Analysis of the Effect of Wearing Extensible and Non-Extensible Lumbar Belts on Biomechanical Factors of the Sit-to-Stand Movement and Pain-Related Psychological Factors Affecting Office Workers with Low Back Pain
Abstract
1. Introduction
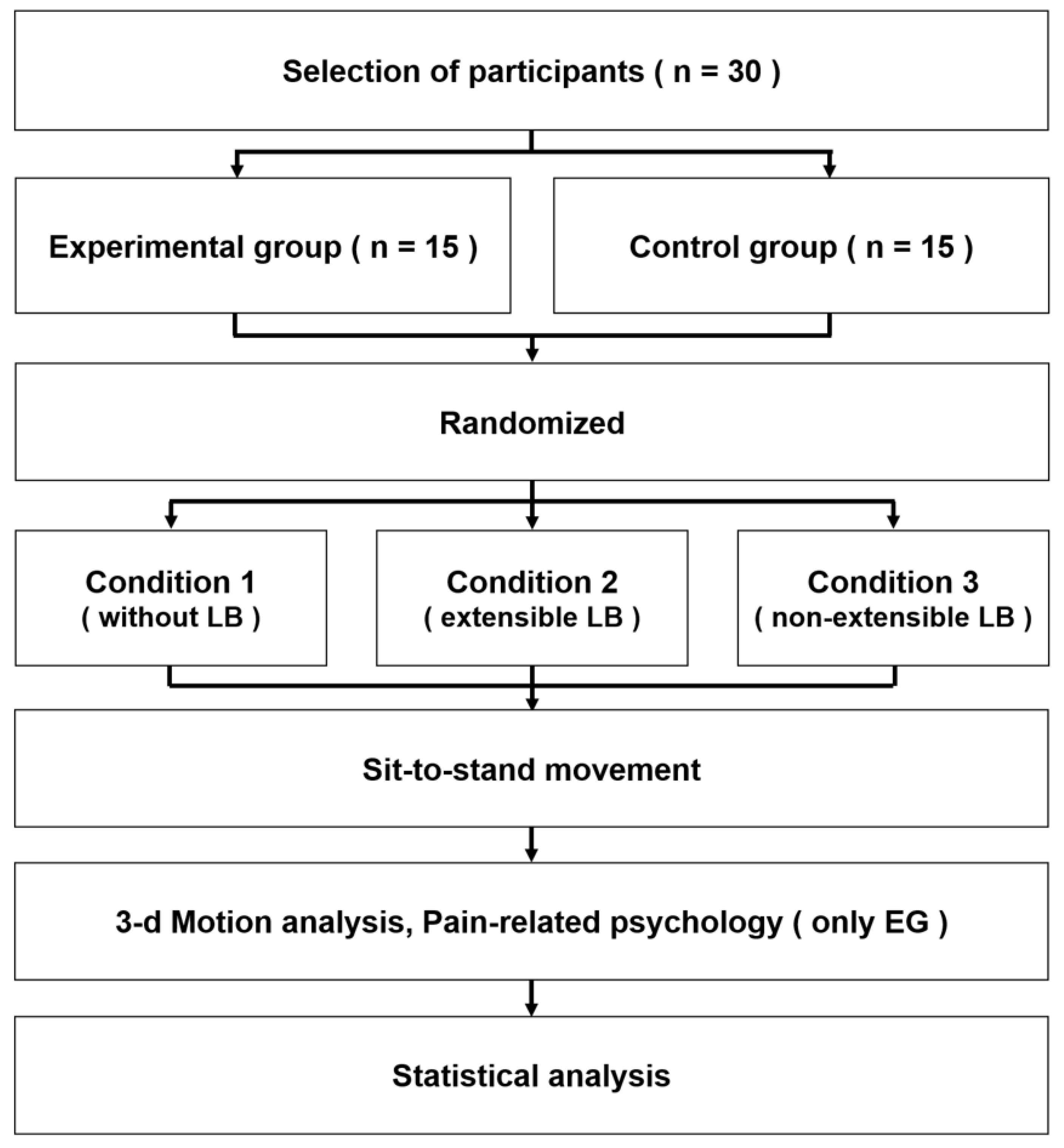
2. Materials and Methods
2.1. Participants
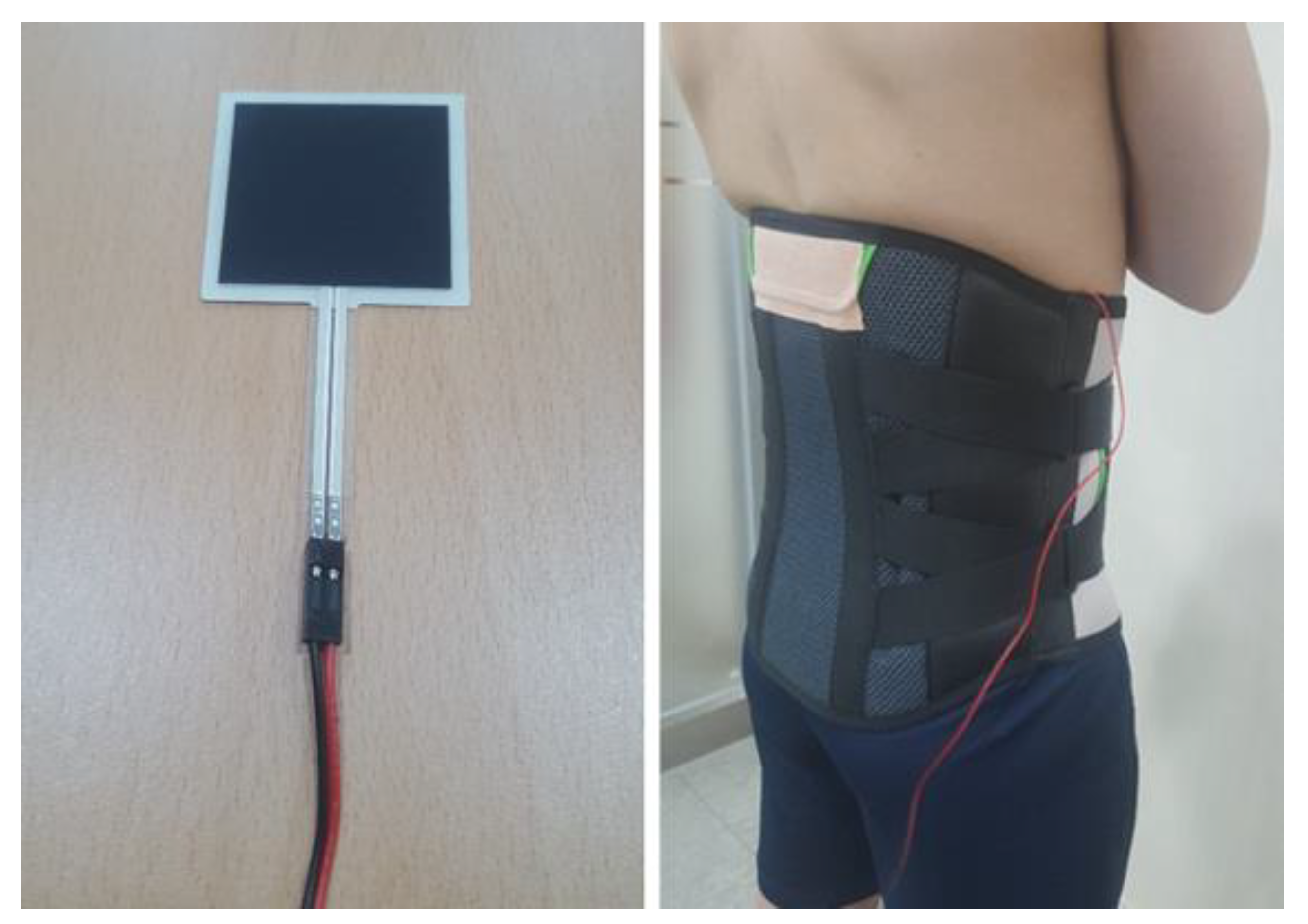
2.2. Lumbar Belts
2.3. Experimental Procedure
2.4. Measurement Methods
2.4.1. Measurement of Biomechanical Variables
2.4.2. Measurement of Pain-Related Psychological Variables
2.5. Data Processing
2.6. Statistical Analysis
3. Results
3.1. Analysis of General Characteristics of the Experimental and Control Groups
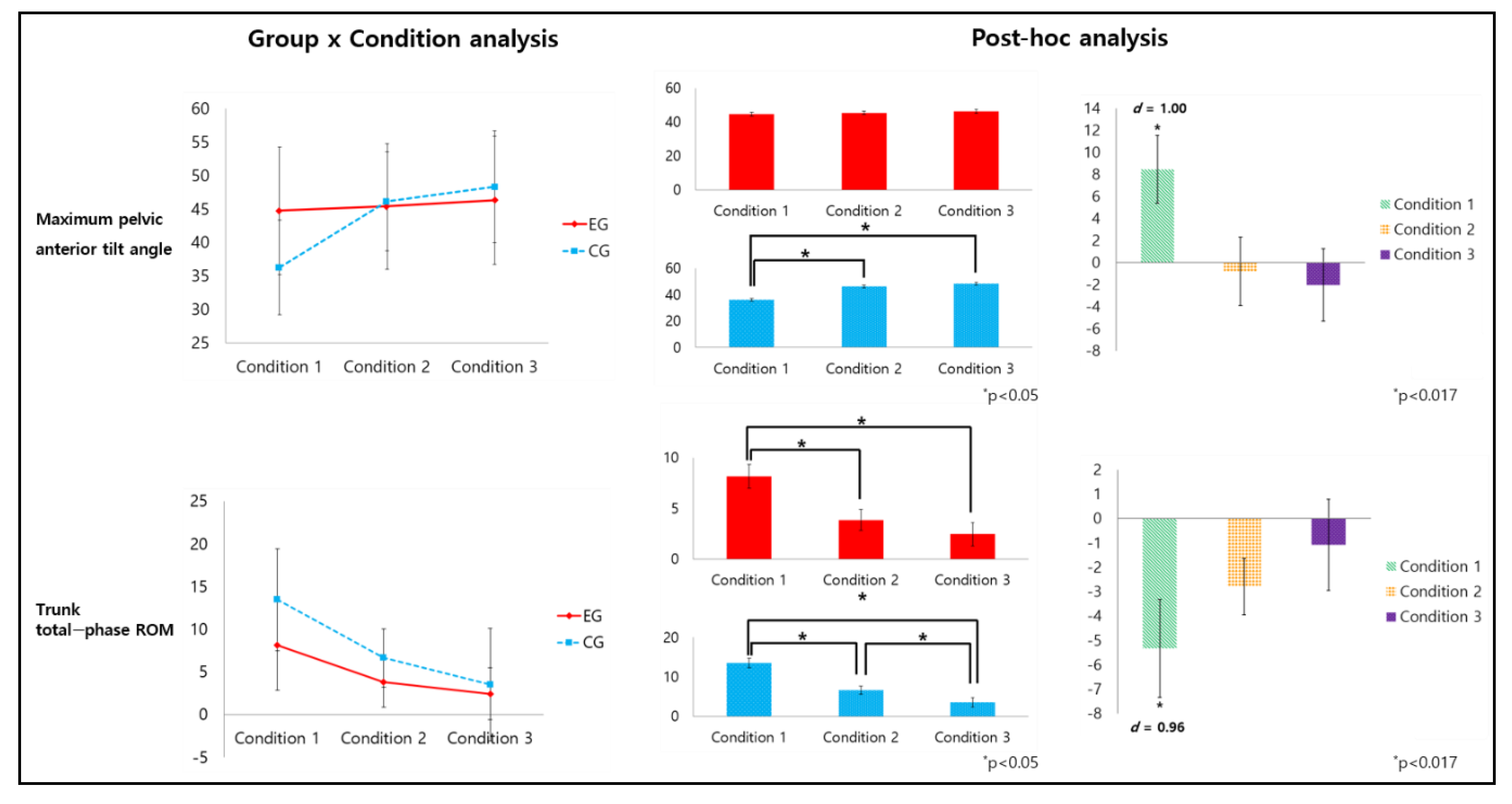
3.2. Analysis of Biomechanical Variables According to the Conditions of Wearing a Lumbar Belt in the Experimental and Control Groups
3.3. Analysis of Pain-Related Psychological Variables According to the Conditions of Wearing a Lumbar Belt in the Experimental Group
4. Discussion
4.1. Analysis of Interactions between Groups and Conditions of Wearing a Lumbar Belt
4.2. Analysis of the Main Effect between the Two Groups
4.3. Analysis of the Main Effects of the Conditions of Wearing Lumbar Belts
4.4. Analysis of Pain-Related Psychological Variables According to Lumbar Belt Conditions
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Freburger, J.K.; Holmes, G.M.; Agans, R.P.; Jackman, A.M.; Darter, J.D.; Wallace, A.S.; Castel, L.D.; Kalsbeek, W.D.; Carey, T.S. The rising prevalence of chronic low back pain. Arch. Intern. Med. 2009, 169, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1545–1602. [CrossRef]
- Dionne, C.E.; Dunn, K.M.; Croft, P.R.; Nachemson, A.L.; Buchbinder, R.; Walker, B.F.; Wyatt, M.; Cassidy, J.D.; Rossignol, M.; Leboeuf-Yde, C.; et al. A consensus approach toward the standardization of back pain definitions for use in prevalence studies. Spine 2008, 33, 95–103. [Google Scholar] [CrossRef]
- Baker, D.I.; King, M.B.; Fortinsky, R.H.; Graff, L.G.t.; Gottschalk, M.; Acampora, D.; Preston, J.; Brown, C.J.; Tinetti, M.E. Dissemination of an evidence-based multicomponent fall risk-assessment and -management strategy throughout a geographic area. J. Am. Geriatr. Soc. 2005, 53, 675–680. [Google Scholar] [CrossRef] [PubMed]
- Hasenbring, M.I.; Hallner, D.; Rusu, A.C. Fear-avoidance- and endurance-related responses to pain: Development and validation of the Avoidance-Endurance Questionnaire (AEQ). Eur. J. Pain 2009, 13, 620–628. [Google Scholar] [CrossRef]
- Schaafsma, F.G.; Anema, J.R.; van der Beek, A.J. Back pain: Prevention and management in the workplace. Best Pract. Res. Clin. Rheumatol. 2015, 29, 483–494. [Google Scholar] [CrossRef]
- Maher, C.; Underwood, M.; Buchbinder, R. Non-specific low back pain. Lancet 2017, 389, 736–747. [Google Scholar] [CrossRef]
