Organizational Support Experiences of Care Home and Home Care Staff in Sweden, Italy, Germany and the United Kingdom during the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
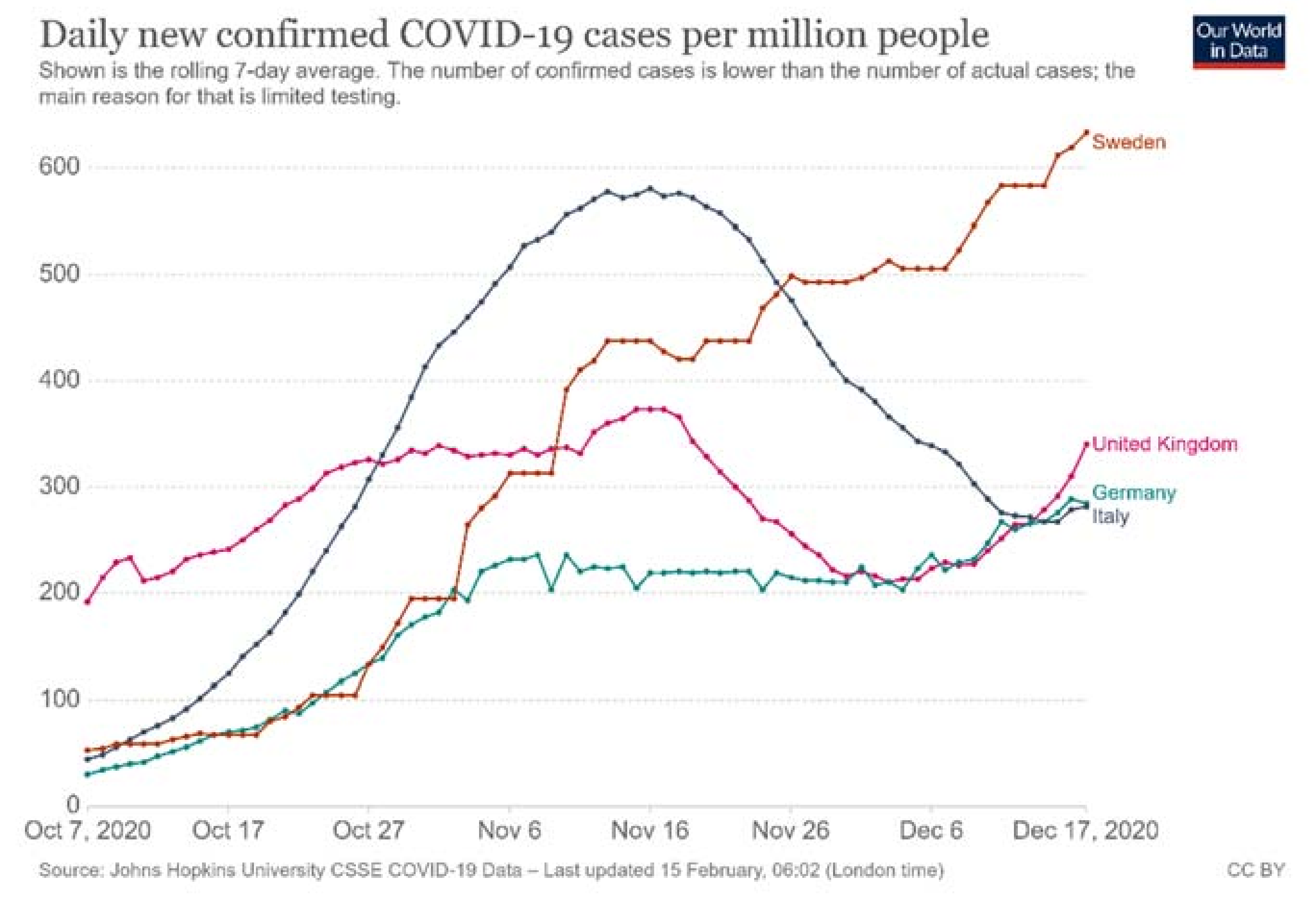
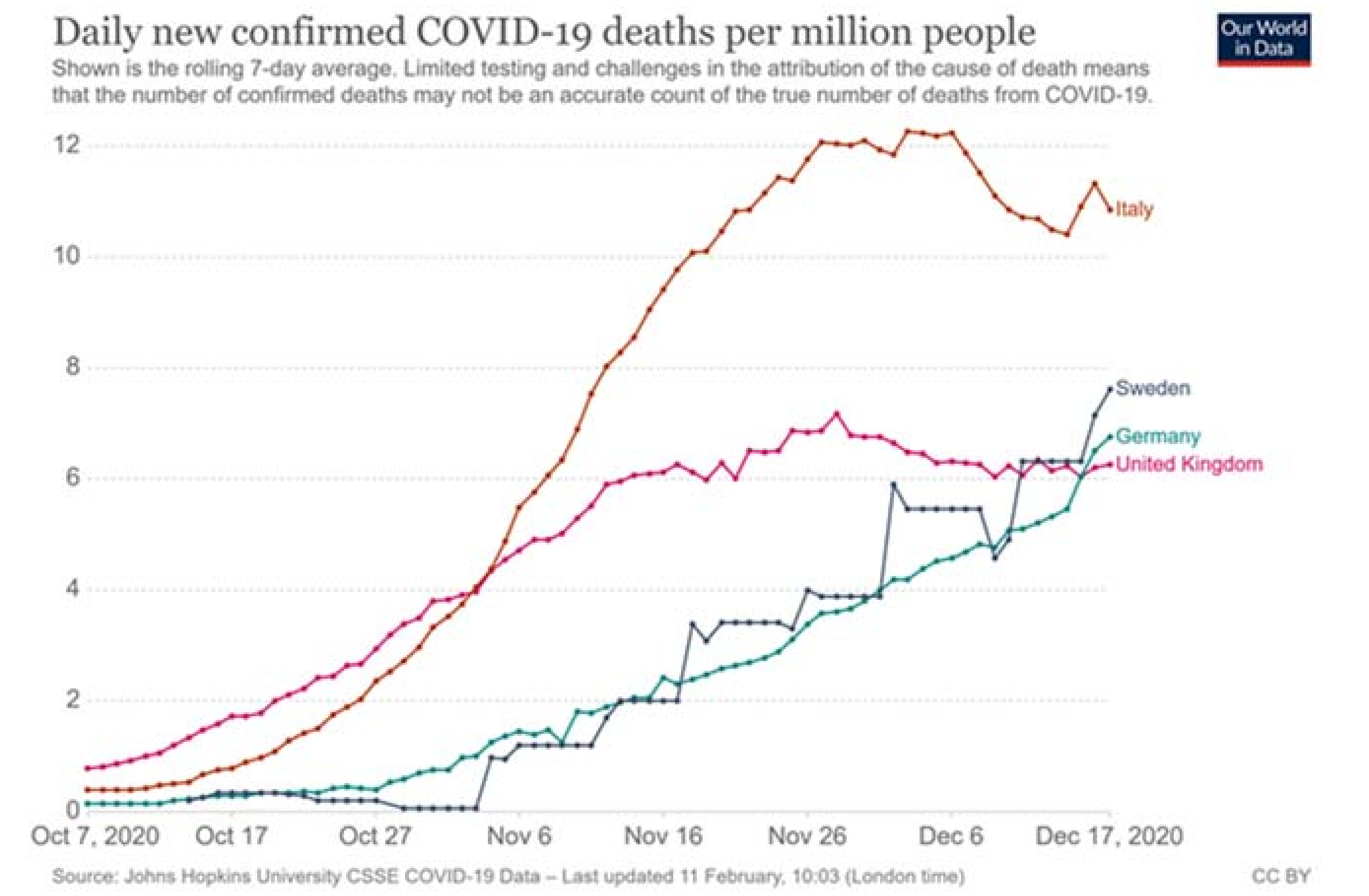
2.2. Data Collection
2.2.1. Questionnaire
2.2.2. Procedure
2.3. Data Analysis
3. Results
3.1. Stress and Anxiety Levels
3.2. Internal Support for the Staff from within the Organization
3.3. External Support for the Organization
3.4. Factors Associated with Stress and Anxiety Levels
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Coronavirus. 2021. Available online: https://www.who.int/health-topics/coronavirus#tab=tab_1 (accessed on 17 June 2021).
- Comas-Herrera, A.; Zalakain, J. Mortality associated with COVID-19 outbreaks in care homes: Early international evidence. In LTCcovid.org. International Long-Term Care Policy Network; CPEC-LSE: London, UK, 2020. [Google Scholar]
- Declercq, A.; de Stampa, M.; Geffen, L.; Heckman, G.; Hirdes, J.; Finne-Soveri, H.; Lum, T.; Millar, N.; Morris, J.N.; Onder, G.; et al. Why, in Almost All Countries, Was Residential Care for Older People So Badly Affected by COVID-19? OSE-Opinion Piece. 2020. Available online: http://www.ose.be/files/publication/OSEPaperSeries/Declercq_Et_Al_2020_OpinionPaper23.pdf (accessed on 20 December 2020).
- Alacevich, C.; Cavalli, N.; Giuntella, O.; Lagravinese, R.; Moscone, F.; Nicodemo, C. Exploring the Relationship between Care Homes and Excess Deaths in the COVID-19 Pandemic: Evidence from Italy. IZA DP.13492. 2020. Available online: http://ftp.iza.org/dp13492.pdf (accessed on 17 June 2021).
