Radiology Community Attitude in Saudi Arabia about the Applications of Artificial Intelligence in Radiology
Abstract
:1. Introduction
2. Materials and Methods
3. Results
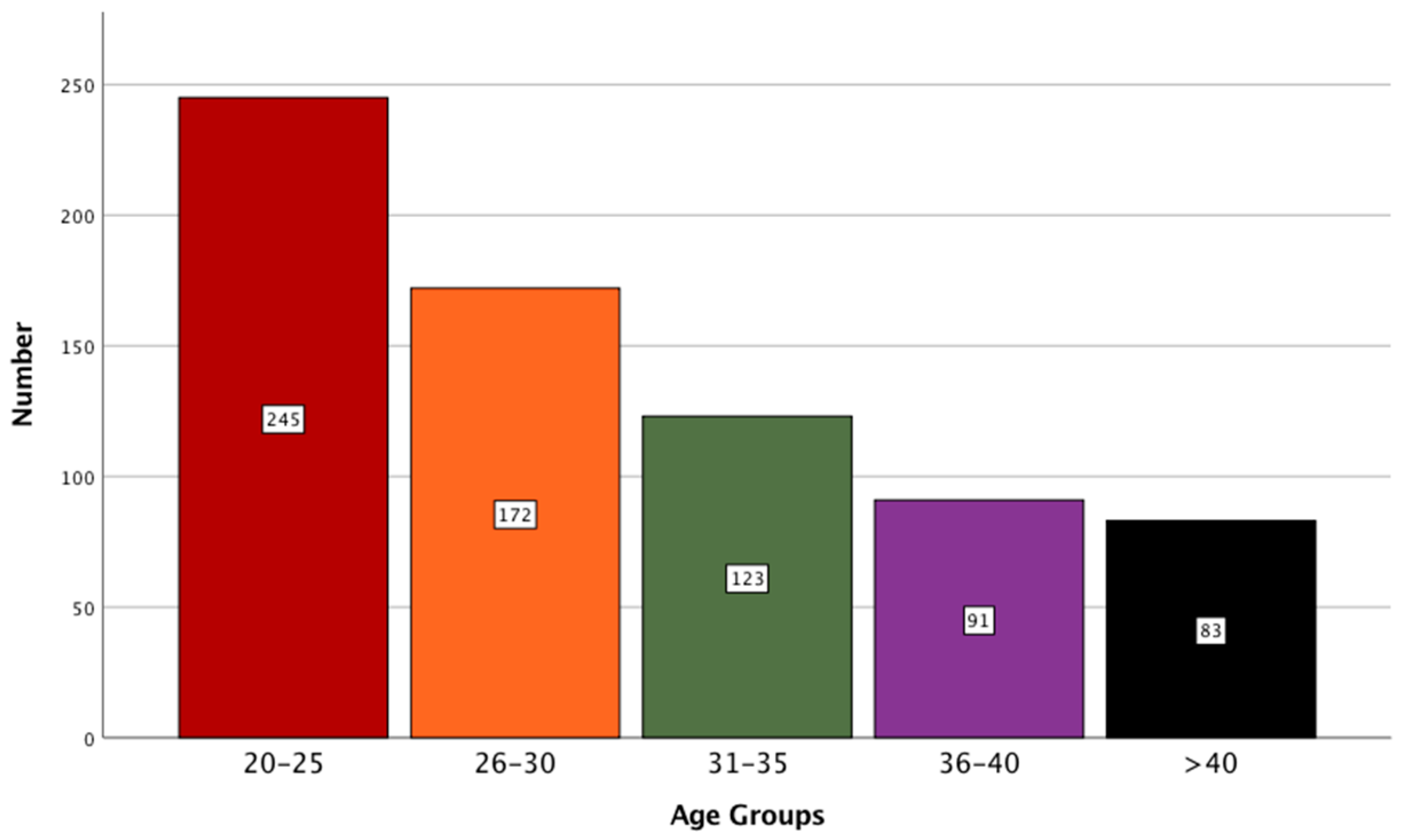
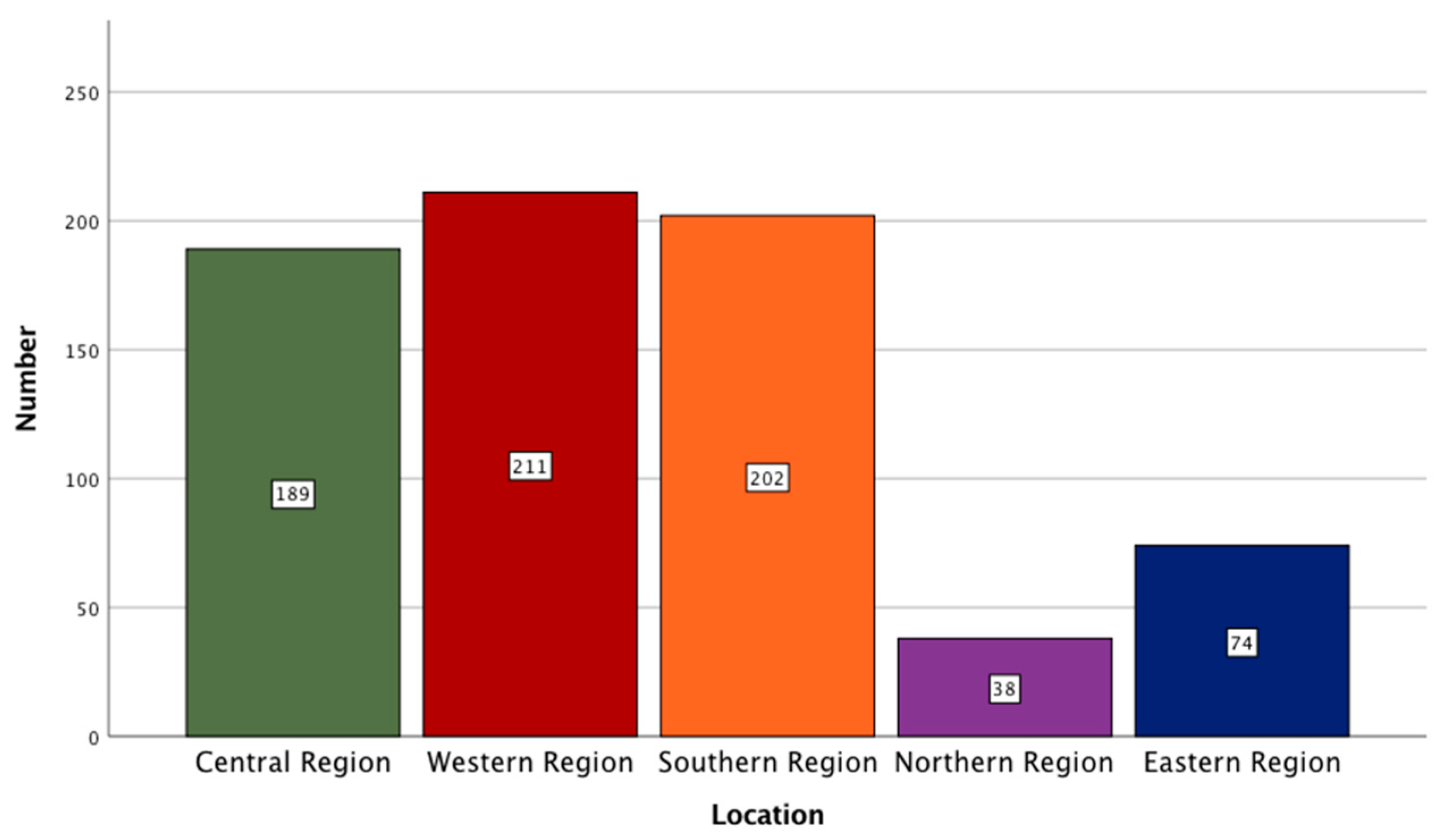
3.1. Descriptive Data Analysis
3.2. AI Awareness
3.3. AI Practices
3.4. AI Outcomes
3.5. AI Responsibilities
3.6. AI Validation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Reyes, M.; Meier, R.; Pereira, S.; Silva, C.A.; Dahlweid, F.-M.; von Tengg-Kobligk, H.; Summers, R.M.; Wiest, R. On the Interpretability of Artificial Intelligence in Radiology: Challenges and Opportunities. Radiol. Artif. Intell. 2020, 2, e190043. [Google Scholar] [CrossRef] [PubMed]
- Tang, A.; Tam, R.; Cadrin-Chênevert, A.; Guest, W.; Chong, J.; Barfett, J.; Chepelev, L.; Cairns, R.; Mitchell, J.R.; Cicero, M.D.; et al. Canadian Association of Radiologists White Paper on Artificial Intelligence in Radiology. Can. Assoc. Radiol. J. 2018, 69, 120–135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- SFR-IA Group; Cerf; French Radiology Community. Artificial intelligence and medical imaging 2018: French Radiology Community white paper. Diagn. Interv. Imaging 2018, 99, 727–742. [Google Scholar] [CrossRef]
- Rubin, D.L. Artificial Intelligence in Imaging: The Radiologist’s Role. J. Am. Coll. Radiol. 2019, 16, 1309–1317. [Google Scholar] [CrossRef]
- International Society of Radiographers and Radiological Technologists; The European Federation Of Radiographer Societies. Artificial Intelligence and the Radiographer/Radiological Technologist Profession: A joint statement of the International Society of Radiographers and Radiological Technologists and the European Federation of Radiographer Societies. Radiography 2020, 26, 93–95. [Google Scholar] [CrossRef]
- Minka, T. A Statistical Learning/Pattern Recognition Glossary. 2006. Available online: http://alumni.media.mit.edu/~tpminka/statlearn/glossary/ (accessed on 21 March 2021).
