Work Fatigue in a Hospital Setting: The Experience at Cheng Hsin General Hospital
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Data Selection
2.2. Measures
2.3. Data Analysis
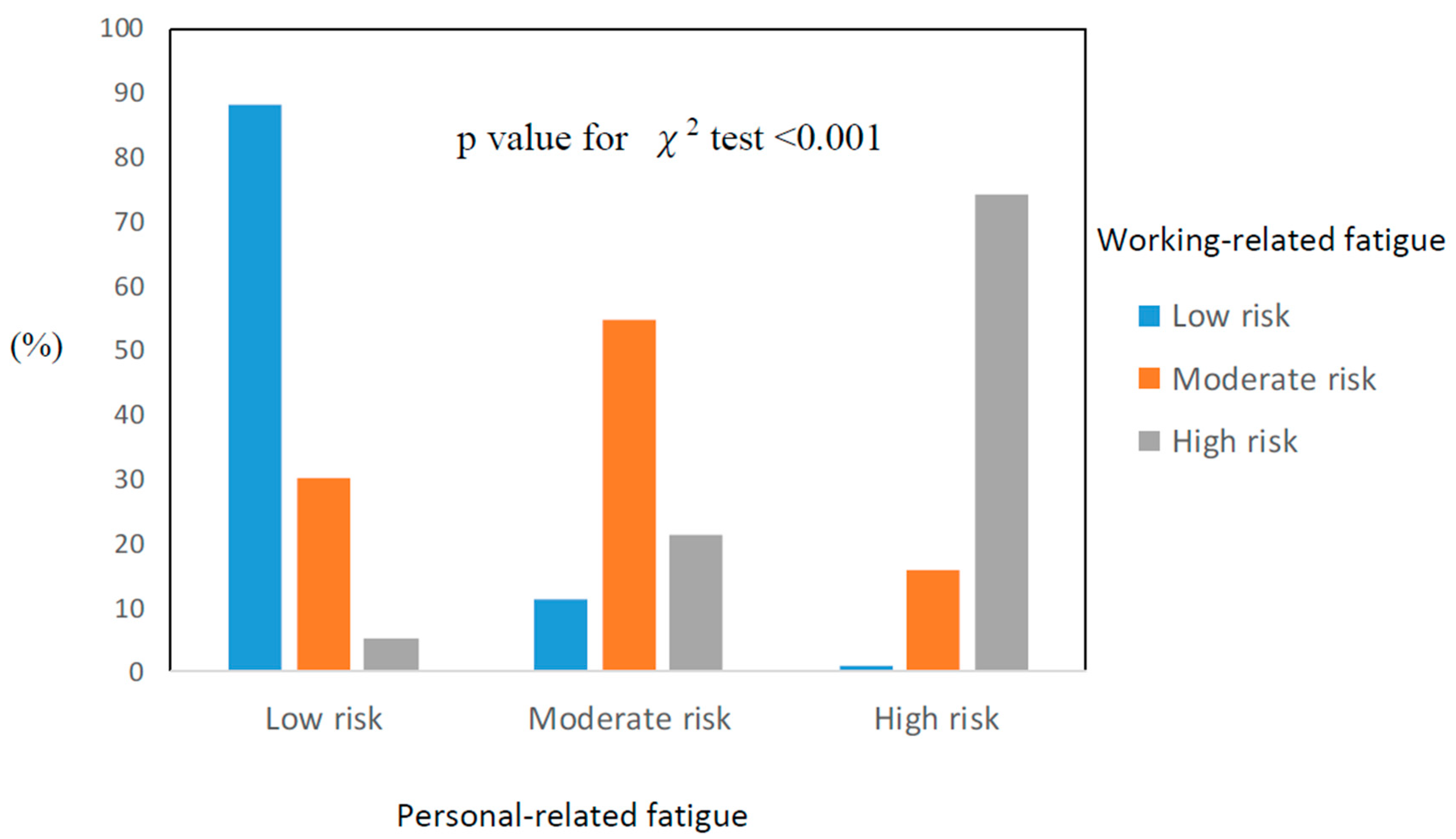
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jacquet, T.; Lepers, R.; Poulin-Charronnat, B.; Bard, P.; Pfister, P.; Pageaux, B. Mental fatigue induced by prolonged motor Imagery increases perception of effort and the activity of motor areas. Neuropsychologia 2021, 150, 107701. [Google Scholar] [CrossRef]
- Min, A.; Min, H.; Hong, H.C. Work schedule characteristics and fatigue among rotating shift nurses in hospital setting: An integrative review. J. Nurs. Manag. 2019, 27, 884–895. [Google Scholar] [CrossRef] [PubMed]
- Jang, H.J.; Kim, O.; Kim, S.; Kim, M.S.; Choi, J.A.; Kim, B.; Dan, H.; Jung, H. Factors affecting physical and mental fatigue among female hospital nurses: The Korea Nurses’ Health Study. Healthcare 2021, 9, 201. [Google Scholar] [CrossRef]
- Ricci, J.A.; Chee, E.; Lorandeau, A.L.; Berger, J. Fatigue in the U.S. workforce: Prevalence and implications for lost productive work time. J. Occup. Environ. Med 2007, 49, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bláfoss, R.; Sundstrup, E.; Jakobsen, M.D.; Brandt, M.; Bay, H.; Andersen, L.L. Physical workload and bodily fatigue after work: Cross-sectional study among 5000 workers. Eur. J. Public Health 2019, 29, 837–842. [Google Scholar] [CrossRef] [PubMed]
- Johnston, D.W.; Allan, J.L.; Powell, D.J.H.; Jones, M.C.; Farquharson, B.; Bell, C.; Johnston, M. Why does work cause fatigue? A real-time investigation of fatigue, and determinants of fatigue in nurses working 12-hour shifts. Ann. Behav. Med. 2019, 53, 551–562. [Google Scholar] [CrossRef] [Green Version]
- Seol, M.J.; Lee, B.S.; Lee, S.K. Effects of labor intensity and fatigue on sleep quality of clinical nurses. J. Korean Acad. Nurs. Adm. 2018, 24, 276–287. [Google Scholar] [CrossRef] [Green Version]
- Yeh, W.Y.; Cheng, Y.; Chen, C.J.; Hu, P.Y.; Kristensen, T.S. Psychometric properties of the Chinese version of Copenhagen burnout inventory among employees in two companies in Taiwan. Int. J. Behav. Med. 2007, 14, 126–133. [Google Scholar] [CrossRef]
- Di Muzio, M.; Dionisi, S.; Di Simone, E.; Cianfrocca, C.; Di Muzio, F.; Fabbian, F.; Barbiero, G.; Tartaglini, D.; Giannetta, N. Can nurses’ shift work jeopardize the patient safety? A systematic review. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 4507–4519. [Google Scholar]