- Comas-Herrera, A.; Glanz, A.; Curry, N.; Deeny, S.; Hatton, C.; Hemmings, N.; Humphries, R.; Lorenz-Dant, K.; Oung, C.; Rajan, S.; et al. The COVID-19 Long-Term Care situation in England. LTCcovid.org, International Long-Term Care Policy Network, CPEC-LSE. 2020. Available online: https://ltccovid.org/2020/11/19/new-report-the-covid-19-long-term-care-situation-in-england/ (accessed on 26 February 2021).
- Smith, D.R.M.; Duval, A.; Pouwels, K.B.; Guillemot, D.; Fernandes, J.; Huynh, B.-T.; Temime, L.; Opatowsk, L. Optimizing COVID-19 surveil lance in long-term care facilities: A modelling study. BMC Med. 2020, 18, 386. [Google Scholar] [CrossRef] [PubMed]
- Kramer, V.; Papazova, I.; Thoma, A.; Kunz, M.; Falkai, P.; Schneider-Axmann, T.; Hierundar, A.; Wagner, E.; Hasan, A. Subjective burden and perspectives of German healthcare workers during the COVID-19 pandemic. Eur. Arch. Psychiatry Clin. Neurosci. 2021, 271, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Shreffer, J.; Petrey, J.; Huecker, M. The impact of COVID-19 on healthcare worker wellness: A scoping review. West. J. Emerg. Med. 2020, 21, 1059–1066. [Google Scholar]
- White, E.M.; Wetle, T.F.; Reddy, A.; Baier, R.R. Front-line Nursing Home Staff Experiences During the COVID-19 Pandemic. J. Am. Med. Dir. Assoc. 2021, 22, 199–203. [Google Scholar] [CrossRef]
- Mulladal, R.; Othman, W.; Hassan, A. Nurses’ Burnout: The Influence of Leader Empowering Behaviors, Work Conditions, and Demographic Traits. INQUIRY J. Health Care Organ. Provis. Financ. 2017, 54, 0046958017724944. [Google Scholar]
- Czuba, K.J.; Kayes, N.M.; McPherson, K.M. Support workers’ experiences of work stress in long-term care settings: A qualitative study. Int. J. Qual. Stud. Health Well-Being 2019, 14, 1622356. [Google Scholar] [CrossRef] [PubMed]
- Happell, B.; Dwyer, T.; Reid-Searl, K.; Burke, K.J.; Caperchione, C.M.; Gaskin, C.J. Nurses and stress: Recognizing causes and seeking solutions. J. Nurs. Manag. 2013, 21, 638–647. [Google Scholar] [CrossRef] [PubMed]
- Hyde, P.; Burns, D.; Killett, A.; Kenkmann, A.; Poland, F.; Gray, R. Organisational aspects of elder mistreatment in long term care. Qual. Ageing Older Adult 2014, 15, 197–209. [Google Scholar] [CrossRef]
- Rajamohan, S.; Porock, D.; Chang, Y.P. Understanding the Relationship Between Staff and Job Satisfaction, Stress, Turnover, and Staff Outcomes in the Person-Centered Care Nursing Home Arena. J. Nurs. Sch. 2019, 51, 560–568. [Google Scholar] [CrossRef]
- Coogle, C.L.; Parham, I.A.; Jablonski, R.; Rachel, J.A. Enhanced care assistant training to address the workforce crisis in home care: Changes related to job satisfaction and career commitment. Care Manag. J. 2007, 8, 71–81. [Google Scholar] [CrossRef]
- Berridge, C.; Tyler, D.A.; Miller, S.C. Staff empowerment practices and CNA retention: Findings from a nationally representative Nursing Home Culture Change Survey. J. Appl. Gerontol. 2018, 37, 419–434. [Google Scholar] [CrossRef] [PubMed]
- Eltaybani, S.; Noguchi-Watanabe, M.; Igarashi, A.; Saito, Y.; Yamamoto-Mitani, N. Factors related to intention to stay in the current workplace among long-term care nurses: A nationwide survey. Int. J. Nurs. Stud. 2018, 80, 118–127. [Google Scholar] [CrossRef] [PubMed]
- Esping-Andersen, G.; Wagner, S. Asymmetries in the Opportunity Structure: Inter-Generational Mobility Trends in Scandinavia and Continental Europe. Res. Soc. Stratif. Mobil. 2013, 30, 473–487. [Google Scholar]
- Baxter, S.; Johnson, M.; Chambers, D. The effects of integrated care: A systematic review of UK and international evidence. BMC Health Serv. Res. 2018, 18, 350. [Google Scholar] [CrossRef]
- Care Quality Commission. About Us. 2021. Available online: https://www.cqc.org.uk/about-us (accessed on 26 February 2021).
