Plasmonic Biosensors for the Detection of Lung Cancer Biomarkers: A Review
Abstract
:1. Introduction
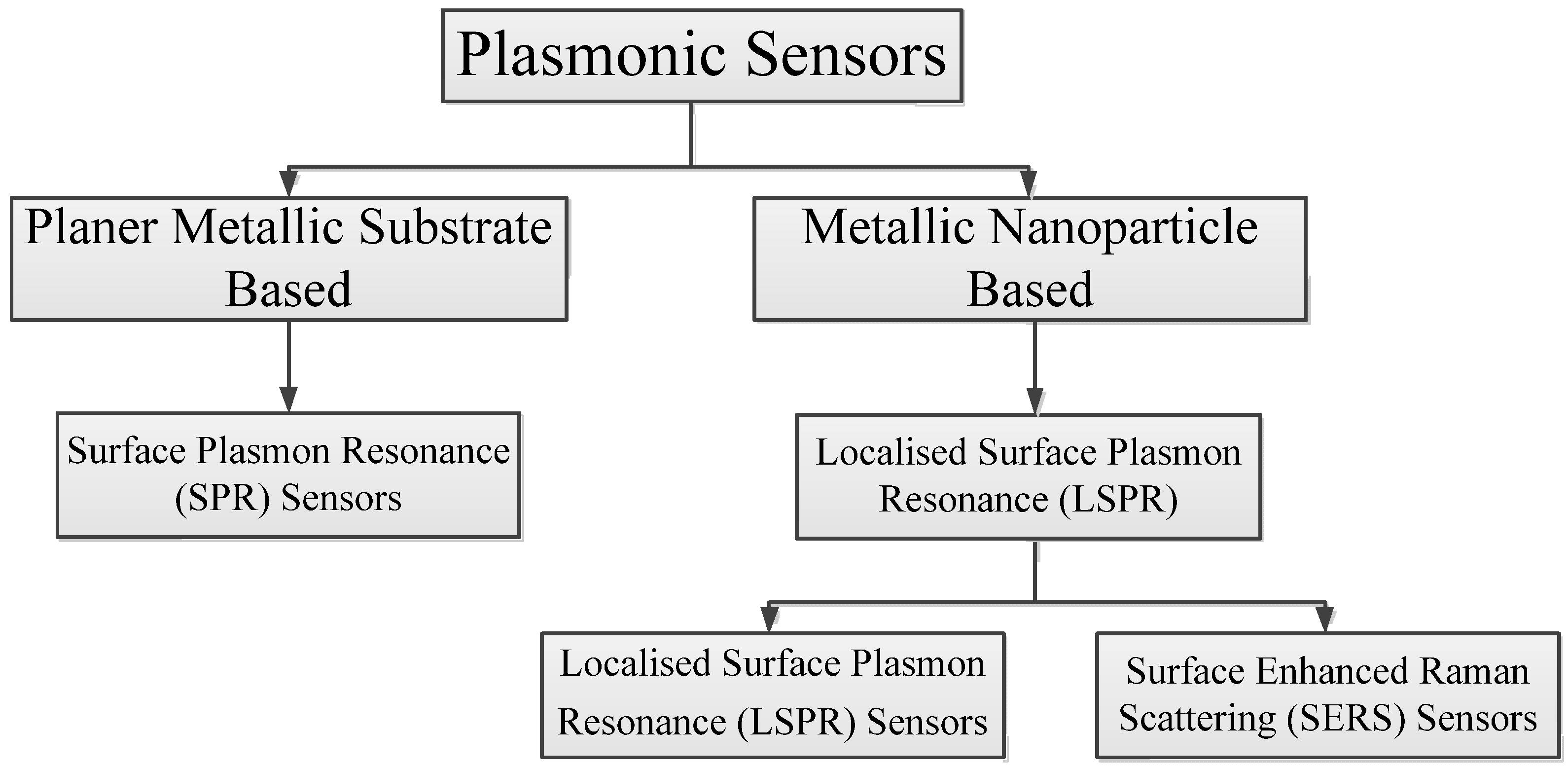
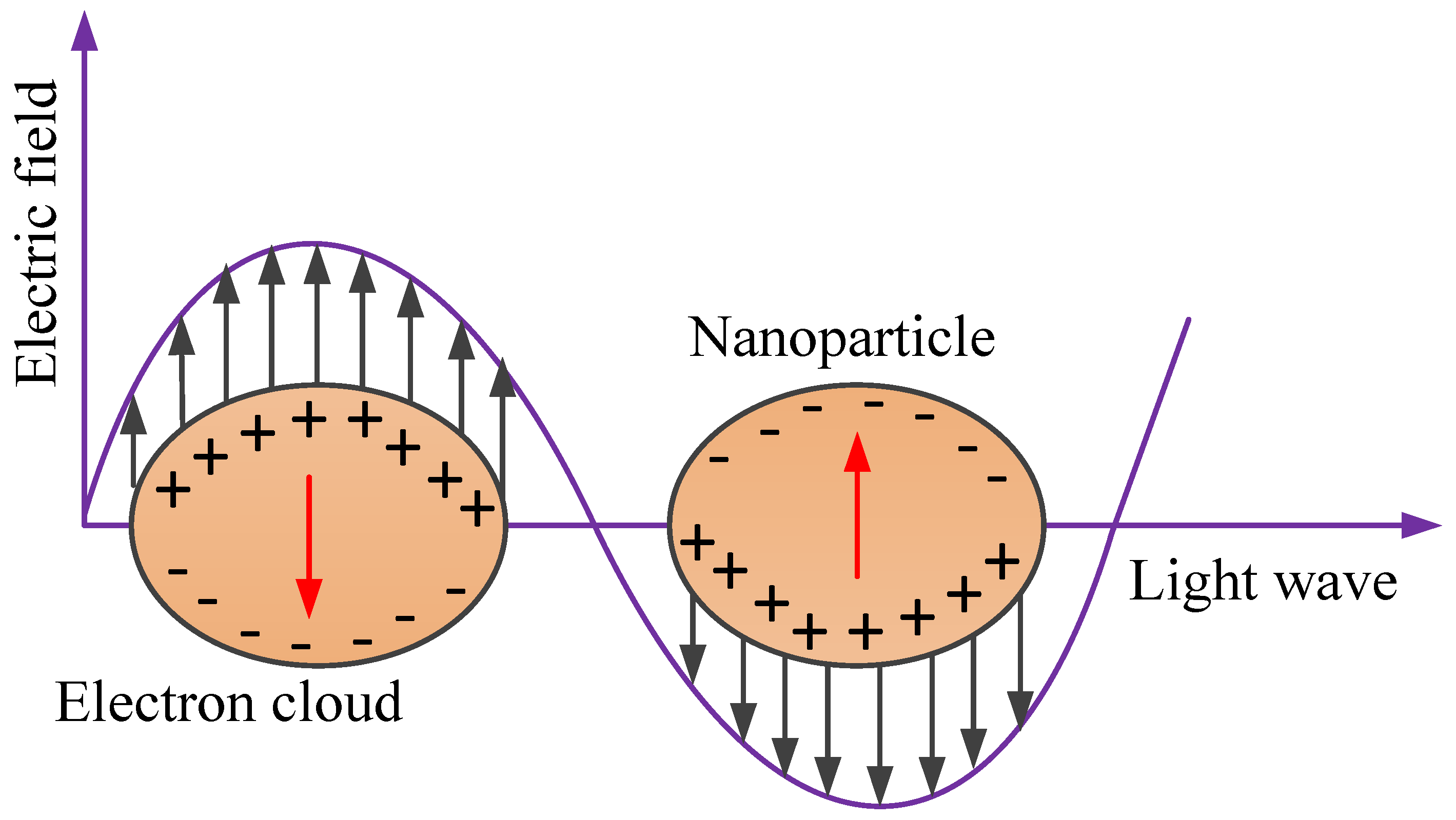
2. Principles of Plasmonic Sensing
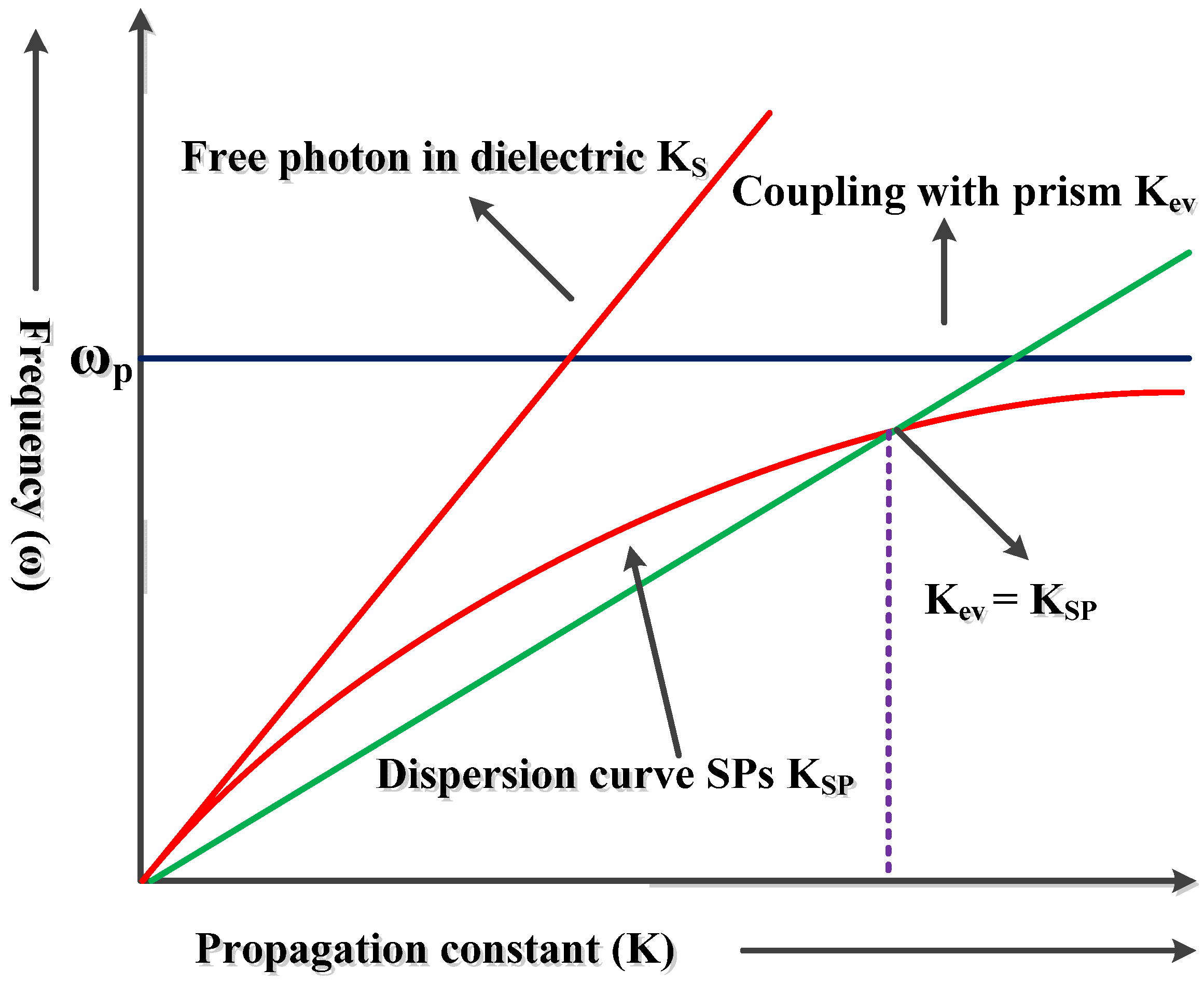
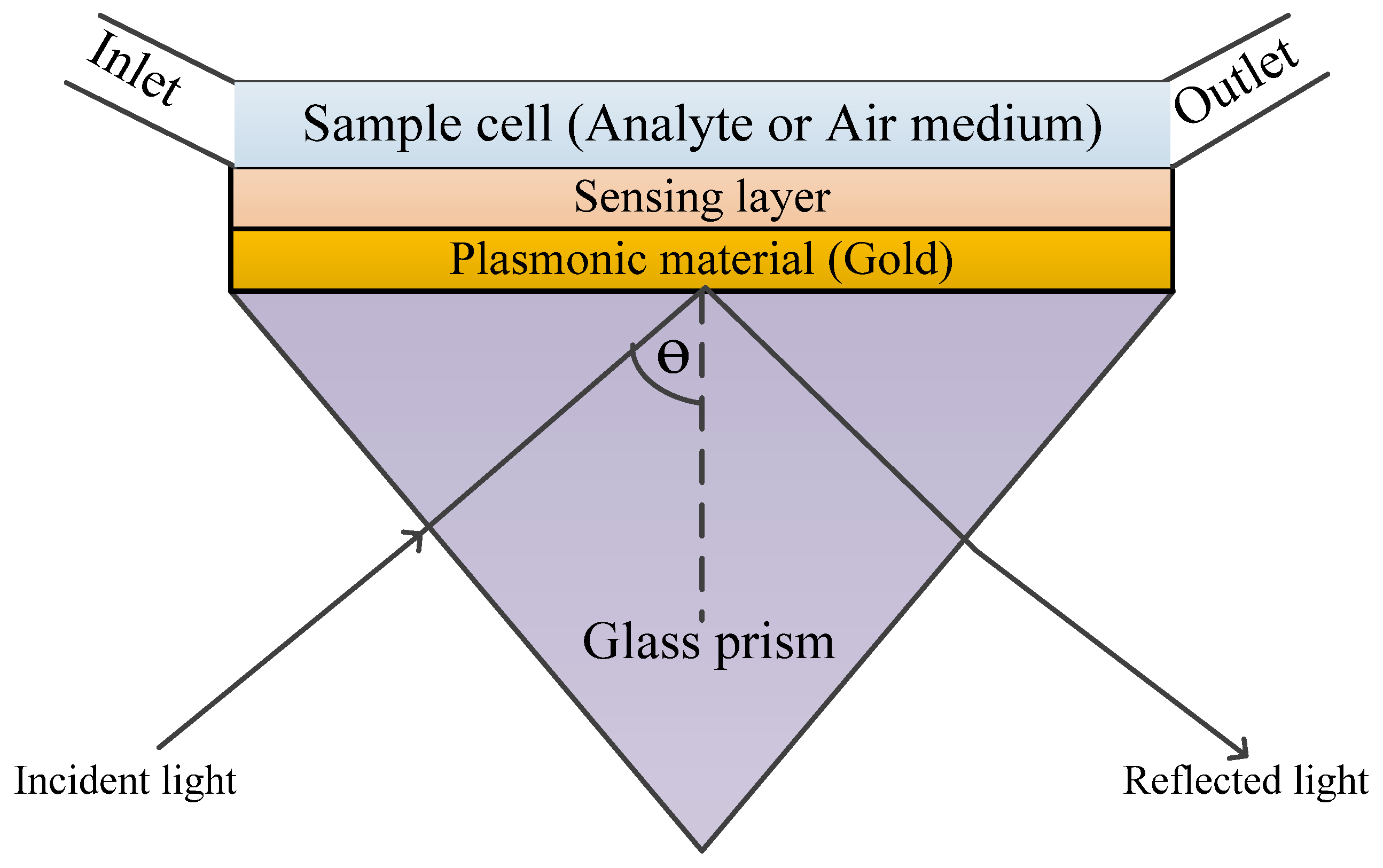
2.1. Surface Plasmon Resonance (SPR)
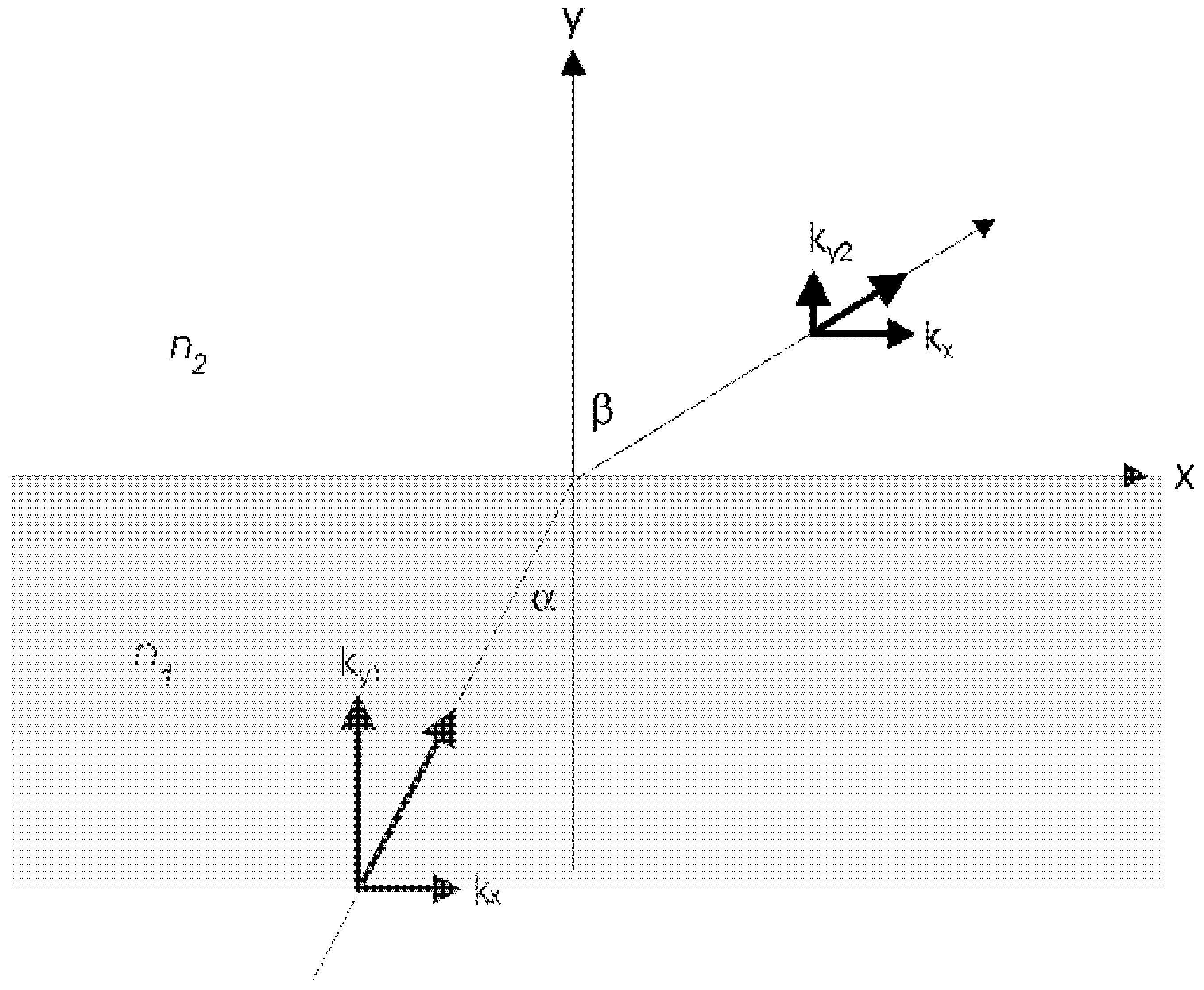
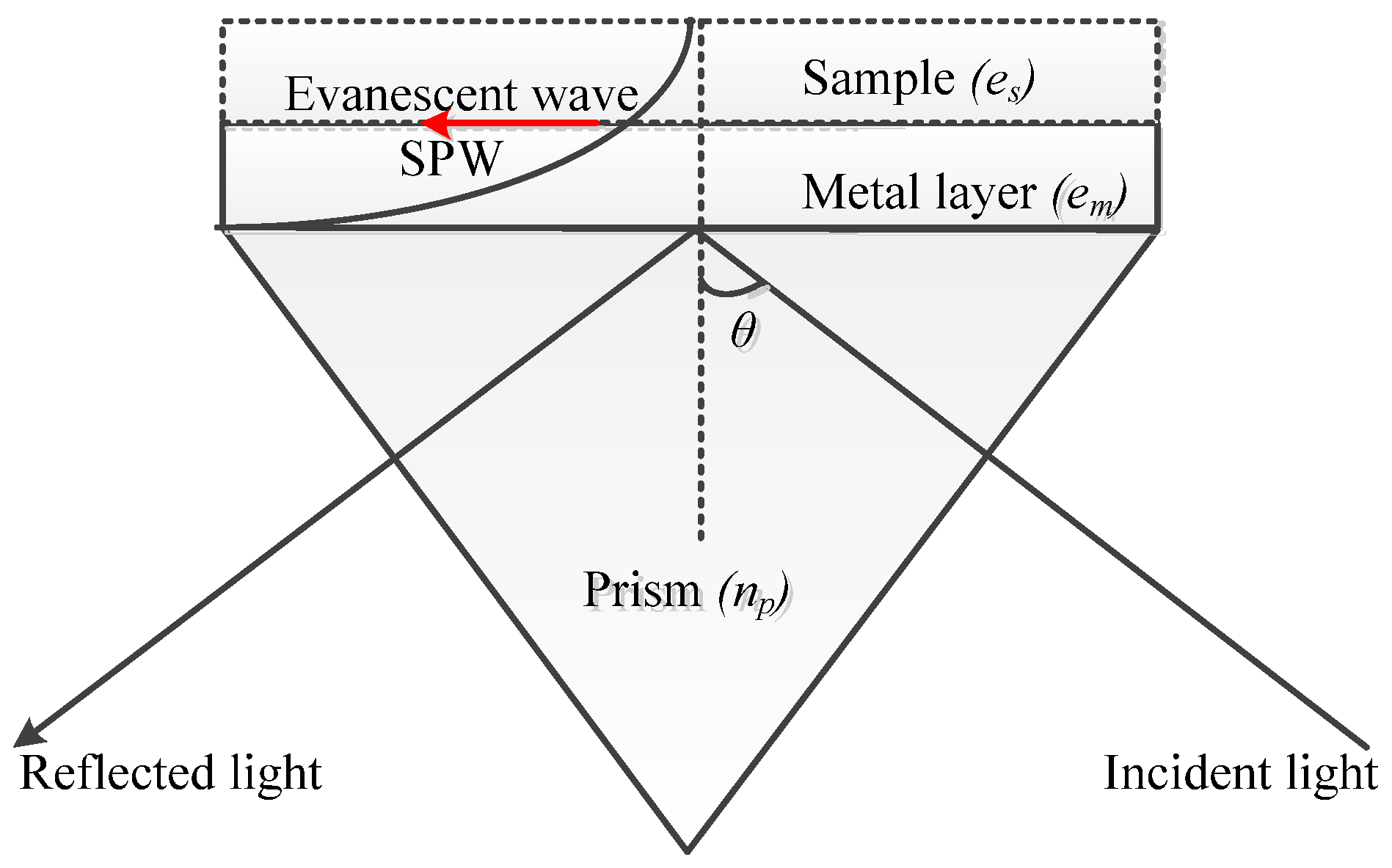
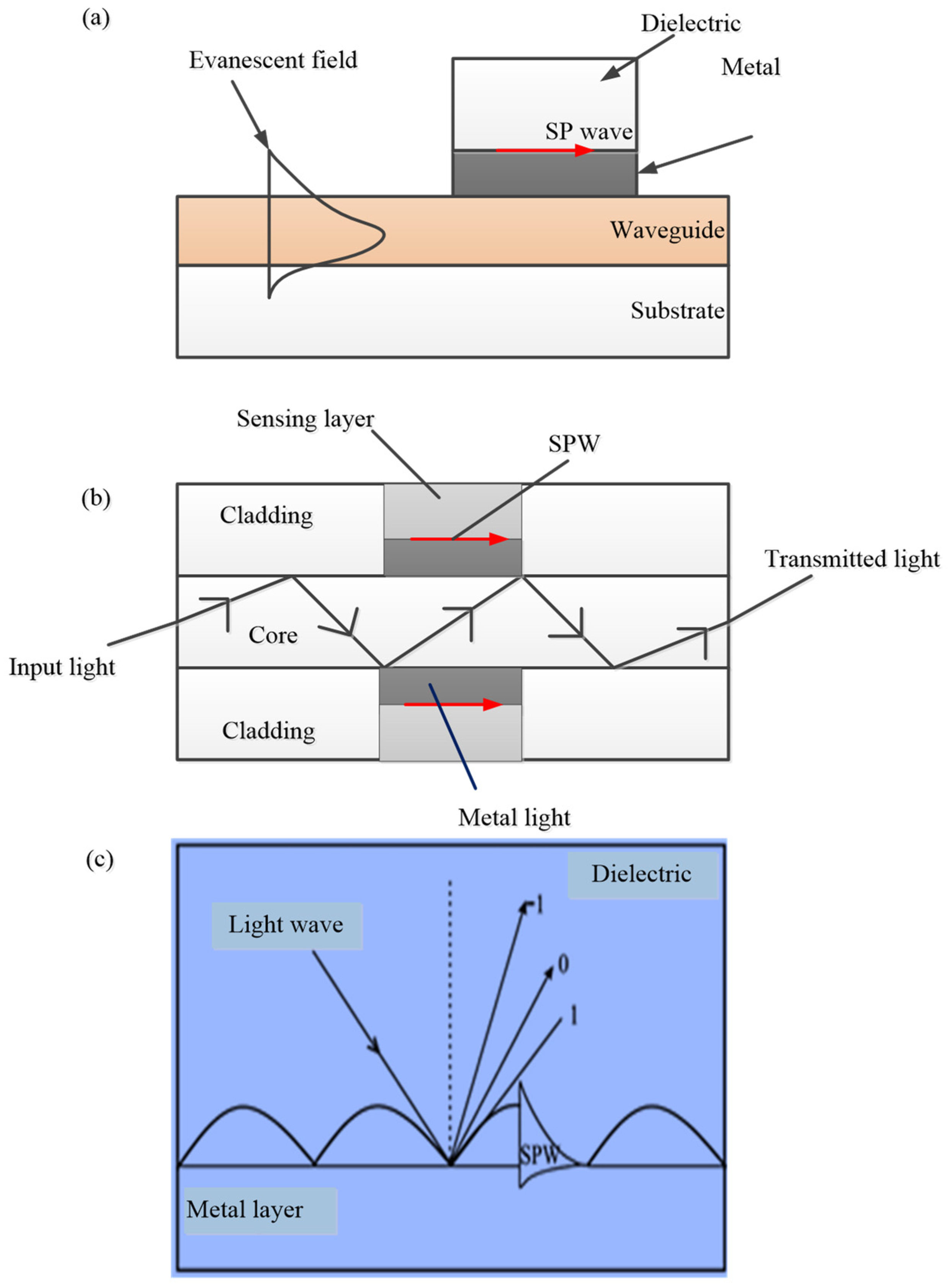
2.1.1. Excitation of Surface Plasmon Waves
- (a)
- Prism couplers
- (b)
- Waveguide couplers
- (c)
- Optical fibre couplers
- (d)
- Grating couplers
2.1.2. Generation of SPR Curve
3. Plasmonic Sensors for the Detection of Lung Cancer Biomarkers