- de Jong, M.; Bonvanie, A.M.; Jolij, J.; Lorist, M.M. Dynamics in typewriting performance reflect mental fatigue during real-life office work. PLoS ONE 2020, 15, e0239984. [Google Scholar] [CrossRef]
- Austin, S.; Fernet, C.; Trépanier, S.G.; Lavoie-Tremblay, M. Fatigue in new registered nurses: A 12-month cross-lagged analysis of its association with work motivation, engagement, sickness absence and turnover intention. J. Nurs. Manag. 2020, 28, 606–614. [Google Scholar] [CrossRef] [PubMed]
- Brzozowski, S.; Rainbow, J.G.; Pinekenstein, B.; Knudsen, É.A.; Steege, L. Exploration of relationships among individual and organizational characteristics, nurse leader fatigue, and turnover intention. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2018, 62, 627–631. [Google Scholar] [CrossRef]
- Juniartha, I.G.N.; Sardjono, T.W.; Ningsih, D.K. A comparison of work-related fatigue and stress among emergency department nurses working in 7-7-10 and 12-12 shifts at the hospitals in Badung and Denpasar. Enferm. Clin. 2020, 30 (Suppl. S7), 74–77. [Google Scholar] [CrossRef]
- Cai, S.; Lin, H.; Hu, X.; Cai, Y.X.; Chen, K.; Cai, W.Z. High fatigue and its associations with health and work related factors among female medical personnel at 54 hospitals in Zhuhai, China. Psychol. Health Med. 2018, 23, 304–316. [Google Scholar] [CrossRef] [PubMed]
- Hardy, G.E.; Shapiro, D.A.; Borrill, C.S. Fatigue in the workforce of National Health Service Trusts: Levels of symptomatology and links with minor psychiatric disorder, demographic, occupational and work role factors. J. Psychosom. Res. 1997, 43, 83–92. [Google Scholar] [CrossRef]
- Winwood, P.C.; Winefield, A.H.; Lushington, K. Work-related fatigue and recovery: The contribution of age, domestic responsibilities and shiftwork. J. Adv. Nurs. 2006, 56, 438–449. [Google Scholar] [CrossRef] [PubMed]
- Barker, L.M.; Nussbaum, M.A. Fatigue, performance and the work environment: A survey of registered nurses. J. Adv. Nurs. 2011, 67, 1370–1382. [Google Scholar] [CrossRef]
- Wong, L.R.; Flynn-Evans, E.; Ruskin, K.J. Fatigue Risk Management: The Impact of Anesthesiology Residents’ Work Schedules on Job Performance and a Review of Potential Countermeasures. Anesth. Analg. 2018, 126, 1340–1348. [Google Scholar] [CrossRef]
- Johnson, A.L.; Jung, L.; Song, Y.; Brown, K.C.; Weaver, M.T.; Richards, K.C. Sleep deprivation and error in nurses who work the night shift. J. Nurs. Adm. 2014, 44, 17–22. [Google Scholar] [CrossRef]