- Thelin, A.; Holmberg, S.; Thelin, N. Functioning in neck and low back pain from a 12-year perspective: A prospective population-based study. J. Rehabil. Med. 2008, 40, 555–561. [Google Scholar] [CrossRef][Green Version]
- Eriksrud, O.; Bohannon, R.W. Relationship of knee extension force to independence in sit-to-stand performance in patients receiving acute rehabilitation. Phys. Ther. 2003, 83, 544–551. [Google Scholar] [CrossRef]
- Hughes, M.A.; Weiner, D.K.; Schenkman, M.L.; Long, R.M.; Studenski, S.A. Chair rise strategies in the elderly. Clin. Biomech. 1994, 9, 187–192. [Google Scholar] [CrossRef]
- Dall, P.M.; Kerr, A. Frequency of the sit to stand task: An observational study of free-living adults. Appl. Ergon. 2010, 41, 58–61. [Google Scholar] [CrossRef]
- Hadgraft, N.T.; Lynch, B.M.; Clark, B.K.; Healy, G.N.; Owen, N.; Dunstan, D.W. Excessive sitting at work and at home: Correlates of occupational sitting and TV viewing time in working adults. BMC Public Health 2015, 15, 899. [Google Scholar] [CrossRef] [PubMed]
- Collins, J.D.; O’Sullivan, L.W. Musculoskeletal disorder prevalence and psychosocial risk exposures by age and gender in a cohort of office based employees in two academic institutions. Int. J. Ind. Ergon. 2015, 46, 85–97. [Google Scholar] [CrossRef]
- Andersson, E.I.; Lin, C.C.; Smeets, R.J. Performance tests in people with chronic low back pain: Responsiveness and minimal clinically important change. Spine 2010, 35, 1559–1563. [Google Scholar] [CrossRef]
- Claeys, K.; Dankaerts, W.; Janssens, L.; Brumagne, S. Altered preparatory pelvic control during the sit-to-stance-to-sit movement in people with non-specific low back pain. J. Electromyogr. Kinesiol. 2012, 22, 821–828. [Google Scholar] [CrossRef] [PubMed]
- McGill, S.M. Linking latest knowledge of injury mechanisms and spine function to the prevention of low back disorders. J. Electromyogr. Kinesiol. 2004, 14, 43–47. [Google Scholar] [CrossRef]
- Sedrez, J.A.; Mesquita, P.V.; Gelain, G.M.; Candotti, C.T. kinematic characteristics of sit-to-stand movements in patients with low back pain: A systematic review. J. Manip. Physiol. Ther. 2019, 42, 532–540. [Google Scholar] [CrossRef] [PubMed]
- Brumagne, S.; Cordo, P.; Lysens, R.; Verschueren, S.; Swinnen, S. The role of paraspinal muscle spindles in lumbosacral position sense in individuals with and without low back pain. Spine 2000, 25, 989–994. [Google Scholar] [CrossRef]
- Newcomer, K.L.; Laskowski, E.R.; Yu, B.; Johnson, J.C.; An, K.N. Differences in repositioning error among patients with low back pain compared with control subjects. Spine 2000, 25, 2488–2493. [Google Scholar] [CrossRef]
- O’Sullivan, P.B.; Burnett, A.; Floyd, A.N.; Gadsdon, K.; Logiudice, J.; Miller, D.; Quirke, H. Lumbar repositioning deficit in a specific low back pain population. Spine 2003, 28, 1074–1079. [Google Scholar] [CrossRef]