- Caselli, D. Did You Say “Social Impact”? Welfare Transformations, Networks of Expertise, and the Financialization of Italian Welfare. Hist. Soc. Res. 2020, 45, 140–160. [Google Scholar]
- Scaccabarozzi, G.; Giorgio Lovaglio, P.; Limonta, F.; Peruselli, C.; Bellentani, M.; Crippa, M. Monitoring the Italian Home Palliative Care Services. Healthcare 2019, 7, 4. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research Electronic Data Capture (REDCap)—A Metadata-Driven Methodology and Workflow Process for Providing Translational Research Informatics Support. J. Biomed. Inform. 2009, 4, 377–381. Available online: http://www.sciencedirect.com/science/article/pii/S1532046408001226 (accessed on 17 June 2021). [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap Consortium: Building an International Community of Software Partners. J. Biomed. Inform. 2019, 95, 103208. Available online: https://www.sciencedirect.com/science/article/pii/S1532046419301261 (accessed on 17 June 2021). [CrossRef]
- Adams, J.G.; Walls, R.M. Supporting the Health Care Workforce During the COVID-19 Global Epidemic. JAMA 2020, 323, 1439–1440. [Google Scholar] [CrossRef] [PubMed]
- Shingler-Nace, A. COVID-19. Nurse Lead. 2020. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7187843/ (accessed on 17 June 2021).
- Ley, C.; Jacobs, B. Perceptions of Nurses Staff During the COVID-19 Pandemic. Maryland Nurses Association’s 117th Annual Convention. Md. Nurse, 2021; 21, 7. [Google Scholar]
- Islam, M.S.; Baker, C.; Huxley, P.; Russell, I.T.; Dennis, M.S. The nature, characteristics and associations of care home staff stress and wellbeing: A national survey. BMC Nurs. 2017, 16, 22. [Google Scholar] [CrossRef] [PubMed]
- Dunn, L.A.; Rout, U.; Carson, J.; Ritter, S.A. Occupational stress amongst care staff working in nursing homes: An empirical investigation. J. Clin. Nurs. 1994, 3, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Intrator, O.; Bowblis, J.R. Shortages of Staff in Nursing Homes During the COVID-19 Pandemic: What are the Driving Factors? J. Am. Med. Dir. Ass. 2020, 21, 1371–1377. [Google Scholar] [CrossRef] [PubMed]
- Senczyszyn, A.; Lion, K.M.; Szcześniak, D.; Trypka, E.; Mazurek, J.; Ciułkowicz, M.; Maćkowiak, M.; Duda-Sikuła, M.; Wallner, R.; Rymaszewska, J. Mental Health Impact of SARS-COV-2 Pandemic on Long-Term Care Facility Personnel in Poland. J. Am. Med. Dir. Ass. 2020, 21, 1576–1577. [Google Scholar] [CrossRef] [PubMed]
- Dolton, P.; Nguyen, D.; Castellanos, M.; Rolfe, H. Brexit and the Health & Social Care Workforce in the UK; National Institute of Economic and Social Research: London, UK, 2018; pp. 1–134. Available online: https://www.basw.co.uk/system/files/resources/Report%20Brexit%20Health%20and%20Social%20Care%20Workforce%20-%20Full%20Report_0.pdf (accessed on 26 February 2021).
- Read, R.; Fenge, L.-A. What does Brexit mean for the UK social care workforce? Perspectives from the recruitment and retention frontline. Health Soc. Care Community 2019, 27, 676–682. [Google Scholar]
- Nicola, M.; Sohrabi, C.; Mathew, G.; Kerwan, A.; Al-Jabir, A.; Griffin, M.; Agha, M.; Agha, R. Health policy and leadership models during the COVID-19 pandemic: A review. Int. J. Surg. 2020, 81, 122–129. [Google Scholar] [CrossRef] [PubMed]
- WHO Regional Office for Europe. Strengthening the Health System Response to COVID-19: Recommendations for the WHO European Region; WHO Regional Office for Europe: Copenhagen, Denmark, 2020. [Google Scholar]
- Vinkers, C.H.; van Amelsvoort, T.; Bisson, J.I.; Branchi, I.; Cryan, J.F.; Domschke, K.; Howes, O.D.; Manchia, M.; Pinto, L.; de Quervain, D.; et al. Stress resilience during the coronavirus pandemic. Eur. Neuropsychopharmacol. 2020, 35, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Rajan, S.; Comas-Herrera, A.; Mckee, M. Did the UK Government Really Throw a Protective Ring Around Care Homes in the COVID-19 Pandemic? J. Long-Term Care 2020, 185–195. [Google Scholar] [CrossRef]
- The Organisation of Resilient Health and Social Care Following the COVID-19 Pandemic. Available online: https://ec.europa.eu/health/sites/default/files/expert_panel/docs/026_health_socialcare_covid19_en.pdf (accessed on 17 June 2021).
