Investigation of the Impact of Dental Care via Composite Resin Restoration among Children with Attention Deficit Hyperactivity Disorder: A Registry-Based Nested Case–Control Study
Abstract
:1. Introduction
2. Materials and Methods
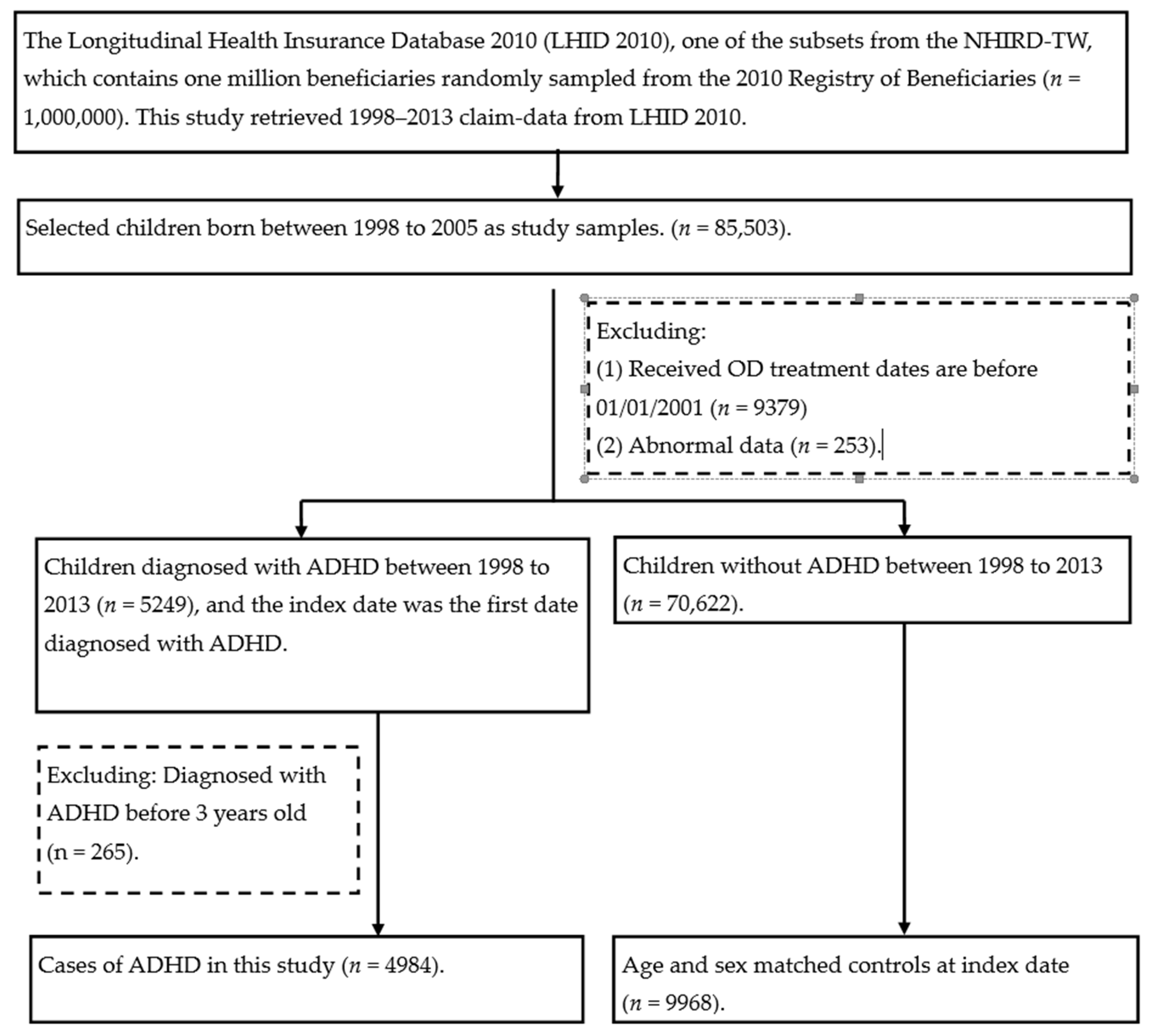
2.1. Study Population
2.2. Study Design and Sampled Individuals
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Woodruff, T.J.; Axelrad, D.A.; Kyle, A.D.; Nweke, O.; Miller, G.G.; Hurley, B.J. Trends in environmentally related childhood illnesses. Pediatrics 2004, 113, 1133–1140. [Google Scholar] [PubMed]
- Wang, Y.C.; Chong, M.Y.; Chou, W.J.; Yang, J.L. Prevalence of attention deficit hyperactivity disorder in primary school children in Taiwan. J. Formos. Med. Assoc. 1993, 92, 133–138. [Google Scholar] [PubMed]
- Tewar, S.; Auinger, P.; Braun, J.M.; Lanphear, B.; Yolton, K.; Epstein, J.N.; Ehrlich, S.; Froehlich, T.E. Association of Bi-sphenol A exposure and Attention-Deficit/Hyperactivity Disorder in a national sample of U.S. children. Environ. Res. 2016, 150, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.-H.; Bae, S.; Kim, B.-N.; Shin, C.H.; Lee, Y.A.; Kim, J.I.; Hong, Y.-C. Prenatal and postnatal bisphenol A exposure and social impairment in 4-year-old children. Environ. Health 2017, 16, 79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olea, N.; Pulgar, R.; Pérez, P.; Olea-Serrano, F.; Rivas, A.; Novillo-Fertrell, A.; Pedraza, V.; Soto, A.M.; Sonnenschein, C. Estrogenicity of resin-based composites and sealants used in dentistry. Environ. Health Perspect. 1996, 104, 298–305. [Google Scholar] [CrossRef] [PubMed]
- Joskow, R.; Barr, D.B.; Barr, J.R.; Calafat, A.M.; Needham, L.L.; Rubin, C. Exposure to bisphenol A from bis-glycidyl dimethacrylate-based dental sealants. J. Am. Dent. Assoc. 2006, 137, 353–362. [Google Scholar] [CrossRef] [PubMed]
- Kingman, A.; Hyman, J.; Masten, S.A.; Jayaram, B.; Smith, C.; Eichmiller, F.; Arnold, M.C.; Wong, P.A.; Schaeffer, J.M.; Solanki, S.; et al. Bisphenol A and other compounds in human saliva and urine associated with the placement of composite restorations. J. Am. Dent. Assoc. 2012, 143, 1292–1302. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.-J.; Lee, S.-Y.; Yuan, S.-S.; Yang, C.-J.; Yang, K.-C.; Huang, T.-S.; Chou, W.-J.; Chou, M.-C.; Lee, M.-J.; Lee, T.-L.; et al. Prevalence rates of youths diagnosed with and medicated for ADHD in a nationwide survey in Taiwan from 2000 to 2011. Epidemiol. Psychiatr. Sci. 2017, 26, 624–634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, C.L.; Weng, S.F.; Ho, C.H. Gender ratios of administrative prevalence and incidence of atten-tion-deficit/hyperactivity disorder (ADHD) across the lifespan: A nationwide population-based study in Taiwan. Psychiatry Res. 2016, 244, 382–387. [Google Scholar] [CrossRef] [PubMed]
