Submandibular Push Exercise Using Visual Feedback from a Pressure Sensor in Patients with Swallowing Difficulties: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
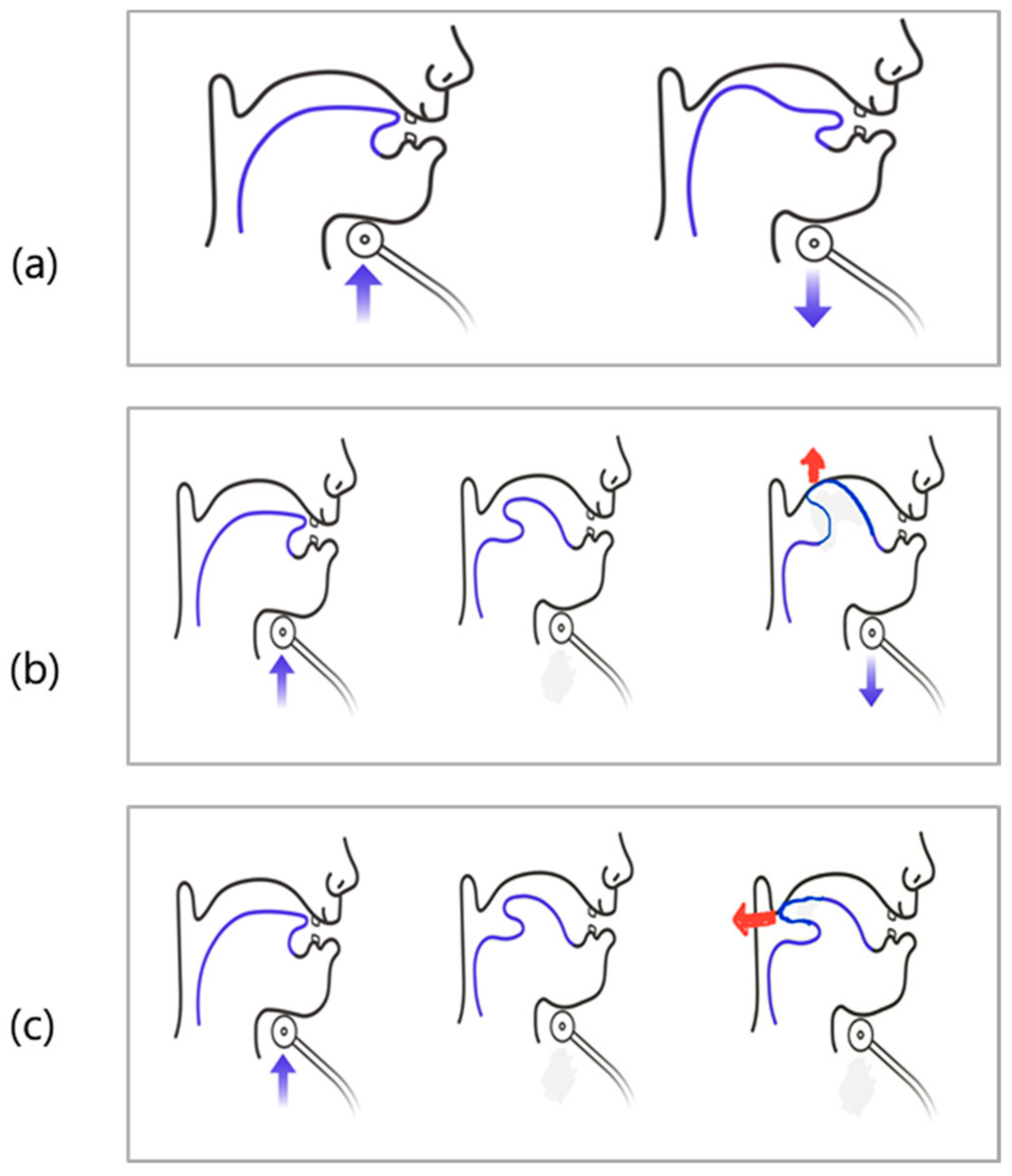
2.2. The Method of Submandibular Push Exercise
2.3. Submandibular Push Exercise Using Visual Feedback from a Pressure Sensor
2.4. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Comparison of Success and Non-Success Group
3.3. Comparison of Each Exercise Trial
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Park, D.; Oh, Y.; Ryu, J.S. Findings of Abnormal Videofluoroscopic Swallowing Study Identified by High-Resolution Manometry Parameters. Arch. Phys. Med. Rehabil. 2016, 97, 421–428. [Google Scholar] [CrossRef] [PubMed]
- Park, D.; Woo, S.B.; Lee, D.H.; Yu, K.J.; Cho, J.Y.; Kim, J.M.; Lee, Z. The Correlation Between Clinical Characteristics and Radionuclide Salivagram Findings in Patients with Brain Lesions: A Preliminary Study. Ann. Rehabil. Med. 2017, 41, 915–923. [Google Scholar] [CrossRef] [PubMed]
- Ertekin, C.; Aydogdu, I. Neurophysiology of swallowing. Clin. Neurophysiol. 2003, 114, 2226–2244. [Google Scholar] [CrossRef]
- Park, D.; Lee, H.H.; Lee, S.T.; Oh, Y.; Lee, J.C.; Nam, K.W.; Ryu, J.S. Normal contractile algorithm of swallowing related muscles revealed by needle EMG and its comparison to videofluoroscopic swallowing study and high resolution manometry studies: A preliminary study. J. Electromyogr. Kinesiol. 2017, 36, 81–89. [Google Scholar] [CrossRef]
- Humbert, I.; Poletto, C.; Sassone, K. L’effetto della stimolazione elettrica di superficie sul movimento hyolaryngeal in individui normali a riposo e durante la deglutizione. J. Appl. Physiol. 2006, 101, 1657–1663. [Google Scholar] [CrossRef]
- Shaw, G.Y.; Sechtem, P.R.; Searl, J.; Keller, K.; Rawi, T.A.; Dowdy, E. Transcutaneous neuromuscular electrical stimulation (VitalStim) curative therapy for severe dysphagia: Myth or reality? Ann. Otol. Rhinol. Laryngol. 2007, 116, 36–44. [Google Scholar] [CrossRef]
- Hwang, J.-M.; Cheong, Y.-S.; Kang, M.-G.; Chun, S.M.; Min, Y.-S.; Lee, Y.-S.; Jung, T.-D. Recommendation of Nasogastric Tube Removal in Acute Stroke Patients Based on Videofluoroscopic Swallow Study. Ann. Rehabil. Med. 2017, 41, 9–15. [Google Scholar] [CrossRef]
