Psychometric Properties of the Self-Healing Assessment Scale for Community-Dwelling Older Adults
Abstract
1. Introduction
2. Methodology
2.1. Instruments and Procedure
2.1.1. Phase 1: Item Development of the Initial Version of SHAS
2.1.2. Phase 2: Scale Development for Examining the Reliability and Validity of SHAS
2.1.3. Phase 3: Scale Evaluation of the Final Version of SHAS
2.2. Sample/Participants
2.3. Ethical Considerations
3. Results
3.1. The Characteristics of the Participants
3.2. Content Validity and Item Analysis
3.3. Exploratory Factorial Analysis and Reliability
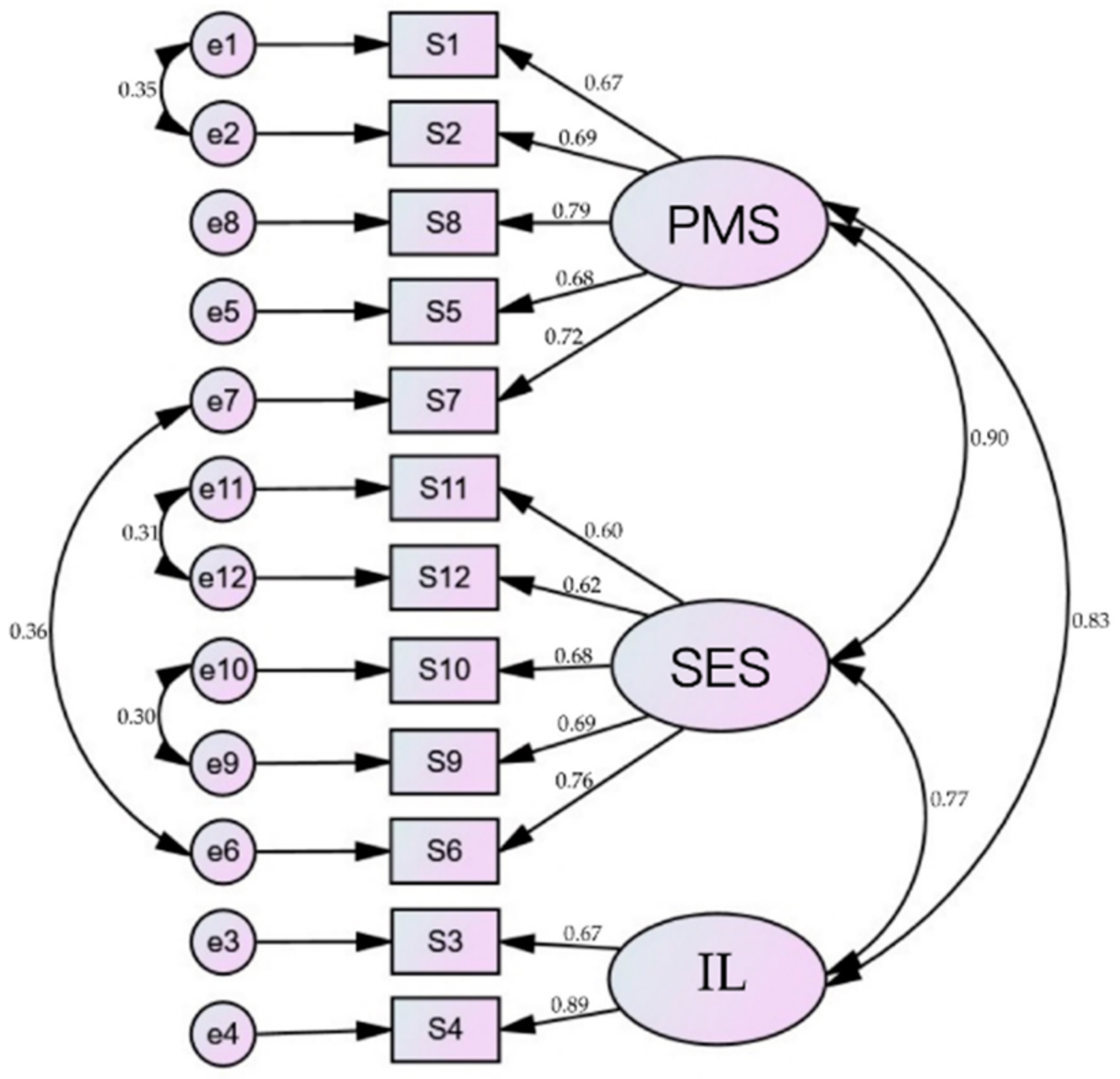
3.4. Confirmatory Factorial Analysis and Concurrent Validity
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Bartholomaeus, J.D.; Van Agteren, J.E.M.; Iasiello, M.P.; Jarden, A.; Kelly, D. Positive aging: The impact of a community wellbeing and resilience program. Clin. Gerontol. 2019, 42, 377–386. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 13 July 2020).
