Abstract
(1) Background: a review of the literature found a lack of standardized pediatric guidelines regarding wound management after cardiac surgery. (2) Objective: the aim of the study is to investigate the cardiac surgical wound management in Italian pediatric cardiac intensive care units. (3) Methods: we sent an online questionnaire to the 13 Italian pediatric cardiac intensive care units. (4) Results: ten pediatric cardiac intensive care units (77%) have a protocol for the management of the cardiac surgical wound. The staff members that mainly have the responsibility for the wound management after cardiac surgery are registered nurses and physicians together both in the pediatric cardiac intensive care units (69%), and when a patient is transferred to another ward (62%). Thirty-eight percent of the pediatric cardiac intensive care units have a protocol used to monitor wound infection, and the staff mostly uses a written shift report (54%) to monitor the infection. (5) Discussion: this is the first survey to investigate the management of the wound after cardiac surgery in Italian pediatric cardiac intensive care units. The small sample size and the fact that the centers involved are only Italian cardiac intensive care units are the limits of this study. (6) Conclusions: in the Italian pediatric cardiac intensive care units it emerged that there is a diversity in the treatments adopted and a lack of specific protocols in the management of the pediatric cardiac surgical wound.
1. Background
Surgical Site Infections (SSIs) are a possible serious complication after cardiac surgery and are associated with increased morbidity (antibiotic use, a second surgery, prolonged hospitalization, prolonged periods of mechanical ventilation, inotropic support) and mortality [1,2]. The incidence of SSIs after pediatric cardiothoracic surgery in the USA is reported to be between 0.25% and 6%, and it has an associated mortality from 7% to 20% [3]. Pediatric recommendations are founded on expert opinions and from data extrapolated from adult guidelines [4]. Adult guidelines are based on risk factors such as obesity, diabetes, and smoking, which are not the same risk factors considered valid for developing SSIs in children [5]. Potential pre-operative, intra-operative, and post-operative risk factors for children include: age lower than one month, the duration of surgery, presence of genetic abnormalities, prolonged extracorporeal circulation time (ECMO), delayed sternal closure, pre-operative hospitalization and prolonged post-operative hospitalization, post-operative hemorrhage, and persistent low cardiac output [1,6,7]. From the literature it has emerged that a consistent number of studies sustained the bundle approach as a valid instrument for reducing the instances of SSIs [2,6,8,9]. Another four studies supported pediatric preventive guidelines and practice bundles as effectual for preventing SSIs [5,10,11,12]. Woodward et al. reported the experience of their center using an evidence-based protocol. The implementation and use of this protocol reduced the SSI rate by 64% between the first and second year of the analyzed study [8]. Even if the majority of those are single-center studies, the benefits of these projects and instruments are real and concrete. We wanted to know the reality in our country, and we wanted to investigate in the Italian Cardiac Intensive Care Units (CICUs) that accept pediatric patients the management and the sensibility about this possible severe complication that is the surgical site infection after cardiac surgery in the pediatric population.
2. Objective of the Study
The aim of this study was to evaluate the management of the wound dressing after cardiac surgery in critically ill children admitted into Italian CICUs.
3. Methods
Between May 2018 and May 2019, we completed a survey contacting the nurse coordinators of the 13 Italian CICUs, through a telematic questionnaire (Appendix A). We wanted to investigate the management of the wound after cardiac surgery in critically ill children admitted in these units. Our questionnaire contained 10 multiple choice questions inquiring about:
- the characteristics of the CICUs (accepting neonatal and pediatric or neonatal, pediatric, and adult patients; the number of beds for pediatric patients and pediatric cases during the year 2017);
- the presence of a standardized protocol for the management of the cardiac wound after cardiac surgery;
- in the case of a standardized protocol, which staff member has the responsibility of monitoring and dressing management;
- the presence of a standardized protocol used to monitor the possible infection of the wound after cardiac surgery;
- in the case of a standardized protocol, how the staff takes note of the presence of the infection and its treatment;
- in the case of the patient’s transfer to another ward, which staff member has the responsibility of monitoring and dressing management.
There was no need for the involvement of the ethics committee since the work involved a descriptive survey. A questionnaire was distributed to 13 nurse coordinators of Italian CICUs. Two PICU registered nurses developed the questionnaire based on their experience. The aim of these 10 questions was to investigate the management and responsibility for monitoring and dressing pediatric cardiac surgery wounds in Italian CICUs. The results were anonymously saved, and it was set a numerical identifier to maintain the confidentiality of each unit. The data has been processed through a descriptive analysis.