- Killett, A.; Burns, D.; Kelly, F.; Brooker, D.; Bowes, A.; La Fontaine, J.; Latham, I.; Wilson, M.; O’Neill, M.A. Digging deep: How organisational culture affects care home residents’ experiences. Ageing Soc. 2016, 36, 160–188. [Google Scholar] [CrossRef][Green Version]
- Care Quality Commission. Residential Social Care. 2021. Available online: https://www.cqc.org.uk/guidance-providers/regulations-enforcement/service-types#care-homes-nursing (accessed on 5 March 2021).
| Sweden n = 212 | Italy n = 103 | Germany n = 120 | UK n = 167 | Total n = 602 | ||
|---|---|---|---|---|---|---|
| Gender, n (%) | Male | 18 (8.8) | 18 (17.5) | 22 (18.3) | 6 (3.6) | 64 (10.8) |
| Female | 186 (91.2) | 85 (82.5) | 97 (80.8) | 161 (96.4) | 529 (89.0) | |
| Non-binary/third gender | 0 (0.0) | 0 (0.0) | 1 (0.8) | 0 (0.0) | 1 (0.2) | |
| Age, Mean (SD) | 45.74 (12.1) | 44.77 (11.3) | 38.69 (12.9) | 44.80 (12.0) | 43.86 (12.4) | |
| Professional role, n (%) | Managers/coordinator | 16 (7.7) | 24 (23.5) | 31 (26.1) | 65 (39.2) | 136 (22.8) |
| Registered nurse | 36 (17.3) | 12 (11.8) | 70 (58.8) | 14 (8.4) | 132 (22.2) | |
| Nursing assistant | 119 (57.2) | 52 (51.0) | 11 (9.2) | 13 (7.8) | 195 (32.8) | |
| Other care staff | 37 (17.8) | 14 (13.7) | 7 (5.9) | 74 (44.6) | 132 (22.2) | |
| Type of organization | Public | 190 (93.1) | 33 (32.0) | 44 (37.0) | 13 (7.8) | 280 (47.2) |
| Private | 13 (6.4) | 67 (65.0) | 41 (34.4) | 151 (90.4) | 272 (45.9) | |
| Non-profit/voluntary | 1 (0.5) | 3 (3.0) | 34 (28.6) | 3 (1.8) | 41 (6.9) |
| Sweden | Italy | Germany | UK | Total | p Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | M (SD) | n | M (SD) | n | M (SD) | n | M (SD) | n | M (SD) | ||
| Manager/ coordinator | 16 | 2.94 (1.06) | 24 | 3.58 (1.02) | 31 | 4.23 (0.81) | 65 | 4.02 (0.93) | 136 | 3.86 (1.01) | 0.001 |
| Registered nurse | 36 | 2.81 (1.31) | 12 | 3.83 (1.03) | 70 | 3.6 (1.00) | 14 | 4.29 (0.73) | 132 | 3.48 (1.16) | 0.001 |
| Nursing assistant | 117 | 3.26 (1.06) | 51 | 3.24 (1.14) | 11 | 3.55 (0.82) | 13 | 3.92 (0.86) | 192 | 3.32 (1.07) | 0.153 |
| Other care staff | 36 | 3.11 (1.04) | 14 | 3.43 (0.76) | 7 | 3.29 (1.11) | 71 | 3.92 (1.05) | 128 | 3.6 (1.08) | 0.002 |
| Total | 206 | 3.14 (1.12) | 101 | 3.42 (1.06) | 119 | 3.74 (0.98) | 164 | 3.99 (0.96) | 590 | 3.54 (1.09) | <0.001 |
| Sweden | Italy | Germany | UK | Total | p Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | M (SD) | n | M (SD) | n | M (SD) | n | M (SD) | n | M (SD) | ||
| I received clear guidelines from my organization | |||||||||||
| Manager/coordinator | 16 | 4.25 (0.68) | 23 | 3.43 (1.20) | 31 | 3.58 (1.43) | 64 | 4.22 (1.13) | 134 | 3.94 (1.22) | 0.010 |
| Registered nurse | 36 | 3.64 (1.07) | 12 | 3.42 (1.08) | 70 | 3.44 (1.00) | 14 | 4.14 (0.77) | 132 | 3.57 (1.02) | 0.114 |
| Nursing assistant | 119 | 4.29 (0.99) | 51 | 4.33 (0.97) | 11 | 3.36 (0.81) | 13 | 3.46 (1.27) | 194 | 4.2 (1.03) | 0.001 |
| Other care staff | 37 | 4.3 (0.78) | 14 | 3.57 (1.22) | 7 | 3.71 (1.7) | 74 | 4.15 (1.22) | 132 | 4.11 (1.15) | 0.177 |
