrossRef]
- Babic, A.; Schnure, N.; Neupane, N.P.; Zaman, M.M.; Rifai, N.; Welch, M.W.; Brais, L.K.; Rubinson, D.A.; Morales-Oyarvide, V.; Yuan, C.; et al. Plasma inflammatory cytokines and survival of pancreatic cancer patients. Clin. Transl. Gastroenterol. 2018, 9, e145. [Google Scholar] [CrossRef]
- Hashimoto, K.; Ikeda, Y.; Korenaga, D.; Tanoue, K.; Hamatake, M.; Kawasaki, K.; Yamaoka, T.; Iwatani, Y.; Akazawa, K.; Takenaka, K. The impact of preoperative serum C-reactive protein on the prognosis of patients with hepatocellular carcinoma. Cancer 2005, 103, 1856–1864. [Google Scholar] [CrossRef]
- Kramer, M.; Heinisch, A.; Wegener, G.; Abbas, M.; Von Klot, C.; Peters, I.; Tezval, H.; Herrmann, T.; Kuczyk, M.; Merseburger, A. C-reaktives Protein vor radikaler Zystektomie. Der. Urol. 2013, 53, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Zhao, J.; Shi, L.; Jin, Y.; Sun, Y.; Shi, X. Prognostic value of circulating C-reactive protein levels in patients with non-small cell lung cancer: A systematic review with meta-analysis. J. Cancer Res. Ther. 2014, 10, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Mandaliya, H.; Jones, M.; Oldmeadow, C.; Nordman, I.I.C. Prognostic biomarkers in stage IV non-small cell lung cancer (NSCLC): Neutrophil to lymphocyte ratio (NLR), lymphocyte to monocyte ratio (LMR), platelet to lymphocyte ratio (PLR) and advanced lung cancer inflammation index (ALI). Transl. Lung Cancer Res. 2019, 8, 886–894. [Google Scholar] [CrossRef] [PubMed]
- Russo, A.; Russano, M.; Franchina, T.; Migliorino, M.R.; Aprile, G.; Mansueto, G.; Berruti, A.; Falcone, A.; Aieta, M.; Gelibter, A.; et al. Neutrophil-to-Lymphocyte Ratio (NLR), Platelet-to-Lymphocyte Ratio (PLR), and Outcomes with Nivolumab in Pretreated Non-Small Cell Lung Cancer (NSCLC): A Large Retrospective Multicenter Study. Adv. Ther. 2020, 37, 1145–1155. [Google Scholar] [CrossRef]
- Palomar-Abril, V.; Soria-Comes, T.; Campos, S.T.; Ureste, M.M.; Bosch, V.G.; Maiques, I.C.M. Dynamic evaluation of neutrophil-to-lymphocyte ratio as prognostic factor in stage III non-small cell lung cancer treated with chemoradiotherapy. Clin. Transl. Oncol. 2020, 22, 2333–2340. [Google Scholar] [CrossRef]
- Kanzaki, H.; Hamamoto, Y.; Nagasaki, K.; Kozuki, T. Impact of neutrophil-to-lymphocyte ratio throughout the course of chemoradiotherapy on overall survival and distant failure in unresectable stage III non-small cell lung cancer. Jpn. J. Radiol. 2021, 39, 914–922. [Google Scholar] [CrossRef]
- Coffelt, S.B.; Wellenstein, M.D.; De Visser, K.E. Neutrophils in cancer: Neutral no more. Nat. Rev. Cancer 2016, 16, 431–446. [Google Scholar] [CrossRef]
- Li, W.; Ma, G.; Wu, Q.; Deng, Y.; Liu, Y.; Wang, J. Prognostic value of lymphocyte-to-monocyte ratio among Asian lung cancer patients: A systematic review and meta-analysis. Oncotarget 2017, 8, 110606–110613. [Google Scholar] [CrossRef]
- Sekine, K.; Kanda, S.; Goto, Y.; Horinouchi, H.; Fujiwara, Y.; Yamamoto, N.; Motoi, N.; Ohe, Y. Change in the lymphocyte-to-monocyte ratio is an early surrogate marker of the efficacy of nivolumab monotherapy in advanced non-small-cell lung cancer. Lung Cancer 2018, 124, 179–188. [Google Scholar] [CrossRef]
- Venkatesulu, B.P.; Mallick, S.; Lin, S.H.; Krishnan, S. A systematic review of the influence of radiation-induced lymphopenia on survival outcomes in solid tumors. Crit. Rev. Oncol. 2018, 123, 42–51. [Google Scholar] [CrossRef]
