A Multi-Country Analysis of Prevalence of Anxiety-Induced Sleep Disturbance and Its Associated Factors among In-School Adolescents in Sub-Saharan Africa Using the Global School-Based Health Survey
Abstract
1. Background
2. Materials and Methods
2.1. Study Design and Source of Data
2.2. Sampling Method
2.3. Study Variables
2.3.1. Outcome Variable
2.3.2. Explanatory Variables
2.4. Statistical Analyses
2.5. Ethical Consideration
3. Results
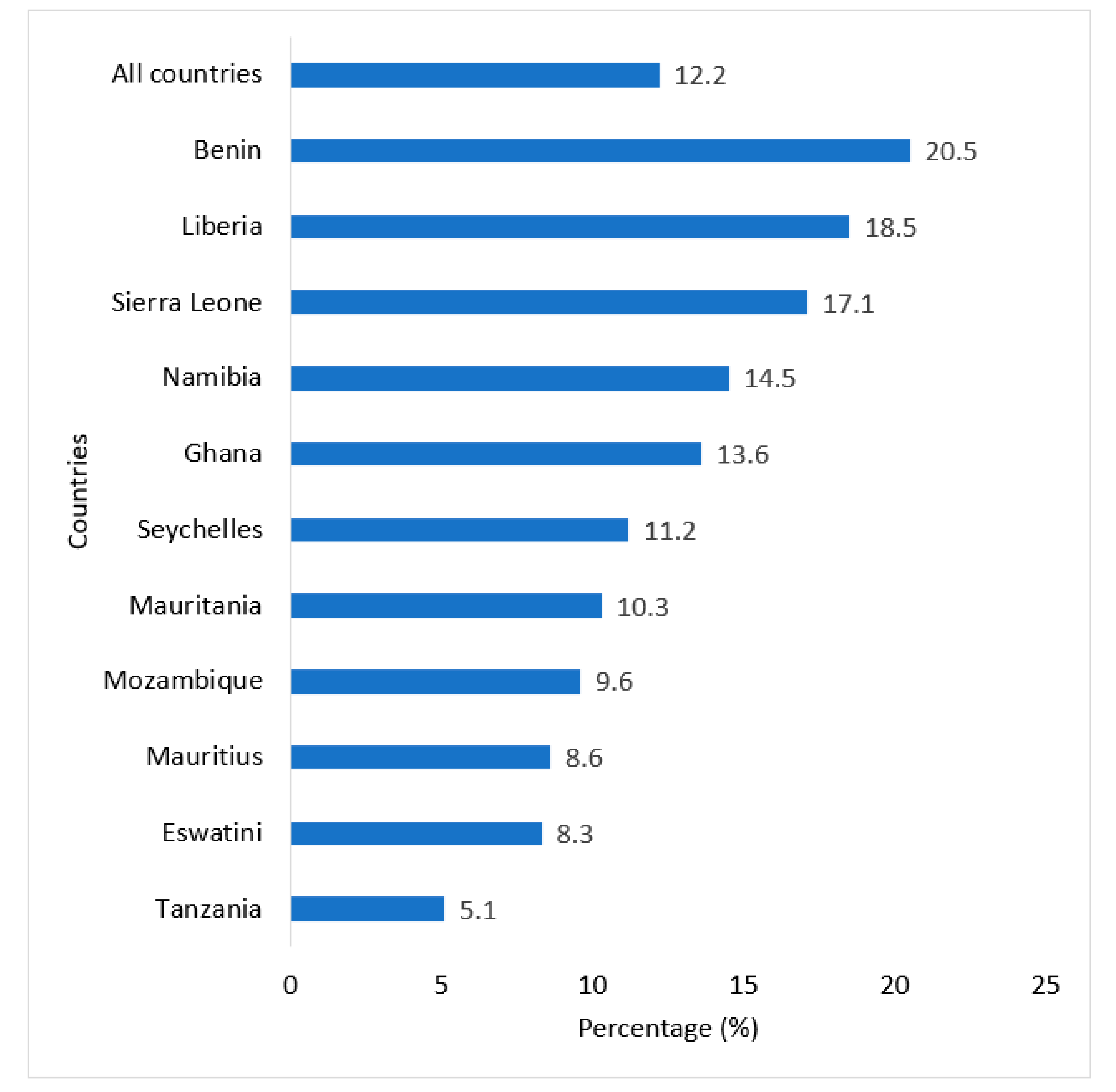
3.1. Prevalence of Anxiety-Induced Sleep Disturbance among In-School Adolescents in SSA
3.2. Prevalence of Anxiety-Induced Sleep Disturbance across the Background Characteristics of the Adolescents in SSA
3.3. Predictors of Anxiety-Induced Sleep Disturbance among the In-School Adolescents in SSA
4. Discussion
Limitations and Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Essau, C.A.; Lewinsohn, P.M.; Olaya, B.; Seeley, J.R. Anxiety disorders in adolescents and psychosocial outcomes at age 30. J. Affect. Disord. 2014, 163, 125–132. [Google Scholar] [CrossRef]
- Joyce-Beaulieu, D.; Sulkowski, M.L. The diagnostic and statistical manual of mental disorders: (DSM-5) model of impairment. In Assessing Impairment; Springer: Boston, MA, USA, 2016; pp. 167–189. [Google Scholar]
- Parekh, R. What Are Anxiety Disorders? American Psychiatric Association. 2019. Available online: https://www.psychiatry.org/patients-families/anxiety-disorders/what-are-anxiety-disorders (accessed on 5 November 2020).
- Seidu, A.A. Loneliness among in-school adolescents in Ghana: Evidence from the 2012 Global School-based Student Health Survey. J. Child Adolesc. Ment. Health 2020, 32, 1–10. [Google Scholar] [CrossRef]
- Jansson-Fröjmark, M.; Lindblom, K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J. Psychosom. Res. 2008, 64, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Alvaro, P.K.; Roberts, R.M.; Harris, J.K. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep 2013, 36, 1059–1068. [Google Scholar] [CrossRef]
- Peltz, J.S.; Rogge, R.D.; Pugach, C.P.; Strang, K. Bidirectional associations between sleep and anxiety symptoms in emerging adults in a residential college setting. Emerg. Adulthood 2017, 5, 204–215. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Adolescent Mental Health. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health.2020 (accessed on 28 November 2020).
- Kessler, R.C.; Angermeyer, M.; Anthony, J.C.; De Graaf, R.O.N.; Demyttenaere, K.; Gasquet, I.; Kawakami, N. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry 2007, 6, 168. [Google Scholar] [PubMed]
- Murphy, W.; de Menil, V.; Betancourt, T.; Collignon, R.; Aikins, A.D.G.; Dawes, A.; Reich, M.R.; Musisi, S.; Kafaar, Z.; Raja, S.; et al. The Culture of Mental Illness and Psychiatric Practice in Africa; Indiana University Press: Bloomington, IN, USA, 2015. [Google Scholar]