| Total | 210 | 4.17 (0.98) | 101 | 3.89 (1.16) | 119 | 3.49 (1.15) | 166 | 4.13 (1.17) | 596 | 3.97 (1.13) | <0.001 |
| I received adequate support from management | |||||||||||
| Manager/coordinator | 16 | 4 (1.10) | 22 | 4 (1.11) | 28 | 4 (1.12) | 63 | 4.24 (1.25) | 129 | 4.12 (1.18) | 0.729 |
| Registered nurse | 36 | 3.58 (1.13) | 12 | 3.25 (1.29) | 69 | 3.26 (1.42) | 14 | 3.93 (1.21) | 131 | 3.42 (1.32) | 0.281 |
| Nursing assistant | 116 | 3.85 (1.11) | 47 | 3.98 (1.26) | 11 | 2.73 (1.68) | 13 | 3.15 (1.41) | 187 | 3.77 (1.24) | 0.005 |
| Other care staff | 37 | 3.97 (1.14) | 14 | 3.29 (1.14) | 7 | 2.57 (1.27) | 72 | 3.78 (1.47) | 130 | 3.72 (1.37) | 0.049 |
| Total | 207 | 3.85 (1.12) | 96 | 3.77 (1.24) | 115 | 3.35 (1.42) | 163 | 3.93 (1.38) | 581 | 3.76 (1.29) | 0.001 |
| I was provided with adequate personal protective equipment | |||||||||||
| Manager/coordinator | 16 | 4.19 (1.22) | 23 | 3.7 (1.40) | 31 | 4.13 (0.99) | 64 | 4.36 (1.15) | 134 | 4.17 (1.18) | 0.144 |
| Registered nurse | 36 | 4.11 (0.98) | 12 | 3.58 (1.31) | 70 | 3.04 (1.29) | 14 | 3.79 (1.12) | 132 | 3.46 (1.27) | 0.000 |
| Nursing assistant | 118 | 4 (1.08) | 48 | 4.17 (1.14) | 11 | 3.36 (1.5) | 13 | 3.46 (1.39) | 190 | 3.97 (1.15) | 0.070 |
| Other care staff | 37 | 4.24 (0.93) | 14 | 3.64 (1.34) | 7 | 3.57 (1.27) | 73 | 3.96 (1.27) | 131 | 3.98 (1.20) | 0.070 |
| Total | 209 | 4.09 (1.04) | 98 | 3.92 (1.26) | 119 | 3.39 (1.31) | 165 | 4.07 (1.24) | 591 | 3.91 (1.22) | <0.001 |
| I received adequate training | |||||||||||
| Manager/coordinator | 16 | 4 (1.03) | 22 | 3.73 (1.08) | 31 | 3.94 (1.36) | 64 | 4.34 (1.06) | 133 | 4.11 (1.15) | 0.113 |
| Registered nurse | 35 | 3.77 (1.06) | 12 | 3.42 (1.51) | 69 | 2.96 (1.19) | 14 | 3.57 (1.02) | 130 | 3.28 (1.22) | 0.008 |
| Nursing assistant | 117 | 3.77 (1.09) | 50 | 4.06 (1.36) | 11 | 3.36 (1.36) | 13 | 3 (1.41) | 191 | 3.77 (1.22) | 0.026 |
| Other care staff | 36 | 4.03 (0.97) | 14 | 3.5 (1.22) | 7 | 2.71 (1.50) | 72 | 3.74 (1.42) | 129 | 3.74 (1.31) | 0.090 |
| Total | 206 | 3.84 (1.06) | 99 | 3.81 (1.31) | 118 | 3.24 (1.33) | 164 | 3.91 (1.31) | 587 | 3.73 (1.25) | <0.001 |
| My voice was listened to | |||||||||||
| Manager/coordinator | 16 | 3.94 (1.06) | 22 | 4.14 (1.08) | 31 | 4.26 (1.09) | 63 | 4.24 (1.13) | 132 | 4.19 (1.10) | 0.772 |
| Registered nurse | 34 | 3.59 (1.02) | 12 | 3.75 (0.87) | 67 | 2.85 (1.29) | 14 | 3.36 (1.08) | 127 | 3.19 (1.21) | 0.007 |
| Nursing assistant | 113 | 3.71 (1.15) | 46 | 3.8 (1.28) | 10 | 2.3 (1.06) | 13 | 2.54 (0.97) | 182 | 3.57 (1.24) | <0.001 |
| Other care staff | 36 | 3.83 (1.21) | 12 | 3.17 (1.47) | 6 | 2.5 (1.22) | 72 | 3.32 (1.47) | 126 | 3.41 (1.41) | 0.092 |
| Total | 201 | 3.74 (1.13) | 93 | 3.8 (1.22) | 114 | 3.17 (1.39) | 163 | 3.63 (1.38) | 571 | 3.6 (1.29) | 0.001 |
| I was able to take my holiday entitlement | |||||||||||
| Manager/coordinator | 16 | 4.56 (1.09) | 23 | 3.96 (0.88) | 31 | 4.1 (1.35) | 65 | 3.32 (1.68) | 135 | 3.76 (1.49) | 0.006 |
| Registered nurse | 35 | 4.8 (0.58) | 11 | 2.55 (1.51) | 68 | 4.15 (1.22) | 14 | 3.5 (1.83) | 128 | 4.12 (1.34) | <0.001 |
