Safety and Efficacy of Specially Designed Texture-Modified Foods for Patients with Dysphagia Due to Brain Disorders: A Prospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Videofluoroscopic Swallowing Study
2.4. Outcome Measures
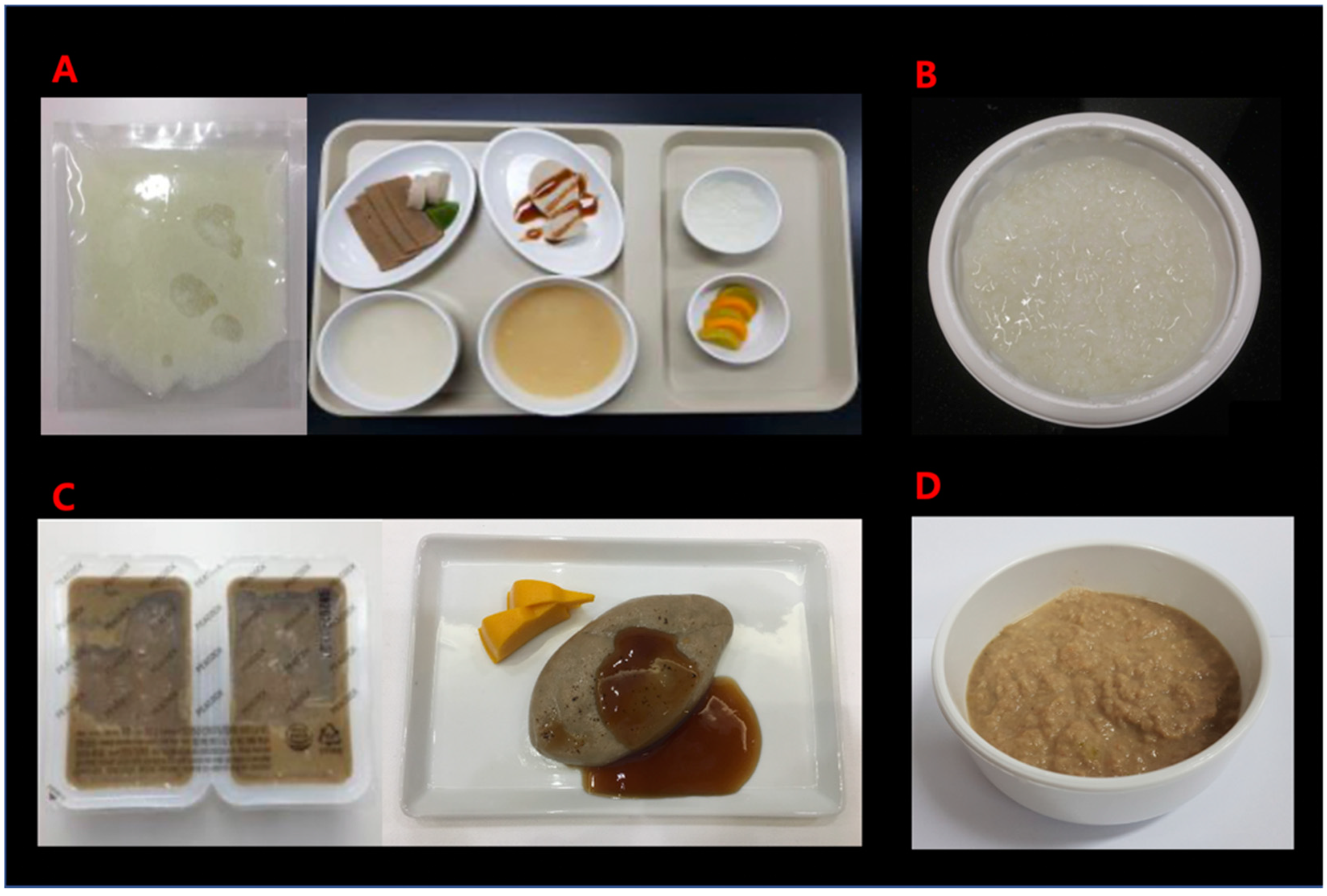
2.5. Texture Analysis of the Study and Control Foods
2.6. Standard Protocol Approvals, Registrations and Patient Consents
2.7. Statistical Analysis
3. Results
3.1. Rice Gruel versus Rice Porridge
3.2. Bulgogi Mousse versus Ground Bulgogi
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bourne, M. Food Texture and Viscosity, 2nd ed.; Academic Press: London, UK, 2002. [Google Scholar]
- Murry, T.; Carrau, R.L.; Chan, K. Clinical Management of Swallowing Disorders, 2nd ed.; Plural Publishing: San Diego, CA, USA, 2006. [Google Scholar]
- Takasaki, K.; Umeki, H.; Enatsu, K.; Tanaka, F.; Sakihama, N.; Kumagami, H.; Takahashi, H. Investigation of pharyngeal swallowing function using high-resolution manometry. Laryngoscope 2008, 118, 1729–1732. [Google Scholar] [CrossRef]
- Bredenoord, A.J.; Smout, A.J. High-resolution manometry. Dig. Liver Dis. 2008, 40, 174–181. [Google Scholar] [CrossRef]
- Omari, T.I.; Rommel, N.; Szczesniak, M.M.; Fuentealba, S.; Dinning, P.G.; Davidson, G.P.; Cook, I.J. Assessment of intraluminal impedance for the detection of pharyngeal bolus flow during swallowing in healthy adults. Am. J. Physiol. Gastrointest. Liver Physiol. 2006, 290, G183–G188. [Google Scholar] [CrossRef]
- Hasegawa, A.; Otoguro, A.; Kumagai, H.; Nakazawa, F. Velocity of Swallowed Gel Food in the Pharynx by Ultrasonic Method. Nippon Shokuhin Kagaku Kogaku Kaishi 2005, 52, 441–447. [Google Scholar] [CrossRef]
- Lee, S.H.; Oh, B.M.; Chun, S.M.; Lee, J.C.; Min, Y.; Bang, S.H.; Kim, H.C.; Han, T.R. The accuracy of the swallowing kinematic analysis at various movement velocities of the hyoid and epiglottis. Ann. Rehabil. Med. 2013, 37, 320–327. [Google Scholar] [CrossRef]
- Hanson, B. A review of diet standardization and bolus rheology in the management of dysphagia. Curr. Opin. Otolaryngol. Head Neck Surg. 2016, 24, 183–190. [Google Scholar] [CrossRef]
- Ekberg, O. Dysphagia: Diagnosis and Treatment, 2nd ed.; Springer: Berlin/Heidelberg, Germany, 2019. [Google Scholar]
- Flynn, E.; Smith, C.H.; Walsh, C.D.; Walshe, M. Modifying the consistency of food and fluids for swallowing difficulties in dementia. Cochrane Database Syst. Rev. 2018, 9, Cd011077. [Google Scholar] [CrossRef]
- O’Keeffe, S.T. Use of modified diets to prevent aspiration in oropharyngeal dysphagia: Is current practice justified? BMC Geriatr. 2018, 18, 167. [Google Scholar] [CrossRef] [PubMed]
- Painter, V.; Le Couteur, D.G.; Waite, L.M. Texture-modified food and fluids in dementia and residential aged care facilities. Clin. Interv. Aging 2017, 12, 1193–1203. [Google Scholar] [CrossRef] [PubMed]
