Recent Advances in the Development of Anti-FLT3 CAR T-Cell Therapies for Treatment of AML
Abstract
:1. Introduction
2. Background on AML
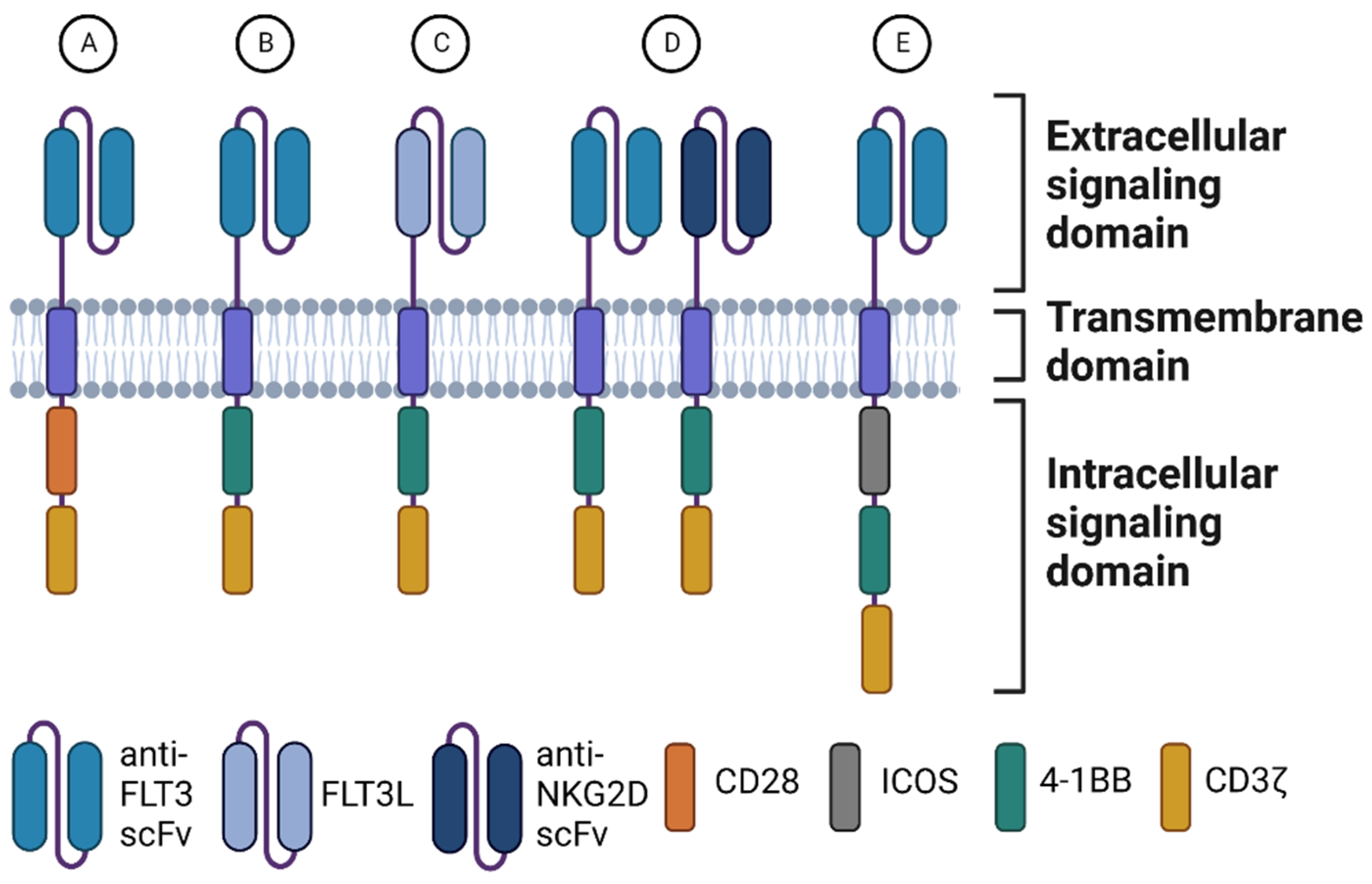
3. Configuration of Chimeric Antigen Receptors
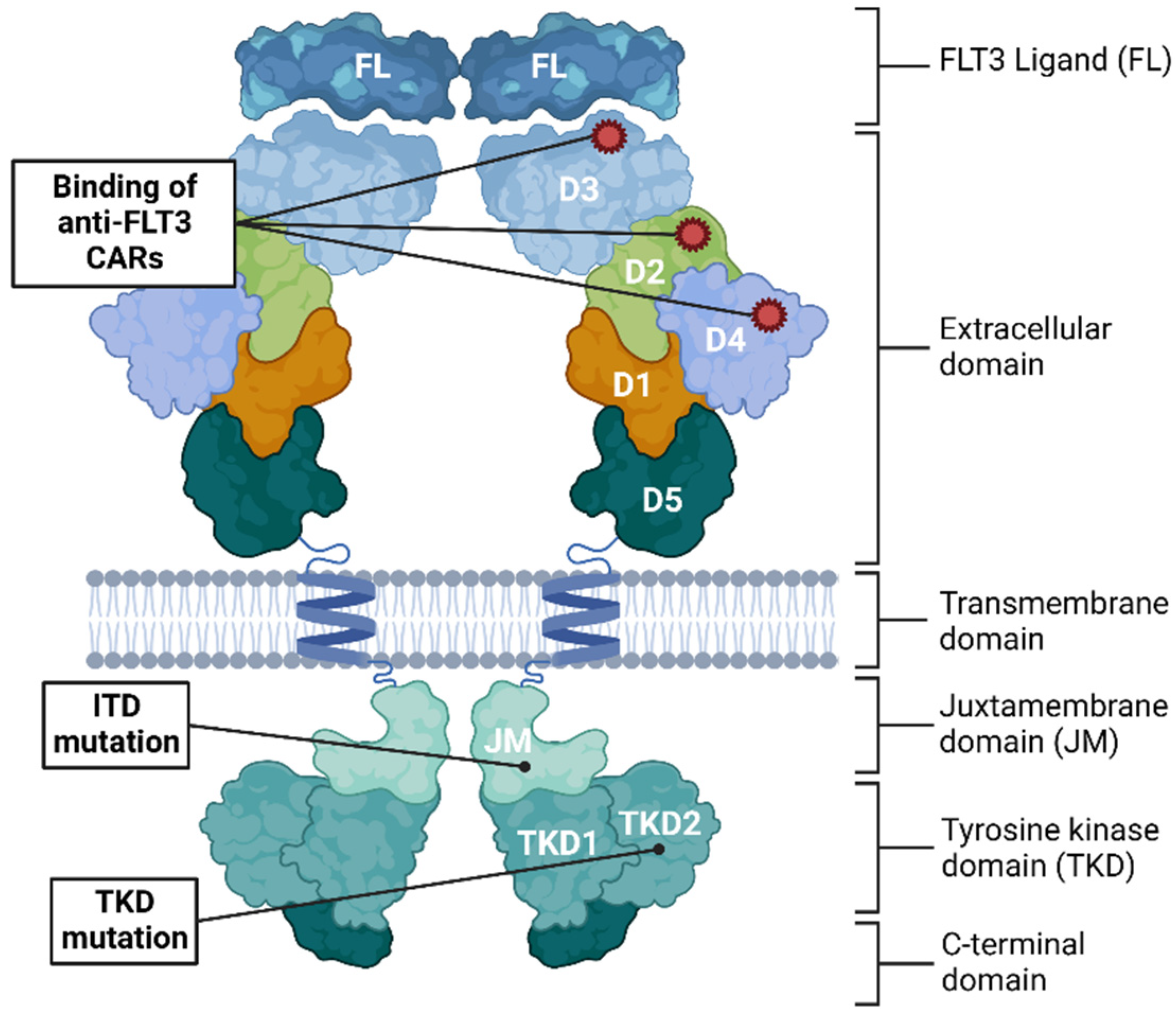
4. The Choice of FLT3 as Target for CAR T-Cell Therapy
5. In Vitro Assessment of Efficacy and Safety of Anti-FLT3 CAR T-Cell Therapies
6. In Vivo Assessment of Efficacy and Safety of Anti-FLT3 CAR T-Cell Therapy
| Reference | Antigen Recognition Domain | CAR Generation | Co-Stimulatory Domain (s) | Proportion of T-Cells with CAR Expression | Cytotoxicity on Cell Line In Vitro E/T | Cytotoxicity on Primary AML Cells In Vitro | Difference Observed in Cytotoxicity between FLT3 Genetic Variants | Lysis of Normal HSPCs | In Vivo |
|---|---|---|---|---|---|---|---|---|---|
| Chen et al. [31] | Anti-FLT3 monoclonal antibody clone 4G8 [59] | 2nd | CD28 | 80–90% | Kasumi: ~7% OCI-AML3: ~12% (E:T = 10:1) | 40–45% (n = 4, FLT3+, ~90%) 28–40% (n = 4, FLT-ITD) | No difference observed | No lysis observed | NSG |
| Jetani et al. [30] | Anti-FLT3 monoclonal antibody clone 4G8 [58] | 2nd | CD28 or 4-1BB | >90% * | MOLM-13: ~79% THP-1: ~85% MV4-11: ~60% (E:T = 10:1) | >80% (n = 3, 2/3 FLT3− ITD+) | Higher MFI -> more cytotoxicity | 50–80% (E:T ratio = 5:1) | NSG |
| Karbowski et al. [32] | Anti-FLT3 scFv from earlier research [62] | 2nd | CD28 | 24–74% | N/A ** | N/A | N/A | N/A | Cynomolgus monkeys |
