Stress, Social Support, and Resilience in Younger Rural Women: A Structural Equation Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Measures
2.2. Analytic Strategy
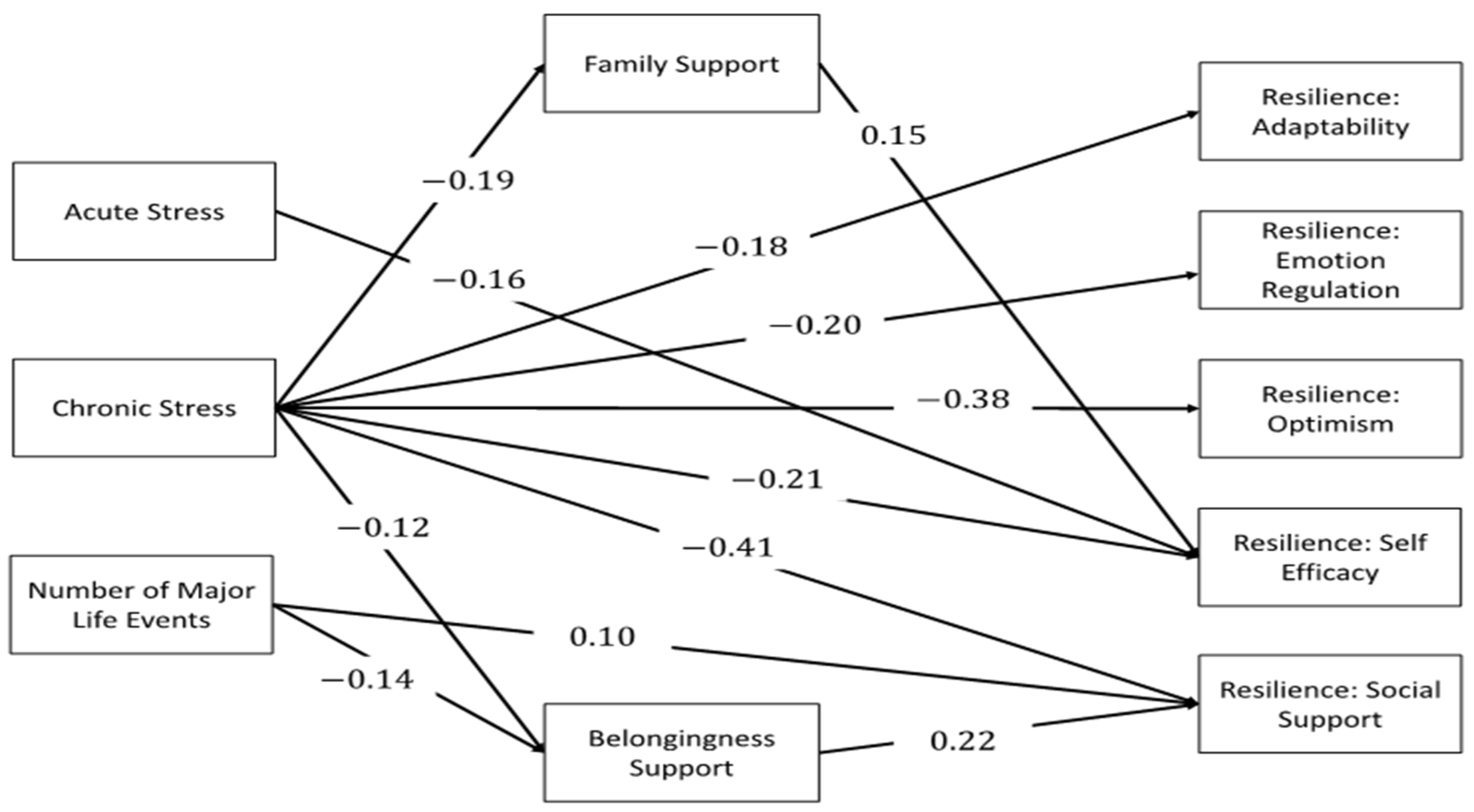
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Center for Disease Control (CDC). Heart Disease. Center for Disease Control and Prevention. 2019. Available online: https://www.cdc.gov/heartdisease/facts.htm (accessed on 5 February 2021).