- Ranschaert, E.R.; Morozov, S.; Algra, P.R. (Eds.) Artificial Intelligence in Medical Imaging: Opportunities, Applications and Risks; Springer International Publishing: Berlin/Heidelberg, Germany, 2019. [Google Scholar] [CrossRef]
- Topol, E.J. High-performance medicine: The convergence of human and artificial intelligence. Nat. Med. 2019, 25, 44–56. [Google Scholar] [CrossRef]
- European Society of Radiology (ESR). Impact of artificial intelligence on radiology: A EuroAIM survey among members of the European Society of Radiology. Insights Imaging 2019, 10, 105. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.; Faes, L.; Kale, A.U.; Wagner, S.K.; Fu, D.J.; Bruynseels, A.; Mahendiran, T.; Moraes, G.; Shamdas, M.; Kern, C.; et al. A comparison of deep learning performance against health-care professionals in detecting diseases from medical imaging: A systematic review and meta-analysis. Lancet Digit. Health 2019, 1, e271–e297. [Google Scholar] [CrossRef]
- Choy, G.; Khalilzadeh, O.; Michalski, M.; Synho, D.; Samir, A.E.; Pianykh, O.S.; Geis, J.R.; Pandharipande, P.V.; Brink, J.A.; Dreyer, K.J. Current Applications and Future Impact of Machine Learning in Radiology. Radiology 2018, 288, 318–328. [Google Scholar] [CrossRef] [PubMed]
- Liew, C. The future of radiology augmented with Artificial Intelligence: A strategy for success. Eur. J. Radiol. 2018, 102, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Hardy, M.; Harvey, H. Artificial intelligence in diagnostic imaging: Impact on the radiography profession. Br. J. Radiol. 2020, 93, 20190840. [Google Scholar] [CrossRef]
- Goldberg, J.E.; Rosenkrantz, A. Artificial Intelligence and Radiology: A Social Media Perspective. Curr. Probl. Diagn. Radiol. 2019, 48, 308–311. [Google Scholar] [CrossRef]
- Gong, B.; Nugent, J.P.; Guest, W.; Parker, W.; Chang, P.J.; Khosa, F.; Nicolaou, S. Influence of Artificial Intelligence on Canadian Medical Students’ Preference for Radiology Specialty: ANational Survey Study. Acad. Radiol. 2019, 26, 566–577. [Google Scholar] [CrossRef]
- Geis, J.R.; Brady, A.; Wu, C.C.; Spencer, J.; Ranschaert, E.; Jaremko, J.L.; Langer, S.G.; Kitts, A.B.; Birch, J.; Shields, W.F.; et al. Ethics of artificial intelligence in radiology: Summary of the joint European and North American multisociety statement. Insights Imaging 2019, 10, 101. [Google Scholar] [CrossRef]
- McKinney, S.M.; Sieniek, M.; Godbole, V.; Godwin, J.; Antropova, N.; Ashrafian, H.; Back, T.; Chesus, M.; Corrado, G.S.; Darzi, A.; et al. International evaluation of an AI system for breast cancer screening. Nature 2020, 577, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Celi, L.A.; Fine, B.; Stone, D.J. An awakening in medicine: The partnership of humanity and intelligent machines. Lancet Digit. Health 2019, 1, e255–e257. [Google Scholar] [CrossRef] [Green Version]
- Nam, J.G.; Park, S.; Hwang, E.J.; Lee, J.H.; Jin, K.-N.; Lim, K.Y.; Vu, T.H.; Sohn, J.H.; Hwang, S.; Goo, J.M.; et al. Development and Validation of Deep Learning–based Automatic Detection Algorithm for Malignant Pulmonary Nodules on Chest Radiographs. Radiology 2019, 290, 218–228. [Google Scholar] [CrossRef] [Green Version]
- Lindsey, R.; Daluiski, A.; Chopra, S.; Lachapelle, A.; Mozer, M.; Sicular, S.; Hanel, D.; Gardner, M.; Gupta, A.; Hotchkiss, R.; et al. Deep neural network improves fracture detection by clinicians. Proc. Natl. Acad. Sci. USA 2018, 115, 11591–11596. [Google Scholar] [CrossRef] [Green Version]