- Sweetland, A.C.; Belkin, G.S.; Verdeli, H. Measuring depression and anxiety in Sub-Saharan Africa. Depress. Anxiety 2014, 31, 223–232. [Google Scholar] [CrossRef]
- American Psychiatric Association. American Psychiatric Association American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (4th edition (DSM-IV)); American Psychiatric Association: Washington, DC, USA, 1994. [Google Scholar]
- Choueiry, N.; Salamoun, T.; Jabbour, H.; El Osta, N.; Hajj, A.; Khabbaz, L.R. Insomnia and relationship with anxiety in university students: A cross-sectional designed study. PLoS ONE 2016, 11, e0149643. [Google Scholar]
- Mazzone, L.; Ducci, F.; Scoto, M.C.; Passaniti, E.; D’Arrigo, V.G.; Vitiello, B. The role of anxiety symptoms in school performance in a community sample of children and adolescents. BMC Public Health 2007, 7, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.M.A.; Khan, M.N. Effects of psychosocial and socio-environmental factors on anxiety disorder among adolescents in Bangladesh. Brain Behav. 2020, 10, e01899. [Google Scholar] [CrossRef] [PubMed]
- Abbo, C.; Kinyanda, E.; Kizza, R.B.; Levin, J.; Ndyanabangi, S.; Stein, D.J. Prevalence, comorbidity and predictors of anxiety disorders in children and adolescents in rural north-eastern Uganda. Child Adolesc. Psychiatry Ment. Health 2013, 7, 21. [Google Scholar] [CrossRef] [PubMed]
- Adewuya, A.O.; Ola, B.A.; Adewumi, T.A. The 12-month prevalence of DSM-IV anxiety disorders among Nigerian secondary school adolescents aged 13–18 years. J. Adolesc. 2007, 30, 1071–1076. [Google Scholar] [CrossRef]
- Stickley, A.; Koyanagi, A.; Koposov, R.; Blatný, M.; Hrdlička, M.; Schwab-Stone, M.; Ruchkin, V. Loneliness and its association with psychological and somatic health problems among Czech, Russian and US adolescents. BMC Psychiatry 2016, 16, 128. [Google Scholar] [CrossRef] [PubMed]
- Acquah, E.O.; Topalli, P.Z.; Wilson, M.L.; Junttila, N.; Niemi, P.M. Adolescent loneliness and social anxiety as predictors of bullying victimisation. Int. J. Adolesc. Youth 2016, 21, 320–331. [Google Scholar] [CrossRef]
- Lee, A.; Hankin, B.L. Insecure attachment, dysfunctional attitudes, and low self-esteem predicting prospective symptoms of depression and anxiety during adolescence. J. Clin. Child Adolesc. Psychol. 2009, 38, 219–231. [Google Scholar] [CrossRef]
- Swearer, S.M.; Hymel, S. Understanding the psychology of bullying: Moving toward a social-ecological diathesis–stress model. Am. Psychol. 2015, 70, 344. [Google Scholar] [CrossRef]