- Beard, J.R.; Officer, A.; de Carvalho, I.A.; Sadana, R.; Pot, A.M.; Michel, J.P.; Lloyd-Sherlock, P.; Epping-Jordan, J.E.; Peeters, G.; Mahanani, W.R.; et al. The World report on ageing and health: A policy framework for healthy ageing. Lancet 2016, 387, 2145–2154. [Google Scholar] [CrossRef]
- Wong, R.Y. A new strategic approach to successful aging and healthy aging. Geriatrics 2018, 3, 86. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. What is Healthy Ageing? Available online: https://www.who.int/%20ageing/healthy-ageing/en/ (accessed on 13 July 2020).
- Dawson-Townsend, K. Social participation patterns and their associations with health and well-being for older adults. SSM Popul. Health 2019, 8, 100424. [Google Scholar] [CrossRef]
- Maula, A.; LaFond, N.; Orton, E.; Iliffe, S.; Audsley, S.; Vedhara, K.; Kendrick, D. Use it or lose it: A qualitative study of the maintenance of physical activity in older adults. BMC Geriatr. 2019, 19, 349. [Google Scholar] [CrossRef]
- Courtin, E.; Knapp, M. Social isolation, loneliness and health in old age: A scoping review. Health Soc. Care Commun. 2017, 25, 799–812. [Google Scholar] [CrossRef]
- Kemperman, A.; van den Berg, P.; Weijs-Perrée, M.; Uijtdewillegen, K. Loneliness of older adults: Social network and the living environment. Int. J. Environ. Res. Public Health 2019, 16, 406. [Google Scholar] [CrossRef] [PubMed]
- Liao, W.C.; Li, C.R.; Lin, Y.C.; Wang, C.C.; Chen, Y.J.; Yen, C.H.; Lin, H.S.; Lee, M.C. Healthy behaviors and onset of functional disability in older adults: Results of a national longitudinal study. J. Am. Geriatr. Soc. 2011, 59, 200–206. [Google Scholar] [CrossRef]
- Ingram, C. A paradigm shift: Healing, quality of life, and a professional choice. J. Pain Symptom Manag. 2014, 47, 198–201. [Google Scholar] [CrossRef]
- Mount, B. Healing, quality of life, and the need for a paradigm shift in health care. J. Palliat. Care 2013, 29, 45–48. [Google Scholar] [CrossRef]
- Sloan, D.H.; BrintzenhofeSzoc, K.; Kichline, T.; Baker, K.; Pinzon, J.P.; Tafe, C.; Li, L.; Cheng, M.J.; Berger, A. An assessment of meaning in life-threatening illness: Development of the Healing Experience in All Life Stressors (HEALS). Patient Relat. Outcome Meas. 2017, 8, 15–21. [Google Scholar] [CrossRef]
- Boyd, K.M. Disease, illness, sickness, health, healing and wholeness: Exploring some elusive concepts. Med Humanit. 2000, 26, 9–17. [Google Scholar] [CrossRef]
- Egnew, T.R. The meaning of healing: Transcending suffering. Ann. Fam. Med. 2005, 3, 255–262. [Google Scholar] [CrossRef]
- Clark, C.C. Inner dialogue: A self-healing approach for nurses and clients. Am. J. Nurs. 1981, 81, 1191–1193. [Google Scholar] [CrossRef]
- Quinn, J.F. The self as healer: Reflections from a nurse’s journey. AACN Clin. Issues 2000, 11, 17–26. [Google Scholar] [CrossRef]
- Robb, W.J. Self-healing: A concept analysis. Nurs. Forum 2006, 41, 60–77. [Google Scholar] [CrossRef]
- Tennant, R. Identity awareness as a holistic approach to self-healing. Geriatr. Nurs. 1981, 2, 355–358. [Google Scholar] [CrossRef]
- Rovesti, M.; Fioranelli, M.; Petrelli, P.; Satolli, F.; Roccia, M.G.; Gianfaldoni, S.; Tchernev, G.; Wollina, U.; Lotti, J.; Feliciani, C.; et al. Health and illness in history, science and society. Open Access Maced. J. Med. Sci. 2018, 6, 163–165. [Google Scholar] [CrossRef] [PubMed]