| Li et al. [35] | Two CARs targeting FLT3 and NKG2D, respectively. FLT3 scFv derived from monoclonal anti-FLT3 antibody clone EB10 [60] | 2nd | 4-1BB | 30% | MOLM-13: ~27% MV4-11: 27% (E:T = 10:1) | N/A | Significant > killing of FLT− MUT+ compared with FLT-MUT- | 7% (E:T = 1:1) 20% (E:T = 10:1) 23% (E:T = 20:1) | NSG |
| Maiorova et al. [36] | Full-length human FLT3 ligand | 3rd | ICOS and 4-1BB | 49% | N/A ** | N/A | N/A | N/A | N/A |
| Sommer et al. [33] | Various anti-FLT3 scFvs from a phage library were screened for binding probabilities. | 2nd | 4-1BB | 30–60% | EOL-1: ~100% MOLM-13: ~100% MV4-11: ~100% (E:T = 3:1) | Around 80% lysis observed | N/A | Significant reduction in HSPCs, not specified in %. (E:T = 1:1) | NSG |
| Wang et al. [34] | The binding domain of human FLT3 ligand. | 2nd | 4-1BB | 40–50% | Measured survival of target: E:T = 1:4 MV4-11: 0% MOLM-13: 0% REH: 25% THP-1: 60% (E:T = 10:1) | Live AML cells after anti-FLT3L CAR T: 5 FLT IDT = 5–30% live AML cells 5 FLT3 WT = 70–20% live AML cells | Higher cytotoxicity against FLT3−ITD | No lysis observed | NSG |
| Disease | Drug | Phase | Status | Country/Sponsor | Clinical Trial Identification |
|---|---|---|---|---|---|
| FLT3-positive relapsed/refractory AML | Anti-FLT3 CAR T | I/II | Recruiting | China/The First Affiliated Hospital of Soochow University | NCT05023707 |
| FLT3-positive relapsed/refractory AML | AMG 553 (anti-FLT3 CAR T) | I | Not yet recruiting | USA/Amgen | NCT03904069 |