3.1. SPR Biosensors for the Detection of Lung Cancer Biomarkers
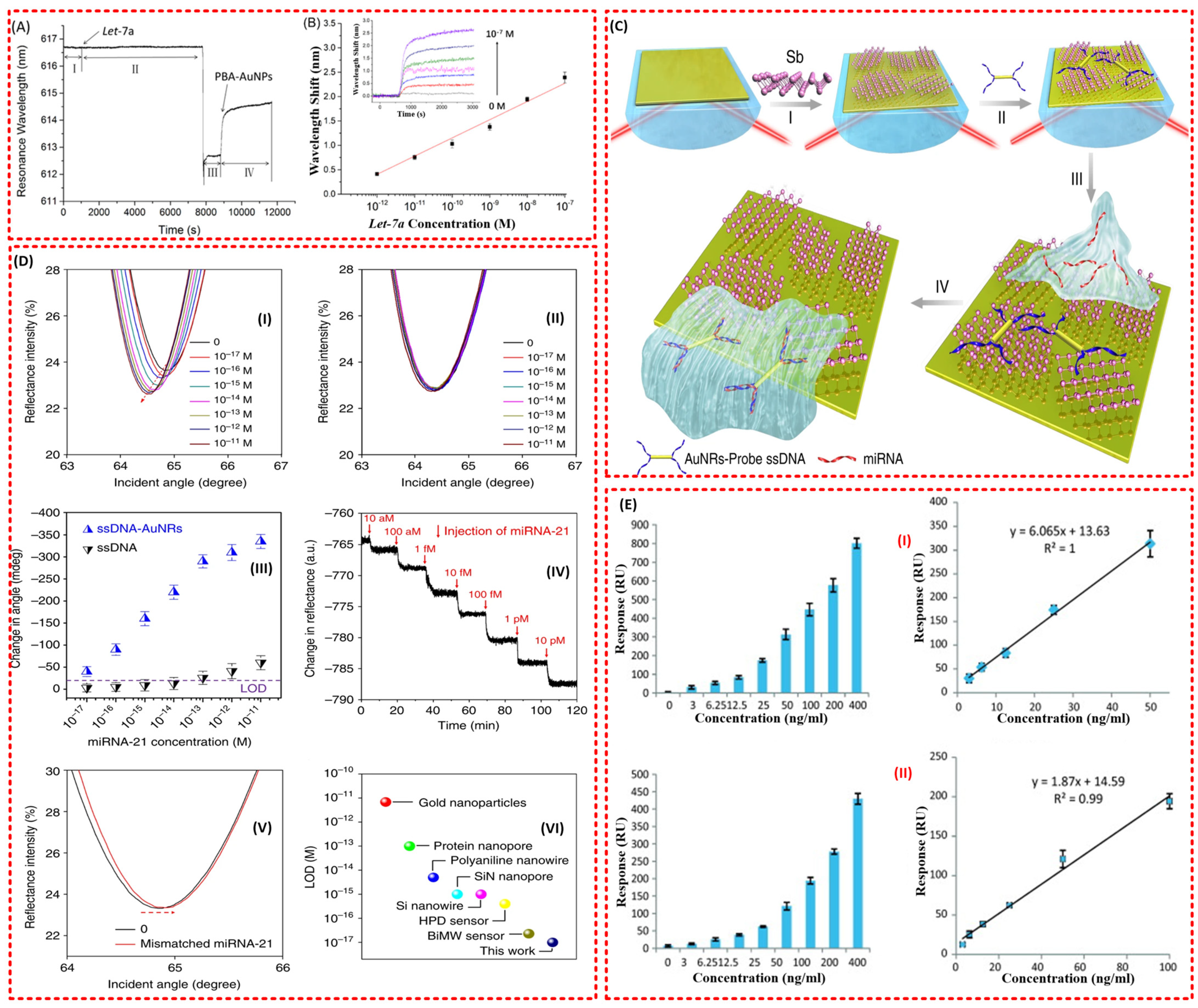
3.1.1. SPR Biosensors for miRNA Detection
3.1.2. SPR Biosensors for Carcinoembryonic Antigen (CEA) Detection
3.1.3. SPR Biosensors for the Detection of Cytokeratin CYFRA 21-1 (CA-19 Fragment or Cytokeratin 19)
3.1.4. SPR Biosensors for the Detection of Volatile Organic Compound (VOC) Biomarkers
3.1.5. SPR Biosensors for the Detection of Other Biomarkers
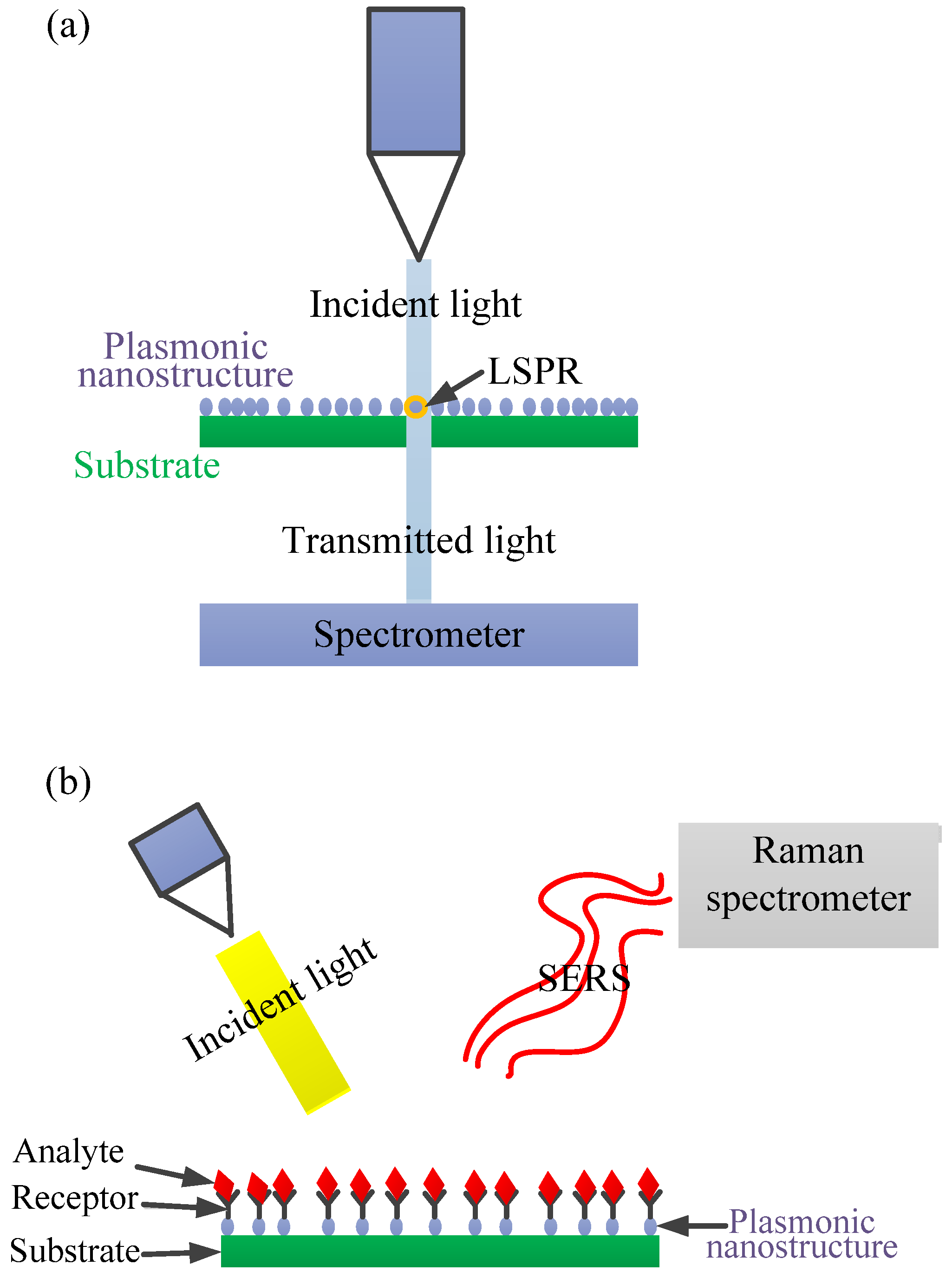
3.2. LSPR Biosensors for the Detection of Lung Cancer Biomarkers
3.2.1. LSPR Biosensors for the Detection of miRNA Biomarkers
3.2.2. LSPR Biosensors for the Detection of Volatile Organic Compound (VOC) Biomarkers