- Fábrega, H., Jr. Evolution of Sickness and Healing; University of California Press: Berkeley, CA, USA, 1997; p. 9. [Google Scholar]
- Dunphy, L.M. Book review: Florence nightingale today: Healing, leadership, global action. Nurs. Sci. Q. 2006, 19, 74–76. [Google Scholar] [CrossRef]
- McKie, J. A personal conceptualization of healing. Aust. J. Holist. Nurs. 2003, 10, 34–38. [Google Scholar] [PubMed]
- Mount, B.M.; Boston, P.H.; Cohen, S.R. Healing connections: On moving from suffering to a sense of well-being. J. Pain Symptom Manag. 2007, 33, 372–388. [Google Scholar] [CrossRef]
- Bernick, L. Caring for older adults: Practice guided by Watson’s caring-healing model. Nurs. Sci. Q. 2004, 17, 128–134. [Google Scholar] [CrossRef] [PubMed]
- McElligott, D. Healing: The journey from concept to nursing practice. J. Holist. Nurs. 2010, 28, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Firth, K.; Smith, K.; Sakallaris, B.R.; Bellanti, D.M.; Crawford, C.; Avant, K.C. Healing, a concept analysis. Glob. Adv. Health Med. 2015, 4, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Loizzo, J.; Charlson, M.; Peterson, J. A program in contemplative self-healing: Stress, allostasis, and learning in the Indo-Tibetan tradition. Ann. N. Y. Acad. Sci. 2009, 1172, 123–147. [Google Scholar] [CrossRef] [PubMed]
- Loizzo, J.; Blackhall, L.J.; Rapgay, L. Tibetan medicine: A complementary science of optimal health. Ann. N. Y. Acad. Sci. 2009, 1172, 218–230. [Google Scholar] [CrossRef]
- Charlson, M.E.; Loizzo, J.; Moadel, A.; Neale, M.; Newman, C.; Olivo, E.; Wolf, E.; Peterson, J.C. Contemplative self healing in women breast cancer survivors: A pilot study in underserved minority women shows improvement in quality of life and reduced stress. BMC Complement. Altern. Med. 2014, 14, 349. [Google Scholar] [CrossRef]
- Offidani, E.; Peterson, J.C.; Loizzo, J.; Moore, A.; Charlson, M.E. Stress and Response to Treatment: Insights from a pilot study using a 4-week contemplative self-healing meditation intervention for posttraumatic stress in breast cancer. J. Evid. Based Complement. Altern. Med. 2017, 22, 715–720. [Google Scholar] [CrossRef]
- Logan, A.C.; Selhub, E.M. Vis Medicatrix naturae: Does nature “minister to the mind”? Biopsychosoc. Med. 2012, 6, 11. [Google Scholar] [CrossRef]
- Prolo, P.; Chiappelli, F.; Fiorucci, A.; Dovio, A.; Sartori, M.L.; Angeli, A. Psychoneuroimmunology: New avenues of research for the twenty-first century. Ann. N. Y. Acad. Sci. 2002, 966, 400–408. [Google Scholar] [CrossRef]
- Scott, C.V.; Hyer, L.A.; McKenzie, L.C. The healing power of laughter: The applicability of humor as a psychotherapy technique with depressed and anxious older adults. Soc. Work Ment. Health 2015, 13, 48–60. [Google Scholar] [CrossRef]
- Mlinac, M.E.; Feng, M.C. Assessment of activities of daily living, self-care, and independence. Arch. Clin. Neuropsychol. 2016, 31, 506–516. [Google Scholar] [CrossRef] [PubMed]
- Quach, A.; Levine, M.E.; Tanaka, T.; Lu, A.T.; Chen, B.H.; Ferrucci, L.; Ritz, B.; Bandinelli, S.; Neuhouser, M.L.; Beasley, J.M.; et al. Epigenetic clock analysis of diet, exercise, education, and lifestyle factors. Aging 2017, 9, 419–446. [Google Scholar] [CrossRef]
- Boateng, G.O.; Neilands, T.B.; Frongillo, E.A.; Melgar-Quiñonez, H.R.; Young, S.L. Best practices for developing and validating scales for health, social, and behavioral research: A primer. Front. Public Health 2018, 6, 149. [Google Scholar] [CrossRef]