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics—2020 Update: A Report from the American Heart Association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef]
- World Health Organization CVD Risk Chart Working Group. World Health Organization cardiovascular disease risk charts: Revised models to estimate risk in 21 global regions. Lancet Glob. Health 2019, 7, e1332–e1345. [Google Scholar] [CrossRef] [Green Version]
- Hemingway, H.; Marmot, M. Evidence-based cardiology: Psychosocial factors in the etiology and prognosis of coronary heart disease. Systematic review of prospective cohort studies. BMJ Br. Med. J. 1999, 318, 1460–1467. [Google Scholar] [CrossRef]
- Nielsen, N.; Kristensen, T.; Prescott, E.; Larsen, K.; Schnohr, P.; Gronbaek, M. Perceived stress and risk of ischemic heart disease: Causation or bias? Epidemiology 2006, 17, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Tawakol, A.; Ishai, A.; Takx, R.A.; Figueroa, A.L.; Ali, A.; Kaiser, Y.; Truong, Q.A.; Solomon, C.J.; Calcagno, C.; Mani, V.; et al. Relation between resting amygdalar activity and cardio-vascular events: A longitudinal and cohort study. Lancet 2017, 389, 834–845. [Google Scholar] [CrossRef] [Green Version]
- Tawakol, A.; Osborne, M.T.; Wang, Y.; Hammed, B.; Tung, B.; Patrich, T.; Oberfeld, B.; Ishai, A.; Shin, L.M.; Nahrendorf, M.; et al. Stress-Associated Neurobiological pathway linking socioeconomic disparities to cardiovascular disease. J. Am. Coll. Cardiol. 2019, 73, 3243–3255. [Google Scholar] [CrossRef] [PubMed]
- Rod, N.H.; Grønbæk, M.; Schnohr, P.; Prescott, E.; Kristensen, T.S. Perceived stress as a risk factor for changes in health behaviour and cardiac risk profile: A longitudinal study. J. Intern. Med. 2009, 266, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Cummings, D.M.; Kirian, K.; Howard, G.; Howard, V.; Yuan, Y.; Muntner, P.; Kissela, B.; Redmond, N.; Judd, S.E.; Safford, M.M. Consequences of comorbidity of elevated stress and/or depressive symptoms and incident cardiovascular outcomes in diabetes: Results from the reasons for geographic and racial differences in stroke (REGARDS) study. Diabetes Care 2016, 39, 101–109. [Google Scholar] [CrossRef] [Green Version]
- Janczura, M.; Bochenek, G.; Nowobilski, R.; Dropinski, J.; Kotula-Horowitz, K.; Laskowica, B.; Stanisz, A.; Lelakowski, J.; Domagala, T. The relationship of metabolic syndrome with stress, coronary heart disease and pulmonary function: An occupational cohort-based study. PLoS ONE 2015, 10, e0133750. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, S.; O’Driscoll, L. Metabolic syndrome: A closer look at the growing epidemic and its associated pathologies. Obes. Rev. 2015, 16, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Vitaliano, P.P.; Scanlan, J.M.; Zhang, J.; Savage, M.V.; Hirsch, I.B.; Siegler, I.C. A path model of chronic stress, the metabolic syndrome, and coronary heart disease. Psychosom. Med. 2002, 64, 418–435. [Google Scholar] [CrossRef]
- Davis, S.K.; Gebreab, S.; Quarells, R.; Gibbons, G.H. Social determinants of cardiovascular health among black and white women residing in Stroke Belt and Buckle regions of the South. Ethn. Dis. 2014, 24, 133–143. [Google Scholar]
- Cross, S.; Mehra, M.R.; Bhatt, D.L.; Nasir, K.; O’Donnell, J.; Califf, R.M.; Warraich, H.J. Rural-urban differences in cardiovascular mortality in the US, 1999–2017. JAMA 2020, 323, 1852–1854. [Google Scholar] [CrossRef] [PubMed]