- Rothenberger, D.A. Physician Burnout and Well-Being: A Systematic Review and Framework for Action. Dis. Colon Rectum 2017, 60, 567–576. [Google Scholar] [CrossRef]
- Tang, C.; Liu, C.; Fang, P.; Xiang, Y.; Min, R. Work-Related Accumulated Fatigue among Doctors in Tertiary Hospitals: A Cross-Sectional Survey in Six Provinces of China. Int. J. Environ. Res. Public Health. 2019, 16, 3049. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heiman, G.W. Research Methods in Psychology, 3rd ed.; Houghton Mifflin Company: Boston, MA, USA; New York, NY, USA, 2002. [Google Scholar]
- Çelik, S.; Ta¸sdemir, N.; Kurt, A.; ˙Ilgezdi, E.; Kubalas, Ö. Fatigue in intensive care nurses and related factors. Int. J. Occup. Environ. Med. 2017, 8, 199–206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variables | Types of Fatigue | ||||||
|---|---|---|---|---|---|---|---|
| Personal-Related | Working-Related | ||||||
| Total | Prevalence | p-Value for | Prevalence | p-Value for | |||
| Number | Number | (%) | χ2-Test | Number | (%) | χ2-Test | |
| Gender | |||||||
| Male | 400 | 128 | (32.0) | <0.001 | 121 | (30.2) | <0.001 |
| Female | 1732 | 754 | (43.5) | 712 | (41.1) | ||
| Age (yrs) | |||||||
| <40 | 1051 | 495 | (47.1) | <0.001 | 487 | (46.3) | <0.001 |
| 40–49 | 621 | 259 | (41.7) | 233 | (37.5) | ||
| 50–59 | 294 | 90 | (30.6) | 81 | (27.6) | ||
| ≥60 | 166 | 38 | (22.9) | 32 | (19.3) | ||
| Seniority (yrs) | |||||||
| <5 | 773 | 324 | (41.9) | 0.23 | 328 | (42.4) | 0.02 |
| 5–10 | 441 | 192 | (43.5) | 179 | (40.6) | ||
| 10–15 | 314 | 134 | (42.7) | 122 | (38.9) | ||
| 15–20 | 268 | 112 | (41.8) | 93 | (34.7) | ||
| ≥20 | 336 | 120 | (35.7) | 111 | (33.0) | ||
| Position | |||||||
| Supervisor | 79 | 22 | (27.8) | <0.001 | 19 | (24.1) | <0.001 |
| Physician | 88 | 43 | (43.4) | 42 | (42.4) | ||
| Nurse | 829 | 430 | (51.9) | 435 | (52.5) | ||
| Nurse practitioner | 160 | 76 | (47.5) | 68 | (42.5) | ||
| Medical personnel | 283 | 87 | (30.7) | 86 | (30.4) | ||
| Administration | 636 | 219 | (34.4) | 180 | (28.3) | ||
| Part-time position | 46 | 5 | (10.9) | 3 | (6.5) | ||
| Health management | |||||||
| Normal | 1315 | 521 | (39.6) | 0.04 | 499 | (37.9) | 0.18 |
| Abnormal | 817 | 361 | (44.2) | 334 | (40.9) | ||
| Total | 2132 | 882 | (41.4) | 833 | (39.1) | ||
| Personal-Related | Working-Related | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Moderate Risk vs. | High Risk vs. | Moderate Risk vs. | High Risk vs. | |||||||||
| Factors | Low Risk | Low Risk | Low Risk | Low Risk | ||||||||