- Ahinkorah, B.O.; Aboagye, R.G.; Arthur-Holmes, F.; Seidu, A.A.; Frimpong, J.B.; Budu, E.; Amoako, B.M.; Hagan, J.E. Predictors of Anxiety-Induced Sleep Disturbance among in-School Adolescents in Ghana: Evidence from the 2012 Global School-Based Health Survey. Behav. Sci. 2021, 11, 20. [Google Scholar] [CrossRef]
- Dashiff, C.; DiMicco, W.; Myers, B.; Sheppard, K. Poverty and adolescent mental health. J. Child Adolesc. Psychiatr. Nurs. 2009, 22, 23–32. [Google Scholar] [CrossRef]
- Osborn, T.L.; Campbell, S.; Ndetei, D.; Weisz, J. Network Analysis Reveals Central Symptoms of Adolescent Depression and Anxiety in Sub-Saharan Africa. arXiv 2020. [Google Scholar] [CrossRef]
- Caraveo-Anduaga, J.J.; Rodríguez, A.S.; Pérez, J.E. Anxiety syndromes and their correlates in children and adolescents: A two-year-follow-up study at primary health care in Mexico City. In New Insights Anxiety Disorders; Durbano, F., Ed.; INTECH Open Access Publisher: London, UK, 2013; pp. 233–258. [Google Scholar]
- Ndetei, D.M.; Mutiso, V.; Maraj, A.; Anderson, K.K.; Musyimi, C.; McKenzie, K. Stigmatizing attitudes toward mental illness among primary school children in Kenya. Soc. Psychiatry Psychiatr. Epidemiol. 2016, 51, 73–80. [Google Scholar] [CrossRef]
- Remes, O.; Brayne, C.; Van Der Linde, R.; Lafortune, L. A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain Behav. 2016, 6, e00497. [Google Scholar] [CrossRef]
- Colman, I.; Ploubidis, G.B.; Wadsworth, M.E.; Jones, P.B.; Croudace, T.J. A longitudinal typology of symptoms of depression and anxiety over the life course. Biol. Psychiatry 2007, 62, 1265–1271. [Google Scholar] [CrossRef]
- van Oort, F.V.A.; Greaves-Lord, K.; Ormel, J.; Verhulst, F.; Huizink, A. Risk indicators of anxiety throughout adolescence: The TRAILS study. Depress. Anxiety 2011, 28, 485–494. [Google Scholar] [CrossRef]
- McLean, C.P.; Asnaani, A.; Litz, B.T.; Hofmann, S.G. Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. J. Psychiatr. Res. 2011, 45, 1027–1035. [Google Scholar] [CrossRef]
- Grills-Taquechel, A.E.; Norton, P.; Ollendick, T.H. A longitudinal examination of factors predicting anxiety during the transition to middle school. Anxiety Stress Coping 2010, 23, 493–513. [Google Scholar] [CrossRef]
- Baxter, A.J.; Scott, K.M.; Vos, T.; Whiteford, H.A. Global prevalence of anxiety disorders: A systematic review and meta-regression. Psychol. Med. 2013, 43, 897. [Google Scholar] [CrossRef]
- Somers, J.M.; Goldner, E.M.; Waraich, P.; Hsu, L. Prevalence and incidence studies of anxiety disorders: A systematic review of the literature. Can. J. Psychiatry 2006, 51, 100–113. [Google Scholar] [CrossRef] [PubMed]
- Steel, Z.; Marnane, C.; Iranpour, C.; Chey, T.; Jackson, J.W.; Patel, V.; Silove, D. The global prevalence of common mental disorders: A systematic review and meta-analysis 1980–2013. Int. J. Epidemiol. 2014, 43, 476–493. [Google Scholar] [CrossRef] [PubMed]