- Havranek, E.P.; Mujahid, M.S.; Barr, D.A.; Blair, I.V.; Cohen, M.S.; Cruz-Flores, S.; Davey-Smith, G.; Dennison-Himmelfarb, C.R.; Lauer, M.S.; Lockwood, D.W.; et al. Social determinants of risk and outcomes for cardiovascular disease: A scientific statement from the American heart association. Circulation 2015, 132, 873–898. [Google Scholar] [CrossRef] [Green Version]
- Howard, G.; Kleindorfer, D.O.; Cushman, M.; Long, D.L.; Jasne, A.; Judd, S.E.; Higginbotham, J.C.; Howard, V.J. Contributors to the excess stroke mortality in rural areas in the United States. Stroke 2017, 48, 1773–1778. [Google Scholar] [CrossRef] [PubMed]
- Kulshreshtha, A.; Goyal, A.; Dabhadkar, K.; Veledar, E.; Vaccarino, V. Urban-rural differences in coronary heart disease mortality in the United States: 1999–2009. Public Health Rep. 2014, 129, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Limdi, N.A.; Howard, V.J.; Higginbotham, J.; Parton, J.; Safford, M.M.; Howard, G. US mortality: Influence of race, geography, and cardiovascular risk among participants in the population-based REGARDS cohort. J. Racial Ethn. Health Disparities 2016, 3, 599–607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, G.K.; Daus, G.P.; Allender, M.; Ramey, C.T.; Martine, E.K.; Perry, C.; De Los Reyes, A.A.; Vedamuthu, I.P. Social determinants of health in the United States: Addressing major health inequality trends for the nation, 1935–2016. Int. J. MCH AIDS 2017, 6, 139–164. [Google Scholar] [CrossRef]
- Keteepe-Arachi, T.; Sharma, S. Cardiovascular disease in women: Understanding symptoms and risk factors. Eur. Cardiol. 2017, 12, 10–13. [Google Scholar] [CrossRef] [Green Version]
- Woodward, M. Cardiovascular disease and female disadvantage. Int. J. Environ. Res. Public Health 2019, 16, 1165. [Google Scholar] [CrossRef] [Green Version]
- Stanhewicz, A.E.; Wenner, M.M.; Stachenfeld, N.S. Sex differences in endothelial function important to vascular health and overall cardiovascular disease risk across the lifespan. Am. J. Physiol. Heart Circ. Physiol. 2018, 315, H1569–H1588. [Google Scholar] [CrossRef]
- Tabloski, P.A. Global aging: Implications for women and women’s health. J. Obstet. Gynecol. Neonatal Nurs. 2004, 33, 627–638. [Google Scholar] [CrossRef]
- Hodes, G.E.; Epperson, C.N. Sex differences in vulnerability and resilience to stress across the life span. Biol. Psychiatry 2019, 86, 421–432. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.O.; Loria, A.S. Sex-specific effects of stress on metabolic and cardiovascular disease: Are women at higher risk? Am. J. Physiol. Regul. Integr. Comp. Physiol. 2017, 313, R1–R9. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Williamson, G. Perceived stress in a probability sample of the United States. In Claremont Symposium on Applied Social Psychology. The Social Psychology of Health; Sapacan, S., Oskamp, S., Eds.; Sage Publications, Inc.: Thousand Oaks, CA, USA, 1988. [Google Scholar]
- Albert, M.A.; Durazo, E.M.; Slopen, N.; Zaslavsky, A.M.; Buring, J.E.; Silva, T.; Chasman, D.; Williams, D.R. Cumulative psychological stress and cardiovascular disease risk in middle aged and older women: Rationale, design, and baseline characteristics. Am. Heart J. 2017, 192, 1–12. [Google Scholar] [CrossRef]