- Vucea, V.; Keller, H.H.; Morrison, J.M.; Duizer, L.M.; Duncan, A.M.; Carrier, N.; Lengyel, C.O.; Slaughter, S.E.; Steele, C.M. Modified Texture Food Use is Associated with Malnutrition in Long Term Care: An Analysis of Making the Most of Mealtimes (M3) Project. J. Nutr. Health Aging 2018, 22, 916–922. [Google Scholar] [CrossRef] [PubMed]
- Cichero, J.A.Y. Age-Related Changes to Eating and Swallowing Impact Frailty: Aspiration, Choking Risk, Modified Food Texture and Autonomy of Choice. Geriatrics 2018, 3, 69. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, A.; Maeda, K.; Tanaka, K.; Ogawa, M.; Kayashita, J. Texture-modified diets are associated with decreased muscle mass in older adults admitted to a rehabilitation ward. Geriat.r Gerontol. Int. 2018, 18, 698–704. [Google Scholar] [CrossRef]
- Frazier, J.; Chestnut, A.H.; Jackson, A.; Barbon, C.E.; Steele, C.M.; Pickler, L. Understanding the Viscosity of Liquids used in Infant Dysphagia Management. Dysphagia 2016, 31, 672–679. [Google Scholar] [CrossRef]
- Steele, C.M.; Alsanei, W.A.; Ayanikalath, S.; Barbon, C.E.; Chen, J.; Cichero, J.A.; Coutts, K.; Dantas, R.O.; Duivestein, J.; Giosa, L.; et al. The influence of food texture and liquid consistency modification on swallowing physiology and function: A systematic review. Dysphagia 2015, 30, 2–26. [Google Scholar] [CrossRef] [PubMed]
- Rosenbek, J.C.; Robbins, J.A.; Roecker, E.B.; Coyle, J.L.; Wood, J.L. A penetration-aspiration scale. Dysphagia 1996, 11, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Han, T.R.; Paik, N.J.; Park, J.W. Quantifying swallowing function after stroke: A functional dysphagia scale based on videofluoroscopic studies. Arch. Phys. Med. Rehabil. 2001, 82, 677–682. [Google Scholar] [CrossRef]
- Kang, A.; Kim, D.; Kang, S.; Seo, K.; Park, H.; Park, K. EMG Activity of Masseter Muscles in the Elderly According to Rheological Properties of Solid Food. Ann. Rehabil. Med. 2016, 40, 447–456. [Google Scholar] [CrossRef]
- Tokifuji, A.; Matsushima, Y.; Hachisuka, K.; Yoshioka, K. Texture, sensory and swallowing characteristics of high-pressure-heat-treated pork meat gel as a dysphagia diet. Meat Sci. 2013, 93, 843–848. [Google Scholar] [CrossRef] [PubMed]
- Zargaraan, A.; Rastmanesh, R.; Fadavi, G.; Zayeri, F.; Mohammadifar, M.A. Rheological aspects of dysphagia-oriented food products: A mini review. Food Sci. Hum. Wellness 2013, 2, 173–178. [Google Scholar] [CrossRef]
- Nyström, M. Extensional Rheometry through Hyperbolic Contraction; Chalmers University of Technology: Göteborg, Sweden, 2015. [Google Scholar]
- Steele, C.M.; Molfenter, S.M.; Péladeau-Pigeon, M.; Stokely, S. Challenges in preparing contrast media for videofluoroscopy. Dysphagia 2013, 28, 464–467. [Google Scholar] [CrossRef] [PubMed]
- Newman, R.; Vilardell, N.; Clavé, P.; Speyer, R. Effect of Bolus Viscosity on the Safety and Efficacy of Swallowing and the Kinematics of the Swallow Response in Patients with Oropharyngeal Dysphagia: White Paper by the European Society for Swallowing Disorders (ESSD). Dysphagia 2016, 31, 232–249. [Google Scholar] [CrossRef]