- Panjabi, M.M. A hypothesis of chronic back pain: Ligament subfailure injuries lead to muscle control dysfunction. Eur. Spine J. 2006, 15, 668–676. [Google Scholar] [CrossRef]
- Boucher, J.A.; Roy, N.; Preuss, R.; Larivière, C. The effect of two lumbar belt designs on trunk repositioning sense in people with and without low back pain. Ann. Phys. Rehabil. Med. 2017, 60, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Van Duijvenbode, I.C.; Jellema, P.; van Poppel, M.N.; van Tulder, M.W. Lumbar supports for prevention and treatment of low back pain. Cochrane Database Syst. Rev. 2008, 2008, Cd001823. [Google Scholar] [CrossRef]
- Larivière, C.; Caron, J.M.; Preuss, R.; Mecheri, H. The effect of different lumbar belt designs on the lumbopelvic rhythm in healthy subjects. BMC Musculoskelet. Disord. 2014, 15, 307. [Google Scholar] [CrossRef]
- Katsuhira, J.; Sasaki, H.; Asahara, S.; Ikegami, T.; Ishihara, H.; Kikuchi, T.; Hirai, Y.; Yamasaki, Y.; Wada, T.; Maruyama, H. Comparison of low back joint moment using a dynamic 3D biomechanical model in different transferring tasks wearing low back belt. Gait Posture 2008, 28, 258–264. [Google Scholar] [CrossRef] [PubMed]
- McGill, S.M.; Kippers, V. Transfer of loads between lumbar tissues during the flexion-relaxation phenomenon. Spine 1994, 19, 2190–2196. [Google Scholar] [CrossRef]
- Wassell, J.T.; Gardner, L.I.; Landsittel, D.P.; Johnston, J.J.; Johnston, J.M. A prospective study of back belts for prevention of back pain and injury. JAMA 2000, 284, 2727–2732. [Google Scholar] [CrossRef]
- Calmels, P.; Queneau, P.; Hamonet, C.; Le Pen, C.; Maurel, F.; Lerouvreur, C.; Thoumie, P. Effectiveness of a lumbar belt in subacute low back pain: An open, multicentric, and randomized clinical study. Spine 2009, 34, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Mi, J.; Ye, J.; Zhao, X.; Zhao, J. Effects of lumbosacral orthoses on postural control in individuals with or without non-specific low back pain. Eur. Spine J. 2018, 27, 180–186. [Google Scholar] [CrossRef]
- Foster, N.E.; Anema, J.R.; Cherkin, D.; Chou, R.; Cohen, S.P.; Gross, D.P.; Ferreira, P.H.; Fritz, J.M.; Koes, B.W.; Peul, W.; et al. Prevention and treatment of low back pain: Evidence, challenges, and promising directions. Lancet 2018, 391, 2368–2383. [Google Scholar] [CrossRef]
- Shahvarpour, A.; Preuss, R.; Sullivan, M.J.L.; Negrini, A.; Larivière, C. The effect of wearing a lumbar belt on biomechanical and psychological outcomes related to maximal flexion-extension motion and manual material handling. Appl. Ergon. 2018, 69, 17–24. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Ippersiel, P.; Robbins, S.; Preuss, R. Movement variability in adults with low back pain during sit-to-stand-to-sit. Clin. Biomech. 2018, 58, 90–95. [Google Scholar] [CrossRef]
- Von Korff, M.; Deyo, R.A.; Cherkin, D.; Barlow, W. Back pain in primary care. Outcomes at 1 year. Spine 1993, 18, 855–862. [Google Scholar] [CrossRef]
