Accreditation and Certification: Do They Improve Hospital Financial and Quality Performance?
Abstract
:1. Introduction
1.1. Accreditation and Professional Certification Costs
1.2. Accreditation and Professional Certification Marketing
1.3. Research Question
1.4. Significance
2. Literature
3. Theoretical Model
4. Materials and Methods
4.1. Data
Unit of Analysis, Location, and Variables
4.2. Dependent Variables
4.3. Independent Variables
4.4. Models
4.5. Software
5. Analyses and Results
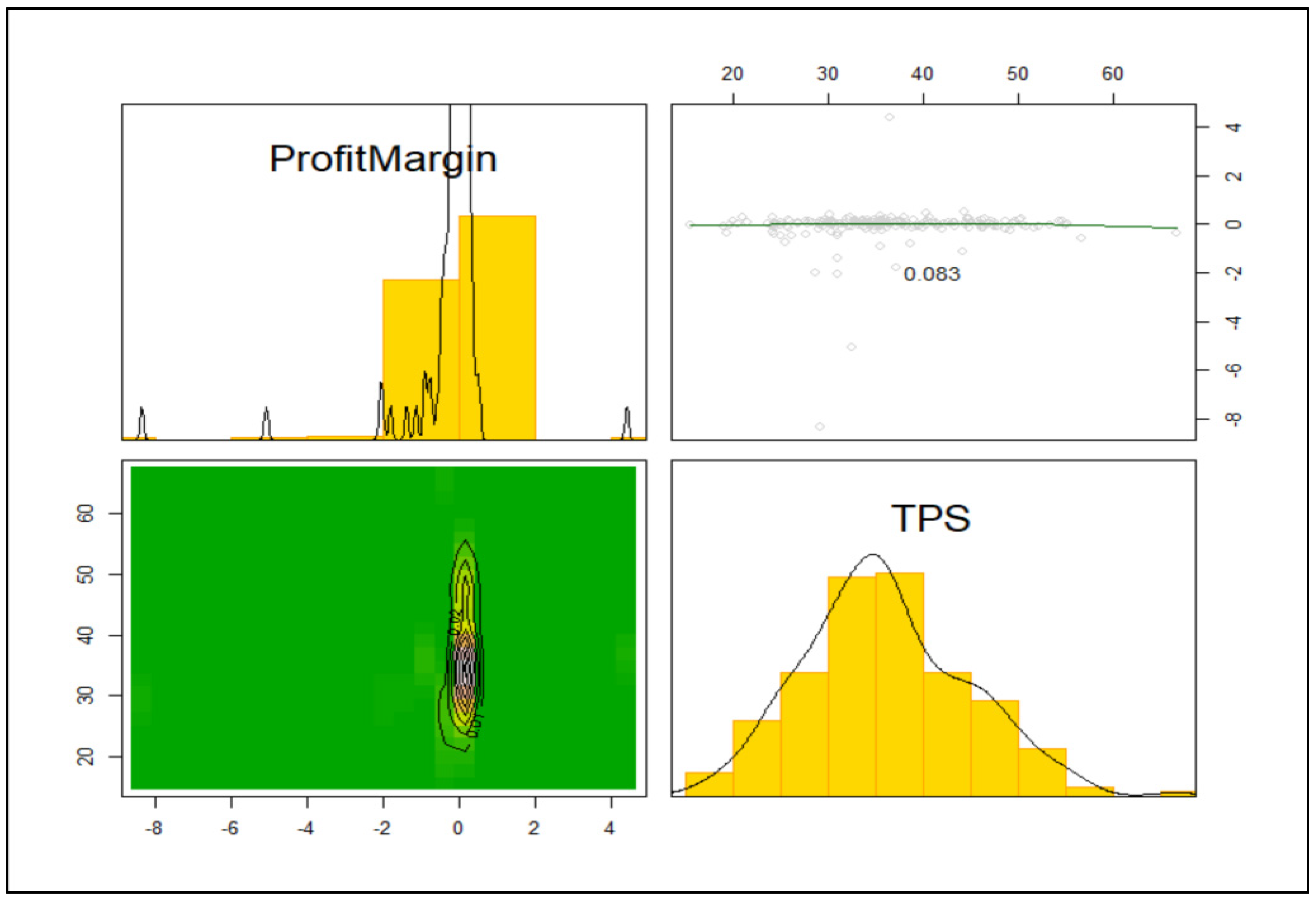
5.1. Dependent Variables Descriptive Statistics
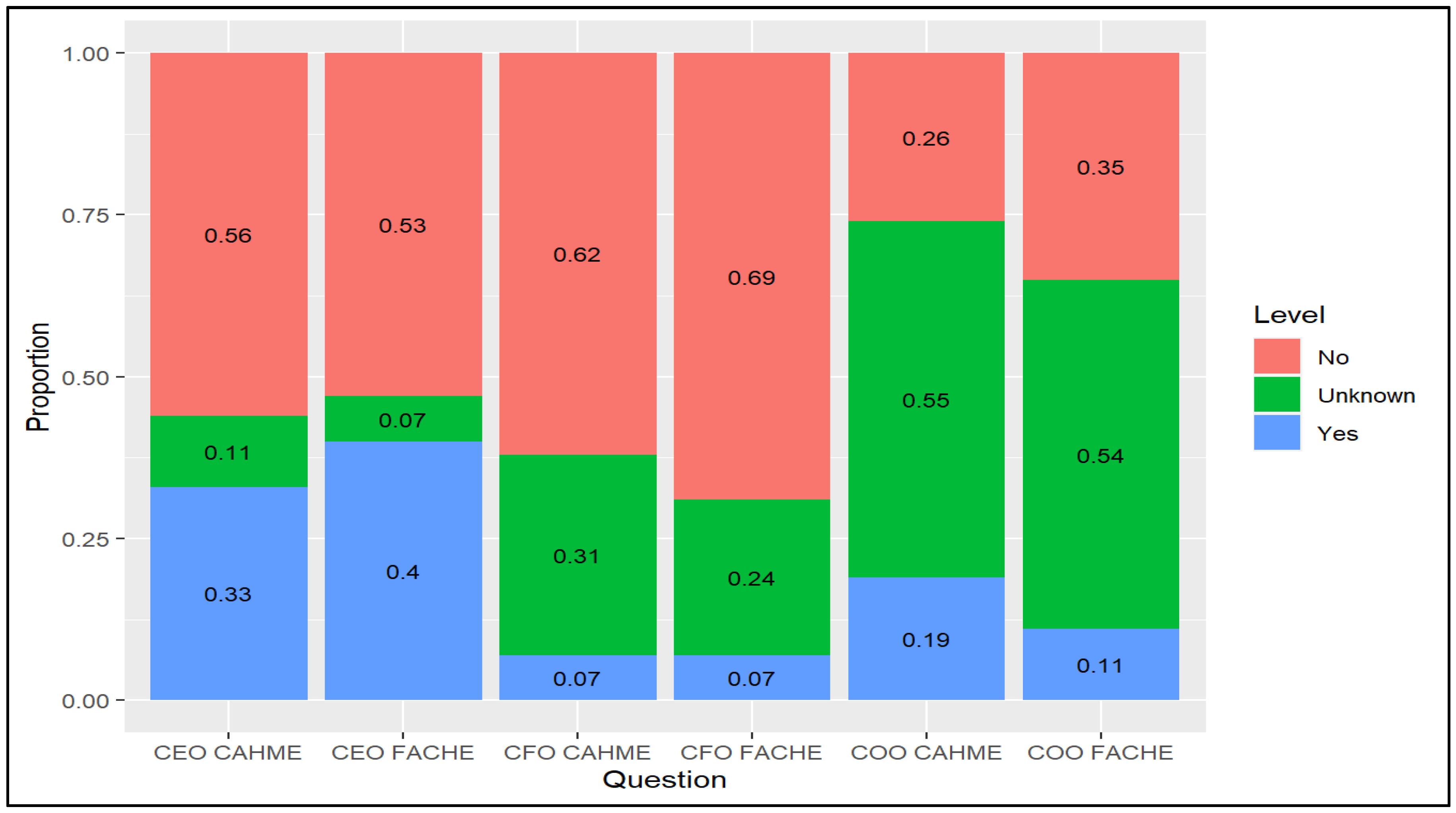
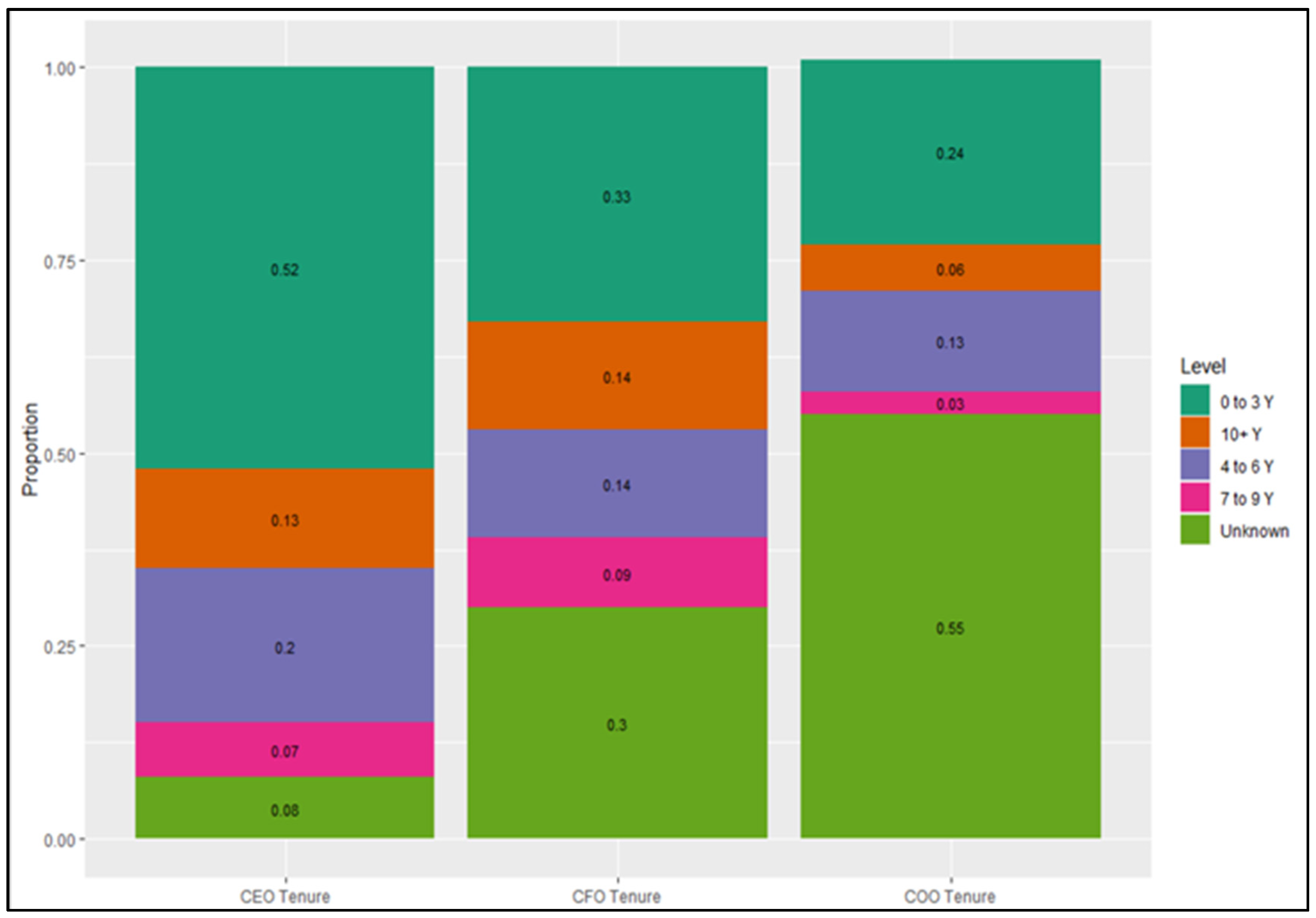
5.2. Independent Variable Descriptive Statistics
6. Models
6.1. Operating Profit Margin
6.2. Total Performance Score
7. Discussion
8. Limitations and Future Research
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- O’Connor, S.J.; Borkowski, N.; Qu, H.; Ivankova, N.V.; Davlyatov, G.K.; Williams, E.S. Stakeholders’ Perception of CAHME- Accredited Graduate Programs in Healthcare Management: A Mixed- Methods Approach. J. Health Adm. Educ. 2020, 37, 7–24. [Google Scholar]
- Kissick, W. Medicine’s Dilemmas: Infinite Needs Versus Finite Resources; Yale University Press: New Haven, CT, USA, 1994. [Google Scholar]
- Crossing the Quality Chasm: A New Health System for the 21st Century; National Academy Press: Washington, DC, USA, 2001.
