Lean Yet Unhealthy: Asian American Adults Had Higher Risks for Metabolic Syndrome than Non-Hispanic White Adults with the Same Body Mass Index: Evidence from NHANES 2011–2016
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Measures
2.3. Statistical Analysis
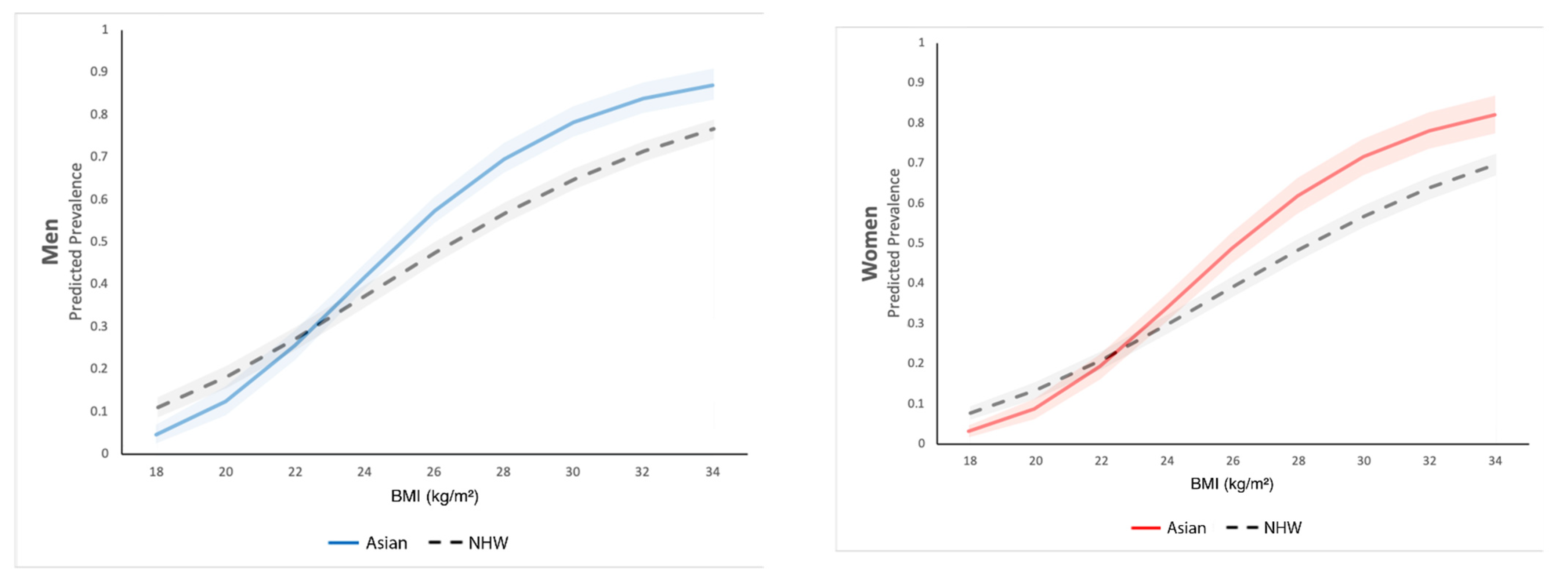
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mottillo, S.; Filion, K.B.; Genest, J.; Joseph, L.; Pilote, L.; Poirier, P.; Rinfret, S.; Schiffrin, E.L.; Eisenberg, M.J. The Metabolic Syndrome and Cardiovascular Risk: A Systematic Review and Meta-Analysis. J. Am. Coll. Cardiol. 2010, 56, 1113–1132. [Google Scholar] [CrossRef] [Green Version]
- Isomaa, B.; Almgren, P.; Tuomi, T.; Forsén, B.; Lahti, K.; Nissén, M.; Taskinen, M.-R.; Groop, L. Cardiovascular Morbidity and Mortality Associated with the Metabolic Syndrome. Diabetes Care 2001, 24, 683–689. [Google Scholar] [CrossRef] [Green Version]
- O’Neill, S.; O’Driscoll, L. Metabolic Syndrome: A Closer Look at the Growing Epidemic and Its Associated Pathologies. Obes. Rev. 2015, 16, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, P.W.F.; D’Agostino, R.B.; Parise, H.; Sullivan, L.; Meigs, J.B. Metabolic Syndrome as a Precursor of Cardiovascular Disease and Type 2 Diabetes Mellitus. Circulation 2005, 112, 3066–3072. [Google Scholar] [CrossRef] [PubMed]
- Hui, W.S.; Liu, Z.; Ho, S.C. Metabolic Syndrome and All-Cause Mortality: A Meta-Analysis of Prospective Cohort Studies. Eur. J. Epidemiol. 2010, 25, 375–384. [Google Scholar] [CrossRef]
- Mente, A.; Yusuf, S.; Islam, S.; McQueen, M.J.; Tanomsup, S.; Onen, C.L.; Rangarajan, S.; Gerstein, H.C.; Anand, S.S. Metabolic Syndrome and Risk of Acute Myocardial Infarction: A Case-Control Study of 26,903 Subjects From 52 Countries. J. Am. Coll. Cardiol. 2010, 55, 2390–2398. [Google Scholar] [CrossRef] [Green Version]
- Kassi, E.; Pervanidou, P.; Kaltsas, G.; Chrousos, G. Metabolic Syndrome: Definitions and Controversies. BMC Med. 2011, 9, 48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C.; et al. Diagnosis and Management of the Metabolic Syndrome. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [Green Version]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.-C.; James, W.P.T.; Loria, C.M.; Smith, S.C. Harmonizing the Metabolic Syndrome. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [Green Version]
- Alberti, K.G.M.; Zimmet, P.; Shaw, J. The Metabolic Syndrome—A New Worldwide Definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- Prasad, H.; Ryan, D.A.; Celzo, M.F.; Stapleton, D. Metabolic Syndrome: Definition and Therapeutic Implications. Postgrad. Med. 2012, 124, 21–30. [Google Scholar] [CrossRef]
- Raji, A.; Seely, E.W.; Arky, R.A.; Simonson, D.C. Body Fat Distribution and Insulin Resistance in Healthy Asian Indians and Caucasians. J. Clin. Endocrinol. Metab. 2001, 86, 5366–5371. [Google Scholar] [CrossRef]