| Recurrent/refractory FLT3 positive AML | TAA05 (anti-FLT3 CAR T) | N/A | Recruiting | China/PersonGen BioTherapeutics (Suzhou) Co., Ltd. | NCT05017883 |
7. Discussion
8. Conclusions and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gross, G.; Waks, T.; Eshhar, Z. Expression of immunoglobulin-T-cell receptor chimeric molecules as functional receptors with antibody-type specificity. Proc. Natl. Acad. Sci. USA 1989, 86, 10024–10028. [Google Scholar] [CrossRef]
- Schuster, S.J.; Svoboda, J.; Chong, E.A.; Nasta, S.D.; Mato, A.R.; Anak, Ö.; Brogdon, J.L.; Pruteanu-Malinici, I.; Bhoj, V.; Landsburg, D.; et al. Chimeric Antigen Receptor T Cells in Refractory B-Cell Lymphomas. N. Engl. J. Med. 2017, 377, 2545–2554. [Google Scholar] [CrossRef]
- Locke, F.L.; Neelapu, S.S.; Bartlett, N.L.; Siddiqi, T.; Chavez, J.C.; Hosing, C.M.; Ghobadi, A.; Budde, L.E.; Bot, A.; Rossi, J.M.; et al. Phase 1 Results of ZUMA-1: A Multicenter Study of KTE-C19 Anti-CD19 CAR T Cell Therapy in Refractory Aggressive Lymphoma. Mol. Ther. 2017, 25, 285–295. [Google Scholar] [CrossRef]
- Maude, S.L.; Frey, N.; Shaw, P.A.; Aplenc, R.; Barrett, D.M.; Bunin, N.J.; Chew, A.; Gonzalez, V.E.; Zheng, Z.; Lacey, S.F.; et al. Chimeric antigen receptor T cells for sustained remissions in leukemia. N. Engl. J. Med. 2014, 371, 1507–1517. [Google Scholar] [CrossRef]
- CAR T Cells: Engineering Patients’ Immune Cells to Treat Their Cancers. June 2022. Available online: https://www.cancer.gov/about-cancer/treatment/research/car-t-cells (accessed on 15 June 2022).