- Yu, K.J.; Park, D. Clinical characteristics of dysphagic stroke patients with salivary aspiration: A STROBE-compliant retrospective study. Medicine 2019, 98, e14977. [Google Scholar] [CrossRef]
- Paik, N.-J.; Kim, S.J.; Lee, H.J.; Jeon, J.Y.; Lim, J.-Y.; Han, T.R. Movement of the hyoid bone and the epiglottis during swallowing in patients with dysphagia from different etiologies. J. Electromyogr. Kinesiol. 2008, 18, 329–335. [Google Scholar] [CrossRef]
- Park, D.; Suh, J.H.; Kim, H.; Ryu, J.S. The Effect of Four-Channel Neuromuscular Electrical Stimulation on Swallowing Kinematics and Pressures: A Pilot Study. Am. J. Phys. Med. Rehabil. 2019, 98, 1051–1059. [Google Scholar] [CrossRef]
- Inokuchi, H.; González-Fernández, M.; Matsuo, K.; Brodsky, M.B.; Yoda, M.; Taniguchi, H.; Okazaki, H.; Hiraoka, T.; Palmer, J.B. Electromyography of Swallowing with Fine Wire Intramuscular Electrodes in Healthy Human: Amplitude Difference of Selected Hyoid Muscles. Dysphagia 2015, 31, 33–40. [Google Scholar] [CrossRef]
- Ferdjallah, M.; Wertsch, J.J.; Shaker, R. Spectral analysis of surface electromyography (EMG) of upper esophageal sphincter-opening muscles during head lift exercise. J. Rehabil. Res. Dev. 2000, 37, 335–340. [Google Scholar]
- Gao, J.; Zhang, H.-J. Effects of chin tuck against resistance exercise versus Shaker exercise on dysphagia and psychological state after cerebral infarction. Eur. J. Phys. Rehabil. Med. 2016, 53, 426–432. [Google Scholar]
- Sze, W.P.; Yoon, W.L.; Escoffier, N.; Liow, S.J.R. Evaluating the Training Effects of Two Swallowing Rehabilitation Therapies Using Surface Electromyography—Chin Tuck Against Resistance (CTAR) Exercise and the Shaker Exercise. Dysphagia 2016, 31, 195–205. [Google Scholar] [CrossRef]
- Yoon, W.L.; Khoo, J.K.P.; Liow, S.J.R. Chin Tuck Against Resistance (CTAR): New Method for Enhancing Suprahyoid Muscle Activity Using a Shaker-type Exercise. Dysphagia 2014, 29, 243–248. [Google Scholar] [CrossRef]
- Mepani, R.; Antonik, S.; Massey, B.; Kern, M.; Logemann, J.; Pauloski, B.; Rademaker, A.; Easterling, C.; Shaker, R. Augmentation of Deglutitive Thyrohyoid Muscle Shortening by the Shaker Exercise. Dysphagia 2009, 24, 26–31. [Google Scholar] [CrossRef]
- Park, S.; Cho, J.Y.; Lee, B.J.; Hwang, J.-M.; Lee, M.; Hwang, S.Y.; Kim, K.; Lee, K.H.; Park, D. Effect of the submandibular push exercise using visual feedback from pressure sensor: An electromyography study. Sci. Rep. 2020, 10, 1–10. [Google Scholar] [CrossRef]