- Steele, C.M.; Cichero, J.A. A question of rheological control. Dysphagia 2008, 23, 199–201. [Google Scholar] [CrossRef] [PubMed]
- Steele, C.M.; Van Lieshout, P.H.; Goff, H.D. The rheology of liquids: A comparison of clinicians’ subjective impressions and objective measurement. Dysphagia 2003, 18, 182–195. [Google Scholar] [CrossRef]
- National Dysphagia Diet Task, F.; American Dietetic, A. National Dysphagia Diet: Standardization for Optimal Care; American Dietetic Association: Chicago, IL, USA, 2002. [Google Scholar]
- The British Dietetic Association and the Royal College of Speech and Language Therapist. National Descriptors for Texture Modification in Adults; The British Dietetic Association and the Royal College of Speech and Language Therapist: London, UK, 2002. [Google Scholar]
- Cichero, J.A.; Steele, C.; Duivestein, J.; Clavé, P.; Chen, J.; Kayashita, J.; Dantas, R.; Lecko, C.; Speyer, R.; Lam, P.; et al. The Need for International Terminology and Definitions for Texture-Modified Foods and Thickened Liquids Used in Dysphagia Management: Foundations of a Global Initiative. Curr. Phys. Med. Rehabil. Rep. 2013, 1, 280–291. [Google Scholar] [CrossRef]
- Cichero, J.A.; Lam, P.; Steele, C.M.; Hanson, B.; Chen, J.; Dantas, R.O.; Duivestein, J.; Kayashita, J.; Lecko, C.; Murray, J.; et al. Development of International Terminology and Definitions for Texture-Modified Foods and Thickened Fluids Used in Dysphagia Management: The IDDSI Framework. Dysphagia 2017, 32, 293–314. [Google Scholar] [CrossRef] [PubMed]
- Higashiguchi, T.; Ito, A.; Nishiyama, H.; Shigematsu, T.; Ishikawa, A.; Kato, H.; Iijima, S.; Kikuchi, N. Appropriate nutritional management in patients with impaired mastication and those with mild dysphagia: A multicenter study of the usefulness of novel foods processed and softened by enzymes. Asia Pac. J. Clin. Nutr. 2017, 26, 1007–1015. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, A.; Momosaki, R.; Kayashita, J.; Fujishima, I. Impact of Multiple Texture-Modified Diets on Oral Intake and Nutritional Status in Older Patients with Pneumonia: A Retrospective Cohort Study. Dysphagia 2020, 35, 574–582. [Google Scholar] [CrossRef]
| Stage 1 | Stage 2 | Stage 3 | Stage 4 | |
|---|---|---|---|---|
| Classifications | Able to chew easily | Able to smash with gums | Able to smash with tongue | Able to swallow without chewing |
| Standards of chewing | Contains hard and big ingredients, a little hard to swallow | Contains hard and big ingredients not easy to swallow | Contains soft and small ingredients, easy to swallow | Hard to swallow if contains solid food |
| Standards of swallowing | Able to swallow commonly | Depends on ingredients, hard to swallow | Have experience hard to swallow water or liquid ingredients | Hard to swallow water or liquid ingredients |
| Hardness (N/m2) | 5 × 105 | 5 × 104 | 2 × 104 | 5 × 103 |
| Rice Gruel vs. Rice Porridge | Bulgogi Mousse vs. Ground Bulgogi | p-Value | |
|---|---|---|---|
| Age (years) (mean ± SD) | 72.00 ± 15.17 | 72.73 ± 12.05 | 0.736 a |
