Co-Design of an Evidenced Informed Service Model of Integrated Palliative Care for Persons Living with Severe Mental Illness: A Qualitative Exploratory Study
Abstract
:1. Background
2. Methods
2.1. Aim
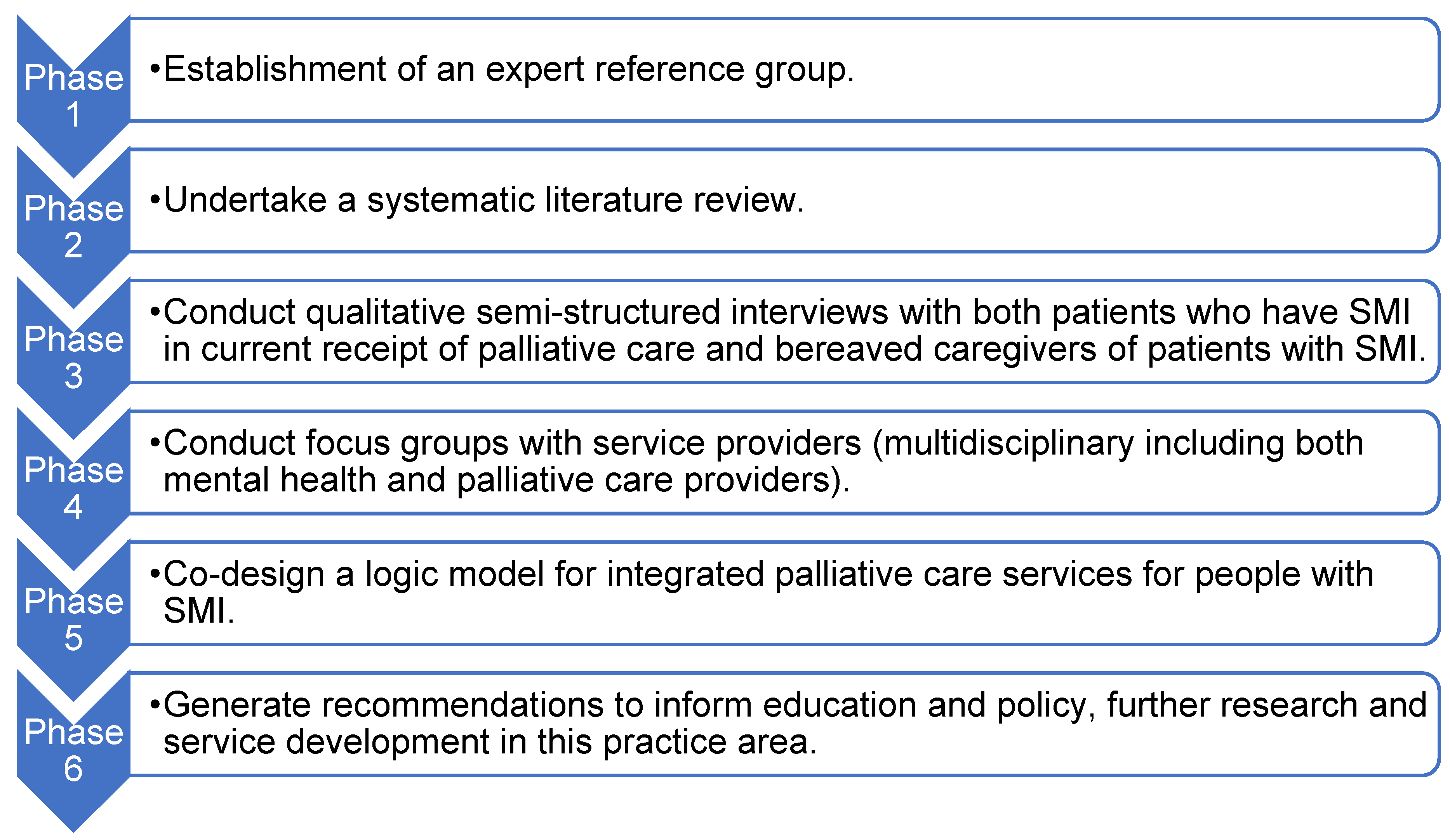
2.2. Study Design
2.3. Analysis (Phases 3–5)
2.4. Rigour
2.5. Ethical Considerations
3. Discussion
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organisation. Mental Disorders. Available online: http://www.who.int (accessed on 19 October 2021).