- Chiarotto, A.; Maxwell, L.J.; Terwee, C.B.; Wells, G.A.; Tugwell, P.; Ostelo, R.W. Roland-Morris Disability Questionnaire and Oswestry Disability Index: Which has better measurement properties for measuring physical functioning in nonspecific low back pain? Systematic review and meta-analysis. Phys. Ther. 2016, 96, 1620–1637. [Google Scholar] [CrossRef] [PubMed]
- Ludvig, D.; Preuss, R.; Lariviere, C. The effect of extensible and non-extensible lumbar belts on trunk muscle activity and lumbar stiffness in subjects with and without low-back pain. Clin. Biomech. 2019, 67, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Orakifar, N.; Shaterzadeh-Yazdi, M.J.; Salehi, R.; Mehravar, M.; Namnik, N. Muscle activity pattern dysfunction during sit to stand and stand to sit in the movement system impairment subgroups of low back pain. Arch. Phys. Med. Rehabil. 2019, 100, 851–858. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, J.; Atkins, S.; Richards, J.; Vincent, H. Modelling of muscle force distributions during barefoot and shod running. J. Hum. Kinet. 2015, 47, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Cappozzo, A.; Catani, F.; Croce, U.D.; Leardini, A. Position and orientation in space of bones during movement: Anatomical frame definition and determination. Clin. Biomech. 1995, 10, 171–178. [Google Scholar] [CrossRef]
- Edwards, R.R.; Campbell, C.M.; Fillingim, R.B. Catastrophizing and experimental pain sensitivity: Only in vivo reports of catastrophic cognitions correlate with pain responses. J. Pain 2005, 6, 338–339. [Google Scholar] [CrossRef]
- Leeuw, M.; Goossens, M.E.; van Breukelen, G.J.; Boersma, K.; Vlaeyen, J.W. Measuring perceived harmfulness of physical activities in patients with chronic low back pain: The Photograph Series of Daily Activities—Short electronic version. J. Pain 2007, 8, 840–849. [Google Scholar] [CrossRef]
- Edwards, R.R.; Smith, M.T.; Stonerock, G.; Haythornthwaite, J.A. Pain-related catastrophizing in healthy women is associated with greater temporal summation of and reduced habituation to thermal pain. Clin. J. Pain 2006, 22, 730–737. [Google Scholar] [CrossRef] [PubMed]
- Etnyre, B.; Thomas, D.Q. Event standardization of sit-to-stand movements. Phys. Ther. 2007, 87, 1651–1666. [Google Scholar] [CrossRef]
- Schenkman, M.; Riley, P.O.; Pieper, C. Sit to stand from progressively lower seat heights—Alterations in angular velocity. Clin. Biomech. 1996, 11, 153–158. [Google Scholar] [CrossRef]
- Stevermer, C.A.; Gillette, J.C. Kinematic and kinetic indicators of sit-to-stand. J. Appl. Biomech. 2016, 32, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Pai, Y.C.; Rogers, M.W. Control of body mass transfer as a function of speed of ascent in sit-to-stand. Med. Sci. Sports Exerc. 1990, 22, 378–384. [Google Scholar] [CrossRef]