- Sengsayadeth, S.; Savani, B.N.; Oluwole, O.; Dholaria, B. Overview of approved CAR-T therapies, ongoing clinical trials, and its impact on clinical practice. eJHaem 2022, 3, 6–10. [Google Scholar] [CrossRef]
- Ivica, N.A.; Young, C.M. Tracking the CAR-T Revolution: Analysis of Clinical Trials of CAR-T and TCR-T Therapies for the Treatment of Cancer (1997–2020). Healthcare 2021, 9, 1062. [Google Scholar] [CrossRef]
- Dohner, H.; Weisdorf, D.J.; Bloomfield, C.D. Acute Myeloid Leukemia. N. Engl. J. Med. 2015, 373, 1136–1152. [Google Scholar] [CrossRef]
- Rose-Inman, H.; Kuehl, D. Acute leukemia. Emerg. Med. Clin. N. Am. 2014, 32, 579–596. [Google Scholar] [CrossRef]
- Döhner, H.; Estey, E.; Grimwade, D.; Amadori, S.; Appelbaum, F.R.; Büchner, T.; Bloomfield, C.D. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 2017, 129, 424–447. [Google Scholar] [CrossRef]
- Schlenk, R.F.; Kayser, S.; Bullinger, L.; Kobbe, G.; Casper, J.; Ringhoffer, M.; Held, G.; Brossart, P.; Lübbert, M.; Salih, H.R.; et al. Differential impact of allelic ratio and insertion site in FLT3-ITD–positive AML with respect to allogeneic transplantation. Blood 2014, 124, 3441–3449. [Google Scholar] [CrossRef] [Green Version]
- Owattanapanich, W.; Utchariyaprasit, E.; Tantiworawit, A.; Rattarittamrong, E.; Niparuck, P.; Puavilai, T.; Julamanee, J.; Saelue, P.; Chanswangphuwana, C.; Polprasert, C.; et al. Improved Survival of Elderly-fit Patients With Acute Myeloid Leukemia Requiring Intensive Therapy: 3-Year Multicenter Analysis From TALWG. Clin. Lymphoma Myeloma Leuk. 2018, 18, e509–e514. [Google Scholar] [CrossRef]
- Miyamura, T.; Moritake, H.; Nakayama, H.; Tanaka, S.; Tomizawa, D.; Shiba, N.; Saito, A.M.; Tawa, A.; Shimada, A.; Iwamoto, S.; et al. Clinical and biological features of paediatric acute myeloid leukaemia ( AML ) with primary induction failure in the Japanese Paediatric Leukaemia/Lymphoma Study Group AML-05 study. Br. J. Haematol. 2019, 185, 284–288. [Google Scholar] [CrossRef]
- Zhang, Z.-H.; Lian, X.-Y.; Yao, D.-M.; He, P.-F.; Ma, J.-C.; Xu, Z.-J.; Guo, H.; Zhang, W.; Lin, J.; Qian, J. Reduced intensity conditioning of allogeneic hematopoietic stem cell transplantation for myelodysplastic syndrome and acute myeloid leukemia in patients older than 50 years of age: A systematic review and meta-analysis. J. Cancer Res. Clin. Oncol. 2017, 143, 1853–1864. [Google Scholar] [CrossRef]
- Surveillance, Epidemiology, and End Results (SEER) Program Populations. AML (2012–2018). Available online: https://seer.cancer.gov/statfacts/html/amyl.html (accessed on 15 June 2022).
- Versluis, J.; Hazenberg, C.L.; Passweg, J.R.; van Putten, W.L.; Maertens, J.; Biemond, B.J.; Cornelissen, J.J. Post-remission treatment with allogeneic stem cell transplantation in patients aged 60 years and older with acute myeloid leukaemia: A time-dependent analysis. Lancet Haematol. 2015, 2, e427–e436. [Google Scholar] [CrossRef]
- Araki, D.; Wood, B.L.; Othus, M.; Radich, J.P.; Halpern, A.B.; Zhou, Y.; Walter, R.B. Allogeneic Hematopoietic Cell Transplantation for Acute Myeloid Leukemia: Time to Move Toward a Minimal Residual Disease-Based Definition of Complete Remission? J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2016, 34, 329–336. [Google Scholar] [CrossRef]
- Gooley, T.A.; Chien, J.W.; Pergam, S.A.; Hingorani, S.; Sorror, M.L.; Boeckh, M.; Martin, P.J.; Sandmaier, B.M.; Marr, K.A.; Appelbaum, F.R.; et al. Reduced Mortality after Allogeneic Hematopoietic-Cell Transplantation. N. Engl. J. Med. 2010, 363, 2091–2101. [Google Scholar] [CrossRef]
- Brocker, T.; Karjalainen, K. Signals through T cell receptor-zeta chain alone are insufficient to prime resting T lymphocytes. J. Exp. Med. 1995, 181, 1653–1659. [Google Scholar] [CrossRef]
- Zhang, H.; Li, F.; Cao, J.; Wang, X.; Cheng, H.; Qi, K.; Wang, G.; Xu, K.; Zheng, J.; Fu, Y.-X.; et al. A chimeric antigen receptor with antigen-independent OX40 signaling mediates potent antitumor activity. Sci. Transl. Med. 2021, 13, eaba7308. [Google Scholar] [CrossRef]