- Dhanapal, R.; Saraswathi, T.; Govind, R.N. Cancer cachexia. J. Oral Maxillofac. Pathol. 2011, 15, 257–260. [Google Scholar] [CrossRef]
- Almasaudi, A.S.; Dolan, R.D.; Edwards, C.A.; McMillan, D.C. Hypoalbuminemia Reflects Nutritional Risk, Body Composition and Systemic Inflammation and is Independently Associated with Survival in Patients with Colorectal Cancer. Cancers 1986, 12, 1986. [Google Scholar] [CrossRef] [PubMed]
- Lim, W.S.; Roh, J.-L.; Kim, S.-B.; Choi, S.-H.; Nam, S.Y.; Kim, S.Y. Pretreatment albumin level predicts survival in head and neck squamous cell carcinoma. Laryngoscope 2017, 127, E437–E442. [Google Scholar] [CrossRef]
- Tanriverdi, O.; Avci, N.; Oktay, E.; Kalemci, S.; Pilanci, K.N.; Cokmert, S.; Menekse, S.; Kocar, M.; Sen, C.A.; Akman, T.; et al. Pretreatment Serum Albumin Level is an Independent Prognostic Factor in Patients with Stage IIIB Non-Small Cell Lung Cancer: A Study of the Turkish Descriptive Oncological Researches Group. Asian Pac. J. Cancer Prev. 2015, 16, 5971–5976. [Google Scholar] [CrossRef] [PubMed]
- Stares, M.; Swan, A.; Cumming, K.; Ding, T.-E.; Leach, J.; Stratton, C.; Thomson, F.; Barrie, C.; MacLennan, K.; Campbell, S.; et al. Hypoalbuminaemia as a Prognostic Biomarker of First-Line Treatment Resistance in Metastatic Non-small Cell Lung Cancer. Front. Nutr. 2021, 8, 734735. [Google Scholar] [CrossRef] [PubMed]
- Rim, C.H.; Yoon, W.S.; Lee, J.A.; Yang, D.S.; Lee, N.K.; Park, Y.J.; Kim, C.Y. Factors predicting intolerance to definitive conventional radiotherapy in geriatric patients. Strahlenther. Onkol. 2018, 194, 894–903. [Google Scholar] [CrossRef]
- Yu, J.M.; Yang, M.; Xu, H.X.; Li, W.; Fu, Z.; Lin, Y.; Shi, Y.Y.; Song, C.H.; Shi, H.P.; Guo, Z.Q.; et al. Association Between Serum C-Reactive Protein Concentration and Nutritional Status of Malignant Tumor Patients. Nutr. Cancer 2018, 71, 240–245. [Google Scholar] [CrossRef]
- Zhu, L.; Chen, S.; Ma, S.; Zhang, S. Glasgow prognostic score predicts prognosis of non-small cell lung cancer: A meta-analysis. SpringerPlus 2016, 5, 439. [Google Scholar] [CrossRef]
- Jin, J.; Hu, K.; Zhou, Y.; Li, W. Clinical utility of the modified Glasgow prognostic score in lung cancer: A meta-analysis. PLoS ONE 2017, 12, e0184412. [Google Scholar] [CrossRef]
- Matsumoto, T.; Itoh, S.; Yoshizumi, T.; Kurihara, T.; Yoshiya, S.; Mano, Y.; Takeishi, K.; Harada, N.; Ikegami, T.; Soejima, Y.; et al. C-reactive protein: Albumin ratio in patients with resectable intrahepatic cholangiocarcinoma. BJS Open 2020, 4, 1146–1152. [Google Scholar] [CrossRef]
- Icard, P.; Schussler, O.; Loi, M.; Bobbio, A.; Lupo, A.M.; Wislez, M.; Iannelli, A.; Fournel, L.; Damotte, D.; Alifano, M. Pre-Disease and Pre-Surgery BMI, Weight Loss and Sarcopenia Impact Survival of Resected Lung Cancer Independently of Tumor Stage. Cancers 2020, 12, 266. [Google Scholar] [CrossRef] [PubMed]
- Fukui, T.; Taniguchi, T.; Kawaguchi, K.; Fukumoto, K.; Nakamura, S.; Sakao, Y.; Yokoi, K. Comparisons of the clinicopathological features and survival outcomes between lung cancer patients with adenocarcinoma and squamous cell carcinoma. Gen. Thorac. Cardiovasc. Surg. 2015, 63, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Wheatley-Price, P.; Blackhall, F.; Lee, S.M.; Ma, C.; Ashcroft, L.; Jitlal, M.; Qian, W.; Hackshaw, A.; Rudd, R.; Booton, R.; et al. The influence of sex and histology on outcomes in non-small-cell lung cancer: A pooled analysis of five randomized trials. Ann. Oncol. 2010, 21, 2023–2028. [Google Scholar] [CrossRef] [PubMed]