- Nuzik, S.; Lamb, R.; VanSant, A.; Hirt, S. Sit-to-stand movement pattern. A kinematic study. Phys. Ther. 1986, 66, 1708–1713. [Google Scholar] [CrossRef]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef]
- Nahm, F.S. Understanding effect sizes. Hanyang Med. Rev. 2015, 35, 40–43. [Google Scholar] [CrossRef][Green Version]
- Shum, G.L.; Crosbie, J.; Lee, R.Y. Effect of low back pain on the kinematics and joint coordination of the lumbar spine and hip during sit-to-stand and stand-to-sit. Spine 2005, 30, 1998–2004. [Google Scholar] [CrossRef]
- Van Poppel, M.N.; de Looze, M.P.; Koes, B.W.; Smid, T.; Bouter, L.M. Mechanisms of action of lumbar supports: A systematic review. Spine 2000, 25, 2103–2113. [Google Scholar] [CrossRef] [PubMed]
- Graham, R.B.; Smallman, C.L.; Sadler, E.M.; Stevenson, J.M. Interjoint coordination and the personal lift-assist device. J. Appl. Biomech. 2013, 29, 194–204. [Google Scholar] [CrossRef][Green Version]
- Roebroeck, M.E.; Doorenbosch, C.A.; Harlaar, J.; Jacobs, R.; Lankhorst, G.J. Biomechanics and muscular activity during sit-to-stand transfer. Clin. Biomech. 1994, 9, 235–244. [Google Scholar] [CrossRef]
- Tully, E.A.; Fotoohabadi, M.R.; Galea, M.P. Sagittal spine and lower limb movement during sit-to-stand in healthy young subjects. Gait Posture 2005, 22, 338–345. [Google Scholar] [CrossRef]
- Crosbie, J.; Nascimento, D.P.; Filho Rde, F.; Ferreira, P. Do people with recurrent back pain constrain spinal motion during seated horizontal and downward reaching? Clin. Biomech. 2013, 28, 866–872. [Google Scholar] [CrossRef] [PubMed]
- Sung, P.S.; Danial, P. Analysis of relative kinematic index with normalized standing time between subjects with and without recurrent low back pain. Eur. Spine J. 2017, 26, 518–527. [Google Scholar] [CrossRef]
- Ivancic, P.C.; Cholewicki, J.; Radebold, A. Effects of the abdominal belt on muscle-generated spinal stability and L4/L5 joint compression force. Ergonomics 2002, 45, 501–513. [Google Scholar] [CrossRef] [PubMed]
- Lavender, S.A.; Shakeel, K.; Andersson, G.B.; Thomas, J.S. Effects of a lifting belt on spine moments and muscle recruitments after unexpected sudden loading. Spine 2000, 25, 1569–1578. [Google Scholar] [CrossRef]
- Larivière, C.; Ludvig, D.; Kearney, R.; Mecheri, H.; Caron, J.M.; Preuss, R. Identification of intrinsic and reflexive contributions to low-back stiffness: Medium-term reliability and construct validity. J. Biomech. 2015, 48, 254–261. [Google Scholar] [CrossRef]
- Jegede, K.A.; Miller, C.P.; Bible, J.E.; Whang, P.G.; Grauer, J.N. The effects of three different types of orthoses on the range of motion of the lumbar spine during 15 activities of daily living. Spine 2011, 36, 2346–2353. [Google Scholar] [CrossRef]
- Utter, A.; Anderson, M.L.; Cunniff, J.G.; Kaufman, K.R.; Jelsing, E.J.; Patrick, T.A.; Magnuson, D.J.; Maus, T.P.; Yaszemski, M.J.; Basford, J.R. Video fluoroscopic analysis of the effects of three commonly-prescribed off-the-shelf orthoses on vertebral motion. Spine 2010, 35, 525–529. [Google Scholar] [CrossRef] [PubMed]