- Zhang, S.; Gu, C.; Huang, L.; Wu, H.; Shi, J.; Zhang, Z.; Zhou, Y.; Zhou, J.; Gao, Y.; Liu, J.; et al. The third-generation anti-CD30 CAR T-cells specifically homing to the tumor and mediating powerful antitumor activity. Sci. Rep. 2022, 12, 10488. [Google Scholar] [CrossRef]
- Long, A.H.; Haso, W.M.; Shern, J.F.; Wanhainen, K.M.; Murgai, M.; Ingaramo, M.; Smith, J.P.; Walker, A.J.; Kohler, M.E.; Venkateshwara, V.R.; et al. 4-1BB costimulation ameliorates T cell exhaustion induced by tonic signaling of chimeric antigen receptors. Nat. Med. 2015, 21, 581–590. [Google Scholar] [CrossRef] [Green Version]
- Gomes-Silva, D.; Mukherjee, M.; Srinivasan, M.; Krenciute, G.; Dakhova, O.; Zheng, Y.; Cabral, J.M.; Rooney, C.M.; Orange, J.S.; Brenner, M.K.; et al. Tonic 4-1BB Costimulation in Chimeric Antigen Receptors Impedes T Cell Survival and Is Vector-Dependent. Cell Rep. 2017, 21, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Drent, E.; Poels, R.; Ruiter, R.; Van De Donk, N.W.C.J.; Zweegman, S.; Yuan, H.; de Bruijn, J.; Sadelain, M.; Lokhorst, H.M.; Groen, R.W.J.; et al. Combined CD28 and 4-1BB Costimulation Potentiates Affinity-tuned Chimeric Antigen Receptor–engineered T Cells. Clin. Cancer Res. 2019, 25, 4014–4025. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Chen, R.; Huang, Y.; Meng, X.; Chen, J.; Liao, C.; Tang, Y.; Zhou, C.; Gao, X.; Sun, J. Tuning the ignition of CAR: Optimizing the affinity of scFv to improve CAR-T therapy. Cell. Mol. Life Sci. 2021, 79, 14. [Google Scholar] [CrossRef] [PubMed]
- Salter, A.I.; Ivey, R.G.; Kennedy, J.J.; Voillet, V.; Rajan, A.; Alderman, E.J.; Voytovich, U.J.; Lin, C.; Sommermeyer, D.; Liu, L.; et al. Phosphoproteomic analysis of chimeric antigen receptor signaling reveals kinetic and quantitative differences that affect cell function. Sci. Signal. 2018, 11, eaat6753. [Google Scholar] [CrossRef] [PubMed]
- Cappell, K.M.; Kochenderfer, J.N. A comparison of chimeric antigen receptors containing CD28 versus 4-1BB costimulatory domains. Nat. Rev. Clin. Oncol. 2021, 18, 715–727. [Google Scholar] [CrossRef]
- Cheng, Z.; Wei, R.; Ma, Q.; Shi, L.; He, F.; Shi, Z.; Jin, T.; Xie, R.; Wei, B.; Chen, J.; et al. In Vivo Expansion and Antitumor Activity of Coinfused CD28- and 4-1BB-Engineered CAR-T Cells in Patients with B Cell Leukemia. Mol. Ther. 2018, 26, 976–985. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Zhang, J.; Wang, M.; Fu, G.; Li, Y.; Pei, L.; Xiong, Z.; Qin, D.; Zhang, R.; Tian, X.; et al. Treatment of acute lymphoblastic leukaemia with the second generation of CD19 CAR-T containing either CD28 or 4-1BB. Br. J. Haematol. 2018, 181, 360–371. [Google Scholar] [CrossRef]
- Jetani, H.; Garcia-Cadenas, I.; Nerreter, T.; Thomas, S.; Rydzek, J.; Meijide, J.B.; Bonig, H.; Herr, W.; Sierra, J.; Einsele, H.; et al. CAR T-cells targeting FLT3 have potent activity against FLT3−ITD+ AML and act synergistically with the FLT3-inhibitor crenolanib. Leukemia 2018, 32, 1168–1179. [Google Scholar] [CrossRef]
- Chen, L.; Mao, H.; Zhang, J.; Chu, J.; Devine, S.; Caligiuri, M.A.; Yu, J. Targeting FLT3 by chimeric antigen receptor T cells for the treatment of acute myeloid leukemia. Leukemia 2017, 31, 1830–1834. [Google Scholar] [CrossRef]
- Karbowski, C.; Goldstein, R.; Frank, B.; Kim, K.; Li, C.-M.; Homann, O.; Hensley, K.; Brooks, B.; Wang, X.; Yan, Q.; et al. Nonclinical Safety Assessment of AMG 553, an Investigational Chimeric Antigen Receptor T-Cell Therapy for the Treatment of Acute Myeloid Leukemia. Toxicol. Sci. 2020, 177, 94–107. [Google Scholar] [CrossRef]
- Sommer, C.; Cheng, H.-Y.; Nguyen, D.; Dettling, D.; Yeung, Y.A.; Sutton, J.; Hamze, M.; Valton, J.; Smith, J.; Djuretic, I.; et al. Allogeneic FLT3 CAR T Cells with an Off-Switch Exhibit Potent Activity against AML and Can Be Depleted to Expedite Bone Marrow Recovery. Mol. Ther. 2020, 28, 2237–2251. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Xu, Y.; Li, S.; Liu, J.; Xing, Y.; Xing, H.; Tian, Z.; Tang, K.; Rao, Q.; Wang, M.; et al. Targeting FLT3 in acute myeloid leukemia using ligand-based chimeric antigen receptor-engineered T cells. J. Hematol. Oncol. 2018, 11, 60. [Google Scholar] [CrossRef] [PubMed]