- Terwee, C.B.; Bot, S.D.; de Boer, M.R.; van der Windt, D.A.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Davis, L.L. Instrument review: Getting the most from a panel of experts. Appl. Nurs. Res. 1992, 5, 194–197. [Google Scholar] [CrossRef]
- Hartley, J. Some thoughts on Likert-type scales. Int. J. Clin. Health Psychol. 2014, 14, 83–86. [Google Scholar] [CrossRef]
- Pett, M.A.; Lackey, N.R.; Sullivan, J.J. Making Sense of Factor Analysis: The Use of Factor Analysis for Instrument Development in Health Care Research; SAGE Publications: Thousand Oaks, CA, USA, 2003. [Google Scholar]
- Swisher, L.L.; Beckstead, J.W.; Bebeau, M.J. Factor analysis as a tool for survey analysis using a professional role orientation inventory as an example. Phys Ther. 2004, 84, 784–799. [Google Scholar] [CrossRef]
- Polit, D.F.; Beck, C.T. Nursing Research: Generating and Assessing Evidence for Nursing Practice; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2017; pp. 335–348. [Google Scholar]
- Kaiser, H.F. An index of factorial simplicity. Psychometrika 1974, 39, 31–36. [Google Scholar] [CrossRef]
- Braeken, J.; van Assen, M.A.L.M. An empirical Kaiser criterion. Psychol. Methods 2017, 22, 450–466. [Google Scholar] [CrossRef]
- Comrey, A.L.; Lee, H.B. A First Course in Factor Analysis, 2nd ed.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1992. [Google Scholar]
- Ursachi, G.; Horodnic, I.A.; Zait, A. How reliable are measurement scales? External factors with indirect influence on reliability estimators. Proc. Econ. 2015, 20, 679–686. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Galenkamp, H.; Stronks, K.; Mokkink, L.B.; Derks, E.M. Measurement invariance of the SF-12 among different demographic groups: The HELIUS study. PLoS ONE 2018, 13, e0203483. [Google Scholar] [CrossRef]
- Li, Y.P.; Huang, H.T. The concept and measurement of quality of life in elderly population. Taiwan Geriatr. Gerontol. 2014, 9, 57–67. [Google Scholar] [CrossRef]
- Wu, Y.C.; Tung, H.H.; Wei, J. Quality of life, demoralization syndrome and health-related lifestyle in cardiac transplant recipients—A longitudinal study in Taiwan. Eur. J. Cardiovasc. Nurs. 2019, 18, 149–162. [Google Scholar] [CrossRef]
- Walters, K.; Kharicha, K.; Goodman, C.; Handley, M.; Manthorpe, J.; Cattan, M.; Morris, S.; Clarke, C.S.; Round, J.; Iliffe, S. Promoting independence, health and well-being for older people: A feasibility study of computer-aided health and social risk appraisal system in primary care. BMC Fam. Pract. 2017, 18, 47. [Google Scholar] [CrossRef]
- Matz-Costa, C.; Carr, D.C.; McNamara, T.K.; James, J.B. Physical, cognitive, social, and emotional mediators of activity involvement and health in later life. Res. Aging 2016, 38, 791–815. [Google Scholar] [CrossRef] [PubMed]
- Hikichi, H.; Kondo, K.; Takeda, T.; Kawachi, I. Social interaction and cognitive decline: Results of a 7-year community intervention. Alzheimers Dement. 2016, 3, 23–32. [Google Scholar] [CrossRef]
- Lin, L.; Lu, L.C.; Chen, H.L.; Wei, J.; Tung, H.H.; Wu, Y.C. Self-healing in post cardiac surgery patients: A qualitative study. AMH 2021, 12, 4–11. [Google Scholar]
- Ministry of Health and Welfare. National Statistic Report of R. O. C. Available online: https://www.moi.gov.tw/stat/chart.aspx (accessed on 13 July 2020).