- Cholewicki, J.; Shah, K.R.; McGill, K.C. The effects of a 3-week use of lumbosacral orthoses on proprioception in the lumbar spine. J. Orthop. Sports Phys. Ther. 2006, 36, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Munoz, F.; Salmochi, J.F.; Faouen, P.; Rougier, P. Low back pain sufferers: Is standing postural balance facilitated by a lordotic lumbar brace? Orthop. Traumatol. Surg. Res. 2010, 96, 362–366. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Larivière, C.; Gagnon, D.; Loisel, P. The effect of load on the coordination of the trunk for subjects with and without chronic low back pain during flexion-extension and lateral bending tasks. Clin. Biomech. 2000, 15, 407–416. [Google Scholar] [CrossRef]
- Penrose, K.W.; Chook, K.; Stump, J.L. Acute and chronic effects of pneumatic lumbar support on muscular strength, flexibility, and functional impairment index. Res. Sports Med. Int. J. 1991, 2, 121–129. [Google Scholar] [CrossRef]
- Ostelo, R.W.; Deyo, R.A.; Stratford, P.; Waddell, G.; Croft, P.; Von Korff, M.; Bouter, L.M.; de Vet, H.C. Interpreting change scores for pain and functional status in low back pain: Towards international consensus regarding minimal important change. Spine 2008, 33, 90–94. [Google Scholar] [CrossRef]
- Volders, S.; Meulders, A.; De Peuter, S.; Vlaeyen, J.W. The reduction of fear of movement-related pain: Does motivational context matter? Clin. J. Pain 2015, 31, 933–945. [Google Scholar] [CrossRef]
- Woby, S.R.; Urmston, M.; Watson, P.J. Self-efficacy mediates the relation between pain-related fear and outcome in chronic low back pain patients. Eur. J. Pain 2007, 11, 711–718. [Google Scholar] [CrossRef]
- Azadinia, F.; Ebrahimi, E.T.; Kamyab, M.; Parnianpour, M.; Cholewicki, J.; Maroufi, N. Can lumbosacral orthoses cause trunk muscle weakness? A systematic review of literature. Spine J. 2017, 17, 589–602. [Google Scholar] [CrossRef]
- Ciriello, V.M. Does wearing a non-expanding weight lifting belt change psychophysically determined maximum acceptable weights and forces. Int. J. Ind. Ergon. 2008, 38, 1045–1050. [Google Scholar] [CrossRef]
- Roelofs, P.D.; Bierma-Zeinstra, S.M.; van Poppel, M.N.; Jellema, P.; Willemsen, S.P.; van Tulder, M.W.; van Mechelen, W.; Koes, B.W. Lumbar supports to prevent recurrent low back pain among home care workers: A randomized trial. Ann. Intern. Med. 2007, 147, 685–692. [Google Scholar] [CrossRef] [PubMed]



| Variable | CG (n = 15) | EG (n = 15) | p |
|---|---|---|---|
| Sex (Male, %) | 9 (60.0) | 8 (53.3) | 0.500 † |
| Age (years) | 34.53 (4.40) | 35.60 (5.19) | 0.549 ‡ |
| Height (cm) | 171.40 (9.83) | 170.20 (8.08) | 0.718 ‡ |
| Weight (kg) | 70.60 (12.50) | 67.40 (14.60) | 0.525 ‡ |