4. Results
This study includes 13 CICUs. All the centers answered the questionnaire. A total of 69% of the CICUs accept neonatal, pediatric, and adult patients, while 31% of them accept neonatal and pediatric clients (Table 1). Ten CICUs have a fixed number of beds for pediatric patients while three units do not have a set number of beds for children undergoing cardiac surgery. The average number of pediatric cases in 2017 for all of the 13 cardiac ICUs was 269.9. Two centers out of thirteen did not respond to this specific question, and one CICU shared the number of cases for the adult and pediatric population together. Ten units (77%) claimed to have adopted a protocol for the management of the wound after cardiac surgery. Eight out of ten units (a total of 62%) enclosed their protocol with their answers to the questionnaire (Figure 1a). Analyzing them we found that only four units are actual protocols, of which just one is pertinent to the covered topic; two are operative instructions; and two are operative surveillance. Nevertheless, none of them are specific for the management of the cardiac wound in the pediatric population: seven argue about surgical wounds in general and referring to the adult population, and one elucidate the external ventricular leads and mediastinitis care. All the centers that do not have a protocol (23%) agree that they would like to have one. When a standardized protocol is used in the CICU, the monitoring and dressing management is either a responsibility of: the registered nurse (RN) (31%), the cardiothoracic surgeon (0%), the CICU physician (0%), or the RN and physician (cardiothoracic surgeon, CICU physician, or multidisciplinary team) together (69%) (Figure 2a). Of the CICUs that responded, 38% have a protocol for monitoring if a wound infection is present after cardiac surgery, while 62% of the CICUs declared that they do not have one (Figure 1b). The monitoring of the wound infection after cardiac surgery occurs through: a written shift report on the patient’s medical record (54%), a validated rating scale (of which one center utilizes a regional infection surveillance) (38%), or a verbal shift report (0%). In the category “Other” (8%) evaluate the presence of the infection through discussion amongst a multidisciplinary team. When the patient is transferred to another ward, the wound is either managed by: the RN (15%), the cardiothoracic surgeon (15%), or the RN and the unit physician together (62%). In the “Other” category (8%) the interviewees specified that the wound is managed by “RN and collegiate evaluation” (Figure 2b).

Table 1.
Characteristics of the studied pediatric cardiac intensive care units (CICUs).
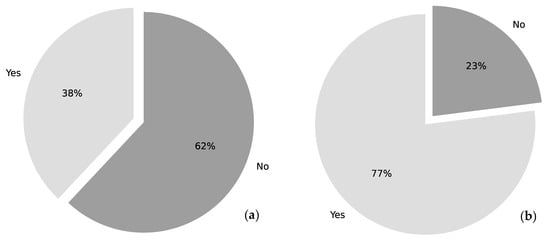
Figure 1.
Standardized protocols used in CICUs. (a) Presence of a standardized protocol for the management of cardiac surgical wound. (b) Presence of a standardized protocol for monitoring the cardiac surgical wound infection.
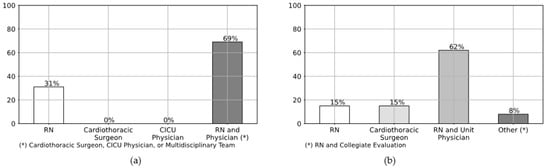
Figure 2.
Monitoring and dressing management of the cardiac surgical wound. (a) Staff member in the CICU who is responsible for monitoring and dressing management. (b) Staff member who is responsible for monitoring and dressing management in case of patient’s transfer to another ward.