- Tikkanen, R.; Abrams, M.K.U.S. Health Care from a Global Perspective, 2019: Higher Spending, Worse Outcomes? Available online: https://www.commonwealthfund.org/publications/issue-briefs/2020/jan/us-health-care-global-perspective-2019 (accessed on 31 August 2020).
- Araujo, C.A.S.; Siqueira, M.M.; Malik, A.M. Hospital accreditation impact on healthcare quality dimensions: A systematic review. Int. J. Qual. Health Care 2020, 32, 531–544. [Google Scholar] [CrossRef]
- Lam, M.B.; Figueroa, J.F.; Feyman, Y.; Reimold, K.E.; Orav, E.J.; Jha, A.K. Association between patient outcomes and accreditation in US hospitals: Observational study. BMJ 2018, 363, k4011. [Google Scholar] [CrossRef] [Green Version]
- Mumford, V.; Forde, K.; Greenfield, D.; Hinchcliff, R.; Braithwaite, J. Health services accreditation: What is the evidence that the benefits justify the costs? Int. J. Qual. Health Care 2013, 25, 606–620. [Google Scholar] [CrossRef]
- Greenfield, D.; Braithwaite, J. Health sector accreditation research: A systematic review. Int. J. Qual. Health Care 2008, 20, 172–183. [Google Scholar] [CrossRef]
- Silvernail, T.S.; Coates, H.R.; Fulton, L.V.; Childress, C.Y. Exploring the U.S. News and World Report Rankings of Masters-Level Graduate Health Management Programs. J. Health Adm. Educ. 2009, 26, 293–307. [Google Scholar]
- Ramamonjiarivelo, Z.; Lieneck, C.; Kruse, C.S.; Greene, L.; Fulton, L. Assessing the Impact of Professional Certifications on Time-to-Hire, Job Satisfaction, and Career Growth of Health Administration Alumni. J. Health Adm. Educ. 2020, 37, 25–44. [Google Scholar]
- Whitehead, L.; Ghosh, M.; Walker, D.K.; Bloxsome, D.; Vafeas, C.; Wilkinson, A. The relationship between specialty nurse certification and patient, nurse and organizational outcomes: A systematic review. Int. J. Nurs. Stud. 2019, 93, 1–11. [Google Scholar] [CrossRef]
- Parks, R.B. Costs of Programmatic Accreditation for Allied Health Education in the CAHEA [Committee on Allied Health Education and Accreditation] System: 1980. Executive Summary. 1981. Available online: https://eric.ed.gov/?id=ED215736 (accessed on 10 September 2020).
- Commission on Accreditation of Healthcare Management Education. 2020. Available online: https://cahme.org/ (accessed on 27 August 2020).
- Association of University Programs in Health Administration. 2020. Available online: https://www.aupha.org/certification/certification (accessed on 6 March 2021).
- American College of Healthcare Executives. Available online: www.ache.org (accessed on 27 August 2020).