| BMI (kg/m2) | 23.85 (2.26) | 23.02 (3.38) | 0.437 ‡ |
| VAS (score) | 3.80 (0.86) | ||
| ODI (%) | 19.60 (4.42) | ||
| Onset (month) | 43.06 (33.35) |
| Variable | Condition 1 (No LB) | Condition 2 (Extensible LB) | Condition 3 (Non-Extensible LB) | P (f) | Post-Hoc | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| CG | EG | CG | EG | CE | EG | Group (G) | Condition (C) | G x C | ||
| Maximum trunk flexion (deg) | 47.07 (10.33) | 41.74 (7.26) | 47.36 (10.86) | 46.05 (6.21) | 48.06 (9.47) | 45.97 (7.01) | 0.338 | 0.022 * (0.41) | 0.100 | C1 < C2, C1 < C3 |
| Maximum anterior pelvic tilt (deg) | 36.27 (7.10) | 44.73 (9.58) | 46.16 (8.40) | 45.38 (9.57) | 48.33 (7.39) | 46.30 (9.43) | 0.528 | <0.001 * (0.99) | <0.001 * (0.79) | CG: C1 < C2, C1 < C3 C1: CG < EG |
| Maximum hip-joint flexion (deg) | 104.21 (8.69) | 107.13 (9.94) | 111.81 (10.19) | 112.14 (9.60) | 115.04 (10.54) | 112.89 (8.04) | 0.939 | <0.001 * (0.87) | 0.162 | C1 < C2, C1 < C3, C2 < C3 |
| Maximum knee-joint flexion (deg) | 77.93 (7.99) | 83.40 (9.65) | 76.43 (7.71) | 81.25 (8.81) | 76.16 (8.14) | 81.78 (9.67) | 0.095 | 0.019 * (0.38) | 0.832 | C1 > C2, C1 > C3 |
| Maximum ankle-joint flexion (deg) | 11.16 (5.84) | 9.48 (3.70) | 10.90 (5.47) | 11.27 (5.77) | 11.94 (4.83) | 10.48 (6.80) | 0.608 | 0.472 | 0.364 | |
| Trunk flexion-phase ROM (deg) | 7.48 (4.34) | 4.55 (3.72) | 1.65 (2.85) | 0.76 (3.26) | 1.14 (3.06) | 0.54 (2.43) | 0.056 | <0.001 * (0.92) | 0.315 | C1 > C2, C1 > C3 |
| Trunk extension-phase ROM (deg) | 24.99 (8.42) | 19.58 (5.85) | 9.98 (7.56) | 7.57 (5.22) | 4.33 (3.13) | 3.36 (2.50) | 0.101 | <0.001 * (2.35) | 0.123 | C1 > C2, C1 > C3, C2 > C3 |
| Trunk total-phase ROM (deg) | 13.47 (5.95) | 8.14 (5.26) | 6.65 (6.62) | 3.85 (3.03) | 3.54 (3.40) | 2.46 (2.96) | 0.052 | <0.001 * (1.50) | 0.016 * (0.41) | CG: C1 > C2, C1 > C3, C2 > C3 EG: C1 > C2, C1 > C3 C1: CG > EG |
| Hip-joint flexion-phase ROM (deg) | 24.97 (6.43) | 26.69 (6.46) | 30.59 (5.93) | 32.93 (6.55) | 30.89 (6.05) | 31.92 (5.31) | 0.416 | <0.001 * (1.12) | 0.648 | C1 < C2, C1 < C3 |
| Hip-joint extension-phase ROM (deg) | 99.90 (7.52) | 105.27 (9.95) | 109.62 (6.39) | 110.00 (10.67) | 110.48 (7.44) | 113.92 (9.69) | 0.279 | <0.001 * (0.98) | 0.202 | C1 < C2, C1 < C3, C2 < C3 |
| Hip-joint total-phase ROM (deg) | 104.73 (8.69) | 109.32 (7.39) | 110.82 (8.09) | 111.88 (10.39) | 112.77 (6.95) | 114.39 (9.45) | 0.345 | 0.003 * (0.55) | 0.452 | C1 < C2, C1 < C3, C2 < C3 |
| Knee-joint flexion-phase ROM (deg) | 5.00 (1.99) | 6.48 (2.04) | 4.87 (1.94) | 6.45 (2.04) | 4.60 (2.33) | 6.50 (2.10) | 0.011 * (0.52) | 0.896 | 0.857 | EG > CG |
| Knee-joint extension-phase ROM (deg) | 76.19 (10.88) | 79.95 (11.94) | 75.24 (12.32) | 76.66 (10.59) | 74.34 (9.71) | 75.06 (9.96) | 0.608 | 0.020 * (0.41) | 0.357 | C1 > C2, C1 > C3 |
| Knee-joint total-phase ROM (deg) | 80.72 (10.86) | 84.64 (10.97) | 76.21 (10.28) | 82.32 (9.72) | 77.51 (9.83) | 80.85 (9.97) | 0.220 | 0.002 * (0.50) | 0.386 | C1 > C2, C1 > C3 |