- Anderson, C.; Milne, G.L.; Park, Y.M.; Sandler, D.P.; Nichols, H.B. Cardiovascular disease risk factors and oxidative stress among premenopausal women. Free Radic. Biol. Med. 2018, 115, 246–251. [Google Scholar] [CrossRef]
- Osório, C.; Probert, T.; Jones, E.; Young, A.H.; Robbins, I. Adapting to stress: Understanding the neurobiology of resilience. Behav. Med. 2017, 43, 307–322. [Google Scholar] [CrossRef] [PubMed]
- Cosco, T.D.; Howse, K.; Brayne, C. Healthy ageing, resilience and wellbeing. Epidemiol. Psychiatr. Sci. 2017, 26, 579–583. [Google Scholar] [CrossRef]
- Liu, H.; Zhang, C.; Ji, Y.; Yang, L. Biological and psychological perspectives of resilience: Is it possible to improve stress resistance? Front. Hum. Neurosci. 2018, 12, 326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DeSimone, J.A.; Harms, P.D.; Vanhove, A.J.; Herian, M.N. Development and validation of the five-by-five resilience scale. Assessment 2017, 24, 778–797. [Google Scholar] [CrossRef] [PubMed]
- Lehrer, H.M.; Steinhardt, M.A.; Dubois, S.K.; Laudenslager, M.L. Perceived stress, psychological resilience, hair cortisol concentration, and metabolic syndrome severity: A moderated mediation model. Psychoneuroendocrinology 2020, 113, 104510. [Google Scholar] [CrossRef]
- Felix, A.S.; Lehman, A.; Nolan, T.S.; Sealy-Jefferson, S.; Breathett, K.; Hood, D.B.; Addison, D.; Anderson, C.M.; Cené, C.W.; Warren, B.J.; et al. Stress, resilience, and cardiovascular disease risk among black women. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005284. [Google Scholar] [CrossRef]
- Yalcin-Siedentopf, N.; Pichler, T.; Welte, A.S.; Hoertnagl, C.M.; Klasen, C.C.; Kemmler, G.; Siedentopf, C.M.; Hofer, A. Sex matters: Stress perception and the relevance of resilience and perceived social support in emerging adults. Arch. Women’s Ment. Health 2021, 24, 403–411. [Google Scholar] [CrossRef] [PubMed]
- Tomaka, J.; Thompson, S.; Palacios, R. The relation of social isolation, loneliness, and social support to disease outcomes among the elderly. J. Aging Health 2006, 18, 359–384. [Google Scholar] [CrossRef] [PubMed]
- Ozbay, F.; Johnson, D.C.; Dimoulas, E.; Morgan, C.A.; Charney, D.; Southwick, S. Social support and resilience to stress: From neurobiology to clinical practice. Psychiatry 2007, 4, 35–40. [Google Scholar] [PubMed]
- Harvey, I.S.; Alexander, K. Perceived social support and preventive health behavioral outcomes among older women. J. Cross-Cult. Gerontol. 2012, 27, 275–290. [Google Scholar] [CrossRef] [Green Version]
- Heaney, C.A.; Israel, B.A. Social Networks and Social Support. Health Behavior and Health Education: Theory, Research, and Practice; Jossey-Bass, Inc.: San Francisco, CA, USA, 2008. [Google Scholar]
- Masten, A.S. Ordinary magic: Resilience processes in development. Annu. Prog. Child Psychiatry Child Dev. 2005, 56, 227–238. [Google Scholar] [CrossRef]
- Perry, B. How children become resilient. Scholast. Parent Child 2002, 10, 33–35. [Google Scholar]
- Bonanno, G.A. Loss, trauma, and human resilience. Am. Psychol. 2004, 59, 20–28. [Google Scholar] [CrossRef] [Green Version]
- United States Census Bureau. 2019. Available online: https://data.census.gov/cedsci/ (accessed on 15 February 2021).
- Creative Research System. Sample Size Calculator. 2012. Available online: https://www.surveysystem.com/sscalc.htm#one (accessed on 21 February 2021).