- Deurenberg, P.; Deurenberg-Yap, M.; Guricci, S. Asians Are Different from Caucasians and from Each Other in Their Body Mass Index/Body Fat per Cent Relationship. Obes. Rev. 2002, 3, 141–146. [Google Scholar] [CrossRef] [Green Version]
- Wulan, S.N.; Westerterp, K.R.; Plasqui, G. Ethnic Differences in Body Composition and the Associated Metabolic Profile: A Comparative Study between Asians and Caucasians. Maturitas 2010, 65, 315–319. [Google Scholar] [CrossRef] [PubMed]
- Dickinson, S.; Colagiuri, S.; Faramus, E.; Petocz, P.; Brand-Miller, J.C. Postprandial Hyperglycemia and Insulin Sensitivity Differ among Lean Young Adults of Different Ethnicities. J. Nutr. 2002, 132, 2574–2579. [Google Scholar] [CrossRef] [Green Version]
- Shelley-Jones, D.C.; Wein, P.; Nolan, C.; Beischer, N.A. Why Do Asian-Born Women Have a Higher Incidence of Gestational Diabetes? An Analysis of Racial Differences in Body Habitus, Lipid Metabolism and the Serum Insulin Response to an Oral Glucose Load. Aust. N. Z. J. Obstet. Gynaecol. 1993, 33, 114–118. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Mohammed, S.A.; Leavell, J.; Collins, C. Race, Socioeconomic Status, and Health: Complexities, Ongoing Challenges, and Research Opportunities. Ann. N. Y. Acad. Sci. 2010, 1186, 69–101. [Google Scholar] [CrossRef] [PubMed]
- Dankwa-Mullan, I.; Rhee, K.B.; Williams, K.; Sanchez, I.; Sy, F.S.; Stinson, N., Jr.; Ruffin, J. The Science of Eliminating Health Disparities: Summary and Analysis of the NIH Summit Recommendations. Am. J. Public Health 2010, 100, S12–S18. [Google Scholar] [CrossRef] [PubMed]
- Holland, A.T.; Palaniappan, L.P. Problems with the Collection and Interpretation of Asian-American Health Data: Omission, Aggregation, and Extrapolation. Ann. Epidemiol. 2012, 22, 397–405. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palaniappan, L.P.; Wong, E.C.; Shin, J.J.; Fortmann, S.P.; Lauderdale, D.S. Asian Americans Have Greater Prevalence of Metabolic Syndrome despite Lower Body Mass Index. Int. J. Obes. 2011, 35, 393–400. [Google Scholar] [CrossRef] [Green Version]
- Zhang, H.; Rodriguez-Monguio, R. Racial Disparities in the Risk of Developing Obesity-Related Diseases: A Cross-Sectional Study. Ethn. Dis. 2012, 22, 308–316. [Google Scholar] [PubMed]
- Jain, A.; Mitchell, S.; Chirumamilla, R.; Zhang, J.; Horn, I.B.; Lewin, A.; Huang, Z.J. Prevalence of Obesity among Young Asian-American Children. Child. Obes. 2012, 8, 518–525. [Google Scholar] [CrossRef] [Green Version]
- Katz, E.G.; Stevens, J.; Truesdale, K.P.; Cai, J.; North, K.E.; Steffen, L.M. Associations of Body Mass Index with Incident Hypertension in American White, American Black and Chinese Asian Adults in Early and Middle Adulthood: The Coronary Artery Risk Development in Young Adults (CARDIA) Study, the Atherosclerosis Risk in Communities (ARIC) Study and the People’s Republic of China (PRC) Study. Asia Pac. J. Clin. Nutr. 2013, 22, 626–634. [Google Scholar]