- Li, K.X.; Wu, H.Y.; Pan, W.Y.; Guo, M.Q.; Qiu, D.Z.; He, Y.J.; Huang, Y.X. A novel approach for relapsed/refractory FLT3(mut+) acute myeloid leukaemia: Synergistic effect of the combination of bispecific FLT3scFv/NKG2D-CAR T cells and gilteritinib. Mol. Cancer 2022, 21, 66. [Google Scholar] [CrossRef]
- Maiorova, V.; Mollaev, M.D.; Vikhreva, P.; Kulakovskaya, E.; Pershin, D.; Chudakov, D.M.; Kibardin, A.; Maschan, M.A.; Larin, S. Natural Flt3Lg-Based Chimeric Antigen Receptor (Flt3-CAR) T Cells Successfully Target Flt3 on AML Cell Lines. Vaccines 2021, 9, 1238. [Google Scholar] [CrossRef]
- Perna, F.; Berman, S.H.; Soni, R.K.; Mansilla-Soto, J.; Eyquem, J.; Hamieh, M.; Hendrickson, R.C.; Brennan, C.W.; Sadelain, M. Integrating Proteomics and Transcriptomics for Systematic Combinatorial Chimeric Antigen Receptor Therapy of AML. Cancer Cell 2017, 32, 506–519.e5. [Google Scholar] [CrossRef] [PubMed]
- Maucher, M.; Srour, M.; Danhof, S.; Einsele, H.; Hudecek, M.; Yakoub-Agha, I. Current Limitations and Perspectives of Chimeric Antigen Receptor-T-Cells in Acute Myeloid Leukemia. Cancers 2021, 13, 6157. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.H.; Kim, S.-Y.; Kim, K.; Jang, H.; Ahn, S.; Kim, K.-M.; Kim, N.K.; Park, W.-Y.; Lee, S.J.; Kim, S.T.; et al. The implication of FLT3 amplification for FLT targeted therapeutics in solid tumors. Oncotarget 2016, 8, 3237–3245. [Google Scholar] [CrossRef]
- Kikushige, Y.; Yoshimoto, G.; Miyamoto, T.; Iino, T.; Mori, Y.; Iwasaki, H.; Niiro, H.; Takenaka, K.; Nagafuji, K.; Harada, M.; et al. Human Flt3 Is Expressed at the Hematopoietic Stem Cell and the Granulocyte/Macrophage Progenitor Stages to Maintain Cell Survival. J. Immunol. 2008, 180, 7358–7367. [Google Scholar] [CrossRef]
- Turner, A.M.; Lin, N.L.; Issarachai, S.; Lyman, S.D.; Broudy, V.C. FLT3 receptor expression on the surface of normal and malignant human hematopoietic cells. Blood 1996, 88, 3383–3390. [Google Scholar] [CrossRef]
- Stirewalt, D.L.; Radich, J.P. The role of FLT3 in haematopoietic malignancies. Nat. Cancer 2003, 3, 650–665. [Google Scholar] [CrossRef]
- Patel, J.P.; Gönen, M.; Figueroa, M.E.; Fernandez, H.; Sun, Z.; Racevskis, J.; Van Vlierberghe, P.; Dolgalev, I.; Thomas, S.; Aminova, O.; et al. Prognostic Relevance of Integrated Genetic Profiling in Acute Myeloid Leukemia. N. Engl. J. Med. 2012, 366, 1079–1089. [Google Scholar] [CrossRef] [PubMed]
- Kottaridis, P.D.; Gale, R.E.; Frew, M.E.; Harrison, G.; Langabeer, S.E.; Belton, A.A.; Walker, H.; Wheatley, K.; Bowen, D.T.; Burnett, A.K.; et al. The presence of a FLT3 internal tandem duplication in patients with acute myeloid leukemia (AML) adds important prognostic information to cytogenetic risk group and response to the first cycle of chemotherapy: Analysis of 854 patients from the United Kingdom Medical Research Council AML 10 and 12 trials. Blood 2001, 98, 1752–1759. [Google Scholar] [CrossRef] [PubMed]
- Medina, K.L. Flt3 Signaling in B Lymphocyte Development and Humoral Immunity. Int. J. Mol. Sci. 2022, 23, 7289. [Google Scholar] [CrossRef] [PubMed]
- Al-Arbeed, I.F.; Wafa, A.; Moassass, F.; Al-Halabi, B.; Al-Achkar, W.; Abou-Khamis, I. Frequency of FLT3 Internal Tandem Duplications in Adult Syrian Patients with Acute Myeloid Leukemia and Normal Karyotype. Asian Pac. J. Cancer Prev. 2021, 22, 3245–3251. [Google Scholar] [CrossRef]
- Fröhling, S.; Schlenk, R.F.; Breitruck, J.; Benner, A.; Kreitmeier, S.; Tobis, K.; Döhner, H.; Döhner, K. Prognostic significance of activating FLT3 mutations in younger adults (16 to 60 years) with acute myeloid leukemia and normal cytogenetics: A study of the AML Study Group Ulm. Blood 2002, 100, 4372–4380. [Google Scholar] [CrossRef]
- Thiede, C.; Steudel, C.; Mohr, B.; Schaich, M.; Schäkel, U.; Platzbecker, U.; Wermke, M.; Bornhäuser, M.; Ritter, M.; Neubauer, A.; et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: Association with FAB subtypes and identification of subgroups with poor prognosis. Blood 2002, 99, 4326–4335. [Google Scholar] [CrossRef]