- Woods, A.; Willison, K.; Kington, C.; Gavin, A. Palliative care for people with severe persistent mental illness: A review of the literature. Can. J. Psychiatry 2008, 53, 725–736. [Google Scholar] [CrossRef] [Green Version]
- Knippenberg, I.; Zaghouli, N.; Engels, Y.; Vissers, K.; Groot, M. Severe mental illness and palliative care: Patient semistructured interviews. BMJ Support. Palliat. Care 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Chochinov, H.M.; Martens, P.J.; Prior, H.J.; Kredentser, M.S. Comparative health care use patterns of people with schizophrenia near the end of life: A population-based study in Manitoba, Canada. Schizophr. Res. 2012, 141, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Burton, M.C.; Warren, M.; Cha, S.S.; Stevens, M.; Blommer, M.; Kung, S.; Lapid, M.I. Identifying Patients in the Acute Psychiatric Hospital Who May Benefit From a Palliative Care Approach. Am. J. Hosp. Palliat. Med. 2014, 33, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.; Hepgul, N.; Higginson, I.J.; Gao, W. End-of-life care and place of death in adults with serious mental illness: A systematic review and narrative synthesis. Palliat. Med. 2020, 34, 49–68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McNamara, B.; Same, A.; Rosenwax, L.; Kelly, B. Palliative care for people with schizophrenia: A quality study of an underserviced group in need. BMC Palliat. Care 2018, 17, 53. [Google Scholar] [CrossRef]
- Trachsel, M.; Hodel, M.A.; Irwin, S.A.; Hoff, P.; Biller-Andorno, N.; Riese, F. Acceptability of palliative care approaches for patients with severe and persistent mental illness: A survey of psychiatrists in Switzerland. BMC Psychiatry 2019, 19, 111. [Google Scholar] [CrossRef] [Green Version]
- Brown, S.; Miranda, K.; Mitchell, C.; Inskip, H. Twenty-five year mortality of a community cohort with schizophrenia. Br. J. Psychiatry 2010, 196, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Kredenster, M.S.; Martens, P.J.; Chochinov, H.M.; Prior, H.J. Cause and rate of death in people with schizophrenia across the lifespan: A population based study in Manitoba. J. Clin. Psychiatry 2014, 75, 154–161. [Google Scholar] [CrossRef]
- Irwin, K.E.; Henderson, D.C.; Knight, H.; Pirl, W.F. Cancer care for individuals with schizophrenia. Cancer 2014, 120, 323–334. [Google Scholar] [CrossRef] [PubMed]
- Rocque, G.B.; Cleary, J.F. Palliative care reduces morbidity and mortality in cancer. Nat. Rev. Clin. Oncol. 2013, 10, 80–89. [Google Scholar] [CrossRef] [PubMed]
- Amano, K.; Morita, T.; Tatara, R.; Katayama, H.; Uno, T.; Takagi, I. Association between early palliative care referrals, inpatient hospice utilization, and aggressiveness of care at the end of life. J. Palliat. Med. 2015, 18, 270–273. [Google Scholar] [CrossRef] [PubMed]
- National Health Service. Addressing Inequalities in End of Life Care. Available online: http://england.nhs.uk (accessed on 19 July 2021).