5. Discussion
To the best of our knowledge, this is the first survey to investigate the management of the wound after cardiac surgery in the Italian CICUs accepting pediatric patients. The organizational structure is different in each CICU regarding the type of patients they accept, neonatal and pediatric, or neonatal, pediatric and adult, and the number of beds allocated for pediatric cases undergoing cardiac surgery. Eight units shared the documentation that they follow for the management of the cardiac wound. Although the documents provided by the eight CICUs are not on-target for the cardiac pediatric population, in four of them, there are indications about the timeline for the disinfection of the incision: one unit cleans the wound 24 to 48 h after the surgery, two CICUs remove the dressing of the first intention wounds 24 to 48 h after the surgery, and one unit removes the dressing of the first intention wounds after 48 h. Scientific evidence recommends that the sternal dressing should stay in place for the first 48 h after sternal closure, and it needs to be replaced only if visibly dirty [6,7,13]. After 48 h, the dressing should be removed [8]. Specific solutions for the disinfection of the surgical wound are listed in these documents provided by the interviewed CICUs: the povidone–iodine solution (the most commonly used), chlorhexidine, hydrogen peroxide, and Amuchina. Although in the literature there are no precise indications about the most appropriate solution for the disinfection of the surgical wound [14], detailed prophylaxis exists that specify pre- and intra-operative recommendations [2,7,9,12,15]. Regarding the antibiotic prophylaxis, Bath et al. (2016) demonstrated that limiting antimicrobial prophylaxis to 48 h after pediatric cardiac surgery neither increase the incidence of SSIs nor alter other clinical outcomes in this population. Furthermore, cefazolin and cefuroxime are equally recommended as first-line agents for antimicrobial prophylaxis in cardiac surgery. Murray et al., (2014) identified that limiting the peri-operative antibiotic prophylaxis after cardiac surgery to 48 h in neonates with a closed sternum and 24 h after sternal closure is safe and does not increase the rate of SSI. Another fundamental aspect that deserves further studies is to establish the best timing for administering pre-operative antibiotics and antiseptic skin preparation [7,8]. Some studies suggest the use of the pre-operative nasal culture [6,15,16,17,18]. However, further studies are needed in order to analyze this association. Less than half of the centers reported having a protocol for monitoring the wound infections after cardiac surgery, and only one center uses regional infection surveillance. This regional guideline is based on the European surgical site infection surveillance protocol (HAI-SSI), which was defined by the European Center for Diseases Prevention and Control (ECDC). This protocol classifies the procedures in diverse categories of intervention according to the US National Healthcare Safety Network (NHHSN). The clinical similarity of the surgical procedures belonging to these categories leads to homogeneous comparisons [19,20,21]. From the literature [5,10,11,12], it is clear that the implementation of quality improvement measures, such as linkage of registry and infection control surveillance, pediatric preventive guidelines and practice bundles, is considered an effective and systematic way to deliver preventive measures of SSIs. Woodward et al. (2012) proposed a hospital wide quality improvement project utilizing a protocolized approach in child cardiac surgery. This protocol was developed using evidence-based- and best practices from the adult and pediatric literature, and it was associated with a decreased number of infections in children. Analyzing the answers collected from this Italian survey, it can be said that in the majority of cases the staff members that have the responsibility for the wound management after cardiac surgery are RNs and physicians together. The analysis of the literature confirms that multidisciplinary work represents a fundamental point in the wound management (Cannon et al., 2016).
Limitations
A limit of this survey is the use of a questionnaire that was created specifically for this research; it was not previously validated. Furthermore, not all the CICUs sent their protocol on the pediatric cardiac surgical wound management, and the documentation sent was in the large part not directly connected to the aim of this study. Ultimately, we are aware of the small sample size and that the centers involved are only Italian CICUs.
6. Conclusions
Analyzing the data collected from this study, we can say that the Italian CICUs that accept pediatric patients follow different protocols for the management of the cardiac surgical wound, and a national standardized protocol or guideline to follow does yet not exist. Nevertheless, in the majority of cases registered nurses and physicians share the responsibility for wound dressing and care. There are diverse fundamental points that can have a positive impact on the cardiac surgical wound outcome, such as the best timing for the administration of antibiotic prophylaxis, the dressing management, and the collaboration between healthcare professionals. The final aim is the reduction in the incidence of SSIs. Further research is necessary for the realization of a national standardized protocol or guideline that incorporates all of these points.
Author Contributions
A.P. and B.T. had the idea of the project and developed the main conceptual ideas. A.P., B.T., P.C.F., V.S. prepared the proofs and the final article. I.D.B. supervised the final work. L.B. performed the statistical analysis. All authors contributed critical feedback. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is contained within the article.
Acknowledgments
We thank the nurse coordinators of all the centers involved: Gaslini Pediatric Hospital (Genoa, Italy), Regina Margherita Hospital (Turin, Italy), Papa Giovanni XXIII Hospital (Bergamo, Italy), University-Hospital of Padua, Gallucci Center (Padua, Italy), Borgo Trento University-Hospital (Verona, Italy), S. Orsola-Malpighi University-Hospital (Bologna, Italy), San Donato Milanese University-Hospital (Milan, Italy), Pediatric Hospital Bambin Gesù (Rome, Italy), del Cuore G. Pasquinucci Hospital (Massa, Italy), G.M. Lancisi Cardiac Hospital (Ancona, Italy), Federico II Hospital (Naples, Italy), Monaldi Hospital (Naples, Italy), Giovanni XXIII Pediatric Hospital (Bari, Italy).