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 386–396. [Google Scholar] [CrossRef]
- Zenk, S.N.; Schulz, A.J.; Izumi, B.T.; Mentz, G.; Israel, B.A.; Lockett, M. Neighborhood food environment role in modifying psychosocial stress–diet relationships. Appetite 2013, 65, 170–177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MacKinnon, D. Introduction to Statistical Mediation Analysis; Lawrence Erlbaum Associates: New York, NY, USA, 2008. [Google Scholar]
- Bentler, P.M. Comparative fit indexes in structural models. Psychol. Bull. 1990, 107, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Browne, M.W.; Cudeck, R. Alternative Ways of Assessing Model Fit. Testing Structural Equation Models; Sage: Beverly Hills, CA, USA, 1993. [Google Scholar]
- Gary, F.; Yarandi, H.; Hassan, M.; Brooks, L.; These, S.; Hopps, J. Chronic stress and depressive symptoms in midlife African American women. J. Natl. Black Nurses Assoc. 2020, 31, 26–31. [Google Scholar]
- Abbott, L.S.; Slate, E.H.; Graven, L.J.; Lemacks, L.L.; Grant, J. Fatalism, social support, and self-management perceptions among rural African Americans living with diabetes and prediabetes. Nurs. Rep. 2021, 11, 242–252. [Google Scholar] [CrossRef]
- Dorfman, L.T.; Mendez, E.C.; Osterhaus, J.K. Stress and resilience in the oral histories of rural older women. J. Women Aging 2009, 21, 303–316. [Google Scholar] [CrossRef]
- Ong, H.L.; Vaingankar, J.A.; Abdin, E.; Sambasivam, R.; Fauziana, R.; Tan, M.; Chong, S.; Goveas, R.R.; Chiam, P.; Subramaniam, M. Resilience and burden in caregivers of older adults: Moderating and mediating effects of perceived social support. BMC Psychiatry 2018, 18, 27. [Google Scholar] [CrossRef] [Green Version]
- Zhang, H.; Zhao, Q.; Cao, P.; Ren, G. Resilience and quality of life: Exploring the mediator role of social support in patients with breast cancer. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2017, 23, 5969–5979. [Google Scholar] [CrossRef]
- Silva Júnior, E.; Eulálio, M.; Souto, R.Q.; Santos, K.L.; Melo, R.; Lacerda, A.R. The capacity for resilience and social support in the urban elderly. Cienc. Saude Coletiva 2019, 24, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Hwang, W.J.; Lee, T.Y.; Lim, K.O.; Bae, D.; Kwak, S.; Park, H.Y.; Kwon, J.S. The effects of four days of intensive mindfulness meditation training (Templestay program) on resilience to stress: A randomized controlled trial. Psychol. Health Med. 2018, 23, 497–504. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Harrison, S.E.; Fairchild, A.J.; Chi, P.; Zhao, J.; Zhao, G. A randomized controlled trial of a resilience-based intervention on psychosocial well-being of children affected by HIV/AIDS: Effects at 6- and 12-month follow-up. Soc. Sci. Med. 2017, 190, 256–264. [Google Scholar] [CrossRef]
- Tunariu, A.D.; Tribe, R.; Frings, D.; Albery, I.P. The iNEAR programme: An existential positive psychology intervention for resilience and emotional wellbeing. Int. Rev. Psychiatry 2017, 29, 362–372. [Google Scholar] [CrossRef] [PubMed]
- Sarrionandia, A.; Ramos-Diaz, E.; Fernandez-Lasarte, O. Resilience as a mediator of emotional intelligence and perceived stress. A cross-county study. Front. Psychol. 2018, 21, 2653. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Varvogli, L.; Darviri, C. Stress management techniques: Evidence-based procedures that reduce stress and promote health. Health Sci. J. 2011, 5, 74–89. [Google Scholar]
- Roy, B.; Riley, C. Transforming Communities to Reduce Stress and Improve Health. Available online: https://www.hsj.gr/medicine/stress-management-techniques-evidencebased-procedures-that-reduce-stress-and-promote-health.pdf (accessed on 13 March 2021).