- Eisinga, R.; Grotenhuis, M.T.; Pelzer, B. The reliability of a two-item scale: Pearson, Cronbach, or Spearman-Brown? Int. J. Public Health 2013, 58, 637–642. [Google Scholar] [CrossRef]
| Questionnaire Items | Mean | Std. Deviation | Skewness | Kurtosis | t | 95% Confidence Interval | |||
|---|---|---|---|---|---|---|---|---|---|
| Statistic | Statistic | Statistic | Std. Error | Statistic | Std. Error | Lower | Upper | ||
| Item 1. | 3.16 | 0.51 | 0.25 | 0.11 | 0.38 | 0.22 | |||
| Item 2. | 3.06 | 0.54 | 0.05 | 0.11 | 0.45 | 0.22 | −13.18 * | −0.64 | −0.47 |
| Item 3. | 3.39 | 0.55 | −0.17 | 0.11 | −0.45 | 0.22 | −30.09 * | −0.94 | −0.82 |
| Item 4. | 3.23 | 0.51 | 0.28 | 0.11 | −0.17 | 0.22 | −18.50 * | −0.75 | −0.60 |
| Item 5. | 3.15 | 0.51 | 0.04 | 0.11 | 1.28 | 0.22 | −14.59 * | −0.65 | −0.50 |
| Item 6. | 3.14 | 0.51 | 0.05 | 0.11 | 1.48 | 0.22 | −17.58 * | −0.84 | −0.67 |
| Item 7. | 3.15 | 0.51 | 0.14 | 0.11 | 0.94 | 0.22 | −19.40 * | −0.87 | −0.71 |
| Item 8. | 3.10 | 0.57 | 0.01 | 0.11 | −0.02 | 0.22 | −21.75 * | −0.98 | −0.82 |
| Item 9. | 3.11 | 0.56 | −0.10 | 0.11 | 0.69 | 0.22 | −15.38 * | −0.77 | −0.60 |
| Item 10. | 3.15 | 0.50 | 0.19 | 0.11 | 1.07 | 0.22 | −15.37 * | −0.70 | −0.55 |
| Item 11. | 3.24 | 0.53 | −0.02 | 0.11 | 0.60 | 0.22 | −18.99 * | −0.82 | −0.67 |
| Item 12. | 3.22 | 0.51 | 0.21 | 0.11 | 0.50 | 0.22 | −17.53 * | −0.76 | −0.60 |
| Item | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | - | |||||||||||
| 2 | 0.65 ** | - | ||||||||||
| 3 | 0.38 ** | 0.38 ** | - | |||||||||
| 4 | 0.53 ** | 0.53 ** | 0.60 ** | - | ||||||||
| 5 | 0.49 ** | 0.51 ** | 0.43 ** | 0.53 ** | - | |||||||
| 6 | 0.46 ** | 0.45 ** | 0.39 ** | 0.52 ** | 0.50 ** | - | ||||||
| 7 | 0.44 ** | 0.47 ** | 0.36 ** | 0.50 ** | 0.42 ** | 0.67 ** | - | |||||
| 8 | 0.54 ** | 0.55 ** | 0.43 ** | 0.55 ** | 0.50 ** | 0.55 ** | 0.65 ** | - | ||||
| 9 | 0.43 ** | 0.39 ** | 0.30 ** | 0.46 ** | 0.47 ** | 0.52 ** | 0.43 ** | 0.47 ** | - | |||
| 10 | 0.37 ** | 0.36 ** | 0.34 ** | 0.46 ** | 0.40 ** | 0.50 ** | 0.48 ** | 0.47 ** | 0.63 ** | - | ||
| 11 | 0.34 ** | 0.36 ** | 0.32 ** | 0.39 ** | 0.34 ** | 0.45 ** | 0.44 ** | 0.40 ** | 0.43 ** | 0.48 ** | - | |
| 12 | 0.33 ** | 0.36 ** | 0.33 ** | 0.45 ** | 0.36 ** | 0.47 ** | 0.45 ** | 0.41 ** | 0.43 ** | 0.47 ** | 0.57 ** | - |
| Questionnaire Items | Factor Loading | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| Factor 1: physical and mental state | |||