- Davis, D.J.; Ringsted, C. Accreditation of undergraduate and graduate medical education: How do the standards contribute to quality? Adv. Health Sci. Educ. 2006, 11, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Barzansky, B.; Hunt, D.; Moineau, G.; Ahn, D.; Lai, C.-W.; Humphrey, H.; Peterson, L. Continuous quality improvement in an accreditation system for undergraduate medical education: Benefits and challenges. Med. Teach. 2015, 37, 1032–1038. [Google Scholar] [CrossRef] [PubMed]
- Anderson, M.M.; Garman, A.N. Preparing Future Healthcare Leaders through Graduate Education Impact of Program Accreditation on Quality Improvement. J. Allied Health 2018, 47, 121–125. [Google Scholar]
- Bowen, D.J.; Hahn, C.A. Credentialing for health care leaders: An overview of ACHE’s FACHE credential and its contributions to the health care management field. World Hosp. Health Serv. Off. J. Int. Hosp. Fed. 2012, 48, 30–32. [Google Scholar]
- Khaliq, A.A.; Walston, S.L. Predictors of hospital CEO affiliation with a professional association. J. Healthc. Manag. 2012, 57, 358–373. [Google Scholar] [CrossRef]
- Mata, H.; Latham, T.P.; Ransome, Y. Benefits of professional organization membership and participation in national conferences: Considerations for students and new professionals. Health Promot. Pract. 2010, 11, 450–453. [Google Scholar] [CrossRef]
- Escoffery, C.; Kenzig, M.; Hyden, C. Getting the most out of professional associations. Health Promot. Pract. 2015, 16, 309–312. [Google Scholar] [CrossRef]
- Gerard, N. Perils of professionalization: Chronicling a crisis and renewing the potential of healthcare management. Health Care Anal. 2019, 27, 269–288. [Google Scholar] [CrossRef]
- DiMaggio, P.J.; Powell, W.W. The iron cage revisited: Institutional isomorphism and collective rationality in organizational fields. Am. Sociol. Rev. 1983, 48, 147–160. [Google Scholar] [CrossRef] [Green Version]
- Alyahya, M.; Hijazi, H.; Harvey, H. Explaining the accreditation process from the institutional isomorphism perspective: A case study of Jordanian primary healthcare centers. Int. J. Health Plan. Manag. 2018, 33, 102–120. [Google Scholar] [CrossRef]
- Romero, E.J. AACSB Accreditation: Addressing Faculty Concerns. Acad. Manag. Learn. Educ. 2008, 7, 245–255. [Google Scholar] [CrossRef]
- Zhao, J.; Ferran, C. Business school accreditation in the changing global marketplace: A comparative study of the agencies and their competitive strategies. J. Int. Educ. Bus. 2016, 9, 52–69. [Google Scholar] [CrossRef]
- Janis, I.L. Victims of Groupthink: A Psychological Study of Foreign-Policy Decisions and Fiascoes; Houghton Mifflin: Oxford, UK, 1972. [Google Scholar]
- Turner, M.E.; Pratkanis, A.R. Twenty-five years of groupthink theory and research: Lessons from the evaluation of a theory. Organ. Behav. Hum. Decis. Process. 1998, 73, 105–115. [Google Scholar] [CrossRef] [Green Version]
- Bang, D.; Frith, C.D. Making better decisions in groups. R. Soc. Open Sci. 2017, 4, 170193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Definitive Healthcare. Available online: https://www.definitivehc.com/ (accessed on 27 August 2020).
- Hospital Compare. Available online: https://www.medicare.gov/hospitalcompare/data/total-performance-scores.html (accessed on 27 August 2020).
- Microsoft Corporation. Microsoft Excel [Internet]. 2016. Available online: https://office.microsoft.com/excel (accessed on 27 August 2020).
- Team, R.C. R: A Language and Environment for Statistical Computing. 2018. Available online: https://www.R-project.org/ (accessed on 27 August 2020).