- Yates, J.A.; Clare, L.; Woods, R.T. Mild cognitive impairment and mood: A systematic review. Rev. Clin. Gerontol. 2013, 23, 317. [Google Scholar] [CrossRef]
- Biaggi, A.; Conroy, S.; Pawlby, S.; Pariante, C.M. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J. Affect. Disord. 2016, 191, 62–77. [Google Scholar] [CrossRef]
- van Heyningen, T.; Honikman, S.; Myer, L.; Onah, M.N.; Field, S.; Tomlinson, M. Prevalence and predictors of anxiety disorders amongst low-income pregnant women in urban South Africa: A cross-sectional study. Arch. Women’s Ment. Health 2017, 20, 765–775. [Google Scholar] [CrossRef] [PubMed]
- Grant, K.A.; McMahon, C.; Austin, M.P. Maternal anxiety during the transition to parenthood: A prospective study. J. Affect. Disord. 2008, 108, 101–111. [Google Scholar] [CrossRef]
- World Health Organization Health for the World’s Adolescents: A Second Chance in the Second Decade. 2014. Available online: http://apps.who.int/adolescent/second-decade/ (accessed on 10 September 2020).
- Baxter, A.J.; Vos, T.; Scott, K.M.; Ferrari, A.J.; Whiteford, H.A. The global burden of anxiety disorders in 2010. Psychol. Med. 2014, 44, 2363. [Google Scholar] [CrossRef]
- Haller, H.; Cramer, H.; Lauche, R.; Gass, F.; Dobos, G.J. The prevalence and burden of subthreshold generalized anxiety disorder: A systematic review. BMC Psychiatry 2014, 14, 128. [Google Scholar] [CrossRef]
- Hawton, K.; Saunders, K.; Topiwala, A.; Haw, C. Psychiatric disorders in patients presenting to hospital following self-harm: A systematic review. J. Affect. Disord. 2013, 151, 821–830. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, A.; Ayers, S.; Smith, H. Pre-and postnatal psychological wellbeing in Africa: A systematic review. J. Affect. Disord. 2010, 123, 17–29. [Google Scholar] [CrossRef] [PubMed]
- Reijntjes, A.; Kamphuis, J.H.; Prinzie, P.; Boelen, P.A.; Van der Schoot, M.; Telch, M.J. Prospective linkages between peer victimization and externalizing problems in children: A meta-analysis. Aggress. Behav. 2011, 37, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Stadler, C.; Feifel, J.; Rohrmann, S.; Vermeiren, R.; Poustka, F. Peer-victimization and mental health problems in adolescents: Are parental and school support protective? Child Psychiatry Hum. Dev. 2010, 41, 371–386. [Google Scholar] [CrossRef]
- Boulton, M.J. Associations between adults’ recalled childhood bullying victimization, current social anxiety, coping, and self-blame: Evidence for moderation and indirect effects. Anxiety Stress Coping 2013, 26, 270–292. [Google Scholar] [CrossRef]
- Coelho, V.A.; Romão, A.M. The relation between social anxiety, social withdrawal and (cyber) bullying roles: A multilevel analysis. Comput. Hum. Behav. 2018, 86, 218–226. [Google Scholar] [CrossRef]