- Ye, J.; Rust, G.; Baltrus, P.; Daniels, E. Cardiovascular Risk Factors among Asian Americans: Results from a National Health Survey. Ann. Epidemiol. 2009, 19, 718–723. [Google Scholar] [CrossRef] [Green Version]
- Wong, R.J.; Chou, C.; Sinha, S.R.; Kamal, A.; Ahmed, A. Ethnic Disparities in the Association of Body Mass Index with the Risk of Hypertension and Diabetes. J. Community Health 2014, 39, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.W.R.; Brancati, F.L.; Yeh, H.-C. Trends in the Prevalence of Type 2 Diabetes in Asians Versus Whites: Results from the United States National Health Interview Survey, 1997–2008. Diabetes Care 2011, 34, 353–357. [Google Scholar] [CrossRef] [Green Version]
- McNeely, M.J.; Boyko, E.J. Type 2 Diabetes Prevalence in Asian Americans: Results of a National Health Survey. Diabetes Care 2004, 27, 66–69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jih, J.; Mukherjea, A.; Vittinghoff, E.; Nguyen, T.T.; Tsoh, J.Y.; Fukuoka, Y.; Bender, M.S.; Tseng, W.; Kanaya, A.M. Using Appropriate Body Mass Index Cut Points for Overweight and Obesity among Asian Americans. Prev. Med. 2014, 65, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Palaniappan, L.P.; Araneta, M.R.G.; Assimes, T.L.; Barrett-Connor, E.L.; Carnethon, M.R.; Criqui, M.H.; Fung, G.L.; Narayan, K.M.V.; Patel, H.; Taylor-Piliae, R.E.; et al. Call to Action: Cardiovascular Disease in Asian Americans. Circulation 2010, 122, 1242–1252. [Google Scholar] [CrossRef] [Green Version]
- Jose, P.O.; Frank, A.T.H.; Kapphahn, K.I.; Goldstein, B.A.; Eggleston, K.; Hastings, K.G.; Cullen, M.R.; Palaniappan, L.P. Cardiovascular Disease Mortality in Asian Americans. J. Am. Coll. Cardiol. 2014, 64, 2486–2494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holland, A.T.; Wong, E.C.; Lauderdale, D.S.; Palaniappan, L.P. Spectrum of Cardiovascular Diseases in Asian-American Racial/Ethnic Subgroups. Ann. Epidemiol. 2011, 21, 608–614. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pan, W.-H.; Yeh, W.-T.; Weng, L.-C. Epidemiology of Metabolic Syndrome in Asia. Asia Pac. J. Clin. Nutr. 2008, 17, 37–42. [Google Scholar]
- Stefan, N.; Schick, F.; Häring, H.-U. Causes, Characteristics, and Consequences of Metabolically Unhealthy Normal Weight in Humans. Cell Metab. 2017, 26, 292–300. [Google Scholar] [CrossRef] [PubMed]
- Conus, F.; Rabasa-Lhoret, R.; Péronnet, F. Characteristics of Metabolically Obese Normal-Weight (MONW) Subjects. Appl. Physiol. Nutr. Metab. 2007, 32, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Leigh, J.A.; Alvarez, M.; Rodriguez, C.J. Ethnic Minorities and Coronary Heart Disease: An Update and Future Directions. Curr. Atheroscler. Rep. 2016, 18, 9. [Google Scholar] [CrossRef] [Green Version]