| 1. I perceive my self-healing as good | 0.78 | ||
| 2. I have a good health status | 0.78 | ||
| 8. I feel a positive vitality everyday | 0.69 | ||
| 5. I have a good management of my health status | 0.60 | ||
| 7. I am in a pleasant mood most of the times | 0.59 | ||
| Factor 2: socioeconomic and environmental status | |||
| 11. My economic status is good | 0.75 | ||
| 12. My community living environment is good | 0.74 | ||
| 10. I have good social support | 0.73 | ||
| 9. My interpersonal relationship is good | 0.65 | ||
| 6. I can reach a peaceful mindset | 0.56 | ||
| Factor 3: independent lifestyle | |||
| 3. I have good daily living functions | 0.84 | ||
| 4. I have good lifestyle | 0.61 | ||
| Eigenvalue | 3.32 | 3.02 | 1.56 |
| % of variance | 27.62 | 25.17 | 13.03 |
| Cumulative % | 27.62 | 52.80 | 65.83 |
| Scale | Components | Cronbach’s α | Mean | Std. Deviation |
|---|---|---|---|---|
| SHAS | 0.91 | 38.10 | 4.45 | |
| Physical and Mental State | 0.85 | 15.62 | 2.07 | |
| Socioeconomic and Environmental State | 0.83 | 15.86 | 2.01 | |
| Independent Lifestyle | 0.74 | 6.62 | 0.94 |
| Components | Physical and Mental State | Socioeconomic and Environmental State | Independent Lifestyle |
|---|---|---|---|
| Physical and Mental State | - | ||
| Socioeconomic and Environmental State | 0.70 ** | - | |
| Independent Lifestyle | 0.66 ** | 0.57 ** | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, Y.-C.; Hsu, H.-I.; Tung, H.-H.; Pan, S.-J.; Lin, S.-W. Psychometric Properties of the Self-Healing Assessment Scale for Community-Dwelling Older Adults. Healthcare 2021, 9, 484. https://doi.org/10.3390/healthcare9040484
Wu Y-C, Hsu H-I, Tung H-H, Pan S-J, Lin S-W. Psychometric Properties of the Self-Healing Assessment Scale for Community-Dwelling Older Adults. Healthcare. 2021; 9(4):484. https://doi.org/10.3390/healthcare9040484
Chicago/Turabian StyleWu, Yi-Chen, Hua-I Hsu, Heng-Hsin Tung, Shi-Jun Pan, and Shu-Wei Lin. 2021. "Psychometric Properties of the Self-Healing Assessment Scale for Community-Dwelling Older Adults" Healthcare 9, no. 4: 484. https://doi.org/10.3390/healthcare9040484
APA StyleWu, Y.-C., Hsu, H.-I., Tung, H.-H., Pan, S.-J., & Lin, S.-W. (2021). Psychometric Properties of the Self-Healing Assessment Scale for Community-Dwelling Older Adults. Healthcare, 9(4), 484. https://doi.org/10.3390/healthcare9040484