- Zou, H.; Hastie, T. Regularization and variable selection via the elastic net. J. R. Stat. Soc. Ser. B Stat. Methodol. 2005, 67, 301–320. [Google Scholar] [CrossRef] [Green Version]
- Tibshirani, R. Regression shrinkage and selection via the lasso. J. R. Stat. Soc. Ser. B Methodol. 1996, 58, 267–268. [Google Scholar] [CrossRef]
- Horel, A.E. Applications of Ridge Analysis Toregression Problems. Chem. Eng. Progress. 1962, 58, 54–59. [Google Scholar]
- Friedman, J.H.; Hastie, T.; Tibshirani, R. Regularization Paths for Generalized Linear Models via Coordinate Descent. J. Stat. Softw. 2010, 33, 22. [Google Scholar] [CrossRef] [Green Version]
| Variables | Definition | Type | Source | Reason |
|---|---|---|---|---|
| Total Performance Score | Weighted Linear Combination of Subordinate Metrics | Quantitative | Centers for Medicare & Medicaid Services | |
| Net Operating Profit Margin | Operating Profit/Net Sales | Quantitative | Definitive Healthcare | |
| 2020 Population Estimate | City of Hospital Population | Quantitative | U.S. Census Bureau | Demographic Control |
| 2020 Population Density | Population/square meter | Quantitative | U.S. Census Bureau | Demographic Control |
| Native American | County % Native American | Quantitative | U.S. Census Bureau | Demographic Control |
| Black/African American | County % African American | Quantitative | U.S. Census Bureau | Demographic Control |
| Proportion over 65 | % over 65 | Quantitative | U.S. Census Bureau | Demographic Control |
| Unemployment, 2019 | County Unemployment Rate | Quantitative | U.S. Census Bureau (BLS) | Economic Control |
| Household Income, 2018 | Median County Income | Quantitative | U.S. Census Bureau | Economic Control |
| Adult Obesity | Rate/100 K | Quantitative | Centers for Disease Prevention and Control | Health Status Control |
| Cancer | Rate/100 K | Quantitative | Centers for Disease Prevention and Control | Health Status Control |
| COPD | Rate/100 K | Quantitative | Centers for Disease Prevention and Control | Health Status Control |
| Diabetes | Rate/100 K | Quantitative | Centers for Disease Prevention and Control | Health Status Control |
| Heart Failure | Rate/100 K | Quantitative | Centers for Disease Prevention and Control | Health Status Control |
| Case Mix Index | Complexity Adjustment | Quantitative | Centers for Disease Prevention and Control | Case Complexity Control |
| CEO Tenure | What is the CEO’s tenure? | {<=3, 4–6, 7–9, 10–12, 13–16, 16+, unknown} years | Secondary Source Mining (Hospital Websites, Linked-In) | Experience Control |
| COO Tenure | What is the COO’s tenure? | {<=3, 4–6, 7–9, 10–12, 13–16, 16+, unknown} years | Secondary Source Mining (Hospital Websites, Linked-In) | Experience Control |
| CFO Tenure | What is the CFO’s tenure? | {<=3, 4–6, 7–9, 10–12, 13–16, 16+, unknown} years | Secondary Source Mining (Hospital Websites, Linked-In) | Experience Control |
| CEO CAHME Status | CEO from CAHME-accredited university? | Qualitative, {No, Yes, Unknown} | Secondary Source Mining (Hospital Websites, Linked-In) | Predictor of Interest |
| COO CAHME Status | COO from CAHME-accredited university? | Qualitative, {No, Yes, Unknown} | Secondary Source Mining (Hospital Websites, LinkedIn) | Predictor of Interest |
| CFO CAHME Status | CFO from CAHME-accredited university? | Qualitative, {No, Yes, Unknown} | Secondary Source Mining (Hospital Websites, LinkedIn) | Predictor of Interest |