- Jones, D.; Prowse, S. Globus pharyngeus: An update for general practice. Br. J. Gen. Pract. 2015, 65, 554–555. [Google Scholar] [CrossRef]
- Kang, J.-H.; Park, R.-Y.; Lee, S.-J.; Kim, J.-Y.; Yoon, S.-R.; Jung, K.-I. The Effect of Bedside Exercise Program on Stroke Patients with Dysphagia. Ann. Rehabil. Med. 2012, 36, 512–520. [Google Scholar] [CrossRef]
- Han, T.R.; Paik, N.-J.; Park, J.W. Quantifying swallowing function after stroke: A functional dysphagia scale based on videofluoroscopic studies. Arch. Phys. Med. Rehabil. 2001, 82, 677–682. [Google Scholar] [CrossRef]
- Rosenbek, J.C.; Robbins, J.A.; Roecker, E.B.; Coyle, J.L.; Wood, J.L. A penetration-aspiration scale. Dysphagia 1996, 11, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Berg, K.O.; Wood-Dauphinee, S.L.; Williams, J.I.; Maki, B. Measuring balance in the elderly: Validation of an instrument. Can. J. Public Health Rev. Can. Sante Publique 1992, 83, S7–S11. [Google Scholar]
- Shah, S.; Vanclay, F.; Cooper, B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J. Clin. Epidemiol. 1989, 42, 703–709. [Google Scholar] [CrossRef]
- Hayashi, T.; Fujiwara, Y.; Sakai, H.; Maeda, T.; Ueta, T.; Shiba, K. Risk factors for severe dysphagia in acute cervical spinal cord injury. Spinal Cord 2017, 55, 940–943. [Google Scholar] [CrossRef]
- Kumar, S.; Selim, M.H.; Caplan, L.R. Medical complications after stroke. Lancet Neurol. 2010, 9, 105–118. [Google Scholar] [CrossRef]
- Wyndaele, J.-J. The management of neurogenic lower urinary tract dysfunction after spinal cord injury. Nat. Rev. Urol. 2016, 13, 705–714. [Google Scholar] [CrossRef] [PubMed]
- Grossman, R.G.; Frankowski, R.F.; Burau, K.D.; Toups, E.G.; Crommett, J.W.; Johnson, M.M.; Fehlings, M.G.; Tator, C.H.; Shaffrey, C.I.; Harkema, S.J.; et al. Incidence and severity of acute complications after spinal cord injury. J. Neurosurg. Spine 2012, 17, 119–128. [Google Scholar] [CrossRef]




| Variables | Success | Fail | p-Value † |
|---|---|---|---|
| Number (n) | 8 | 4 | - |
| Gender (n) | - | ||
| Male | 7 | 4 | |
| Female | 1 | 0 | |
| Age (years) | 64.13 ± 14.47 | 57.00 ± 18.12 | 0.497 |
| Disease duration (days) | 39.00 ± 26.54 | 57.50 ± 33.56 | 0.443 |
| Initial behavior parameter | |||
| BBS | 15.50 ± 13.75 | 0.00 ± 0.00 | 0.014 * |
| MMSE | 21.75 ± 4.55 | 21.00 ± 2.70 | 0.347 |