- Huss, M.; Hölling, H.; Kurth, B.-M.; Schlack, R. How often are German children and adolescents diagnosed with ADHD? Prevalence based on the judgment of health care professionals: Results of the German health and examination survey (KiGGS). Eur. Child Adolesc. Psychiatry 2008, 17, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Laugesen, B.; Mohr-Jensen, C.; Boldsen, S.K.; Jørgensen, R.; Sørensen, E.E.; Grønkjær, M.; Rasmussen, P.; Lauritsen, M.B. Attention deficit hyperactivity disorder in childhood: Healthcare use in a Danish birth cohort during the first 12 years of life. J. Pediatr. 2018, 197, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, T.; Kubo, K.; Nishikawa, Y.; Aou, S. Postnatal exposure to low-dose bisphenol A influences various emotional conditions. J. Toxicol. Sci. 2013, 38, 539–546. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gioiosa, L.; Parmigiani, S.; Saal, F.S.V.; Palanza, P. The effects of bisphenol A on emotional behavior depend upon the timing of exposure, age and gender in mice. Horm. Behav. 2013, 63, 598–605. [Google Scholar] [CrossRef] [PubMed]
- Fleisch, A.F.; Sheffield, P.E.; Chinn, C.; Edelstein, B.L.; Landrigan, P.J. Bisphenol A and Related Compounds in Dental Materials. Pediatrics 2010, 126, 760–768. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kang, G.; Kim, J.Y.; Kim, J.; Won, P.J.; Name, J.H. Release of bisphenol A from resin composite used to bond orthodontic lingual retainers. Am. J. Orthod. Dentofacial. Orthop. 2011, 140, 779–789. [Google Scholar] [CrossRef] [PubMed]
- Maserejian, N.N.; Trachtenberg, F.L.; Hauser, R.; McKinlay, S.; Shrader, P.; Tavares, M.; Bellinger, D.C. Dental Composite Restorations and Psychosocial Function in Children. Pediatrics 2012, 130, e328–e338. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McKinney, C.; Rue, T.; Sathyanarayana, S.; Martin, M.; Seminario, A.L.; DeRouen, T. Dental sealants and restorations and urinary bisphenol A concentrations in children in the 2003-2004 National Health and Nutrition Examination Survey. J. Am. Dent. Assoc. 2014, 145, 745–750. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.-H.; Yi, S.-K.; Kim, S.-Y.; Kim, J.-S.; Son, S.-A.; Jeong, S.-H.; Kim, J.-B. Salivary bisphenol A levels and their association with composite resin restoration. Chemosphere 2017, 172, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Thapar, A.; Cooper, M.; Jefferies, R.; Stergiakouli, E. What causes attention deficit hyperactivity disorder? Arch. Dis. Child. 2012, 97, 260–265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michalowicz, J. Bisphenol A—sources, toxicity and biotransformation. Environ. Toxicol. Pharmacol. 2014, 27, 738–758. [Google Scholar] [CrossRef] [PubMed]
| Total n = 14,952 | With ADHD n = 4984 | Without ADHD n = 9968 | p | ||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Composite resin treatment number | 10,196 | 68.2 | 3500 | 70.2 | 6696 | 67.2 | 0.0002 |
| Age at index date (Mean ± SD) | 7.45 ± 2.20 | 7.45 ± 2.20 | 0.9946 | ||||
| Follow up time (Mean ± SD/years) | 3.17 ± 2.15 | 3.15 ± 2.15 | 0.8596 | ||||
| Sex | 1.00 | ||||||
| female | 3279 | 21.9 | 1093 | 21.9 | 2186 | 21.9 | |
| male | 11,673 | 78.1 | 3891 | 78.1 | 7782 | 78.1 | |