| CEO FACHE Status | CEO holds FACHE? | Qualitative, {No, Yes, Unknown} | Secondary Source Mining (Hospital Websites, LinkedIn) | Predictor of Interest |
| COO FACHE Status | COO holds FACHE? | Qualitative, {No, Yes, Unknown} | Secondary Source Mining (Hospital Websites, LinkedIn) | Predictor of Interest |
| CFO FACHE Status | CFO holds FACHE? | Qualitative, {No, Yes, Unknown} | Secondary Source Mining (Hospital Websites, LinkedIn) | Predictor of Interest |
| Do any of the CEO, COO, CFO have credentials/come from CAHME programs? | Recoded response based on previous 6 questions | Qualitative, {No, Yes} | Feature Engineering | Predictor of Interest |
| Variable | Mean | SD | Median | Minimum | Maximum |
|---|---|---|---|---|---|
| Profit Margin | −0.086 | 0.830 | 0.031 | −8.349 | 4.424 |
| TPS | 36.061 | 8.614 | 35.500 | 15.500 | 66.670 |
| County Population | 1,196,559.633 | 1,493,919.487 | 423,163.000 | 7306.000 | 4,713,325.000 |
| Population Density | 22,299.124 | 38,486.127 | 5453.706 | 856.992 | 246,914.129 |
| Native American | 0.003 | 0.002 | 0.002 | 0.000 | 0.014 |
| Hispanic American | 0.375 | 0.215 | 0.339 | 0.066 | 0.991 |
| African American | 0.111 | 0.075 | 0.094 | 0.000 | 0.335 |
| Age 65+ | 0.135 | 0.035 | 0.122 | 0.095 | 0.301 |
| Unemployment | 3.570 | 0.940 | 3.300 | 2.100 | 9.800 |
| Income | 59,678.804 | 15,568.709 | 59,838.000 | 30,490.000 | 102,858.000 |
| Adult Obese/100 K | 31.117 | 4.643 | 30.000 | 21.800 | 47.300 |
| Cancer/100 K | 7.582 | 0.923 | 7.701 | 4.376 | 9.088 |
| COPD/100 K | 11.447 | 2.634 | 10.760 | 7.286 | 18.890 |
| Diabetes/100 K | 29.544 | 4.853 | 28.681 | 19.646 | 47.152 |
| Heart Failure/100 K | 15.855 | 2.871 | 15.589 | 10.345 | 27.965 |
| Case Mix Index | 1.737 | 0.308 | 1.817 | 0.980 | 2.234 |
| Any FACHE Certification | 0.503 | 0.510 | 1.000 | 0.000 | 1.000 |
| Any CAHME Certification | 0.492 | 0.501 | 0.000 | 0.000 | 1.000 |
| Any Certification | 0.764 | 0.426 | 1.000 | 0.000 | 1.000 |
| Variable | Estimate | Std. Error | t Value | Pr (>|t|) |
|---|---|---|---|---|
| Native | −0.173 | 0.069 | −2.509 | 0.013 |
| Population Density | 0.163 | 0.070 | 2.341 | 0.020 |
| Any Certification | −0.225 | 0.069 | −3.273 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brooks, M.; Beauvais, B.M.; Kruse, C.S.; Fulton, L.; Mileski, M.; Ramamonjiarivelo, Z.; Shanmugam, R.; Lieneck, C. Accreditation and Certification: Do They Improve Hospital Financial and Quality Performance? Healthcare 2021, 9, 887. https://doi.org/10.3390/healthcare9070887
Brooks M, Beauvais BM, Kruse CS, Fulton L, Mileski M, Ramamonjiarivelo Z, Shanmugam R, Lieneck C. Accreditation and Certification: Do They Improve Hospital Financial and Quality Performance? Healthcare. 2021; 9(7):887. https://doi.org/10.3390/healthcare9070887
Chicago/Turabian StyleBrooks, Matthew, Brad M. Beauvais, Clemens Scott Kruse, Lawrence Fulton, Michael Mileski, Zo Ramamonjiarivelo, Ramalingam Shanmugam, and Cristian Lieneck. 2021. "Accreditation and Certification: Do They Improve Hospital Financial and Quality Performance?" Healthcare 9, no. 7: 887. https://doi.org/10.3390/healthcare9070887
APA StyleBrooks, M., Beauvais, B. M., Kruse, C. S., Fulton, L., Mileski, M., Ramamonjiarivelo, Z., Shanmugam, R., & Lieneck, C. (2021). Accreditation and Certification: Do They Improve Hospital Financial and Quality Performance? Healthcare, 9(7), 887. https://doi.org/10.3390/healthcare9070887