- Kale, M.S.; Mhango, G.; Gomez, J.; Sigel, K.; Smith, C.B.; Bonomi, M.; Wisnivesky, J.P. Treatment Toxicity in Elderly Patients with Advanced Non–Small Cell Lung Cancer. Am. J. Clin. Oncol. 2017, 40, 470–476. [Google Scholar] [CrossRef] [PubMed]
| Median or n (Range or %) | |||
|---|---|---|---|
| Patients | Sex | Male | 25 (48.1) |
| Female | 27 (51.9) | ||
| Age (years) | 66 (47–79) | ||
| BMI (kg/m2) | 25.14 (16.48–39.12) | ||
| ECOG | 0 | 16 (30.8) | |
| 1 | 30 (57.7) | ||
| 2 | 6 (11.5) | ||
| Tumor | T-stage | T1 | 4 (7.7) |
| T2 | 14 (26.9) | ||
| T3 | 16 (30.8) | ||
| T4 | 18 (34.6) | ||
| N-stage | N0 | 6 (11.5) | |
| N1 | 2 (3.9) | ||
| N2 | 26 (50.0) | ||
| N3 | 18 (34.6) | ||
| Histology | Adeno | 29 (55.8) | |
| Squamous cell | 17 (32.7) | ||
| Spindle cell (sarcomatoid) | 1 (1.9) | ||
| Neuroendocrine (large cell) | 3 (5.8) | ||
| NOS | 2 (3.8) | ||
| Treatment | CRT | Definitive | 43 (82.7) |
| Neoadjuvant-intended | 9 (17.3) | ||
| Induction CT | Yes | 17 (32.7) | |
| No | 35 (67.3) | ||
| Total dose (Gy) | 66.6 (45–66.6) | ||
| Baseline | CRP (mg/dL) | 1.37 (0.03–21.43) | |
| Albumin (g/dL) | 4.1 (2.8–4.9) | ||
| CAR | 0.32 (0.01–7.14) | ||
| Hemoglobin (g/dL) | 12.35 (8.0–15.2) | ||
| Leukocytes (/nL) | 8.39 (3.29–80.95) | ||
| Thrombocytes (/nL) | 312.5 (117–679) | ||
| GPS | 0 | 20 (38.5) | |
| 1 | 29 (55.8) | ||
| 2 | 3 (5.8) | ||
| Nadir | Hemoglobin (g/dL) | 10.0 (6.0–12.3) | |
| Leukocytes (/nL) | 2.28 (0.15–7.13) | ||
| Thrombocytes (/nL) | 144 (10–305) |
| HR | 95% CI | p-Value | |
|---|---|---|---|
| OS | 2.178 | 1.101–4.310 | 0.022 |
| PFS | 2.005 | 1.026–3.918 | 0.038 |
| LPFS | 3.723 | 1.365–10.151 | 0.006 |
| DMFS | 1.658 | 0.749–3.671 | 0.208 |
| HR | 95% CI | p-Value | ||
|---|---|---|---|---|
| LPFS | CAR | 3.562 | 1.294–9.802 | 0.011 |
| Leukocytes nadir | 0.266 | 0.085–0.836 | 0.013 | |
| Sex | removed |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frey, A.; Martin, D.; D’Cruz, L.; Fokas, E.; Rödel, C.; Fleischmann, M. C-Reactive Protein to Albumin Ratio as Prognostic Marker in Locally Advanced Non-Small Cell Lung Cancer Treated with Chemoradiotherapy. Biomedicines 2022, 10, 598. https://doi.org/10.3390/biomedicines10030598
Frey A, Martin D, D’Cruz L, Fokas E, Rödel C, Fleischmann M. C-Reactive Protein to Albumin Ratio as Prognostic Marker in Locally Advanced Non-Small Cell Lung Cancer Treated with Chemoradiotherapy. Biomedicines. 2022; 10(3):598. https://doi.org/10.3390/biomedicines10030598
Chicago/Turabian StyleFrey, Alina, Daniel Martin, Louisa D’Cruz, Emmanouil Fokas, Claus Rödel, and Maximilian Fleischmann. 2022. "C-Reactive Protein to Albumin Ratio as Prognostic Marker in Locally Advanced Non-Small Cell Lung Cancer Treated with Chemoradiotherapy" Biomedicines 10, no. 3: 598. https://doi.org/10.3390/biomedicines10030598
APA StyleFrey, A., Martin, D., D’Cruz, L., Fokas, E., Rödel, C., & Fleischmann, M. (2022). C-Reactive Protein to Albumin Ratio as Prognostic Marker in Locally Advanced Non-Small Cell Lung Cancer Treated with Chemoradiotherapy. Biomedicines, 10(3), 598. https://doi.org/10.3390/biomedicines10030598