- Adams, R.E.; Fredstrom, B.K.; Duncan, A.W.; Holleb, L.J.; Bishop, S.L. Using self-and parent-reports to test the association between peer victimization and internalizing symptoms in verbally fluent adolescents with ASD. J. Autism Dev. Disord. 2014, 44, 861–872. [Google Scholar] [CrossRef] [PubMed]
- Tsaousis, I. The relationship of self-esteem to bullying perpetration and peer victimization among schoolchildren and adolescents: A meta-analytic review. Aggress. Violent Behav. 2016, 31, 186–199. [Google Scholar] [CrossRef]
- Hiller, T.S.; Steffens, M.C.; Ritter, V.; Stangier, U. On the context dependency of implicit selfesteem in social anxiety disorder. J. Behav. Ther. Exp. Psychiatry 2017, 57, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Finning, K.; Ukoumunne, O.C.; Ford, T.; Danielsson-Waters, E.; Shaw, L.; De Jager, I.R.; Moore, D.A. The association between child and adolescent depression and poor attendance at school: A systematic review and meta-analysis. J. Affect. Disord. 2019, 245, 928–938. [Google Scholar] [CrossRef]
- Egger, H.L.; Costello, J.E.; Angold, A. School refusal and psychiatric disorders: A community study. J. Am. Acad. Child Adolesc. Psychiatry 2003, 42, 797–807. [Google Scholar] [CrossRef]
- Asante, K.O.; Kugbey, N.; Osafo, J.; Quarshie, E.N.B.; Sarfo, J.O. The prevalence and correlates of suicidal behaviors (ideation, plan and attempt) among adolescents in senior high schools in Ghana. SSM-Popul. Health 2017, 3, 427–434. [Google Scholar] [CrossRef]
- Conway, C.C.; Latzman, R.D.; Krueger, R.F. A meta-structural model of common clinical disorder and personality disorder symptoms. J. Personal. Disord. 2020, 34, 88–106. [Google Scholar] [CrossRef]
- O’Neil Rodriguez, K.A.; Kendall, P.C. Suicidal ideation in anxiety-disordered youth: Identifying predictors of risk. J. Clin. Child Adolesc. Psychol. 2014, 43, 51–62. [Google Scholar] [CrossRef]
- O’Neil, K.A.; Puleo, C.M.; Benjamin, C.L.; Podell, J.L.; Kendall, P.C. Suicidal ideation in anxiety-disordered youth. Suicide Life-Threat. Behav. 2012, 42, 305–317. [Google Scholar] [CrossRef]
- Seidu, A.A.; Amu, H.; Dadzie, L.K.; Amoah, A.; Ahinkorah, B.O.; Ameyaw, E.K.; Kissah-Korsah, K. Suicidal behaviors among in-school adolescents in Mozambique: Cross-sectional evidence of the prevalence and predictors using the Global School-Based Health Survey data. PLoS ONE 2020, 15, e0236448. [Google Scholar] [CrossRef]
- Glodosky, N.C.; Cuttler, C. Motives Matter: Cannabis use motives moderate the associations between stress and negative affect. Addict. Behav. 2020, 102, 106188. [Google Scholar] [CrossRef]
- Cuttler, C.; Spradlin, A.; McLaughlin, R.J. A naturalistic examination of the perceived effects of cannabis on negative affect. J. Affect. Disord. 2018, 235, 198–205. [Google Scholar] [CrossRef]