- Borgi, M.; Collacchi, B.; Ortona, E.; Cirulli, F. Stress and coping in women with breast cancer: Unravelling the mechanisms to improve resilience. Neurosci. Biobehav. Rev. 2020, 119, 406–421. [Google Scholar] [CrossRef] [PubMed]
- Abbott, L.S.; Slate, E.H.; Lemacks, J.L. Influencing cardiovascular health habits in the rural, deep south. Results of a cluster randomized trial. Health Educ. Res. 2019, 34, 200–208. [Google Scholar] [CrossRef]
- Abbott, L.S.; Slate, E.H.; Graven, L.J. Cardiovascular disease risk among rural residents living with diabetes and prediabetes: A cluster randomized trial. Public Health Nurs. 2019, 37, 16–24. [Google Scholar] [CrossRef] [Green Version]
- Abbott, L.S.; Williams, C.; Slate, E.H.; Gropper, S. Promoting heart health among rural African Americans. J. Cardiovasc. Nurs. 2018, 33, E8–E14. [Google Scholar] [CrossRef]
- Abbott, L.S.; Slate, E.H. Improving cardiovascular disease knowledge among rural participants: The results of a cluster randomized trial. Healthcare 2018, 6, 71. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.; Geng, L. Effects of socioeconomic status on physical and psychological health: Lifestyle as a mediator. Int. J. Environ. Res. Public Health 2019, 16, 281. [Google Scholar] [CrossRef] [Green Version]
- Syed, I.U. Clearing the Smoke Screen: Smoking, Alcohol Consumption, and Stress Management Techniques among Canadian Long-Term Care Workers. Int. J. Environ. Res. Public Health 2020, 17, 6027. [Google Scholar] [CrossRef] [PubMed]

| Variable | Level | n | % |
|---|---|---|---|
| Marital Status | Single | 239 | 67.5 |
| Married | 81 | 22.9 | |
| Other | 34 | 9.6 | |
| Race | Black | 289 | 81.6 |
| White | 55 | 15.5 | |
| Other | 10 | 2.8 | |
| Ethnicity | Hispanic | 11 | 3.1 |
| Not Hispanic | 343 | 96.9 | |
| Highest Education | Some HS | 64 | 18.1 |
| HS/GED | 169 | 47.7 | |
| Some College | 102 | 28.8 | |
| BS/BA or higher | 16 | 4.5 | |
| Employment | Full-time | 127 | 35.9 |
| Part-time | 77 | 21.8 | |
| Not employed | 149 | 42.1 | |
| Children Under 18 | Yes | 244 | 68.9 |
| No | 110 | 31.1 | |
| Financial Insecurity | Yes | 256 | 72.3 |
| No | 98 | 27.7 | |
| Min, Max | M | SD | |
| Age | 18, 44 | 32.68 | 7.84 |
| Number of Children | 0, 8 | 1.52 | 1.52 |
| Dependent Variable | Independent Variable | Coefficient | Standard Error | p |
|---|---|---|---|---|
| Family Support | Chronic Stress | −0.19 | 0.06 | 0.001 |
| Family Support | Acute Stress | 0.01 | 0.02 | 0.455 |
| Family Support | Major Life Events | −0.12 | 0.06 | 0.063 |
| Belongingness Support | Chronic Stress | −0.12 | 0.06 | 0.035 |
| Belongingness Support | Acute Stress | 0.06 | 0.04 | 0.091 |
| Belongingness Support | Major Life Events | −0.14 | 0.06 | 0.020 |
| Resilience—Adaptability | Family Support | 0.07 | 0.05 | 0.208 |
| Resilience—Adaptability | Belongingness Support | 0.09 | 0.06 | 0.108 |
| Resilience—Adaptability | Chronic Stress | −0.18 | 0.05 | 0.001 |
| Resilience—Adaptability | Acute Stress | −0.63 | 0.04 | 0.080 |
| Resilience—Adaptability | Major Life Events | −0.03 | 0.05 | 0.628 |
| Resilience—Emotional Regulation | Family Support | −0.02 | 0.07 | 0.789 |
| Resilience—Emotional Regulation | Belongingness Support | 0.01 | 0.06 | 0.897 |