- Blanc, D.; Racine, V.; Khalil, A.; Deloche, M.; Broyelle, J.-A.; Hammouamri, I.; Sinitambirivoutin, E.; Fiammante, M.; Verdier, E.; Besson, T.; et al. Artificial intelligence solution to classify pulmonary nodules on CT. Diagn. Interv. Imaging 2020, 101, 803–810. [Google Scholar] [CrossRef]
- Uyumazturk, B.; Kiani, A.; Rajpurkar, P.; Wang, A.; Ball, R.L.; Gao, R.; Yu, Y.; Jones, E.; Langlotz, C.P.; Martin, B.; et al. Deep Learning for the Digital Pathologic Diagnosis of Cholangiocarcinoma and Hepatocellular Carcinoma: Evaluating the Impact of a Web-based Diagnostic Assistant. arXiv 2019, arXiv:1911.07372. [Google Scholar]
- Dos Santos, D.P.; Giese, D.; Brodehl, S.; Chon, S.-H.; Staab, W.; Kleinert, R.; Maintz, D.; Baeßler, B. Medical students’ attitude towards artificial intelligence: A multicentre survey. Eur. Radiol. 2019, 29, 1640–1646. [Google Scholar] [CrossRef] [PubMed]
- Huisman, M.; Ranschaert, E.; Parker, W.; Mastrodicasa, D.; Koci, M.; de Santos, D.P.; Coppola, F.; Morozov, S.; Zins, M.; Bohyn, C.; et al. An international survey on AI in radiology in 1,041 radiologists and radiology residents part 1: Fear of replacement, knowledge, and attitude. Eur. Radiol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Coppola, F.; Faggioni, L.; Regge, D.; Giovagnoni, A.; Golfieri, R.; Bibbolino, C.; Miele, V.; Neri, E.; Grassi, R. Artificial intelligence: Radiologists’ expectations and opinions gleaned from a nationwide online survey. Radiol. Med. 2021, 126, 63–71. [Google Scholar] [CrossRef]
- Savadjiev, P.; Chong, J.; Dohan, A.; Vakalopoulou, M.; Reinhold, C.; Paragios, N.; Gallix, B. Demystification of AI-driven medical image interpretation: Past, present and future. Eur. Radiol. 2019, 29, 1616–1624. [Google Scholar] [CrossRef] [PubMed]
- Davenport, T.; Kalakota, R. The potential for artificial intelligence in healthcare. Future Healthc. J. 2019, 6, 94–98. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Questions | Answers | No. | % |
|---|---|---|---|
| Have you ever read or heard about artificial intelligence and its role in radiology? | Agree | 437 | 61.2 |
| Disagree | 277 | 38.8 | |
| Is your knowledge about artificial intelligence based on what is published in the media? | Agree | 453 | 63.4 |
| Disagree | 261 | 36.6 | |
| Are you keen to attend conferences and courses about artificial intelligence in radiology? | Agree | 311 | 43.6 |
| Disagree | 403 | 56.4 | |
| Are you involved in research projects on developing applications of artificial intelligence? | Agree | 170 | 23.8 |
| Disagree | 544 | 76.2 | |
| Does artificial intelligence contribute in the preparation of radiographic reports? | Agree | 389 | 54.5 |
| Disagree | 325 | 45.5 |
| Questions | Answers | No. | % |
|---|---|---|---|
| Artificial intelligence contributes to obtain high-quality images | Agree | 509 | 71.3 |
| Disagree | 205 | 28.7 | |
| Artificial intelligence contributes to the archiving system (PACS) | Agree | 576 | 80.7 |
| Disagree | 138 | 19.3 | |
| Artificial intelligence contributes toward the selection of appropriate scanning protocols for CT/MRI imaging | Agree | 456 | 63.9 |
| Disagree | 258 | 36.1 | |
| Is the weakness in training new graduates on artificial intelligence skills one of the greatest obstacles to the application of artificial intelligence in the work environment? | Agree | 493 | 69 |
| Disagree | 221 | 31 | |
| Will the application of artificial intelligence threaten some radiological professions ? | Agree | 312 | 43.7 |
| Disagree | 402 | 56.3 |
| Questions | Answers | No. | % |
|---|---|---|---|
| Can the result of radiographic examination by the artificial intelligence be considered reliable in routine cases? | Agree | 285 | 39.9 |
| Disagree | 429 | 60.1 | |