| OR | 95%CI | p-Value | OR | 95%CI | p-Value | OR | 95%CI | p-Value | OR | 95%CI | p-Value | |
| Gender | ||||||||||||
| female vs. male | 1.19 | 0.89–1.58 | 0.25 | 1.40 | 0.90–2.18 | 0.14 | 1.21 | 0.88–1.65 | 0.24 | 1.03 | 0.69–1.53 | 0.91 |
| Seniority (yrs) | ||||||||||||
| >20 vs. <5 | 0.89 | 0.66–1.20 | 0.44 | 0.61 | 0.39–0.96 | 0.03 | 0.84 | 0.61–1.15 | 0.28 | 0.53 | 0.34–0.81 | 0.003 |
| 15–20 vs. <5 | 1.11 | 0.81–1.53 | 0.52 | 0.92 | 0.59–1.45 | 0.73 | 0.89 | 0.64–1.25 | 0.52 | 0.59 | 0.38–0.93 | 0.02 |
| 10–15 vs. <5 | 1.11 | 0.82–1.50 | 0.52 | 1.03 | 0.69–1.56 | 0.87 | 1.04 | 0.75–1.42 | 0.83 | 0.77 | 0.51–1.15 | 0.20 |
| 5–10 vs. <5 | 1.12 | 0.85–1.46 | 0.43 | 1.04 | 0.73–1.49 | 0.83 | 0.98 | 0.74–1.31 | 0.91 | 0.92 | 0.66–1.29 | 0.64 |
| Position | ||||||||||||
| Supervisor or Part-time | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - |
| Physician | 2.47 | 1.27–4.79 | 0.007 | 3.33 | 1.26–8.80 | 0.02 | 3.35 | 1.67–6.68 | 0.001 | 3.30 | 1.17–9.31 | 0.02 |
| Nurse | 3.07 | 1.81–5.20 | <0.001 | 4.48 | 1.98–10.15 | <0.001 | 3.75 | 2.11–6.64 | <0.001 | 7.44 | 3.12–17.70 | <0.001 |
| Nurse practitioner | 2.76 | 1.50–5.08 | 0.001 | 2.92 | 1.16–7.37 | 0.02 | 2.78 | 1.44–5.35 | 0.002 | 4.09 | 1.56–10.73 | 0.004 |
| Medical personnel | 1.39 | 0.79–2.46 | 0.26 | 1.65 | 0.69–3.97 | 0.26 | 1.62 | 0.88–3.00 | 0.12 | 2.59 | 1.04–6.45 | 0.04 |
| Administration | 1.89 | 1.12–3.20 | 0.02 | 1.21 | 0.52–2.83 | 0.66 | 1.67 | 0.94–2.96 | 0.08 | 1.89 | 0.78–4.59 | 0.16 |
| Health management | ||||||||||||
| Normal vs. Abnormal | 0.81 | 0.66-0.99 | 0.04 | 0.81 | 0.61–1.07 | 0.13 | 0.87 | 0.71–1.08 | 0.21 | 0.77 | 0.59–1.01 | 0.06 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tung, T.-H.; Hsiung, M.-C. Work Fatigue in a Hospital Setting: The Experience at Cheng Hsin General Hospital. Healthcare 2021, 9, 776. https://doi.org/10.3390/healthcare9060776
Tung T-H, Hsiung M-C. Work Fatigue in a Hospital Setting: The Experience at Cheng Hsin General Hospital. Healthcare. 2021; 9(6):776. https://doi.org/10.3390/healthcare9060776
Chicago/Turabian StyleTung, Tao-Hsin, and Ming-Chon Hsiung. 2021. "Work Fatigue in a Hospital Setting: The Experience at Cheng Hsin General Hospital" Healthcare 9, no. 6: 776. https://doi.org/10.3390/healthcare9060776
APA StyleTung, T.-H., & Hsiung, M.-C. (2021). Work Fatigue in a Hospital Setting: The Experience at Cheng Hsin General Hospital. Healthcare, 9(6), 776. https://doi.org/10.3390/healthcare9060776