| Resilience—Emotional Regulation | Chronic Stress | −0.20 | 0.05 | <0.001 |
| Resilience—Emotional Regulation | Acute Stress | −0.12 | 0.07 | 0.111 |
| Resilience—Emotional Regulation | Major Life Events | −0.01 | 0.05 | 0.898 |
| Resilience—Optimism | Family Support | 0.023 | 0.062 | 0.709 |
| Resilience—Optimism | Belongingness Support | 0.02 | 0.05 | 0.725 |
| Resilience—Optimism | Chronic Stress | −0.38 | 0.05 | <0.001 |
| Resilience—Optimism | Acute Stress | 0.03 | 0.04 | 0.449 |
| Resilience—Optimism | Major Life Events | 0.03 | 0.05 | 0.586 |
| Resilience—Self-Efficacy | Family Support | 0.15 | 0.06 | 0.018 |
| Resilience—Self-Efficacy | Belongingness Support | 0.11 | 0.06 | 0.064 |
| Resilience—Self-Efficacy | Chronic Stress | −0.21 | 0.05 | <0.001 |
| Resilience—Self-Efficacy | Acute Stress | −0.16 | 0.08 | 0.042 |
| Resilience—Self-Efficacy | Major Life Events | −0.01 | 0.06 | 0.916 |
| Resilience—Social Support | Family Support | 0.09 | 0.05 | 0.100 |
| Resilience—Social Support | Belongingness Support | 0.22 | 0.05 | <0.001 |
| Resilience—Social Support | Chronic Stress | −0.41 | 0.04 | <0.001 |
| Resilience—Social Support | Acute Stress | −0.08 | 0.05 | 0.116 |
| Resilience—Social Support | Major Life Events | 0.10 | 0.05 | 0.031 |
| Relationship | Effect Type | Coefficient | Standard Error | p |
|---|---|---|---|---|
| Chronic Stress to Resilience—Self-Efficacy | Total Effect | −0.252 | 0.053 | <0.001 |
| Total Indirect | −0.040 | 0.016 | 0.014 | |
| Indirect through Family Support | −0.028 | 0.014 | 0.055 | |
| Indirect through Belongingness Support | −0.012 | 0.009 | 0.162 | |
| Total Direct | −0.212 | 0.054 | <0.001 | |
| Chronic Stress to Resilience—Social Support | Total Effect | −0.448 | 0.044 | <0.001 |
| Total Indirect | −0.042 | 0.016 | 0.010 | |
| Indirect through Family Support | −0.017 | 0.010 | 0.094 | |
| Indirect through Belongingness Support | −0.026 | 0.014 | 0.065 | |
| Total Direct | −0.405 | 0.044 | <0.001 | |
| Number of Major Life Events to Resilience—Social Support | Total Effect | 0.063 | 0.050 | 0.208 |
| Total Indirect | −0.040 | 0.017 | 0.021 | |
| Indirect through Family Support | −0.010 | 0.009 | 0.243 | |
| Indirect through Belongingness Support | −0.029 | 0.015 | 0.045 | |
| Total Direct | 0.103 | 0.048 | 0.031 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abbott, L.S.; Graven, L.J.; Schluck, G.; Williams, K.J. Stress, Social Support, and Resilience in Younger Rural Women: A Structural Equation Model. Healthcare 2021, 9, 812. https://doi.org/10.3390/healthcare9070812
Abbott LS, Graven LJ, Schluck G, Williams KJ. Stress, Social Support, and Resilience in Younger Rural Women: A Structural Equation Model. Healthcare. 2021; 9(7):812. https://doi.org/10.3390/healthcare9070812
Chicago/Turabian StyleAbbott, Laurie S., Lucinda J. Graven, Glenna Schluck, and Krystal J. Williams. 2021. "Stress, Social Support, and Resilience in Younger Rural Women: A Structural Equation Model" Healthcare 9, no. 7: 812. https://doi.org/10.3390/healthcare9070812
APA StyleAbbott, L. S., Graven, L. J., Schluck, G., & Williams, K. J. (2021). Stress, Social Support, and Resilience in Younger Rural Women: A Structural Equation Model. Healthcare, 9(7), 812. https://doi.org/10.3390/healthcare9070812