- Buckner, J.D.; Bonn-Miller, M.O.; Zvolensky, M.J.; Schmidt, N.B. Marijuana use motives and social anxiety among marijuana-using young adults. Addict. Behav. 2007, 32, 2238–2252. [Google Scholar] [CrossRef]
- Bittner, A.; Egger, H.L.; Erkanli, A.; Jane Costello, E.; Foley, D.L.; Angold, A. What do childhood anxiety disorders predict? J. Child Psychol. Psychiatry 2007, 48, 1174–1183. [Google Scholar] [CrossRef] [PubMed]
| Country | Year of Publication | Population | Sample a | Percentage |
|---|---|---|---|---|
| Benin | 2016 | 2536 | 2219 | 8.7 |
| Eswatini | 2013 | 3680 | 2944 | 11.6 |
| Ghana | 2012 | 3632 | 2821 | 11.1 |
| Liberia | 2017 | 2744 | 1499 | 5.9 |
| Mauritania | 2010 | 2063 | 1531 | 6.0 |
| Mauritius | 2017 | 3012 | 2491 | 9.8 |
| Mozambique | 2015 | 1918 | 1319 | 5.2 |
| Namibia | 2013 | 4531 | 3525 | 13.8 |
| Seychelles | 2015 | 2540 | 1891 | 7.4 |
| Sierra Leone | 2017 | 2798 | 2118 | 8.3 |
| Tanzania | 2014 | 3793 | 3096 | 12.2 |
| All countries | 33,247 | 25,454 | 100.0 |
| n = 25,454 | Anxiety-Induced Sleep Disturbance | ||||
|---|---|---|---|---|---|
| Variables | Frequency | Percentage | No (%) | Yes (%) | p-Value |
| Age | <0.001 | ||||
| 14 years or younger | 8222 | 32.3 | 90.5 | 9.5 | |
| 15 years or older | 17,232 | 67.7 | 86.5 | 13.5 | |
| Sex | 0.001 | ||||
| Female | 13,153 | 51.7 | 87.2 | 12.8 | |
| Male | 12,301 | 48.3 | 88.5 | 11.5 | |
| Felt lonely | <0.001 | ||||
| No | 22,273 | 87.5 | 90.8 | 9.2 | |
| Yes | 3181 | 12.5 | 66.7 | 33.3 | |
| Bullied | <0.001 | ||||
| No | 15,579 | 61.2 | 91.2 | 8.8 | |
| Yes | 9875 | 38.8 | 82.5 | 17.5 | |
| Suicidal ideation | <0.001 | ||||
| No | 21,323 | 83.8 | 90.0 | 10.0 | |
| Yes | 4131 | 16.2 | 76.7 | 23.3 | |
| Suicidal plan | <0.001 | ||||
| No | 20,904 | 82.1 | 89.8 | 10.2 | |
| Yes | 4550 | 17.9 | 78.6 | 21.4 | |
| Suicidal attempt | <0.001 | ||||
| No | 21,261 | 83.5 | 89.8 | 10.2 | |
| Yes | 4193 | 16.5 | 77.8 | 22.3 | |
| Current marijuana use | <0.001 | ||||
| No | 24,508 | 96.3 | 88.2 | 11.8 | |
| Yes | 946 | 3.7 | 78.0 | 22.0 | |
| Truancy | <0.001 | ||||
| No | 18,694 | 73.4 | 89.4 | 10.6 | |
| Yes | 6760 | 26.6 | 83.5 | 16.5 | |
| Close friends | <0.001 | ||||
| No | 2581 | 10.1 | 85.2 | 14.8 | |
| Yes | 22,873 | 89.9 | 88.1 | 11.9 | |
| Peer support | 0.533 | ||||
| No | 17,310 | 68.0 | 87.9 | 12.1 | |
| Yes | 8144 | 32.0 | 87.6 | 12.4 | |
| Parental or guardian supervision | 0.234 | ||||
| No | 14,519 | 57.0 | 87.6 | 12.4 | |
| Yes | 10,935 | 43.0 | 88.1 | 11.9 | |
| Parental or guardian connectedness | 0.042 | ||||
| No | 15,215 | 59.8 | 87.5 | 12.5 | |
| Yes | 10,239 | 40.2 | 88.3 | 11.7 | |
| Parental or guardian bonding | 0.058 | ||||