3.2.3. LSPR Biosensors for the Detection of Other Biomarkers
3.3. SERS Biosensors for the Detection of Lung Cancer Biomarkers
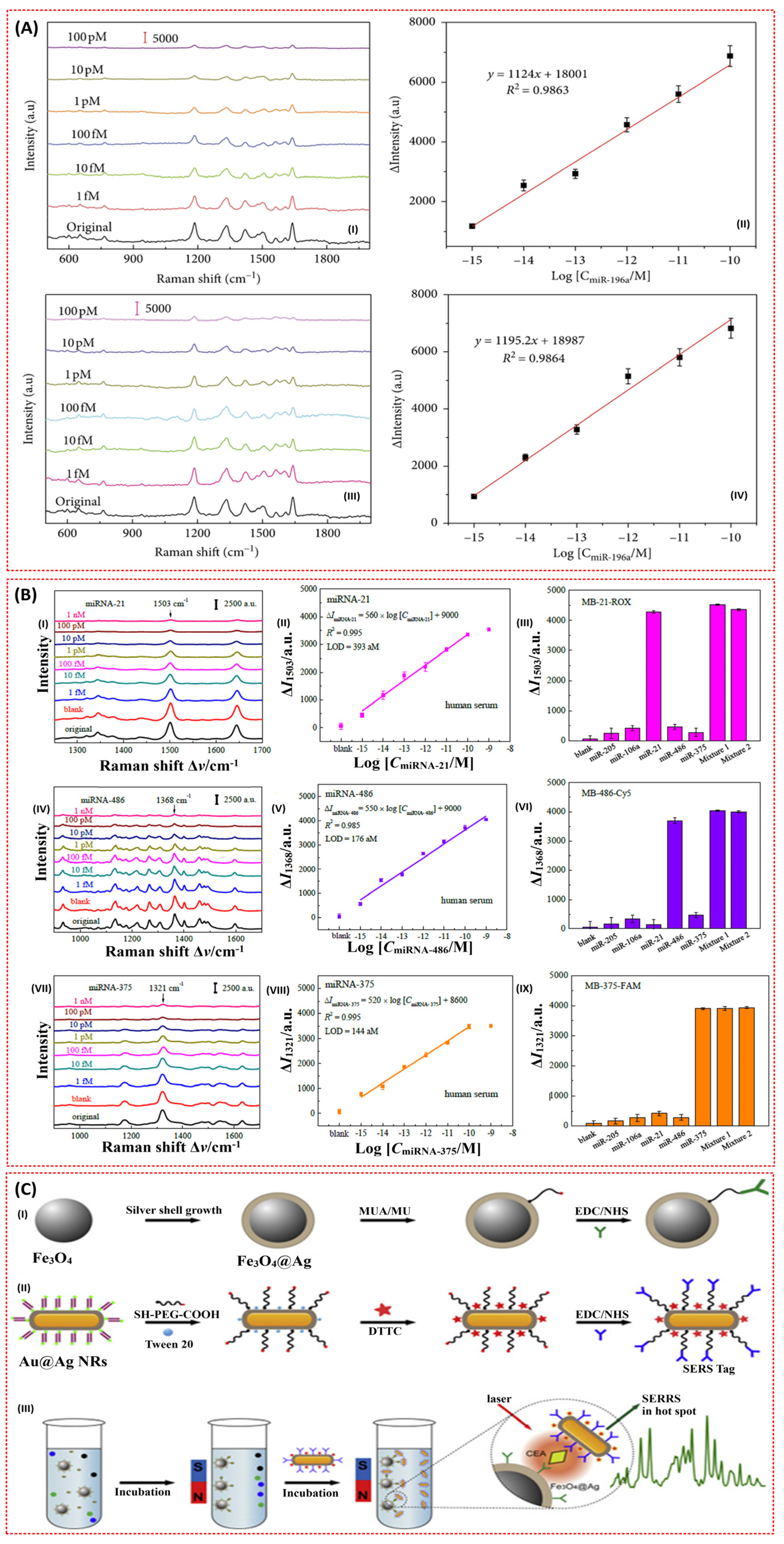
3.3.1. SERS Biosensors for the Detection of miRNA Biomarkers
3.3.2. SERS Biosensors for the Detection of Carcinoembryonic Antigen (CEA) Biomarkers
3.3.3. SERS Biosensors for the Detection of VOC Biomarkers
3.3.4. SERS Biosensors for the Detection of Other Biomarkers
4. Conclusions and Future Outlook
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Available online: https://www.chestnet.org/News/CHEST-News/2020/07/World-Lung-Cancer-Day-2020-Fact-Sheet (accessed on 25 September 2021).