- Kiyoi, H.; Towatari, M.; Yokota, S.; Hamaguchi, M.; Ohno, R.; Saito, H.; Naoe, T. Internal tandem duplication of the FLT3 gene is a novel modality of elongation mutation which causes constitutive activation of the product. Leukemia 1998, 12, 1333–1337. [Google Scholar] [CrossRef]
- Kennedy, V.E.; Smith, C.C. FLT3 Mutations in Acute Myeloid Leukemia: Key Concepts and Emerging Controversies. Front. Oncol. 2020, 10, 612880. [Google Scholar] [CrossRef]
- Guan, W.; Zhou, L.; Li, Y.; Yang, E.; Liu, Y.; Lv, N.; Fu, L.; Ding, Y.; Wang, N.; Fang, N.; et al. Profiling of somatic mutations and fusion genes in acute myeloid leukemia patients with FLT3-ITD or FLT3-TKD mutation at diagnosis reveals distinct evolutionary patterns. Exp. Hematol. Oncol. 2021, 10, 27. [Google Scholar] [CrossRef]
- Warren, M.; Luthra, R.; Yin, C.C.; Ravandi, F.; Cortes, J.E.; Kantarjian, H.M.; Medeiros, L.J.; Zuo, Z. Clinical impact of change of FLT3 mutation status in acute myeloid leukemia patients. Mod. Pathol. 2012, 25, 1405–1412. [Google Scholar] [CrossRef] [Green Version]
- Whitman, S.P.; Archer, K.; Feng, L.; Baldus, C.; Becknell, B.; Carlson, B.D.; Carroll, A.J.; Mrózek, K.; Vardiman, J.W.; George, S.L.; et al. Absence of the wild-type allele predicts poor prognosis in adult de novo acute myeloid leukemia with normal cytogenetics and the internal tandem duplication of FLT3: A cancer and leukemia group B study. Cancer Res. 2001, 61, 7233–7239. [Google Scholar] [PubMed]
- Bacher, U.; Haferlach, C.; Kern, W.; Haferlach, T.; Schnittger, S. Prognostic relevance of FLT3-TKD mutations in AML: The combination matters—An analysis of 3082 patients. Blood 2008, 111, 2527–2537. [Google Scholar] [CrossRef] [PubMed]
- Verstraete, K.; Vandriessche, G.; Januar, M.; Elegheert, J.; Shkumatov, A.V.; Desfosses, A.; Van Craenenbroeck, K.; Svergun, D.I.; Gutsche, I.; Vergauwen, B.; et al. Structural insights into the extracellular assembly of the hematopoietic Flt3 signaling complex. Blood 2011, 118, 60–68. [Google Scholar] [CrossRef]
- Griffith, J.; Black, J.; Faerman, C.; Swenson, L.; Wynn, M.; Lu, F.; Lippke, J.; Saxena, K. The Structural Basis for Autoinhibition of FLT3 by the Juxtamembrane Domain. Mol. Cell 2004, 13, 169–178. [Google Scholar] [CrossRef]
- Schnittger, S.; Bacher, U.; Haferlach, C.; Alpermann, T.; Kern, W.; Haferlach, T. Diversity of the juxtamembrane and TKD1 mutations (Exons 13-15) in the FLT3 gene with regards to mutant load, sequence, length, localization, and correlation with biological data. Genes Chromosom. Cancer 2012, 51, 910–924. [Google Scholar] [CrossRef]
- Hofmann, M.; Große-Hovest, L.; Nübling, T.; Pyż, E.; Bamberg, M.L.; Aulwurm, S.; Bühring, H.-J.; Schwartz, K.; Haen, S.; Schilbach, K.; et al. Generation, selection and preclinical characterization of an Fc-optimized FLT3 antibody for the treatment of myeloid leukemia. Leukemia 2012, 26, 1228–1237. [Google Scholar] [CrossRef]
- Rappold, I.; Ziegler, B.L.; Köhler, I.; Marchetto, S.; Rosnet, O.; Birnbaum, D.; Simmons, P.J.; Zannettino, A.; Hill, B.; Neu, S.; et al. Functional and phenotypic characterization of cord blood and bone marrow subsets expressing FLT3 (CD135) receptor tyrosine kinase. Blood 1997, 90, 111–125. [Google Scholar]
- Williams, B.; Atkins, A.; Zhang, H.; Lu, D.; Jimenez, X.; Li, H.; Wang, M.-N.; Ludwig, D.; Balderes, P.; Witte, L.; et al. Cell-based selection of internalizing fully human antagonistic antibodies directed against FLT3 for suppression of leukemia cell growth. Leukemia 2005, 19, 1432–1438. [Google Scholar] [CrossRef] [PubMed]
- van Alphen, C.; Cloos, J.; Beekhof, R.; Cucchi, D.G.; Piersma, S.R.; Knol, J.C.; Jimenez, C.R. Phosphotyrosine-based Phosphoproteomics for Target Identification and Drug Response Prediction in AML Cell Lines. Mol. Cell. Proteom. 2020, 19, 884–899. [Google Scholar] [CrossRef]
- Brauchle, B.; Goldstein, R.L.; Karbowski, C.M.; Henn, A.; Li, C.-M.; Bücklein, V.L.; Krupka, C.; Boyle, M.C.; Koppikar, P.; Haubner, S.; et al. Characterization of a Novel FLT3 BiTE Molecule for the Treatment of Acute Myeloid Leukemia. Mol. Cancer Ther. 2020, 19, 1875–1888. [Google Scholar] [CrossRef] [PubMed]
- U.S. National Library of Medicine. Available online: Clinicaltrials.gov (accessed on 15 June 2022).