| No | 15,690 | 61.6 | 87.5 | 12.5 | |
| Yes | 9764 | 38.4 | 88.3 | 11.7 | |
| Variable | Model I | Model II |
|---|---|---|
| aOR [95% CI] | aOR [95% CI] | |
| Age | ||
| 14 years or younger | Ref. | Ref. |
| 15 years or older | 1.50 *** [1.37, 1.63] | 1.26 *** [1.15, 1.39] |
| Sex | ||
| Female | Ref. | Ref. |
| Male | 0.86 *** [0.80, 0.93] | 0.88 ** [0.81, 0.95] |
| Bullied | ||
| No | Ref. | |
| Yes | 1.54 *** [1.42, 1.67] | |
| Felt lonely | ||
| No | Ref. | |
| Yes | 3.85 *** [3.52, 4.22] | |
| Suicidal ideation | ||
| No | Ref. | |
| Yes | 1.70 *** [1.52, 1.90] | |
| Suicidal plan | ||
| No | Ref. | |
| Yes | 1.26 *** [1.13, 1.41] | |
| Suicidal attempt | ||
| No | Ref. | |
| Yes | 1.21 ** [1.08, 1.35] | |
| Current marijuana use | ||
| No | Ref. | |
| Yes | 1.27 * [1.06, 1.52] | |
| Truancy | ||
| No | Ref. | |
| Yes | 1.33 *** [1.22, 1.46] | |
| Close friends | ||
| No | Ref. | |
| Yes | 0.95 [0.84, 1.07] | |
| Parental or guardian connectedness | ||
| No | Ref. | |
| Yes | 1.05 [0.97, 1.15] | |
| N | 25,454 | 25,454 |
| Pseudo R 2 | 0.0053 | 0.1149 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahinkorah, B.O.; Aboagye, R.G.; Arthur-Holmes, F.; Hagan, J.E., Jr.; Okyere, J.; Budu, E.; Dowou, R.K.; Adu, C.; Seidu, A.-A. A Multi-Country Analysis of Prevalence of Anxiety-Induced Sleep Disturbance and Its Associated Factors among In-School Adolescents in Sub-Saharan Africa Using the Global School-Based Health Survey. Healthcare 2021, 9, 234. https://doi.org/10.3390/healthcare9020234
Ahinkorah BO, Aboagye RG, Arthur-Holmes F, Hagan JE Jr., Okyere J, Budu E, Dowou RK, Adu C, Seidu A-A. A Multi-Country Analysis of Prevalence of Anxiety-Induced Sleep Disturbance and Its Associated Factors among In-School Adolescents in Sub-Saharan Africa Using the Global School-Based Health Survey. Healthcare. 2021; 9(2):234. https://doi.org/10.3390/healthcare9020234
Chicago/Turabian StyleAhinkorah, Bright Opoku, Richard Gyan Aboagye, Francis Arthur-Holmes, John Elvis Hagan, Jr., Joshua Okyere, Eugene Budu, Robert Kokou Dowou, Collins Adu, and Abdul-Aziz Seidu. 2021. "A Multi-Country Analysis of Prevalence of Anxiety-Induced Sleep Disturbance and Its Associated Factors among In-School Adolescents in Sub-Saharan Africa Using the Global School-Based Health Survey" Healthcare 9, no. 2: 234. https://doi.org/10.3390/healthcare9020234
APA StyleAhinkorah, B. O., Aboagye, R. G., Arthur-Holmes, F., Hagan, J. E., Jr., Okyere, J., Budu, E., Dowou, R. K., Adu, C., & Seidu, A.-A. (2021). A Multi-Country Analysis of Prevalence of Anxiety-Induced Sleep Disturbance and Its Associated Factors among In-School Adolescents in Sub-Saharan Africa Using the Global School-Based Health Survey. Healthcare, 9(2), 234. https://doi.org/10.3390/healthcare9020234