| Nursing assistant | 111 | 4.68 (0.81) | 43 | 4.14 (0.97) | 11 | 4.45 (0.93) | 12 | 3.67 (1.67) | 177 | 4.47 (0.98) | 0.000 |
| Other care staff | 35 | 4.63 (1.06) | 14 | 3.29 (1.33) | 6 | 4.33 (1.63) | 70 | 3.86 (1.43) | 125 | 4.03 (1.39) | 0.006 |
| Total | 199 | 4.69 (0.84) | 92 | 3.77 (1.19) | 116 | 4.17 (1.25) | 162 | 3.6 (1.59) | 569 | 4.13 (1.31) | <0.001 |
| Sweden | Italy | Germany | UK | Total | p Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | M (SD) | n | M (SD) | n | M (SD) | n | M (SD) | n | M (SD) | ||
| My organization received clear guidelines | |||||||||||
| Manager/coordinator | 16 | 4.56 (0.63) | 24 | 2.79 (1.28) | 30 | 2.7 (1.34) | 65 | 3.45 (1.35) | 135 | 3.3 (1.38) | <0.001 |
| Registered nurse | 36 | 3.67 (0.99) | 11 | 3.27 (1.49) | 63 | 3.21 (1.15) | 14 | 3.79 (1.12) | 124 | 3.41 (1.15) | 0.142 |
| Nursing assistant | 118 | 4.31 (0.90) | 48 | 4.42 (0.96) | 11 | 4.09 (0.70) | 13 | 3.62 (1.19) | 190 | 4.28 (0.94) | 0.044 |
| Other care staff | 36 | 4.39 (0.64) | 14 | 3.36 (1.08) | 7 | 3.43 (1.62) | 71 | 3.93 (1.25) | 128 | 3.97 (1.15) | 0.014 |
| Total | 209 | 4.24 (0.89) | 98 | 3.72 (1.31) | 111 | 3.17 (1.25) | 164 | 3.71 (1.28) | 582 | 3.8 (1.22) | <0.001 |
| My organization was supported by the local community | |||||||||||
| Manager/coordinator | 16 | 4.25 (0.77) | 24 | 3.29 (1.20) | 29 | 2.97 (1.12) | 63 | 3.75 (1.27) | 132 | 3.55 (1.23) | 0.002 |
| Registered nurse | 36 | 3.56 (1.03) | 11 | 3.09 (1.30) | 60 | 2.88 (1.24) | 14 | 3.43 (1.16) | 121 | 3.17 (1.20) | 0.047 |
| Nursing assistant | 116 | 3.7 (1.19) | 49 | 3.96 (1.26) | 9 | 2.67 (1.22) | 13 | 3.62 (1.33) | 187 | 3.71 (1.24) | 0.036 |
| Other care staff | 35 | 3.89 (1.05) | 14 | 3 (0.88) | 5 | 2.2 (0.84) | 68 | 3.63 (1.26) | 122 | 3.57 (1.20) | 0.005 |
| Total | 206 | 3.75 (1.11) | 99 | 3.56 (1.25) | 103 | 2.85 (1.18) | 159 | 3.67 (1.25) | 567 | 3.53 (1.23) | <0.001 |
| My organization was supported by clients’ families | |||||||||||
| Manager/coordinator | 13 | 3.92 (1.26) | 24 | 3.25 (0.99) | 31 | 3.16 (1.07) | 65 | 4.06 (0.93) | 133 | 3.69 (1.08) | 0.000 |
| Registered nurse | 32 | 3.66 (0.83) | 12 | 3.08 (1.24) | 63 | 2.92 (1.14) | 14 | 3.5 (0.76) | 121 | 3.2 (1.08) | 0.009 |
| Nursing assistant | 112 | 3.81 (1.12) | 49 | 3.84 (1.14) | 10 | 3.2 (0.92) | 13 | 3.38 (1.12) | 184 | 3.76 (1.12) | 0.220 |
| Other care staff | 32 | 3.84 (0.88) | 14 | 3 (1.11) | 7 | 3.29 (1.25) | 71 | 3.82 (1.19) | 124 | 3.7 (1.13) | 0.054 |
| Total | 192 | 3.8 (1.04) | 100 | 3.48 (1.15) | 111 | 3.04 (1.10) | 164 | 3.86 (1.07) | 567 | 3.61 (1.12) | <0.001 |
| Management | Registered Nurse | Nursing Assistant | Other Care Staff | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient | p-Value | Coefficient | p-Value | Coefficient | p-Value | Coefficient | p-Value | Coefficient | p-Value | |
| Country (ref: Sweden) | ||||||||||
| Italy | 1.34 ± 0.85 | 0.113 | 1.89 ± 0.78 | 0.015 | −0.14 ± 0.46 | 0.759 | 0.13 ± 0.76 | 0.868 | 0.32 ± 0.29 | 0.273 |
| Germany | 1.57 ± 0.85 | 0.064 | 2.12 ± 0.55 | <0.001 | −0.05 ± 0.81 | 0.947 | 0.15 ± 1.06 | 0.889 | 0.78 ± 0.29 | 0.007 |