- Jia, Z.; Patra, A.; Kutty, V.K.; Venkatesan, T. Critical review of volatile organic compound analysis in breath and in vitro cell culture for detection of lung cancer. Metabolites 2019, 9, 52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Available online: https://gco.iarc.fr/today/data/factsheets/populations/682-saudi-arabia-fact-sheets.pdf (accessed on 28 September 2021).
- Rudnicka, J.; Kowalkowski, T.; Buszewski, B. Searching for selected VOCs in human breath samples as potential markers of lung cancer. Lung Cancer 2019, 135, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Khanmohammadi, A.; Aghaie, A.; Vahedia, E.; Qazvini, A.; Ghanei, M.; Afkhami, A.; Hajian, A.; Bagheri, H. Electrochemical biosensors for the detection of lung cancer biomarkers: A review. Talanta 2020, 206, 120251. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.N.; Medbery, C.; Sharma, S.; Pablo, J.; Kimsey, F.; Perry, D.; Muacevic, A.; Mahadevan, A. Stereotactic body radiotherapy for centrally located early-stage non-small cell lung cancer or lung metastases from the RSSearch® patient registry. Radiat. Oncol. 2015, 10, 113. [Google Scholar] [CrossRef] [Green Version]
- Wang, L. Screening and biosensor-based approaches for lung cancer detection. Sensors 2017, 17, 2420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altintas, Z.; Uludag, Y.; Gurbuz, Y.; Tothill, I.E. Surface plasmon resonance based immunosensor for the detection of the cancer biomarker carcinoembryonic antigen. Talanta 2011, 86, 377–383. [Google Scholar] [CrossRef] [Green Version]
- Ghosal, R.; Kloer, P.; Lewis, K. A review of novel biological tools used in screening for the early detection of lung cancer. Postgrad. Med. J. 2009, 85, 358–363. [Google Scholar] [CrossRef]
- Saalberg, Y.; Wolff, M. VOC breath biomarkers in lung cancer. Clin. Chim. Acta 2016, 459, 5–9. [Google Scholar] [CrossRef]
- Fourkala, E.-O.; Blyuss, O.; Field, H.; Gunu, R.; Ryan, A.; Barth, J.; Jacobs, I.; Zaikin, A.; Dawnay, A.; Menon, U. Sex hormone measurements using mass spectrometry and sensitive extraction radioimmunoassay and risk of estrogen receptor negative and positive breast cancer: Case control study in UK Collaborative Cancer Trial of Ovarian Cancer Screening (UKCTOCS). Steroids 2016, 110, 62–69. [Google Scholar] [CrossRef]
- Arya, S.K.; Bhansali, S. Lung cancer and its early detection using biomarker-based biosensors. Chem. Rev. 2011, 111, 6783–6809. [Google Scholar] [CrossRef]
- Roointan, A.; Ahmad, T.; Wani, S.I.; Rehman, M.-U.; Hussain, K.K.; Ahmed, B.; Abrahim, S.; Savardashtaki, A.; Gandomani, G.; Gandomani, M.; et al. Early detection of lung cancer biomarkers through biosensor technology: A review. J. Pharm. Biomed. Anal. 2019, 164, 93–103. [Google Scholar] [CrossRef]
- Zhou, J.; Huang, Z.-A.; Kumar, U.; Chen, D.D.Y. Review of recent developments in determining volatile organic compounds in exhaled breath as biomarkers for lung cancer diagnosis. Anal. Chim. Acta 2017, 996, 1–9. [Google Scholar] [CrossRef]
- Busze Buszewski, B.; Ligor, T.; Jezierski, T.; Piesik, A.W.; Walczak, M.; Rudnicka, J. Identification of volatile lung cancer markers by gas chromatography—Mass spectrometry: Comparison with discrimination by canines. Anal. Bioanal. Chem. 2012, 404, 141–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shabaninejada, Z.; Yousefi, F.; Movahedpour, A.; Ghasemi, Y.; Dokanehiifard, S.; Rezaei, S.; Aryan, R.; Savardashtaki, A.; Mirzaei, H. Electrochemical-based biosensors for microRNA detection: Nanotechnology comes into view. Anal. Biochem. 2019, 581, 113349. [Google Scholar] [CrossRef]
- Zhang, Y.; Yang, D.; Weng, L.; Wang, L. Early lung cancer diagnosis by biosensors. Int. J. Mol. Sci. 2013, 14, 15479–15509. [Google Scholar] [CrossRef] [PubMed]
- Lou, J.; Wang, Y.; Tong, L. Microfiber optical sensors: A review. Sensors 2014, 14, 5823–5844. [Google Scholar] [CrossRef] [Green Version]
- Gauglitz, G. Direct optical sensors: Principles and selected applications. Anal. Bioanal. Chem. 2005, 381, 141–155. [Google Scholar] [CrossRef] [PubMed]
- Fraden, J. Handbook of Modern Sensors; Springer: Berlin/Heidelberg, Germany, 2010. [Google Scholar]
- Tuchin, V.V. Handbook of Optical Sensing of Glucose in Biological Fluids and Tissues; CRC Press: Boca Raton, FL, USA, 2008. [Google Scholar]
- Santos, J.L.; Farahi, F. Handbook of Optical Sensors; CRC Press: Boca Raton, FL, USA, 2014. [Google Scholar]
- Chen, X.; Wong, C.K.; Yuan, C.A.; Zhang, G. Nanowire-based gas sensors. Sens. Actuators B Chem. 2013, 177, 178–195. [Google Scholar] [CrossRef]
- Tabassum, R.; Mishra, S.K.; Gupta, B.D. Surface plasmon resonance-based fiber optic hydrogen sulphide gas sensor utilizing Cu–ZnO thin films. Phys. Chem. Chem. Phys. 2013, 15, 11868–11874. [Google Scholar] [CrossRef]
- Ahuja, D.; Parande, D. Optical sensors and their applications. J. Sci. Res. Rev. 2012, 1, 060–068. [Google Scholar]
- Gramotnev, D.K.; Bozhevolnyi, S.I. Plasmonics beyond the diffraction limit. Nat. Photonics 2010, 4, 83–91. [Google Scholar] [CrossRef]
- Barizuddin, S.; Bok, S.; Gangopadhyay, S. Plasmonic sensors for disease detection-a review. J. Nanomed. Nanotechnol. 2016, 7, 1000373. [Google Scholar]
- Cathcart, N.; Chen, J.I.L. Sensing biomarkers with plasmonics. Anal. Chem. 2020, 92, 7373–7381. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhu, X.; Wu, M.; Xia, N.; Wang, J.; Zhou, F. Simultaneous and label-free determination of wild-type and mutant p53 at a single surface plasmon resonance chip preimmobilized with consensus DNA and monoclonal antibody. Anal. Chem. 2009, 81, 8441–8446. [Google Scholar] [CrossRef]
- Kajikawa, K. Sensing Based on Localized Surface Plasmon Resonance in Metallic Nanoparticles. In Nanoparticle Technology Handbook; Elsevier: Amsterdam, The Netherlands, 2018; pp. 631–633. [Google Scholar]
- Barozzi, M.; Manicardi, A.; Vannucci, A.; Candiani, A.; Sozzi, M.; Konstantaki, M.; Pissadakis, S.; Corradini, R.; Selleri, S.; Cucinotta, A. Optical fiber sensors for label-free DNA detection. J. Light. Technol. 2016, 35, 3461–3472. [Google Scholar] [CrossRef]
- Wang, F.; Anderson, M.; Bernards, M.T.; Hunt, H.K. PEG functionalization of whispering gallery mode optical microresonator biosensors to minimize non-specific adsorption during targeted, label-free sensing. Sensors 2015, 15, 18040–18060. [Google Scholar] [CrossRef] [Green Version]
- Verschueren, D.V.; Pud, S.; Shi, X.; De Angelis, L.; Kuipers, L.; Dekker, C. Label-free optical detection of DNA translocations through plasmonic nanopores. ACS Nano 2018, 13, 61–70. [Google Scholar] [CrossRef]
- Shrivastav, A.M.; Cvelbar, U.; Abdulhalim, I. A comprehensive review on plasmonic-based biosensors used in viral diagnostics. Commun. Biol. 2021, 4, 1–12. [Google Scholar] [CrossRef]
- Qiu, G.; Gai, Z.; Tao, Y.; Schmitt, J.; Kullak-Ublick, G.A.; Wang, J.J. Dual-functional plasmonic photothermal biosensors for highly accurate severe acute respiratory syndrome coronavirus 2 detection. ACS Nano 2020, 14, 5268–5277. [Google Scholar] [CrossRef] [Green Version]
- Ahmadivand, A.; Gerislioglu, B.; Ramezani, Z.; Kaushik, A.; Manickam, P.; Ghoreishi, S.A. Functionalized terahertz plasmonic metasensors: Femtomolar-level detection of SARS-CoV-2 spike proteins. Biosens. Bioelectron. 2021, 177, 112971. [Google Scholar] [CrossRef]
- Kim, D.M.; Park, J.S.; Jung, S.-W.; Yeom, J.; Yoo, S.M. Biosensing applications using nanostructure-based localized surface plasmon resonance sensors. Sensors 2021, 21, 3191. [Google Scholar] [CrossRef] [PubMed]
- Song, C.Y.; Yang, Y.J.; Yang, B.Y.; Sun, Y.Z.; Zhao, Y.P.; Wang, L.H. An ultrasensitive SERS sensor for simultaneous detection of multiple cancer-related miRNAs. Nanoscale 2016, 8, 17365–17373. [Google Scholar] [CrossRef]
- Fu, J.-H.; Zhong, Z.; Xie, D.; Guo, Y.-J.; Kong, D.-X.; Zhao, Z.-X.; Zhao, Z.-X.; Li, M. SERS-Active MIL-100 (Fe) Sensory Array for Ultrasensitive and Multiplex Detection of VOCs. Angewandte Chemie 2020, 132, 20670–20679. [Google Scholar] [CrossRef]
- Kooyman, R.P. Physics of surface plasmon resonance. In Handbook of Surface Plasmon Resonance 1; Royal Society of Chemistry: Cambridge, UK, 2008. [Google Scholar]
- Tang, Y.; Zeng, X.; Liang, J. Surface plasmon resonance: An introduction to a surface spectroscopy technique. J. Chem. Educ. 2010, 87, 742–746. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Usman, F.; Dennis, J.O.; Seong, K.C.; Ahmed, A.Y.; Ferrell, T.L.; Fen, Y.W.; Sadrolhosseini, A.R.; Ayodele, O.B.; Meriaudeau, F.; Saidu, A. Enhanced Sensitivity of Surface Plasmon Resonance Biosensor Functionalized with Doped Polyaniline Composites for the Detection of Low-Concentration Acetone Vapour. J. Sens. 2019, 2019, 5786105. [Google Scholar] [CrossRef] [Green Version]
- Gupta, B.D.; Pathak, A.; Semwal, V. Carbon-based nanomaterials for plasmonic sensors: A review. Sensors 2019, 19, 3536. [Google Scholar] [CrossRef] [Green Version]
- Yao, Y.; Yi, B.; Xiao, J.; Li, Z. Surface plasmon resonance biosensors and its application. In Proceedings of the 2007 1st International Conference on Bioinformatics and Biomedical Engineering, Wuhan, China, 6–8 July 2007; pp. 1043–1046. [Google Scholar]
- Mukhtar, W.; Menon, P.S.; Shaari, S.; Malek, M.; Abdullah, A. Angle shifting in surface plasmon resonance: Experimental and theoretical verification. J. Phys. Conf. Ser. 2013, 431, 012028. [Google Scholar] [CrossRef]
- Nivedha, S.; Babu, P.R.; Senthilnathan, K. Surface plasmon resonance: Physics and technology. Curr. Sci. 2018, 115, 00113891. [Google Scholar] [CrossRef]
- Prabowo, B.A.; Purwidyantri, A.; Liu, K.-C. Surface plasmon resonance optical sensor: A review on light source technology. Biosensors 2018, 8, 80. [Google Scholar] [CrossRef] [Green Version]