- Echeverria, S.E.; Mustafa, M.; Pentakota, S.R.; Kim, S.; Hastings, K.G.; Amadi, C.; Palaniappan, L. Social and Clinically-Relevant Cardiovascular Risk Factors in Asian Americans Adults: NHANES 2011–2014. Prev. Med. 2017, 99, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Narayan, K.M.V.; Aviles-Santa, L.; Oza-Frank, R.; Pandey, M.; Curb, J.D.; McNeely, M.; Araneta, M.R.G.; Palaniappan, L.; Rajpathak, S.; Barrett-Connor, E. Report of a National Heart, Lung, and Blood Institute Workshop: Heterogeneity in Cardiometabolic Risk in Asian Americans in the U.S.: Opportunities for Research. J. Am. Coll. Cardiol. 2010, 55, 966–973. [Google Scholar] [CrossRef] [Green Version]
- Hastings, K.G.; Jose, P.O.; Kapphahn, K.I.; Frank, A.T.H.; Goldstein, B.A.; Thompson, C.A.; Eggleston, K.; Cullen, M.R.; Palaniappan, L.P. Leading Causes of Death among Asian American Subgroups (2003–2011). PLoS ONE 2015, 10, e0124341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CDC/National Center for Health Statistics NHANES 2011–2012 Overview. Available online: https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/overview.aspx?BeginYear=2011 (accessed on 4 November 2021).
- CDC/National Center for Health Statistics NHANES 2013–2014 Overview. Available online: https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?BeginYear=2013 (accessed on 4 November 2021).
- CDC/National Center for Health Statistics NHANES 2015–2016 Overview. Available online: https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/overview.aspx?BeginYear=2013 (accessed on 4 November 2021).
- Mirel, L.B.; Mohadjer, L.K.; Dohrmann, S.M.; Clark, J.; Burt, V.L.; Johnson, C.L.; Curtin, L.R. National Health and Nutrition Examination Survey: Estimation Procedures, 2007–2010. Vital Health Stat. 2 2013, 159, 1–17. [Google Scholar]
- Alberti, K.G.M.M.; Zimmet, P.; Shaw, J. Metabolic Syndrome—A New World-Wide Definition. A Consensus Statement from the International Diabetes Federation. Diabet. Med. 2006, 23, 469–480. [Google Scholar] [CrossRef]
- WHO. Expert Consultation Appropriate Body-Mass Index for Asian Populations and Its Implications for Policy and Intervention Strategies. Lancet 2004, 363, 157–163. [Google Scholar] [CrossRef]
- Yang, L.; Toriola, A.T. Leisure-Time Physical Activity and Circulating 25-Hydroxyvitamin D Levels in Cancer Survivors: A Cross-Sectional Analysis Using Data from the US National Health and Nutrition Examination Survey. BMJ Open 2017, 7, e016064. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd ed.; U.S. Department of Health and Human Services: Washington, DC, USA, 2018.
- Tucker, L.A. Physical Activity and Telomere Length in U.S. Men and Women: An NHANES Investigation. Prev. Med. 2017, 100, 145–151. [Google Scholar] [CrossRef]
- Taylor, A.L.; Denniston, M.M.; Klevens, R.M.; McKnight-Eily, L.R.; Jiles, R.B. Association of Hepatitis C Virus with Alcohol Use among U.S. Adults: NHANES 2003–2010. Am. J. Prev. Med. 2016, 51, 206–215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NHANES. Subsample Notes and Data. Available online: https://wwwn.cdc.gov/nchs/nhanes/search/subsample_weights.aspx (accessed on 13 February 2020).