| MBI | 31.13 ± 25.93 | 4.75 ± 5.25 | 0.124 |
| BDI | 26.57 ± 14.42 | 18.00 ± 24.04 | 0.558 |
| PAS | 4.17 ± 3.48 | 4.75 ± 3.30 | 0.655 |
| VDS | 33.00 ± 20.13 | 35.62 ± 19.33 | 0.915 |
| Variables | Mean ± SD | p-Value a | p-Value b | p-Value c | p-Value d | |
|---|---|---|---|---|---|---|
| Count (n) | D1 | 10.00 ± 2.20 | 0.861 | 0.332 | 0.461 | 0.546 |
| D2 | 10.12 ± 1.72 | - | 0.340 | 0.234 | 0.581 | |
| D3 | 9.62 ± 1.768 | - | - | 0.023 * | 0.167 | |
| D4 | 10.63 ± 1.506 | - | - | - | 0.832 | |
| D5 | 10.50 ± 3.071 | - | - | - | - | |
| Fmax (g) | D1 | 87.29 ± 31.16 | 0.028 * | 0.012 * | 0.017 * | 0.012 * |
| D2 | 106.01 ± 29.27 | - | 0.012 * | 0.012 * | 0.012 * | |
| D3 | 137.32 ± 31.53 | - | - | 0.889 | 0.050 | |
| D4 | 143.78 ± 39.13 | - | - | - | 0.123 | |
| D5 | 167.77 ± 37.39 | - | - | - | - | |
| Area (g·sec) | D1 | 1033.19 ± 609.56 | 0.025 * | 0.025 * | 0.025 * | 0.012 * |
| D2 | 1530.04 ± 573.82 | - | 0.123 | 0.093 * | 0.012 * | |
| D3 | 1772.32 ± 762.61 | - | - | 0.674 | 0.036 * | |
| D4 | 1810.33 ± 791.13 | - | - | - | 0.050 | |
| D5 | 2212.13 ± 548.62 | - | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, J.-M.; Jung, H.; Kim, C.-H.; Lee, Y.-S.; Lee, M.; Hwang, S.Y.; Kim, A.-R.; Park, D. Submandibular Push Exercise Using Visual Feedback from a Pressure Sensor in Patients with Swallowing Difficulties: A Pilot Study. Healthcare 2021, 9, 407. https://doi.org/10.3390/healthcare9040407
Hwang J-M, Jung H, Kim C-H, Lee Y-S, Lee M, Hwang SY, Kim A-R, Park D. Submandibular Push Exercise Using Visual Feedback from a Pressure Sensor in Patients with Swallowing Difficulties: A Pilot Study. Healthcare. 2021; 9(4):407. https://doi.org/10.3390/healthcare9040407
Chicago/Turabian StyleHwang, Jong-Moon, Hyunwoo Jung, Chul-Hyun Kim, Yang-Soo Lee, Myunghwan Lee, Soo Yeon Hwang, Ae-Ryoung Kim, and Donghwi Park. 2021. "Submandibular Push Exercise Using Visual Feedback from a Pressure Sensor in Patients with Swallowing Difficulties: A Pilot Study" Healthcare 9, no. 4: 407. https://doi.org/10.3390/healthcare9040407
APA StyleHwang, J.-M., Jung, H., Kim, C.-H., Lee, Y.-S., Lee, M., Hwang, S. Y., Kim, A.-R., & Park, D. (2021). Submandibular Push Exercise Using Visual Feedback from a Pressure Sensor in Patients with Swallowing Difficulties: A Pilot Study. Healthcare, 9(4), 407. https://doi.org/10.3390/healthcare9040407