- Wijaya, E.; Lenaerts, C.; Maricot, S.; Hastanin, J.; Habraken, S.; Vilcot, J.-P.; Boukherroub, R.; Szunerits, S. Surface plasmon resonance-based biosensors: From the development of different SPR structures to novel surface functionalization strategies. Curr. Opin. Solid State Mater. Sci. 2011, 15, 208–224. [Google Scholar] [CrossRef]
- Kurihara, K.; Suzuki, K. Theoretical understanding of an absorption-based surface plasmon resonance sensor based on Kretchmann’s theory. Anal. Chem. 2002, 74, 696–701. [Google Scholar] [CrossRef] [PubMed]
- Ozdemir, S.; Turhan-Sayan, G. Temperature effects on surface plasmon resonance: Design considerations for an optical temperature sensor. J. Lightwave Technol. 2003, 21, 805. [Google Scholar] [CrossRef]
- Srivastava, S.K.; Verma, R.; Gupta, B.D. Theoretical modeling of a self-referenced dual mode SPR sensor utilizing indium tin oxide film. Opt. Commun. 2016, 369, 131–137. [Google Scholar] [CrossRef]
- Ferhan, A.R.; Jackman, J.A.; Park, J.H.; Cho, N.-J.; Kim, D.-H. Nanoplasmonic sensors for detecting circulating cancer biomarkers. Adv. Drug Deliv. Rev. 2018, 125, 48–77. [Google Scholar] [CrossRef] [PubMed]
- Long, Y.-T.; Jing, C. Localized Surface Plasmon Resonance Based Nanobiosensors; Springer: Berlin/Heidelberg, Germany, 2014. [Google Scholar]
- Alharbi, R.; Irannejad, M.; Yavuz, M. A short review on the role of the metal-graphene hybrid nanostructure in promoting the localized surface plasmon resonance sensor performance. Sensors 2019, 19, 862. [Google Scholar] [CrossRef] [Green Version]
- Hong, Y.; Huh, Y.-M.; Yoon, D.S.; Yang, J. Nanobiosensors based on localized surface plasmon resonance for biomarker detection. J. Nanomater. 2012, 2012, 111. [Google Scholar] [CrossRef] [Green Version]
- Pérez-Juste, J.; Pastoriza-Santos, I.; Liz-Marzán, L.M.; Mulvaney, P. Gold nanorods: Synthesis, characterization and applications. Coord. Chem. Rev. 2005, 249, 1870–1901. [Google Scholar] [CrossRef]
- Ganesan, S.; Venkatakrishnan, K.; Tan, B. Wrinkled metal based quantum sensor for In vitro cancer diagnosis. Biosens. Bioelectron. 2020, 151, 111967. [Google Scholar] [CrossRef]
- Potara, M.; Boca, S.; Licarete, E.; Damert, A.; Alupei, M.-C.; Chiriac, M.T.; Popescu, O.; Schmidt, U.; Astilean, S. Chitosan-coated triangular silver nanoparticles as a novel class of biocompatible, highly sensitive plasmonic platforms for intracellular SERS sensing and imaging. Nanoscale 2013, 5, 6013–6022. [Google Scholar] [CrossRef]
- Langer, J.; Aberasturi, D.J.D.; Aizpurua, J.; Alvarez-Puebla, R.A.; Auguié, B.; Baumberg, J.J.; Bazan, G.C.; Bell, S.E.J.; Boisen, A.; Brolo, A.G. Present and future of surface-enhanced Raman scattering. ACS Nano 2019, 14, 28–117. [Google Scholar] [CrossRef] [Green Version]
- Ambros, V.; Bartel, B.; Bartel, D.P.; Burge, C.B.; Carrington, J.C.; Chen, X.; Dreyfuss, G.; Eddy, S.R.; Griffiths-Jones, S.; Marshall, M. A uniform system for microRNA annotation. RNA 2003, 9, 277–279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wahid, F.; Shehzad, A.; Khan, T.; Kim, Y.Y. MicroRNAs: Synthesis, mechanism, function, and recent clinical trials. Biochim. Biophys. Acta 2010, 1803, 1231–1243. [Google Scholar] [CrossRef] [Green Version]
- Qian, S.; Lin, M.; Ji, W.; Yuan, H.; Zhang, Y.; Jing, Z.; Zhao, J.; Masson, J.-F.; Peng, W. Boronic acid functionalized Au nanoparticles for selective microRNA signal amplification in fiber-optic surface plasmon resonance sensing system. ACS Sensors 2018, 3, 929–935. [Google Scholar] [CrossRef] [PubMed]
- Xue, T.; Liang, W.; Li, Y.; Sun, Y.; Xiang, Y.; Zhang, Y.; Dai, Z.; Duo, Y.; Wu, L.; Qi, K. Ultrasensitive detection of miRNA with an antimonene-based surface plasmon resonance sensor. Nat. Commun. 2019, 10, 1–9. [Google Scholar] [CrossRef]
- Singh, M.K.; Pal, S.; Prajapati, Y.; Saini, J. Highly sensitive antimonene based SPR biosensor for miRNA detection. Mater. Today Proc. 2020, 28, 1776–1780. [Google Scholar] [CrossRef]
- Nie, W.; Wang, Q.; Zou, L.; Zheng, Y.; Liu, X.; Yang, X.; Wang, K. Low-fouling surface plasmon resonance sensor for highly sensitive detection of microRNA in a complex matrix based on the DNA tetrahedron. Anal. Chem. 2018, 90, 12584–12591. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.; Yan, Y.; Li, S.; Zhang, Y.; Cheng, W.; Cheng, Q.; Ding, S. Surface plasmon resonance biosensor for highly sensitive detection of microRNA based on DNA super-sandwich assemblies and streptavidin signal amplification. Anal. Chim. Acta 2015, 874, 59–65. [Google Scholar] [CrossRef]
- Mujica, M.L.; Zhang, Y.; Bédioui, F.; Gutiérrez, F.; Rivas, G. Label-free graphene oxide–based SPR genosensor for the quantification of microRNA21. Anal. Bioanal. Chem. 2020, 412, 3539–3546. [Google Scholar] [CrossRef]
- Li, R.; Feng, F.; Chen, Z.-Z.; Bai, Y.-F.; Guo, F.-F.; Wu, F.-Y.; Zhou, G. Sensitive detection of carcinoembryonic antigen using surface plasmon resonance biosensor with gold nanoparticles signal amplification. Talanta 2015, 140, 143–149. [Google Scholar] [CrossRef]
- Teotia, P.K.; Kaler, R. 1-D grating based SPR biosensor for the detection of lung cancer biomarkers using Vroman effect. Opt. Commun. 2018, 406, 188–191. [Google Scholar] [CrossRef]
- Zhou, J.; Tao, F.; Zhu, J.; Lin, S.; Wang, Z.; Wang, X.; Ou, J.-Y.; Li, Y.; Liu, Q.H. Portable tumor biosensing of serum by plasmonic biochips in combination with nanoimprint and microfluidics. Nanophotonics 2019, 8, 307–316. [Google Scholar] [CrossRef]
- Ono, A.; Takahashi, T.; Mori, K.; Akamatsu, H.; Shukuya, T.; Taira, T.; Kenmotsu, H.; Naito, T.; Murakami, H.; Nakajima, T. Prognostic impact of serum CYFRA 21–1 in patients with advanced lung adenocarcinoma: A retrospective study. BMC Cancer 2013, 13, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiu, N.-F.; Yang, H.-T. High-sensitivity detection of the lung cancer biomarker CYFRA21-1 in serum samples using a Carboxyl-MoS2 functional film for SPR-based immunosensors. Front. Bioeng. Biotechnol. 2020, 8, 234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, H.; Wang, X.; Wang, J.; Fu, W.; Yao, C. A SPR biosensor based on signal amplification using antibody-QD conjugates for quantitative determination of multiple tumor markers. Sci. Rep. 2016, 6, 1–9. [Google Scholar] [CrossRef]
- Ribaut, C.; Voisin, V.; Malachovská, V.; Dubois, V.; Mégret, P.; Wattiez, R.; Caucheteur, C. Small biomolecule immunosensing with plasmonic optical fiber grating sensor. Biosens. Bioelectron. 2016, 77, 315–322. [Google Scholar] [CrossRef]
- Chiu, N.-F.; Lin, T.-L.; Kuo, C.-T. Highly sensitive carboxyl-graphene oxide-based surface plasmon resonance immunosensor for the detection of lung cancer for cytokeratin 19 biomarker in human plasma. Sens. Actuators B Chem. 2018, 265, 264–272. [Google Scholar] [CrossRef]
- Ribaut, C.; Voisin, V.; Malachovská, V.; Dubois, V.; Mégret, P.; Wattiez, R.; Caucheteur, C. Cancer biomarker sensing using packaged plasmonic optical fiber gratings: Towards in vivo diagnosis. Biosens. Bioelectron. 2017, 92, 449–456. [Google Scholar] [CrossRef]
- Loyez, M.; Larrieu, J.-C.; Chevineau, S.; Remmelink, M.; Leduc, D.; Bondue, B.; Lambert, P.; Devière, J.; Wattiez, R.; Caucheteur, C. In situ cancer diagnosis through online plasmonics. Biosens. Bioelectron. 2019, 131, 104–112. [Google Scholar] [CrossRef] [Green Version]
- Cainap, C.; Pop, L.A.; Balacescu, O.; Cainap, S.S. Early diagnosis and screening in lung cancer. Am. J. Cancer Res. 2020, 10, 1993. [Google Scholar] [PubMed]
- Horvath, I.; Lazar, Z.; Gyulai, N.; Kollai, M.; Losonczy, G. Exhaled biomarkers in lung cancer. Eur. Respir. J. 2009, 34, 261–275. [Google Scholar] [CrossRef]
- Mehta, B.; Benkstein, K.D.; Semancik, S.; Zaghloul, M.E. Gas sensing with bare and graphene-covered optical nano-antenna structures. Sci. Rep. 2016, 6, 1–10. [Google Scholar] [CrossRef]
- Zhao, Y.; Zaghloul, M.; Lilach, Y.; Benkstein, K.; Semancik, S. Metal Organic Framework-Coated Optical VOC Gas Sensor. In Proceedings of the 2018 IEEE Photonics Conference (IPC), Reston, VA, USA, 30 September–4 October 2018; pp. 1–2. [Google Scholar]
- Sudheer, V.; Kumar, S.S.; Sankararaman, S. Ultrahigh Sensitivity Surface Plasmon Resonance–Based Fiber-Optic Sensors Using Metal-Graphene Layers with Ti3C2Tx MXene Overlayers. Plasmonics 2020, 15, 457–466. [Google Scholar] [CrossRef]
- Li, Y.; Zhang, Y.; Qiu, F.; Qiu, Z. Proteomic identification of exosomal LRG1: A potential urinary biomarker for detecting NSCLC. Electrophoresis 2011, 32, 1976–1983. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Zeng, X.; An, Z.; Yang, Y.; Eisenbaum, M.; Gu, X.; Jornet, J.M.; Dy, G.K.; Reid, M.E.; Gan, Q.; et al. Sensitive detection of exosomal proteins via a compact surface plasmon resonance biosensor for cancer diagnosis. ACS Sensors 2018, 3, 1471–1479. [Google Scholar] [CrossRef]
- Mohammadzadeh-Asl, S.; Aghanejad, A.; de la Guardia, M.; Dolatabadi, J.E.N.; Keshtkar, A. Surface plasmon resonance signal enhancement based on erlotinib loaded magnetic nanoparticles for evaluation of its interaction with human lung cancer cells. Opt. Laser Technol. 2021, 133, 106521. [Google Scholar] [CrossRef]
- Wang, Y.; Zeng, S.; Crunteanu, A.; Xie, Z.; Humbert, G.; Ma, L.; Wei, Y.; Brunel, A.; Bessette, B.; Orlianges, J.-C. Targeted Sub-Attomole Cancer Biomarker Detection Based on Phase Singularity 2D Nanomaterial-Enhanced Plasmonic Biosensor. Nano-Micro Lett. 2021, 13, 1–11. [Google Scholar] [CrossRef]
- Law, W.-C.; Yong, K.-T.; Baev, A.; Prasad, P.N. Sensitivity improved surface plasmon resonance biosensor for cancer biomarker detection based on plasmonic enhancement. ACS Nano 2011, 5, 4858–4864. [Google Scholar] [CrossRef]
- Available online: https://nicoyalife.com/nicoya-surface-plasmon-resonance-resources/what-is-spr/lspr-vs-spr-2/#:~:text=Although%20SPR%20sensors%20have%20a,biomolecular%20binding%20events%20is%20similar.&text=This%20smaller%20sensing%20volume%20means,less%20sensitive%20to%20bulk%20effects (accessed on 30 July 2021).