Conflicts of Interest
The authors declare that they have no conflict of interest. The authors declare that they have not used any source of funding.
Appendix A. Questionnaire for the Nurse Coordinators of the Italian Pediatric Cardiac Intensive Care Units (CICUs)
1. Name of the Hospital and Region of the Paeditric Cardiac Intensive Care Unit:
______________________________
2. Type of patients accepted in the Unit:
- ○
- Neonatal/Pediatric patients
- ○
- Neonatal/Pediatric patients and adult patients
3. Number of beds for pediatric patients:
______________________________
4. Number of pediatric cases in 2017:
______________________________
5. Does the unit adopt a standardized protocol for the management of the cardiac wound after cardiac surgery?
- ○
- YES (If possible, attach the document)
- ○
- NO
6. If your answer to the previous question is NO, would you feel the need in the CICU to adopt one?
- ○
- YES
- ○
- NO
7. If your answer to question 5 is YES, who is the staff member of the CICU that has the responsibility for monitoring and dressing management?
- ○
- Registered Nurse
- ○
- Cardiothoracic Surgeon
- ○
- CICU Physician
- ○
- Registered Nurse and Physician (Cardiothoracic Surgeon, CICU Physician, or Multidisciplinary Team)
- ○
- Other ……………………………………………….
8. Does the unit adopt a standardized protocol for monitoring the cardiac surgery wound infection?
- ○
- YES
- ○
- NO
9. If your answer to the previous question is YES, could you please select the adopted method in the unit for monitoring these infections?
- ○
- Validated rating scale (name: _____________________________)
- ○
- Verbal shift record
- ○
- Written shift report on the patient’s medical record
- ○
- Other ………………………………………………………….
10. When the patient is transferred to another ward, who is the staff member that has the responsibility for monitoring and dressing management?
- ○
- Registered Nurse
- ○
- Cardiothoracic Surgeon
- ○
- Registered Nurse and Unit Physician
- ○
- Other……………………………………………….
References
- Barker, G.M.; O’Brien, S.M.; Welke, K.F.; Jacobs, M.L.; Jacobs, J.P.; Benjamin, D.K.; Peterson, E.D.; Jaggers, J.; Li, J.S. Major Infection After Pediatric Cardiac Surgery: A Risk Estimation Model. Ann. Thorac. Surg. 2010, 89, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Murray, M.T.; Corda, R.; Turcotte, R.; Bacha, E.; Saiman, L.; Krishnamurthy, G. Implementing a Standardized Perioperative Antibiotic Prophylaxis Protocol for Neonates Undergoing Cardiac Surgery. Ann. Thorac. Surg. 2014, 98, 927–933. [Google Scholar] [CrossRef] [PubMed]
- Sochet, A.A.; Cartron, A.M.; Nyhan, A.; Spaeder, M.C.; Song, X.; Brown, A.T.; Klugman, D. Surgical Site Infection After Pediatric Cardiothoracic Surgery: Impact on Hospital Cost and Length of Stay. World J. Pediatric Congenit. Heart Surg. 2017, 8, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Bratzler, D.; Dellinger, E.P.; Olsen, K.M.; Perl, T.M.; Auwaerter, P.G.; Bolon, M.K.; Fish, D.N.; Napolitano, L.M.; Sawyer, R.; Slain, D.; et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am. J. Health Pharm. 2013, 70, 195–283. [Google Scholar] [CrossRef] [PubMed]
- Woodward, C.S.; Son, M.; Calhoon, J.; Michalek, J.; Husain, S.A. Sternal Wound Infections in Pediatric Congenital Cardiac Surgery: A Survey of Incidence and Preventative Practice. Ann. Thorac. Surg. 2011, 91, 799–804. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Corcoran, C.; Van Dorn, C.S.; Pribble, C.; Thorell, E.A.; Pavia, A.T.; Ward, C.; Smout, R.; Bratton, S.L.; Burch, P.T. Reducing pediatric sternal wound infections: A quality improvement project. Pediatric Crit. Care Med. 2017, 18, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Blasco, J.I.; Campins-Martí, M.; Soler-Palacín, P.; Balcells, J.; Abella, R.; Gran, F.; Castillo, F.; Nuño, R.; Sanchez-De-Toledo, J. Impact of the implementation of an interdisciplinary infection control program to prevent surgical wound infection in pediatric heart surgery. Eur. J. Nucl. Med. Mol. Imaging 2015, 174, 957–963. [Google Scholar] [CrossRef]