- Alizadeh, D.; Wong, R.A.; Yang, X.; Wang, D.; Pecoraro, J.R.; Kuo, C.-F.; Aguilar, B.; Qi, Y.; Ann, D.K.; Starr, R.; et al. IL15 Enhances CAR-T Cell Antitumor Activity by Reducing mTORC1 Activity and Preserving Their Stem Cell Memory Phenotype. Cancer Immunol. Res. 2019, 7, 759–772. [Google Scholar] [CrossRef] [PubMed]
- Willier, S.; Rothämel, P.; Hastreiter, M.; Wilhelm, J.; Stenger, D.; Blaeschke, F.; Rohlfs, M.; Kaeuferle, T.; Schmid, I.; Albert, M.H.; et al. CLEC12A and CD33 coexpression as a preferential target for pediatric AML combinatorial immunotherapy. Blood 2021, 137, 1037–1049. [Google Scholar] [CrossRef] [PubMed]
- Ehninger, A.; Kramer, M.; Röllig, C.; Thiede, C.; Bornhäuser, M.; Von Bonin, M.; Oelschlägel, U. Distribution and levels of cell surface expression of CD33 and CD123 in acute myeloid leukemia. Blood Cancer J. 2014, 4, e218. [Google Scholar] [CrossRef] [PubMed]
- Weisberg, E.; Ray, A.; Nelson, E.; Adamia, S.; Barrett, R.; Sattler, M.; Zhang, C.; Daley, J.F.; Frank, D.; Fox, E.; et al. Reversible Resistance Induced by FLT3 Inhibition: A Novel Resistance Mechanism in Mutant FLT3-Expressing Cells. PLoS ONE 2011, 6, e25351. [Google Scholar] [CrossRef]
- Bojko, P.; Pawloski, D.; Stellberg, W.; Schröder, J.; Seeber, S. Flt3 ligand and thrombopoietin serum levels during peripheral blood stem cell mobilization with chemotherapy and recombinant human glycosylated granulocyte colony-stimulating factor (rhu-G-CSF, lenograstim) and after high-dose chemotherapy. Ann. Hematol. 2002, 81, 522–528. [Google Scholar]
- Perl, A.E.; Martinelli, G.; Cortes, J.E.; Neubauer, A.; Berman, E.; Paolini, S.; Montesinos, P.; Baer, M.R.; Larson, R.A.; Ustun, C.; et al. Gilteritinib or Chemotherapy for Relapsed or Refractory FLT3-Mutated AML. N. Engl. J. Med. 2019, 381, 1728–1740. [Google Scholar] [CrossRef]
- Barros, L.; Paixão, E.; Valli, A.; Naozuka, G.; Fassoni, A.; Almeida, R. CARTmath—A Mathematical Model of CAR-T Immunotherapy in Preclinical Studies of Hematological Cancers. Cancers 2021, 13, 2941. [Google Scholar] [CrossRef]
- Mooney, C.J.; Cunningham, A.; Tsapogas, P.; Toellner, K.-M.; Brown, G. Selective Expression of Flt3 within the Mouse Hematopoietic Stem Cell Compartment. Int. J. Mol. Sci. 2017, 18, 1037. [Google Scholar] [CrossRef]
- Wiebking, V.; Lee, C.M.; Mostrel, N.; Lahiri, P.; Bak, R.; Bao, G.; Roncarolo, M.G.; Bertaina, A.; Porteus, M.H. Genome editing of donor-derived T-cells to generate allogenic chimeric antigen receptor-modified T cells: Optimizing αβ T cell-depleted haploidentical hematopoietic stem cell transplantation. Haematologica 2020, 106, 847–858. [Google Scholar] [CrossRef]
- Jensen, T.I.; Axelgaard, E.; Bak, R.O. Therapeutic gene editing in haematological disorders with CRISPR/Cas9. Br. J. Haematol. 2018, 185, 821–835. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pedersen, M.G.; Møller, B.K.; Bak, R.O. Recent Advances in the Development of Anti-FLT3 CAR T-Cell Therapies for Treatment of AML. Biomedicines 2022, 10, 2441. https://doi.org/10.3390/biomedicines10102441
Pedersen MG, Møller BK, Bak RO. Recent Advances in the Development of Anti-FLT3 CAR T-Cell Therapies for Treatment of AML. Biomedicines. 2022; 10(10):2441. https://doi.org/10.3390/biomedicines10102441
Chicago/Turabian StylePedersen, Maya Graham, Bjarne Kuno Møller, and Rasmus O. Bak. 2022. "Recent Advances in the Development of Anti-FLT3 CAR T-Cell Therapies for Treatment of AML" Biomedicines 10, no. 10: 2441. https://doi.org/10.3390/biomedicines10102441
APA StylePedersen, M. G., Møller, B. K., & Bak, R. O. (2022). Recent Advances in the Development of Anti-FLT3 CAR T-Cell Therapies for Treatment of AML. Biomedicines, 10(10), 2441. https://doi.org/10.3390/biomedicines10102441