- Willets, K.A.; Van Duyne, R.P. Localized surface plasmon resonance spectroscopy and sensing. Annu. Rev. Phys. Chem. 2007, 58, 267–297. [Google Scholar] [CrossRef] [Green Version]
- Yonzon, C.R.; Jeoung, E.; Zou, S.; Schatz, G.C.; Mrksich, M.; Van Duyne, R.P. A comparative analysis of localized and propagating surface plasmon resonance sensors: The binding of concanavalin A to a monosaccharide functionalized self-assembled monolayer. J. Am. Chem. Soc. 2004, 126, 12669–12676. [Google Scholar] [CrossRef]
- Liu, Y.; Huang, C.Z. Real-time dark-field scattering microscopic monitoring of the in situ growth of single Ag@ Hg nanoalloys. ACS Nano 2013, 7, 11026–11034. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Zhang, L.; Zhang, Y.; Wang, B.; Wang, Y.; Fan, Q.; Huang, W.; Wang, L. Plasmonic nanobiosensor based on hairpin DNA for detection of trace oligonucleotides biomarker in cancers. ACS Appl. Mater. Interfaces 2015, 7, 2459–2466. [Google Scholar] [CrossRef] [PubMed]
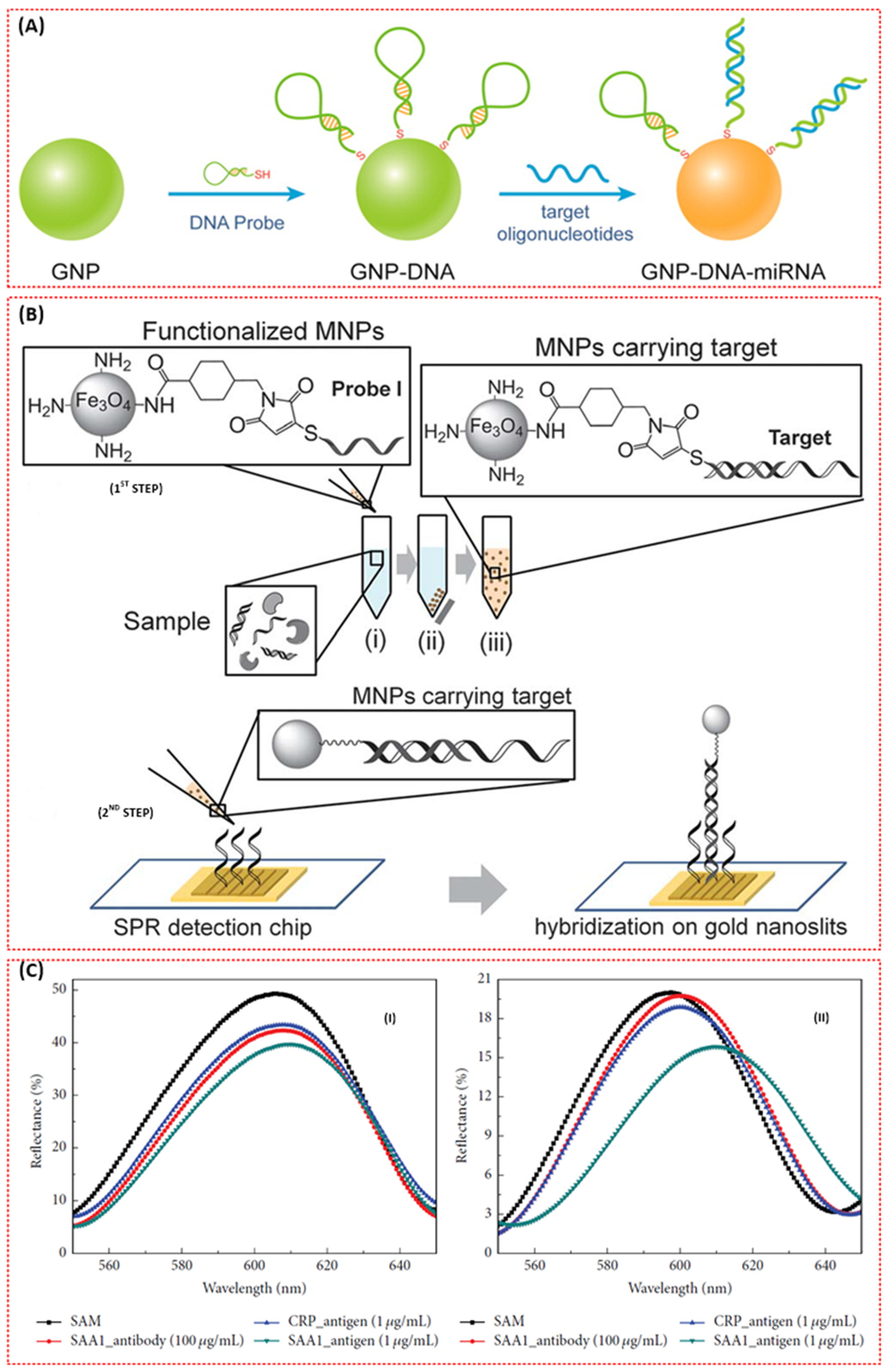
- Mousavi, M.Z.; Chen, H.-Y.; Wu, S.-H.; Peng, S.-W.; Lee, K.-L.; Wei, P.-K.; Cheng, J.-Y. Magnetic nanoparticle-enhanced SPR on gold nanoslits for ultra-sensitive, label-free detection of nucleic acid biomarkers. Analyst 2013, 138, 2740–2748. [Google Scholar] [CrossRef]
- Krishnan, S.; Mani, V.; Wasalathanthri, D.; Kumar, C.V.; Rusling, J.F. Attomolar detection of a cancer biomarker protein in serum by surface plasmon resonance using superparamagnetic particle labels. Angew. Chem. Int. Ed. 2011, 50, 1175–1178. [Google Scholar] [CrossRef]
- Lee, J.-S.; Kim, S.-W.; Jang, E.-Y.; Kang, B.-H.; Lee, S.-W.; Sai-Anand, G.; Lee, S.-H.; Kwon, D.-H.; Kang, S.-W. Rapid and sensitive detection of lung cancer biomarker using nanoporous biosensor based on localized surface plasmon resonance coupled with interferometry. J. Nanomater. 2015, 2015, 1. [Google Scholar] [CrossRef] [Green Version]
- Wang, G.; Guo, Y.; Liu, Y.; Zhou, W.; Wang, G. Algorithm-Assisted Detection and Imaging of microRNAs in Living Cancer Cells via the Disassembly of Plasmonic Core-Satellite Probes Coupled with Strand Displacement Amplification. ACS Sensors 2021, 6, 958–966. [Google Scholar] [CrossRef] [PubMed]
- Portela, A.; Calvo-Lozano, O.; Estevez, M.-C.; Escuela, A.M.; Lechuga, L.M. Optical nanogap antennas as plasmonic biosensors for the detection of miRNA biomarkers. J. Mater. Chem. B 2020, 8, 4310–4317. [Google Scholar] [CrossRef] [PubMed]
- Mühlschlegel, P.; Eisler, H.-J.; Martin, O.J.F.; Hecht, B.; Pohl, D.W. Resonant optical antennas. Science 2005, 308, 1607–1609. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, L.; Zhang, Y.; Hu, Y.; Fan, Q.; Yang, W.; Li, A.; Li, S.; Huang, W.; Wang, L. Refractive index dependent real-time plasmonic nanoprobes on a single silver nanocube for ultrasensitive detection of the lung cancer-associated miRNAs. Chem. Commun. 2014, 51, 294–297. [Google Scholar] [CrossRef]
- Sönnichsen, C.; Reinhard, B.M.; Liphardt, J.; Alivisatos, P. A molecular ruler based on plasmon coupling of single gold and silver nanoparticles. Nat. Biotechnol. 2005, 23, 741–745. [Google Scholar] [CrossRef] [Green Version]
- Ma, D.; Huang, C.; Zheng, J.; Tang, J.; Li, J.; Yang, J.; Yang, R. Quantitative detection of exosomal microRNA extracted from human blood based on surface-enhanced Raman scattering. Biosens. Bioelectron. 2018, 101, 167–173. [Google Scholar] [CrossRef]
- Xia, Y.; Wang, L.; Li, J.; Chen, X.; Lan, J.; Yan, A.; Lei, Y.; Yang, S.; Yang, H.; Chen, J. A ratiometric fluorescent bioprobe based on carbon dots and acridone derivate for signal amplification detection exosomal microRNA. Anal. Chem. 2018, 90, 8969–8976. [Google Scholar] [CrossRef] [PubMed]
- Miti, A.; Sophie, T.; Philipp, M.; Andrea, C.; Wolfgang, F.; Giampaolo, Z. A miRNA biosensor based on localized surface plasmon resonance enhanced by surface-bound hybridization chain reaction. Biosens. Bioelectron. 2020, 167, 112465. [Google Scholar] [CrossRef]
- Wu, W.; Yu, X.; Wu, J.; Wu, T.; Fan, Y.; Chen, W.; Zhao, M.; Wu, H.; Li, X.; Ding, S. Surface plasmon resonance imaging-based biosensor for multiplex and ultrasensitive detection of NSCLC-associated exosomal miRNAs using DNA programmed heterostructure of Au-on-Ag. Biosens. Bioelectron. 2021, 175, 112835. [Google Scholar] [CrossRef]
- Al Mubarak, Z.H.; Premaratne, G.; Dharmaratne, A.; Mohammadparast, F.; Andiappan, M.; Krishnan, S. Plasmonic nucleotide hybridization chip for attomolar detection: Localized gold and tagged core/shell nanomaterials. Lab Chip 2020, 20, 717–721. [Google Scholar] [CrossRef] [PubMed]
- Kreno, L.E.; Leong, K.; Farha, O.K.; Allendorf, M.; Van Duyne, R.P.; Hupp, J.T. Metal–organic framework materials as chemical sensors. Chem. Rev. 2012, 112, 1105–1125. [Google Scholar] [CrossRef]
- Achmann, S.; Hagen, G.; Kita, J.; Malkowsky, I.M.; Kiener, C.; Moos, R. Metal-organic frameworks for sensing applications in the gas phase. Sensors 2009, 9, 1574–1589. [Google Scholar] [CrossRef] [Green Version]
- Kreno, L.E.; Hupp, J.T.; Van Duyne, R.P. Metal− organic framework thin film for enhanced localized surface plasmon resonance gas sensing. Anal. Chem. 2010, 82, 8042–8046. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.; Yang, Y.; Zhang, N.; Ji, D.; Gu, X.; Jornet, J.M.; Wu, Y.; Gan, Q. Plasmonic interferometer array biochip as a new mobile medical device for cancer detection. IEEE J. Sel. Top. Quantum Electron. 2018, 25, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Soler, M.; Belushkin, A.; Cavallini, A.; Kebbi-Beghdadi, C.; Greub, G.; Altug, H. Multiplexed nanoplasmonic biosensor for one-step simultaneous detection of Chlamydia trachomatis and Neisseria gonorrhoeae in urine. Biosens. Bioelectron. 2017, 94, 560–567. [Google Scholar] [CrossRef]
- Li, X.; Soler, M.; Özdemir, C.I.; Belushkin, A.; Yesilköy, F.; Altug, H. Plasmonic nanohole array biosensor for label-free and real-time analysis of live cell secretion. Lab Chip 2017, 17, 2208–2217. [Google Scholar] [CrossRef]
- Sun, X.; Huang, L.; Zhang, R.; Xu, W.; Huang, J.; Gurav, D.D.; Vedarethinam, V.; Chen, R.; Lou, J.; Wang, Q. Metabolic fingerprinting on a plasmonic gold chip for mass spectrometry based in vitro diagnostics. ACS Central Sci. 2018, 4, 223–229. [Google Scholar] [CrossRef] [Green Version]
- Zhu, S.; Li, H.; Yang, M.; Pang, S.W. Label-free detection of live cancer cells and DNA hybridization using 3D multilayered plasmonic biosensor. Nanotechnology 2018, 29, 365503. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Wang, J.; Zhang, J.; Liu, Y.; Wu, L.; Shen, J.; Zhang, Y.; Hu, Y.; Fan, Q.; Huang, W.; et al. Individual Au-nanocube based plasmonic nanoprobe for cancer relevant microRNA biomarker detection. ACS Sensors 2017, 2, 1435–1440. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Li, B.; Chen, L.; Wang, Y.; Gao, D.; Ma, X.; Wu, A. Brushing, a simple way to fabricate SERS active paper substrates. Anal. Methods 2014, 6, 2066–2071. [Google Scholar] [CrossRef]
- Li, B.; Zhang, W.; Chen, L.; Lin, B. A fast and low-cost spray method for prototyping and depositing surface-enhanced Raman scattering arrays on microfluidic paper based device. Electrophoresis 2013, 34, 2162–2168. [Google Scholar] [CrossRef]
- Xia, J.; Liu, Y.; Ran, M.; Lu, D.; Cao, X.; Wang, Y. SERS Platform Based on Bimetallic Au-Ag Nanowires-Decorated Filter Paper for Rapid Detection of miR-196ain Lung Cancer Patients Serum. J. Chem. 2020, 2020, 5073451. [Google Scholar] [CrossRef]
- Fu, X.; Cheng, Z.; Yu, J.; Choo, P.; Chen, L.; Choo, J. A SERS-based lateral flow assay biosensor for highly sensitive detection of HIV-1 DNA. Biosens. Bioelectron. 2016, 78, 530–537. [Google Scholar] [CrossRef]
- Rong, Z.; Wang, C.; Wang, J.; Wang, D.; Xiao, R.; Wang, S. Magnetic immunoassay for cancer biomarker detection based on surface-enhanced resonance Raman scattering from coupled plasmonic nanostructures. Biosens. Bioelectron. 2016, 84, 15–21. [Google Scholar] [CrossRef]
- Tyagi, S.; Kramer, F.R. Molecular beacons: Probes that fluoresce upon hybridization. Nat. Biotechnol. 1996, 14, 303–308. [Google Scholar] [CrossRef]