- Woodward, C.; Taylor, R.; Son, M.; Taeed, R.; Jacobs, M.L.; Kane, L.; Jacobs, J.P.; Husain, S.A. Multicenter Quality Improvement Project to Prevent Sternal Wound Infections in Pediatric Cardiac Surgery Patients. World J. Pediatr. Congenit. Heart Surg. 2017, 8, 453–459. [Google Scholar] [CrossRef] [PubMed]
- Bath, S.; Lines, J.; Loeffler, A.M.; Malhotra, A.; Turner, R.B. Impact of standardization of antimicrobial prophylaxis duration in pediatric cardiac surgery. J. Thorac. Cardiovasc. Surg. 2016, 152, 1115–1120. [Google Scholar] [CrossRef] [PubMed]
- Cannon, M.; Hersey, D.; Harrison, S.; Joy, B.; Naguib, A.; Galantowicz, M.; Simsic, J. Improving Surveillance and Prevention of Surgical Site Infection in Pediatric Cardiac Surgery. Am. J. Crit. Care 2016, 25, e30–e37. [Google Scholar] [CrossRef] [PubMed]
- Staveski, S.; Abrajano, C.; Casazza, M.; Bair, E.; Quan, H.; Dong, E.; Petty, A.; Felix, K.; Roth, S.J. Silver-Impregnated Dressings for Sternotomy Incisions to Prevent Surgical Site Infections in Children. Am. J. Crit. Care 2016, 25, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Nayar, V.; Kennedy, A.; Pappas, J.; Atchley, K.D.; Field, C.; Smathers, S.; Teszner, E.E.; Sammons, J.S.; Coffin, S.E.; Gerber, J.S.; et al. Improving Cardiac Surgical Site Infection Reporting and Prevention by Using Registry Data for Case Ascertainment. Ann. Thorac. Surg. 2016, 101, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Costello, J.M.; Graham, D.A.; Morrow, D.F.; Morrow, J.; Potter-Bynoe, G.; Sandora, T.J.; Pigula, F.A.; Laussen, P.C. Risk Factors for Surgical Site Infection After Cardiac Surgery in Children. Ann. Thorac. Surg. 2010, 89, 1833–1842. [Google Scholar] [CrossRef] [PubMed]
- Berríos-Torres, S.I.; Umscheid, C.A.; Bratzler, D.; Leas, B.; Stone, E.C.; Kelz, R.R.; Reinke, C.E.; Morgan, S.; Solomkin, J.S.; Mazuski, J.E.; et al. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surg. 2017, 152, 784–791. [Google Scholar] [CrossRef] [PubMed]
- Silvetti, S.; Ranucci, M.; Isgrò, G.; Villa, V.; Costa, E. Preoperative colonization in pediatric cardiac surgery and its impact on postoperative infections. Pediatr. Anesth. 2017, 27, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Woodward, C.S.; Son, M.; Taylor, R.; Husain, S.A. Prevention of Sternal Wound Infection in Pediatric Cardiac Surgery: A protocolized approach. World J. Pediatr. Congenit. Heart Surg. 2012, 3, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Lex, D.J.; Toth, R.; Cserép, Z.; Breuer, T.; Sápi, E.; Szatmari, A.; Gál, J.; Székely, A. Postoperative differences between colonization and infection after pediatric cardiac surgery-a propensity matched analysis. J. Cardiothorac. Surg. 2013, 8, 166. [Google Scholar] [CrossRef] [PubMed]
- Katayanagi, T. Nasal Methicillin-Resistant S. Aureus is a Major Risk for Mediastinitis in Pediatric Cardiac Surgery. Ann. Thorac. Cardiovasc. Surg. 2015, 21, 37–44. [Google Scholar] [CrossRef] [PubMed][Green Version]
- ECDC Technical Document. Surveillance of Surgical Site Infections in European Hospitals-HAISSI Protocol Version 1.02; ECDC: Stockholm, Sweden, 2012. [Google Scholar] [CrossRef]
- Horan, T.C.; Andrus, M.; Dudeck, M.A. CDC/NHSN surveillance definition of health care–associated infection and criteria for specific types of infections in the acute care setting. Am. J. Infect. Control. 2008, 36, 309–332. [Google Scholar] [CrossRef] [PubMed]
- National Healthcare Safety Network. Surgical Site Infection (SSI) Event. Guidelines and Procedures for Monitoring SSI 2016. Available online: http://www.cdc.gov/nhsn/PDFs/pscManual/9pscSSIcurrent.pdf (accessed on 6 May 2019).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).