- Department of Health. Service Framework for Mental Health and Wellbeing 2018–2021; DOH: Belfast, UK, 2018. [Google Scholar]
- Cai, X.; Cram, P.; Li, Y. Origination of medical advance directives among nursing home residents with and without serious mental illness. Psychiatr. Serv. 2011, 62, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Ewert, B.; Hodiamont, F.; van Wijngaarden, J.; Payne, S.; Groot, M.; Hasselaar, J.; Menten, J.; Radbruch, L. Building a taxonomy of integrated palliative care initiatives: Results from a focus group. BMJ Support. Palliat. Care 2016, 6, 14–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brazil, K. A Call for Integrated and Coordinated Palliative Care. J. Palliat. Med. 2018, 21, S27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shefer, G.; Henderson, C.; Howard, L.M.; Murray, J.; Thornicroft, G. Diagnostic overshadowing and other challenges involved in the diagnostic process of patients with mental illness who present in emergency departments with physical symptoms—A qualitative study. PLoS ONE 2014, 9, e111682. [Google Scholar] [CrossRef]
- Donald, E.E.; Stajduhar, K.I. A scoping review of palliative care for persons with severe persistent mental illness. Palliat. Support. Care 2019, 17, 479–487. [Google Scholar] [CrossRef]
- Sleeman, K.; de Brito, M.; Etkind, S.; Nkhoma, K.; Guo, P.; Higginson, I.J.; Gomes, B.; Harding, R. The escalating global burden of serious-health related suffering: Projections to 2060 by world regions, age groups, and health conditions. Lancet Glob. Health. 2019, 7, e883–e892. [Google Scholar] [CrossRef] [Green Version]
- Ruggeri, M.; Leese, M.; Thornicroft, G.; Bisoffi, G.; Tansella, M. Definition and prevalence of severe and persistent mental illness. Br. J. Psychiatry 2000, 177, 149–155. [Google Scholar] [CrossRef] [Green Version]
- Mulder, C.L.; van der Gaag, M.; Bruggeman, R.; Cahn, W.; Delespaul, P.A.E.; Dries, P.; Faber, G. Routine Outcome Monitoring for patients with severe mental illness: A consensus document. Tijdschr. Voor Psychiatr. 2010, 52, 169–179. [Google Scholar]
- Delespaul, P.H.; de consensusgroep, E.P.A. Consensus regarding the definition of persons with severe mental illness and the number of such persons in the Netherlands. Tijdschr. Voor Psychiatr. 2013, 55, 427–438. [Google Scholar]
- Creswell, J.W. Research Design: Qualitative, Quantitative and Mixed Methods Approaches; Sage: London, UK, 2013. [Google Scholar]
- Polit, D.F.; Beck, C.T. Nursing Research: Principles and Methods, 7th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2016. [Google Scholar]
- Capili, B. How Does Research Start? Am. J. Nurs. 2020, 120, 41–44. [Google Scholar] [CrossRef]
- Bettany-Saltikov, J.; McSherry, R. How to Do a Systematic Literature Review in Nursing: A Step by Step Guide; Open University Press: London, UK, 2016. [Google Scholar]
- Addington Hall, J.; Mc Pierson, C. After-death interviews with surrogates/bereaved family members: Some issues of validity. J. Pain Symptom Manag. 2001, 22, 784–790. [Google Scholar] [CrossRef]
- McVeigh, C.; Reid, J.; Larkin, P.; Porter, S.; Hudson, P. The provision of generalist and specialist palliative care for patients with non-malignant respiratory disease in the North and Republic of Ireland: A qualitative study. BMC Palliat. Care 2018, 17, 6. [Google Scholar] [CrossRef] [Green Version]
- Bakitas, M.; Ahles, T.A.; Skalla, K.; Brokaw, F.C.; Byock, I.; Hanscom, B.; Lyons, K.; Hegel, M.T. Proxy perspectives regarding end-of-life care for persons with cancer. Cancer 2008, 112, 1854–1861. [Google Scholar] [CrossRef] [Green Version]
- Donnelly, S.; Prizeman, G.; Coimín, D.Ó.; Koran, B.; Haynes, G. Voices that matter: End-of-life care on two acute hospitals from the perspective of bereaved relatives. BMC Palliat. Care 2018, 17, 117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trotter, R. Qualitative research sample design and sample size: Resolving and unresolved issues and inferential imperatives. Prev. Med. 2012, 55, 398–400. [Google Scholar] [CrossRef] [PubMed]