- Xie, N.; Huang, J.; Yang, X.; Yang, Y.; Quan, K.; Wang, H.; Ying, L.; Ou, M.; Wang, K. A DNA tetrahedron-based molecular beacon for tumor-related mRNA detection in living cells. Chem. Commun. 2016, 52, 2346–2349. [Google Scholar] [CrossRef]
- Chon, H.; Lee, S.; Son, S.W.; Oh, C.H.; Choo, J. Highly sensitive immunoassay of lung cancer marker carcinoembryonic antigen using surface-enhanced Raman scattering of hollow gold nanospheres. Anal. Chem. 2009, 81, 3029–3034. [Google Scholar] [CrossRef]
- Chen, L.; Choo, J. Recent advances in surface-enhanced Raman scattering detection technology for microfluidic chips. Electrophoresis 2008, 29, 1815–1828. [Google Scholar] [CrossRef]
- Lee, S.; Kim, S.; Choo, J.; Shin, S.Y.; Lee, Y.H.; Choi, H.Y.; Ha, S.; Kang, K.; Oh, C.H. Biological imaging of HEK293 cells expressing PLCγ1 using surface-enhanced Raman microscopy. Anal. Chem. 2007, 79, 916–922. [Google Scholar] [CrossRef]
- Qiao, X.; Su, B.; Liu, C.; Song, Q.; Luo, D.; Mo, G.; Wang, T. Selective surface enhanced Raman scattering for quantitative detection of lung cancer biomarkers in superparticle@ MOF structure. Adv. Mater. 2018, 30, 1702275. [Google Scholar] [CrossRef] [PubMed]
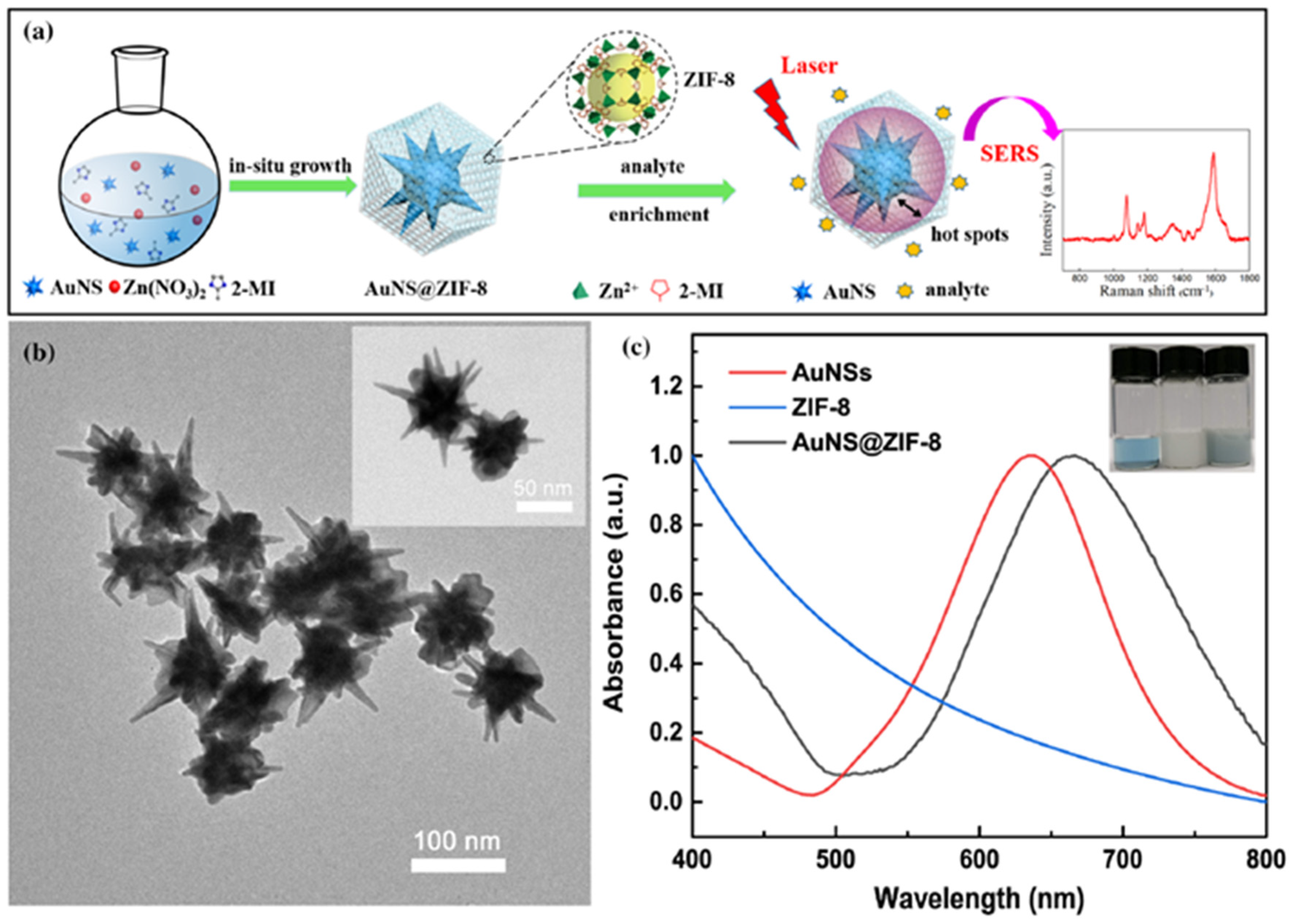
- Fu, Y.; Xin, M.; Chong, J.; Li, R.; Huang, M.J. Plasmonic gold nanostars@ ZIF-8 nanocomposite for the ultrasensitive detection of gaseous formaldehyde. J. Mater. Sci. 2021, 56, 4151–4160. [Google Scholar] [CrossRef]
- Xia, Z.; Li, D.; Deng, W. Identification and Detection of Volatile Aldehydes as Lung Cancer Biomarkers by Vapor Generation Combined with Paper-Based Thin-Film Microextraction. Anal. Chem. 2021, 93, 4924–4931. [Google Scholar] [CrossRef]
- Zhang, Z.; Yu, W.; Wang, J.; Luo, D.; Qiao, X.; Qin, X.; Wang, T. Ultrasensitive surface-enhanced Raman scattering sensor of gaseous aldehydes as biomarkers of lung cancer on dendritic Ag nanocrystals. Anal. Chem. 2017, 89, 1416–1420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wen, H.; Wang, H.; Hai, J.; He, S.; Chen, F.; Wang, B. Photochemical synthesis of porous CuFeSe2/Au heterostructured nanospheres as SERS sensor for ultrasensitive detection of lung cancer cells and their biomarkers. ACS Sustain. Chem. Eng. 2019, 7, 5200–5208. [Google Scholar] [CrossRef]
- Huang, Y.; Xie, T.; Zou, K.; Gu, Y.; Yang, G.-H.; Zhang, F.-L.; Qu, L.-L.; Yang, S. Ultrasensitive SERS detection of exhaled biomarkers of lung cancer using a multifunctional solid phase extraction membrane. Nanoscale 2021, 13, 13344–13352. [Google Scholar] [CrossRef]
- Tian, Y.; Zhou, Y.; Gu, Q.; Qiu, T.; He, X.; Chen, J.; Qi, R.; Huang, R.; Zheng, T. Cu-doping SnO2-NiO pn Heterostructure for Significant Raman Enhancement with EF> 1010: Toward Ultrasensitive VOCs Sensing. Res. Square 2021. [Google Scholar] [CrossRef]
- Yang, T.; Guo, X.; Wu, Y.; Wang, H.; Fu, S.; Wen, Y.; Yang, H. Facile and label-free detection of lung cancer biomarker in urine by magnetically assisted surface-enhanced Raman scattering. ACS Appl. Mater. Interfaces 2014, 6, 20985–20993. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Xin, X.; Zhang, T.; Li, W.; Li, J.; Lu, R. Raspberry-like polyamide@ Ag hybrid nanoarrays with flexible cores and SERS signal enhancement strategy for adenosine detection. Chem. Eng. J. 2021, 422, 129983. [Google Scholar] [CrossRef]
- Zhang, J.; Dong, Y.; Zhu, W.; Xie, D.; Zhao, Y.; Yang, D.; Li, M. Ultrasensitive detection of circulating tumor DNA of lung cancer via an enzymatically amplified SERS-based frequency shift assay. ACS Appl. Mater. Interfaces 2019, 11, 18145–18152. [Google Scholar] [CrossRef]
- Zhang, X.; Zheng, Y.; Liu, X.; Lu, W.; Dai, J.; Lei, D.Y.; MacFarlane, D.R. Hierarchical porous plasmonic metamaterials for reproducible ultrasensitive surface-enhanced Raman spectroscopy. Adv. Mater. 2015, 27, 1090–1096. [Google Scholar] [CrossRef] [PubMed]
- Chen, I.-H.; Xue, L.; Hsu, C.-C.; Paez, J.S.P.; Pan, L.; Andaluz, H.; Wendt, M.K.; Iliuk, A.B.; Zhu, J.-K.; Tao, W.A. Phosphoproteins in extracellular vesicles as candidate markers for breast cancer. Proc. Natl. Acad. Sci. USA 2017, 114, 3175–3180. [Google Scholar] [CrossRef] [Green Version]
- Dong, S.; Wang, Y.; Liu, Z.; Zhang, W.; Yi, K.; Zhang, X.; Zhang, X.; Jiang, C.; Yang, S.; Wang, F. Beehive-inspired macroporous SERS probe for cancer detection through capturing and analyzing exosomes in plasma. ACS Appl. Mater. Interfaces 2020, 12, 5136–5146. [Google Scholar] [CrossRef]
- Qi, D.; Lu, L.; Xi, Z.; Wang, L.; Zhang, J. Enhanced photocatalytic performance of TiO2 based on synergistic effect of Ti3+ self-doping and slow light effect. Appl. Catal. B Environ. 2014, 160, 621–628. [Google Scholar] [CrossRef]
| Type | Disadvantages | Time |
|---|---|---|
| Chest X-ray | Production of radiation, low sensitivity and specificity | Few seconds |
| CT | Costly, high false-positive rate, low sensitivity, production of radiation | 5 min |
| MRI | Costly, not suitable for all cancer types | 40–60 min |
| PET | Costly, requirement of radioactive substance and sophisticated instruments, not suitable for patients with other complications | 90–240 min |
| Classifications | Subclass | Biomarker |
|---|---|---|
| Genetic and epigenetic biomarkers | Mutations, rearrangements, amplifications, or deletions in genes | Epidermal growth factor receptors (c-ErbB-1, c-ErbB-2), K-ras and p53 mutant, FHIT, COX2, RASSFIA, MET, Her2, BRAF, PIK3CA, RET, PTEN, IL-8 Mrna |
| DNA hyper-methylation of genes | SHOX2, CDKN2A, RASSF1A, APC, AC ESR1, HOXA9, CDH13, PRCS3, DAPK | |
| miRNAs | miR-205, miR-210, miR-708, miR-486, miR-21, miR-200b, miR-375, miR-137 | |
| Protein biomarkers | - | CEA, NSE, CYFRA 21-1, vascular endothelial growth factor (VEGF), haptoglobin-R 2, KLKB1, R-enolase (ENO1), APOA1, chromogranin A, TPA, bombesin-like gastrin-releasing peptide, cytokeratin-7, tumour M2-pyruvate kinase, nitrated ceruloplasmin, CD34 and CD59 glycoproteins, transthyretin (TTR), cytokeratin 17 and 18, GM2 activator protein (GM2AP), ProGRP, carbohydrate antigens 19-9, 125 and 15-3 (CA 19-9, CA 125, CA 15-3), annexin II, R-1-acid glycoprotein, protein gene product 9.5 (PGP 9.5), BB isoenzyme of creatine kinase (CK-BB), plasma kallikrein B1, cytokeratin fragment 21-1, and Ig-free light chain |
| VOC | Concentration Trends | Concentration Range in Healthy Subjects (ppb) | Concentration Range in Lung Cancer Patients (ppb) |
|---|---|---|---|
| 1,2,4-trimethyl benzene | ↑ | - | - |
| 2,4-dimethyl heptane | ↑↓ | - | - |
| 3-hydroxy-2-butanone | ↑ | 1.35–3.18 | 1.35–2.86 |
| Acetone | ↑↓ | 44.2–531.45 | 34.57–390.60 |
| Benzene | ↑↓ | 1.38–14.97 | 1.29–3.82 |
| Butane | ↑↓ | - | - |
| Decane | ↑ | - | - |
| Heptane | ↑ | - | - |
| Heptanal | ↑ | - | - |
| Ethanol | ↑↓ | - | - |
| Hexanal | ↑↓ | - | - |
| Isoprene | ↑↓ | - | - |
| Octane | ↑ | - | - |
| Pentane | ↑↓ | 6.84–14.36 | 1.73–17.50 |
| Propyl benzene | ↑ | - | - |
| Styrene | ↑↓ | - | - |
| Toluene | ↑ | 1.45–37.21 | 1.12–17.10 |
| Undecane | ↑ | - | - |
| Cyclohexane | ↑ | - | - |
| Propanol | - | - | 4.37–13.15 |
| Ethyl benzene | ↑ | 2.22–18.38 | 1.45–3.16 |
| Propanal | ↓ | 1.56–3.44 | 1.56–3.74 |
| Pentanal | - | - | - |
| Butanal | - | 1.35–1.87 | 1.32–2.55 |
| Methyl ethyl ketone | - | - | - |
| 2-methyl-1,3-butadiene | - | - | - |
| 2-Pentanone, methyl propyl ketone | ↑ | 1.80–4.11 | 3.25–8.77 |
| Benzaldehyde | ↑ | - | - |
| Methyl cyclopentane | ↑ | - | - |
| Octanal | - | - | - |
| Nonanal | ↑ | - | - |
| Acetyldehyde | ↑↓ | - | - |
| Dimethyl sulfide | ↓ | - | - |
| 4-Methyl octane | ↑ | - | - |
| Propane | - | - | - |
| 2-Methyl pentane, isohexane | ↑ | 2.37–10.80 | 0.93–3.77 |
| S/N | Sensing Layer Material (Functional Material) | Analyte (Biomarker) | Configuration | LOD | Size | Ref. |
|---|---|---|---|---|---|---|
| 1 | Gold layer + SAM + anti-cytokeratin 17 antibody (AbCK17) | Cytokeratin 17 protein (CK17) | Optical fibre SPR | - | Portable | [76] |
| 2 | Gold layer + carboxyl-functionalised Graphene oxide (GO-COOH) composites + anti-CK19 antibody | Cytokeratin 19 biomarker | BI-SPR 3000 | 1 fg/mL. | Bulk | [75] |
| 3 | Gold layer + SAM + anti-CK17 antibodies | Cytokeratin-17 proteins | Optical fibre SPR | - | Portable | [77] |
| 4 | Gold layer + antimonene + AuNR-ssDNA | miRNA (miRNA-21 and miRNA-155) | Prism SPR (kretchmann) | 10 aM | Bulk | [63] |