| Comorbidity | |||||||
| autism | 430 | 2.9 | 392 | 7.8 | 38 | 0.4 | <0.001 |
| mental retardation | 526 | 3.5 | 473 | 9.4 | 53 | 0.5 | <0.001 |
| developmental delay | 1687 | 11.3 | 923 | 18.5 | 391 | 3.9 | <0.001 |
| Living district | <0.001 | ||||||
| Taipei | 5662 | 38.4 | 2245 | 46.2 | 3417 | 34.6 | |
| Northern | 2291 | 15.5 | 731 | 15.0 | 1560 | 15.8 | |
| Central | 2603 | 17.7 | 668 | 13.8 | 1935 | 19.6 | |
| Southern | 1907 | 12.9 | 490 | 10.1 | 1417 | 14.3 | |
| Kao-Ping | 1981 | 13.4 | 638 | 13.1 | 1343 | 13.6 | |
| Eastern | 304 | 2.06 | 87 | 1.79 | 217 | 2.2 | |
| Urbanization level | <0.001 | ||||||
| urban | 11,415 | 77.4 | 3973 | 81.8 | 7442 | 75.3 | |
| suburban | 1229 | 8.33 | 336 | 6.9 | 893 | 9.03 | |
| rural | 2104 | 14.3 | 550 | 11.3 | 1554 | 15.7 | |
| Total (n = 14,952) | Case (n = 4984) | Control (n = 9968) | Odds Ratio | 95% CI | ||
|---|---|---|---|---|---|---|
| Without composite resin restoration | 4756 | 3272 | 1484 | 1 | ||
| With composite resin restoration | total | 10,196 | 3500 | 6696 | 1.25 | 1.13–1.38 |
| female | 2294 | 772 | 1522 | 1.14 | 0.92–1.41 | |
| male | 7902 | 2728 | 5174 | 1.29 | 1.14–1.43 |
| Odds Ratio | 95% CI | ||
|---|---|---|---|
| Without composite resin treatment | 1 | ||
| With composite resin treatment | 1–3 times | 1.19 | 1.08–1.32 |
| 4–7 times | 1.08 | 0.97–1.02 | |
| 8–11 times | 1.10 | 0.97–1.24 | |
| ≥12 times | 1.24 | 1.12–1.38 |
| Total (n = 14,952) | Odds Ratio | 95% CI | ||
|---|---|---|---|---|
| n | ||||
| Without composite resin treatment | 4756 | 1 | -- | |
| With composite resin treatment | ≤1 years | 1639 | 1.19 | 1.04–1.35 |
| >1 years | 8557 | 1.25 | 1.14–1.37 | |
| ≤3 years | 5443 | 1.21 | 1.10–1.32 | |
| >3 years | 4753 | 1.30 | 1.16–1.50 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hu, C.-J.; Yu, H.-C.; Chang, Y.-C. Investigation of the Impact of Dental Care via Composite Resin Restoration among Children with Attention Deficit Hyperactivity Disorder: A Registry-Based Nested Case–Control Study. Healthcare 2021, 9, 803. https://doi.org/10.3390/healthcare9070803
Hu C-J, Yu H-C, Chang Y-C. Investigation of the Impact of Dental Care via Composite Resin Restoration among Children with Attention Deficit Hyperactivity Disorder: A Registry-Based Nested Case–Control Study. Healthcare. 2021; 9(7):803. https://doi.org/10.3390/healthcare9070803
Chicago/Turabian StyleHu, Chien-Jen, Hui-Chieh Yu, and Yu-Chao Chang. 2021. "Investigation of the Impact of Dental Care via Composite Resin Restoration among Children with Attention Deficit Hyperactivity Disorder: A Registry-Based Nested Case–Control Study" Healthcare 9, no. 7: 803. https://doi.org/10.3390/healthcare9070803
APA StyleHu, C.-J., Yu, H.-C., & Chang, Y.-C. (2021). Investigation of the Impact of Dental Care via Composite Resin Restoration among Children with Attention Deficit Hyperactivity Disorder: A Registry-Based Nested Case–Control Study. Healthcare, 9(7), 803. https://doi.org/10.3390/healthcare9070803