| Male: Female (n) | 23:27 | 26:25 | 0.482 b |
| Diagnosis (n) | 0.350 c | ||
| Ischemic stroke | 23 | 27 | |
| Hemorrhagic stroke | 13 | 6 | |
| Alzheimer’s disease | 6 | 12 | |
| Parkinson’s disease | 4 | 3 | |
| Brain tumor | 2 | 1 | |
| Hypoxic ischemic brain injury | 1 | 0 | |
| Traumatic brain injury | 1 | 2 | |
| Disease duration (n) | 0.622 b | ||
| <6 months | 25 | 28 | |
| ≥6 months | 25 | 23 |
| Temperature | Rice Gruel | Bulgogi Mousse | Rice Porridge | Rice Gruel + Bonorex | Bulgogi Mousse + Bonorex | Rice Porridge + Bonorex | |
|---|---|---|---|---|---|---|---|
| 40~50 °C | Hardness (N/m2) | 569 ± 76 | 4479 ± 359 | 1824 ± 240 | 483 ± 89 | 5603 ± 1882 | - |
| Adhesiveness (N·mm) | 1.13 ± 0.07 | 4.01 ± 0.13 | 3.86 ± 0.54 | 0.33 ± 0.02 | 2.35 ± 0.72 | - | |
| UDF stage | 4 | 3 | 4 | 4 | 3 | - | |
| Calories (kcal/100 g) | 64.72 | 72.57 | 51.85 | - | - | - | |
| 20~25 °C | Hardness (N/m2) | 1049 ± 229 | 17,077 ± 648 | 1681 ± 41 | 1386 ± 109 | 18,871 ± 367 | 1894 ± 157 |
| Adhesiveness (N·mm) | 1.23 ± 0.14 | 4.90 ± 0.28 | 4.60 ± 0.59 | 0.28 ± 0.04 | 4.00 ± 0.31 | 2.27 ± 0.47 | |
| UDF stage | 4 | 3 | 4 | 4 | 3 | 4 |
| Rice Gruel a | Rice Porridge b | p-Value | Bulgogi Mousse a | Ground Bulgogi b | p-Value | |
|---|---|---|---|---|---|---|
| Oropharyngeal transit time (seconds) | 39.88 ± 18.40 | 61.08 ± 28.59 | <0.001 c* | 40.29 ± 28.03 | 37.51 ± 19.94 | 0.486 c |
| Number of swallows required to maximally eliminate the food materials from the oropharyngeal space | 4 (3;6) | 5 (4;7) | <0.001 d* | 3 (2;4) | 2 (2;3) | 0.007 d* |
| The vallecular residue after swallowing scale score | 1 (1;1) | 1 (1;1) | 0.132 d | 1 (1;2) | 1 (1;2) | 1.000 d |
| The pyriform sinus residue after swallowing scale score | 1 (0;1) | 1 (0;1) | 0.054 d | 1 (0;1) | 1 (0;1) | 0.819 d |
| The Penetration-Aspiration Scale score | 1 (1;2) | 1 (1;2) | 0.317 d | 1 (1;1) | 1 (1;2) | 0.038 d* |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwak, S.; Choo, Y.J.; Choi, K.T.; Chang, M.C. Safety and Efficacy of Specially Designed Texture-Modified Foods for Patients with Dysphagia Due to Brain Disorders: A Prospective Study. Healthcare 2021, 9, 728. https://doi.org/10.3390/healthcare9060728
Kwak S, Choo YJ, Choi KT, Chang MC. Safety and Efficacy of Specially Designed Texture-Modified Foods for Patients with Dysphagia Due to Brain Disorders: A Prospective Study. Healthcare. 2021; 9(6):728. https://doi.org/10.3390/healthcare9060728
Chicago/Turabian StyleKwak, Soyoung, Yoo Jin Choo, Kyu Tae Choi, and Min Cheol Chang. 2021. "Safety and Efficacy of Specially Designed Texture-Modified Foods for Patients with Dysphagia Due to Brain Disorders: A Prospective Study" Healthcare 9, no. 6: 728. https://doi.org/10.3390/healthcare9060728
APA StyleKwak, S., Choo, Y. J., Choi, K. T., & Chang, M. C. (2021). Safety and Efficacy of Specially Designed Texture-Modified Foods for Patients with Dysphagia Due to Brain Disorders: A Prospective Study. Healthcare, 9(6), 728. https://doi.org/10.3390/healthcare9060728