| 5 | Gold layer + SAM + cytokeratin 7 antibodies (AbCK7) | Cytokeratin 7 (CK7) | Tilt fibre Bragg grating SPR | 0.4 nM. | Portable | [74] |
| 6 | Gold layer + SAM (MUDA) + monoclonal mouse anti-CEA antibody | Carcinoembryonic antigen (CEA) | BIOCORE 3000 SPR | 3 ng/mL | Bulk | [8] |
| 7 | Gold layer + SAM + biotinylated anti-EGFR antibodies, biotinylated anti-PD-L1 antibodies, and biotinylated anti-IgG antibodies | Exosomal protein biomarkers (epidermal growth factor receptor (EGFR) and programmed death-ligand 1 (PD-L1)) | Compact SPR chip | 2 × 1010 exosomes/mL | Portable | [84] |
| 8 | PNA pieces (gold) + SAM (MUA) + anti-CEA (anti-CA 19-9/anti-CA 242) | Carcinoembryonic antigen (CEA) | Compact reflection optical fibre SPR | less than 5 ng/mL | Portable | [70] |
| 9 | Au film + DNA tetrahedron probes (DTPs) | MicroRNA Let-7a | Prism-coupling-based SPR | 0.8 fM | Bulk | [65] |
| 10 | Au film + capture single-stranded DNA (HS-ssDNA) + phenylboronic acid modified AuNPs (PBA-AuNPs) | MicroRNA (miRNA) (Let-7a) | Fibre-optic SPR | 2.7 × 10−13 M (0.27 pM) | - | [62] |
| 11 | Au film + mAbCEA-C3 + CEA+ bio- mAbCEA-B5 antibodies (mAbCEA-C3) + GNPs | Carcinoembryonic antigen (CEA) | Biacore X™ (Uppsala, Sweden) and CM5 sensor chop | 1.0 ng/mL. (SA–GNPs enhanced sandwich Format) | Bulk | [68] |
| 12 | Gold layer + SAM + carboxyl-MoS2 + anti-CYFRA21-1 | Cytokeratin 19 fragment (CYFRA21-1) | BI-SPR 3000 dual channel instrument (Biosensing Instrument Inc., Tempe, AZ, United States) | 0.05 pg/mL | Bulk | [72] |
| 13 | Gold layer + SAM (HDT) + AuNP + SAM (AHT) + anti-CYFRA 21-1 + anti-CYFRA 21-1/quantum dot (QD) conjugates | Cytokeratin fragment 21-1 (CYFRA 21-1) | Prism-coupling-based SPR | 0.1 ng/mL | Bulk | [73] |
| 14 | Gold layer + SAM + microRNA + DNA super-sandwich assemblies and biotin–strepavidin | MicroRNA | Biacore XTM (Prism based SPR) | 9 pM | Bulk | [66] |
| 15 | Au film + antimonene | miRNA | Angular interrogation method based on Kretschmann geometry | - | [64] | |
| 16 | Gold film + 3-mercaptopropane sulfonate (MPS) + poly (diallyldimethylammonium chloride)-graphene oxide (PDDA-GO)2 | miRNA-21 | Single channel autolab e-spr springle instrument (Prism SPR) | 0.3 fM | Bulk | [67] |
| 17 | Metal film (Au, Ag, and Al)/graphene/Ti3C2Tx MXene | Acetone and ethanol | Fibre-optic SPR sensor | - | Portable | [82] |
| 18 | Gold film + monoclonal anti-human TNF-α antibody + antigen + anti-human TNF-α antibody | Tumour necrosis factor alpha (TNF-α) antigen | Prism SPR (phase interrogation) | 0.03 pM | Bulk | [87] |
| 19 | Au film + erlotinib-MNPs | A549 cells | Prism coupling | - | Bulk | [85] |
| 20 | Au film + Ge2Sb2Te5 | TNF-α cancer marker | Phase interrogation-based prism coupling | 10−15 mol/L | Bulk | [86] |
| S/N | Plasmonic Nanostructure | Analyte (Biomarker) | Functional Material | LOD | Size | Ref. |
|---|---|---|---|---|---|---|
| 1 | Gold nanoslits | mRNA (heterogeneous nuclear ribonucleoproteins (hnRNP B1)) | Magnetic nanoparticles (MNPs) | 30 fM | Bulk | [93] |
| 2 | Ring-hole Au nanostructure | Exosomal EGFR (epidermal growth factor receptor) | Biotinylated anti-EGFR antibodies | - | Portable | [109] |
| 3 | Au nanosquares | A549 live cancer cell | O2 plasma treatment | 5×103 cells ml−1 | Bulk | [113] |
| 4 | Nanogap antennas (pairs of goldnanodisks) | miRNA-210 | Complementary DNA capture probe | 0.78 nM | Bulk | [97] |
| 5 | Gold nanoparticles (GNPs) | DNA and miRNA-21 | Single-strand DNA probes (ssDNA) | 3 nM | Bulk | [92] |
| 6 | Silver nanocubes (AgNCs) | MiRNA (miR-21) | Thiolated single-stranded DNA (ssDNA) | 0.1 fM. | Bulk | [99] |
| 7 | Nanoporous anodic aluminum oxide (AAO)-Au | Serum amyloid A1 (SAA1) | SAA1 antibody | 100 ag/mL | Bulk | [95] |
| 8 | Au nanoparticles | miR-17 | DNA hairpin | 1 pM | Bulk | [103] |
| 9 | AgNCs and AuNPs | miRNA-21, miRNA-378, miRNA-200, and miRNA-139 | DNA tetrahedral framework (DTF) and single-stranded DNA (ssDNA) functionalised silver nanocube (AgNC) + ssDNA-AuNPs | 1.68 fM | Bulk | [104] |
| 10 | Au nanoholes | Acetone and ethanol | Cu 1,3,5-benzenetricarboxylic acid (Cu-BTC) metal organic frameworks (MOFs) | 5 μmol/mol | Bulk | [81] |
| 11 | Gold nanocubes (AuNCs) | MicroRNA205 (miR-205) | Single-stranded DNA (ssDNA) | 5 pM | Bulk | [114] |
| 12 | Au50@Au13 core-satellite (DNA/AuNPs) | miRNA-21 | DNA | 2 pM | Less bulky | [96] |
| 13 | Fe3O4@Au NPs | miRNA-155 | DNA | 80 aM | Less bulky | [105] |
| S/N | Plasmonic Nanostructure | Analyte (Biomarker) | Functional Material | LOD | Size | Ref. |
|---|---|---|---|---|---|---|
| 1 | Silver nanotriangles (AgNTs) | Lung cancer cells (A549) | Para-aminothiophenol (p-ATP labelled chitosan | - | Bulk | [58] |
| 2 | CuFeSe2/Au heterostructure nanospheres | Aldehydes and lung cancer cells | 4-aminothiophenol (4-ATP)-aldehydes Folic acid (FA)—lung cancer cells | 1.0 ppb (aldehydes) | Bulk | [129] |
| 3 | Silver-coated AuNRs (Au@Ag NRs) | Carcinoembryonic antigen (CEA) | Detection antibody | 4.75 fg/mL | Bulk | [119] |
| 4 | Ag nanorod array | miRNA-21, miRNA-486, and miRNA-375 | Hairpin-shaped molecular beacons (MBs) | 393 aM (miRNA-21), 176 aM (miRNA-486) and 144 aM (miRNA-375) | Bulk | [38] |
| 5 | Gold superparticles (GSPs) | Gaseous aldehydes | ZIF-8 metal organic framework layer | 10 ppb | Bulk | [125] |
| 6 | Hollow gold nanospheres (HGNs) | Carcinoembryonic antigen (CEA) | Magnetic beads/monoclonal anti-CEA antibodies | 1–10 pg/Ml | Bulk | [122] |
| 7 | Au/Ag nanoparticles | Adenosine | Fe3O4/Au/Ag nanocomposite | 0.5 nM | Portable | [132] |
| 8 | Bimetallic Au-Ag nanowire decorated filter paper | miR-196a | Target hairpin DNA | 96.58 aM (in PBS) and 130 aM (in serum) | Bulk | [117] |
| 9 | Aluminum-based quantum structure (QS) | CEA | - | Femtomolar concentration (10–15 M) | Bulk | [57] |
| 10 | Au-coated TiO2 macroporous inverse opal (MIO) structure | Exosomes | - | - | Bulk | [137] |
| 11 | Gold nanostars | Gaseous formaldehyde | Porous ZIF-8 metal–organic frameworks (MOFs)/4-aminothiophenol (4-ATP) | Parts per billion (ppb) level | Bulk | [126] |
| 12 | Dendritic Ag nanocrystals | Aldehydes | 4-ATP molecules | Parts per billion (ppb) level | Bulk | [128] |
| 13 | Gold nanoparticles | Toluene Acetone and chloroform | MOFs of MIL-100(Fe) composed of Fe clusters and 1,3,5-benzenetricarboxylic acid (TMA) | 0.48 ppb | Bulk | [39] |
| 14 | Silver nanoparticle films (AgNFs) | Circulating tumour DNA (ctDNA) | Hairpin DNA-rN1-DNA probe | 1.2 × 10−16 M | Bulk | [134] |
| 15 | SnO2-NiOx/Cu-Cu | Pyrene (PYR), 2-naphthalenethiol (2-NT) and 4-ethylbenzaldehyde (EBZA) | phthalocyanine | ppb level | Bulk | [131] |
| 16 | Ag NPs@ZIF-67/g-C3N4 | Benzaldehyde | 4-ATP molecules | 1.35 nM | Bulk | [130] |
| 17 | Polyamide-Ag film | Adenosine | MPBA-modified AgNPs (amplification) | 9.83 × 10−10 M | Bulk | [133] |
| 18 | GNRs-QDs@NU- 901 | Benzaldehyde | - | sub-ppb level | Bulk | [127] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Usman, F.; Dennis, J.O.; Aljameel, A.I.; Ali, M.K.M.; Aldaghri, O.; Ibnaouf, K.H.; Zango, Z.U.; Beygisangchin, M.; Alsadig, A.; Meriaudeau, F. Plasmonic Biosensors for the Detection of Lung Cancer Biomarkers: A Review. Chemosensors 2021, 9, 326. https://doi.org/10.3390/chemosensors9110326
Usman F, Dennis JO, Aljameel AI, Ali MKM, Aldaghri O, Ibnaouf KH, Zango ZU, Beygisangchin M, Alsadig A, Meriaudeau F. Plasmonic Biosensors for the Detection of Lung Cancer Biomarkers: A Review. Chemosensors. 2021; 9(11):326. https://doi.org/10.3390/chemosensors9110326
Chicago/Turabian StyleUsman, Fahad, John Ojur Dennis, A.I. Aljameel, M.K.M. Ali, O. Aldaghri, K.H. Ibnaouf, Zakariyya Uba Zango, Mahnoush Beygisangchin, Ahmed Alsadig, and Fabrice Meriaudeau. 2021. "Plasmonic Biosensors for the Detection of Lung Cancer Biomarkers: A Review" Chemosensors 9, no. 11: 326. https://doi.org/10.3390/chemosensors9110326
APA StyleUsman, F., Dennis, J. O., Aljameel, A. I., Ali, M. K. M., Aldaghri, O., Ibnaouf, K. H., Zango, Z. U., Beygisangchin, M., Alsadig, A., & Meriaudeau, F. (2021). Plasmonic Biosensors for the Detection of Lung Cancer Biomarkers: A Review. Chemosensors, 9(11), 326. https://doi.org/10.3390/chemosensors9110326