| Ankle-joint flexion-phase ROM (deg) | 6.57 (2.63) | 6.86 (1.79) | 6.45 (3.80) | 5.58 (1.83) | 6.88 (2.81) | 5.68 (1.86) | 0.473 | 0.211 | 0.150 | |
| Ankle-joint extension-phase ROM (deg) | 11.99 (3.48) | 10.42 (3.10) | 11.49 (4.89) | 9.89 (3.69) | 11.39 (4.91) | 9.77 (4.02) | 0.237 | 0.524 | 0.999 | |
| Ankle-joint total-phase ROM (deg) | 15.24 (4.66) | 14.81 (4.26) | 15.10 (4.62) | 14.71 (3.85) | 14.94 (4.55) | 14.28 (3.25) | 0.697 | 0.855 | 0.970 | |
| Anterior-posterior GRF (N/kg) | −46.42 (12.41) | −41.85 (12.69) | −48.35 (10.48) | −47.78 (12.71) | −48.29 (13.26) | −48.87 (10.42) | 0.701 | 0.040 * (0.38) | 0.291 | C1 < C2, C1 < C3 |
| Medial-lateral GRF (N/kg) | 68.58 (14.78) | 63.34 (17.79) | 69.11 (12.91) | 63.54 (13.61) | 66.76 (12.07) | 61.50 (10.63) | 0.262 | 0.386 | 0.994 | |
| Vertical GRF (N/kg) | 588.44 (38.37) | 572.12 (31.94) | 596.84 (29.14) | 579.49 (45.78) | 603.27 (43.55) | 590.32 (30.24) | 0.212 | 0.009 * (0.43) | 0.906 | C1 < C3 |
| Variable | Condition 1 (No LB) | Condition 2 (Extensible LB) | Condition 3 (Non-Extensible LB) | p (f) | Post-Hoc |
|---|---|---|---|---|---|
| VAS | 4.07 (0.88) | 3.27 (0.70) | 3.47 (0.74) | 0.001 * (0.83) | C1 > C2, C1 > C3 |
| PHODA | 4.27 (0.59) | 3.20 (0.68) | 3.40 (0.51) | <0.001 * (2.00) | C1 > C2, C1 > C3 |
| PC | 2.53 (0.64) | 1.80 (0.41) | 1.87 (0.35) | 0.001 * (0.97) | C1 > C2, C1 > C3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Im, S.-C.; Cho, H.-Y.; Lee, J.-H.; Kim, K. Analysis of the Effect of Wearing Extensible and Non-Extensible Lumbar Belts on Biomechanical Factors of the Sit-to-Stand Movement and Pain-Related Psychological Factors Affecting Office Workers with Low Back Pain. Healthcare 2021, 9, 1601. https://doi.org/10.3390/healthcare9111601
Im S-C, Cho H-Y, Lee J-H, Kim K. Analysis of the Effect of Wearing Extensible and Non-Extensible Lumbar Belts on Biomechanical Factors of the Sit-to-Stand Movement and Pain-Related Psychological Factors Affecting Office Workers with Low Back Pain. Healthcare. 2021; 9(11):1601. https://doi.org/10.3390/healthcare9111601
Chicago/Turabian StyleIm, Sang-Cheol, Ho-Young Cho, Jae-Hong Lee, and Kyoung Kim. 2021. "Analysis of the Effect of Wearing Extensible and Non-Extensible Lumbar Belts on Biomechanical Factors of the Sit-to-Stand Movement and Pain-Related Psychological Factors Affecting Office Workers with Low Back Pain" Healthcare 9, no. 11: 1601. https://doi.org/10.3390/healthcare9111601
APA StyleIm, S.-C., Cho, H.-Y., Lee, J.-H., & Kim, K. (2021). Analysis of the Effect of Wearing Extensible and Non-Extensible Lumbar Belts on Biomechanical Factors of the Sit-to-Stand Movement and Pain-Related Psychological Factors Affecting Office Workers with Low Back Pain. Healthcare, 9(11), 1601. https://doi.org/10.3390/healthcare9111601