| UK | 1.80 ± 0.78 | 0.021 | 3.22 ± 0.87 | <0.001 | 0.98 ± 0.72 | 0.173 | 1.31 ± 0.66 | 0.046 | 1.59 ± 0.31 | <0.001 |
| Age | −0.03 ± 0.02 | 0.093 | 0.05 ± 0.02 | 0.002 | 0.00 ± 0.01 | 0.706 | −0.03 ± −0.04 | 0.014 | 0.00 ± 0.01 | 0.643 |
| Gender (ref: male) | ||||||||||
| Female | 0.47 ± 0.55 | 0.397 | −0.46 ± 0.63 | 0.462 | 0.29 ± 0.57 | 0.615 | 0.52 ± 0.64 | 0.417 | −1.27 ± 1.14 | 0.268 |
| Organization (ref: Public organization) | ||||||||||
| Private | 0.25 ± 0.62 | 0.688 | −0.75 ± 0.48 | 0.118 | −0.67 ± 0.47 | 0.154 | −0.15 ± 0.58 | 0.796 | −0.32 ± 0.24 | 0.185 |
| Non-profit | 1.60 ± 0.90 | 0.076 | −0.83 ± 0.55 | 0.127 | 0.17 ± 1.43 | 0.908 | 0.22 ± 1.10 | 0.844 | 0.35 ± 0.38 | 0.350 |
| My management supported me adequately (1 point increase) | −0.68 ± 0.24 | 0.005 | −0.34 ± 0.18 | 0.054 | −0.37 ± 0.21 | 0.088 | 0.01 ± 0.27 | 0.972 | −0.36 ± 0.10 | <0.001 |
| My voice has been listened to by my organization (1 point increase) | 0.47 ± 0.25 | 0.060 | 0.13 ± 0.19 | 0.512 | −0.04 ± 0.22 | 0.848 | −0.24 ± 0.27 | 0.374 | 0.17 ± 0.10 | 0.106 |
| I have been able to take the holiday leave I am entitled to this year (1 point increase) | −0.11 ± 0.12 | 0.351 | −0.33 ± 0.17 | 0.045 | −0.29 ± 0.19 | 0.122 | −0.31 ± 0.16 | 0.061 | 0.32 ± 0.29 | 0.273 |
| Support from within the Organization | External Support | Cumulative COVID-19-Related Deaths Per Million Population by the Beginning of the Study | Stress and Anxiety Level | |
|---|---|---|---|---|
| Sweden | very high | high | high | low |
| Italy | high | medium | high | medium |
| Germany | medium | low | low | high |
| UK | high | high | very high | high |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lethin, C.; Kenkmann, A.; Chiatti, C.; Christensen, J.; Backhouse, T.; Killett, A.; Fisher, O.; Malmgren Fänge, A. Organizational Support Experiences of Care Home and Home Care Staff in Sweden, Italy, Germany and the United Kingdom during the COVID-19 Pandemic. Healthcare 2021, 9, 767. https://doi.org/10.3390/healthcare9060767
Lethin C, Kenkmann A, Chiatti C, Christensen J, Backhouse T, Killett A, Fisher O, Malmgren Fänge A. Organizational Support Experiences of Care Home and Home Care Staff in Sweden, Italy, Germany and the United Kingdom during the COVID-19 Pandemic. Healthcare. 2021; 9(6):767. https://doi.org/10.3390/healthcare9060767
Chicago/Turabian StyleLethin, Connie, Andrea Kenkmann, Carlos Chiatti, Jonas Christensen, Tamara Backhouse, Anne Killett, Oliver Fisher, and Agneta Malmgren Fänge. 2021. "Organizational Support Experiences of Care Home and Home Care Staff in Sweden, Italy, Germany and the United Kingdom during the COVID-19 Pandemic" Healthcare 9, no. 6: 767. https://doi.org/10.3390/healthcare9060767
APA StyleLethin, C., Kenkmann, A., Chiatti, C., Christensen, J., Backhouse, T., Killett, A., Fisher, O., & Malmgren Fänge, A. (2021). Organizational Support Experiences of Care Home and Home Care Staff in Sweden, Italy, Germany and the United Kingdom during the COVID-19 Pandemic. Healthcare, 9(6), 767. https://doi.org/10.3390/healthcare9060767