| The results of radiographic examination by the artificial intelligence need to be verified by the radiologist | Agree | 568 | 79.6 |
| Disagree | 146 | 20.4 | |
| Does conflict in results and interpretation between the various artificial intelligence algorithms and the opinion of the doctor cause stress and anxiety for the patient | Agree | 425 | 59.5 |
| Disagree | 289 | 40.5 | |
| The radiologists are the only ones responsible for the results of the utilization of artificial intelligence | Agree | 182 | 25.5 |
| Disagree | 532 | 74.5 | |
| Shared responsibility must be applied between artificial intelligence companies, hospitals, and international organizations regarding the results of using of artificial intelligence | Agree | 595 | 83.3 |
| Disagree | 119 | 16.7 |
| Questions | Answers | No. | % |
|---|---|---|---|
| The validity of the results from artificial intelligence must be verified | Agree | 628 | 88 |
| Disagree | 86 | 12 | |
| The patient should be aware of the use of artificial intelligence, and his or her consent should be obtained | Agree | 463 | 64.8 |
| Disagree | 251 | 35.2 | |
| The use of artificial intelligence contributes to the improvement of patient care | Agree | 437 | 61.2 |
| Disagree | 277 | 38.8 | |
| Should information issued about artificial intelligence be available only to radiologists? | Agree | 238 | 33.3 |
| Disagree | 476 | 66.7 | |
| Does the use of artificial intelligence enhance the capabilities of both physicians and radiologists and make them more efficient? | Agree | 445 | 62.3 |
| Disagree | 269 | 37.7 |
| Questions | Answers | No. | % |
|---|---|---|---|
| The use of artificial intelligence makes medical services more accurate | Agree | 463 | 64.8 |
| Disagree | 251 | 35.2 | |
| The use of artificial intelligence makes medical services more humane | Agree | 189 | 26.5 |
| Disagree | 525 | 73.5 | |
| Artificial intelligence must be included in the curriculum and training of medicine and health sciences colleges | Agree | 585 | 81.9 |
| Disagree | 129 | 18.1 | |
| Artificial intelligence cannot dispense with the role of physician and radiologist but makes a change in the work environment | Agree | 635 | 88.9 |
| Disagree | 79 | 11.1 | |
| The interaction between man and machine will be one of the most important medical skills in the future. | Agree | 617 | 86.4 |
| Disagree | 97 | 13.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alelyani, M.; Alamri, S.; Alqahtani, M.S.; Musa, A.; Almater, H.; Alqahtani, N.; Alshahrani, F.; Alelyani, S. Radiology Community Attitude in Saudi Arabia about the Applications of Artificial Intelligence in Radiology. Healthcare 2021, 9, 834. https://doi.org/10.3390/healthcare9070834
Alelyani M, Alamri S, Alqahtani MS, Musa A, Almater H, Alqahtani N, Alshahrani F, Alelyani S. Radiology Community Attitude in Saudi Arabia about the Applications of Artificial Intelligence in Radiology. Healthcare. 2021; 9(7):834. https://doi.org/10.3390/healthcare9070834
Chicago/Turabian StyleAlelyani, Magbool, Sultan Alamri, Mohammed S. Alqahtani, Alamin Musa, Hajar Almater, Nada Alqahtani, Fay Alshahrani, and Salem Alelyani. 2021. "Radiology Community Attitude in Saudi Arabia about the Applications of Artificial Intelligence in Radiology" Healthcare 9, no. 7: 834. https://doi.org/10.3390/healthcare9070834
APA StyleAlelyani, M., Alamri, S., Alqahtani, M. S., Musa, A., Almater, H., Alqahtani, N., Alshahrani, F., & Alelyani, S. (2021). Radiology Community Attitude in Saudi Arabia about the Applications of Artificial Intelligence in Radiology. Healthcare, 9(7), 834. https://doi.org/10.3390/healthcare9070834