- Francis, J.J.; Johnston, M.; Robertson, C.; Glidewell, L.; Entwhistle, L.; Eccles, M.P.; Grimshaw, J.M. What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol. Health 2010, 25, 1229–1245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sandelowski, M. Theoretical Saturation. In The SAGE Encyclopedia of Qualitative Research Methods; Given, L.M., Ed.; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2008; Volume 2, pp. 875–876. [Google Scholar]
- Walker, S.; Read, S. Accessing vulnerable research populations: An experience with gatekeepers of ethical approval. Int. J. Palliat. Nurs. 2011, 17, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Green, J.; Thorogood, N. Qualitative Methods for Health Research, 2nd ed.; Sage: London, UK, 2009. [Google Scholar]
- Hudson, P.; Trauer, T.; Kelly, B.; O’Connor, M.; Thomas, K.; Summers, M.; Zordan, R.; White, V. Reducing the psychological distress of family carers of home based palliative care patients: Longer term effects from a randomised controlled trial. Psycho-Oncol. 2014, 24, 1987–1993. [Google Scholar]
- Jamshed, S. Qualitative research method-interviewing and observation. J. Basic Clin. Pharm. 2014, 5, 87–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DeJonckheere, M.; Vaughn, L.M. Semi structured interviewing in primary care research: A balance of relationship and rigour. Fam. Med. Community Health 2019, 7, e000057. [Google Scholar] [CrossRef] [Green Version]
- Price, B. Laddered questions and qualitative data research interviews. J. Adv. Nurs. 2002, 37, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Patton, M.Q. Qualitative Research and Evaluation Methods; SAGE: London, UK, 2002. [Google Scholar]
- Morse, J.M.; Field, P.A. Nursing research. In The Application of Qualitative Approaches, 2nd ed.; Chapman & Hall: London, UK, 1996. [Google Scholar]
- Robinson, J. Focus groups. In SAGE Research Methods Foundations; Atkinson, P., Delamont, S., Cernat, A., Sakshaug, J.W., Williams, R.A., Eds.; Thousand Oaks California 2019, 2019; Available online: http://methods.sagepub.com/foundations/focus-groups/doi.org/26421036821959 (accessed on 20 July 2021).
- Guest, G.; Namey, E.; McKenna, K. How many focus groups are enough? Building an evidence base for nonprobability sample sizes. Field Methods 2016, 29, 3–22. [Google Scholar] [CrossRef]
- Tausch, A.P.; Menold, N. Methodological Aspects of Focus Groups in Health Research: Results of Qualitative Interviews with Focus Group Moderators. Glob. Qual. Nurs. Res. 2016, 3, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woodyatt, C.R.; Finnegan, C.A.; Stephenson, R. In-person versus online focus group discussions: A comparative analysis of quality data. Qual. Health Res. 2016, 26, 741–749. [Google Scholar] [CrossRef] [PubMed]
- McConnell, T.; Porter, S. The experience of providing end of life care at a children’s hospice: A qualitative study. BMC Palliat. Care 2017, 16, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oliver, S.; Clarke-Jones, L.; Rees, R.; Milne, R.; Buchanan, P.; Gabbay, J.; Oakley, A.; Stein, K. Involving consumers in research and development agenda setting for the NHS: Developing an evidenced-based approach. Health Technol. Assess. 2004, 8, 1–148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Donetto, S.; Tsianakas, V.; Robert, G. Using Experienced-Based-Co-Design to Improve the Quality of Healthcare: Mapping Where We Are Now in Establishing Future Directions; Kings College London: London, UK, 2014. [Google Scholar]
- University of Wisconsin-Extension. Program Development and Evaluation: Logic Models. Available online: https://fyi.unexpected.edu/programdevelopment/logic-models/ (accessed on 10 July 2021).
- Glasgow, R.E.; McKay, G.; Piette, J.; Reynolds, K.D. The RE-AIM framework for evaluating interventions: What can it tell us about approaches to chronic illness management? Patient Educ. Couns. 2001, 44, 119–127. [Google Scholar] [CrossRef]
- Medical Research Council. Developing and Evaluating Complex Interventions. Available online: https:mrc.ukrainian.org/documents/pdf/complex-interventions-guidance (accessed on 10 July 2021).
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Roller, M.R.; Lavrakas, P.J. Applied Qualitative Research Design: A Total Quality Framework Approach; The Guildford Press: New York, NY, USA, 2015. [Google Scholar]
- Chen, C.; Draucker, C.B.; Carpenter, J.S. What women say about their dysmenorrhea: A qualitative thematic analysis. BMC Women’s Health 2018, 18, 47. [Google Scholar] [CrossRef] [PubMed]
- Houghton, C.; Murphy, K.; Meehan, B.; Thomas, J.; Brooker, D.; Casey, D. From screening to synthesis: Using nvivo to enhance transparency in qualitative evidence synthesis. J. Clin. Nurs. 2017, 26, 873–881. [Google Scholar] [CrossRef] [PubMed]
- Lincoln, Y.S.; Guba, E.G. Naturalistic Inquiry; Sage Publications Inc.: Newbury Park, CA, USA, 1985. [Google Scholar]
- Nobel, H.; Hale, R. Triangulation in research, with examples. Evid. -Based Nurs. 2019, 22, 67–69. [Google Scholar] [CrossRef] [PubMed]
- Korstjens, I.; Moser, A. Series: Practical guidance to qualitative research. Part 4: Trustworthiness and publishing. Eur. J. Gen. Pr. 2018, 24, 120–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dempsey, L.; Dowling, M.; Larkin, P.; Murphy, K. Sensitive interviewing in qualitative research. Res. Nurs. Health 2016, 39, 480–490. [Google Scholar] [CrossRef]
- Perkins, E.; Gambles, M.; Houten, R.; Harper, S.; Haycox, A.; O’Brien, T.; Richards, S.; Chen, H.; Nolan, K.; Ellershaw, J. The care of dying people in nursing homes and intensive care units: A qualitative mixed-methods study. Health Serv. Deliv. 2016, 4, 20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Living with Schizophrenia. Available online: https://livingwithschizophrenia.org (accessed on 19 July 2021).
| People with Severe Mental Illness. | |
| Inclusion Criteria | Exclusion Criteria |
| Diagnosis of severe mental illness (as per operational definition) | No diagnosis of severe mental illness |
| Currently receiving palliative care | Not receiving palliative care |
| Over 18 years of age | Under 18 years of age |
| Capacity to take part in the study—as determined by the clinical gatekeeper | Does not have capacity to take part—as determined by the clinical gatekeeper |
| Can understand and speak English | Not fluent in English |
| Caregivers | |
| Inclusion Criteria | Exclusion Criteria |
| Bereaved caregiver of a patient with severe mental illness who has died 6–18 months earlier | Bereaved carer of patient who had died and not had a severe mental illness |
| Over 18 years of age | Under 18 years of age |
| Can understand and speak English | Not fluent in English |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Healthcare professionals involved in the care of people who have a severe mental illness and or palliative care | Healthcare professionals not involved in either severe mental illness or palliative care delivery |
| Employed within the recruiting Health and Social Trusts | Have a non-permanent contract with the Health and Social Trust, e.g., agency staff |
| Have an appropriate professional qualification in their field of work | Not fluent in English |
| Can understand and speak English |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tinkler, M.; Reid, J.; Brazil, K. Co-Design of an Evidenced Informed Service Model of Integrated Palliative Care for Persons Living with Severe Mental Illness: A Qualitative Exploratory Study. Healthcare 2021, 9, 1710. https://doi.org/10.3390/healthcare9121710
Tinkler M, Reid J, Brazil K. Co-Design of an Evidenced Informed Service Model of Integrated Palliative Care for Persons Living with Severe Mental Illness: A Qualitative Exploratory Study. Healthcare. 2021; 9(12):1710. https://doi.org/10.3390/healthcare9121710
Chicago/Turabian StyleTinkler, Marianne, Joanne Reid, and Kevin Brazil. 2021. "Co-Design of an Evidenced Informed Service Model of Integrated Palliative Care for Persons Living with Severe Mental Illness: A Qualitative Exploratory Study" Healthcare 9, no. 12: 1710. https://doi.org/10.3390/healthcare9121710
APA StyleTinkler, M., Reid, J., & Brazil, K. (2021). Co-Design of an Evidenced Informed Service Model of Integrated Palliative Care for Persons Living with Severe Mental Illness: A Qualitative Exploratory Study. Healthcare, 9(12), 1710. https://doi.org/10.3390/healthcare9121710