- Taylor, J.M.G.; Cooper, K.L.; Wei, J.T.; Sarma, A.V.; Raghunathan, T.E.; Heeringa, S.G. Use of Multiple Imputation to Correct for Nonresponse Bias in a Survey of Urologic Symptoms among African-American Men. Am. J. Epidemiol. 2002, 156, 774–782. [Google Scholar] [CrossRef] [Green Version]
- StataCorp. Stata Statistical Software: Release 16; StataCorp LLC: College Station, TX, USA, 2019. [Google Scholar]
- Misra, A.; Vikram, N.K. Insulin Resistance Syndrome (Metabolic Syndrome) and Obesity in Asian Indians: Evidence and Implications. Nutrition 2004, 20, 482–491. [Google Scholar] [CrossRef] [PubMed]
- Misra, A.; Khurana, L. The Metabolic Syndrome in South Asians: Epidemiology, Determinants, and Prevention. Metab. Syndr. Relat. Disord. 2009, 7, 497–514. [Google Scholar] [CrossRef]
- Shai, I.; Jiang, R.; Manson, J.E.; Stampfer, M.J.; Willett, W.C.; Colditz, G.A.; Hu, F.B. Ethnicity, Obesity, and Risk of Type 2 Diabetes in Women: A 20-Year Follow-up Study. Diabetes Care 2006, 29, 1585–1590. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chait, A.; den Hartigh, L.J. Adipose Tissue Distribution, Inflammation and Its Metabolic Consequences, Including Diabetes and Cardiovascular Disease. Front. Cardiovasc. Med. 2020, 7, 22. [Google Scholar] [CrossRef] [Green Version]
- Regitz-Zagrosek, V.; Lehmkuhl, E.; Weickert, M.O. Gender Differences in the Metabolic Syndrome and Their Role for Cardiovascular Disease. Clin. Res. Cardiol. 2006, 95, 147. [Google Scholar] [CrossRef] [Green Version]
- Beigh, S.H.; Jain, S. Prevalence of Metabolic Syndrome and Gender Differences. Bioinformation 2012, 8, 613–616. [Google Scholar] [CrossRef] [PubMed]
- Borjas, G.J.; Slusky, D.J.G. Health, Employment, and Disability: Implications from the Undocumented Population; National Bureau of Economic Research: Cambridge, MA, USA, 2018. [Google Scholar]
| Criteria: Central Obesity (Defined as Waist Circumference ≥90 cm for South and East Asian Men and ≥80 cm for South and East Asian Women, with Ethnicity-Specific Values, Assumed if BMI is >30 kg/m2) Plus, Any Two of the Following Four Factors… | |
|---|---|
| Raised triglycerides | ≥150 mg/dL |
| Reduced HDL cholesterol | Or specific treatment for this lipid abnormality |
| <40 mg/dL in males; <50 mg/dL in females | |
| Or specific treatment for this lipid abnormality | |
| Raised blood pressure | ≥130/85 mmHg |
| Or treatment of previously identified hypertension | |
| Raised fasting plasma glucose | ≥100 mg/dL |
| Or previously diagnosed T2DM | |
| Asian Americans (n = 2121) | Non-Hispanic Whites (n = 6318) | |
|---|---|---|
| Sociodemographic characteristics mean or % (se) | ||
| BMI, mean | 24.77 (0.11) | 28.84 (0.14) |
| Age, mean | 44.18 (0.69) | 48.98 (0.43) |
| Family income to poverty line ratio (mean) | 3.06 (0.08) | 3.23 (0.07) |
| Sex | ||
| Female | 53.55% (0.01) | 51.35% (0.01) |
| Male | 46.45% (0.01) | 48.65% (0.01) |
| Marital Status | ||
| Currently married | 65.68% (0.02) | 56.73% (0.01) |
| Other | 34.32% (0.02) | 43.27% (0.01) |
| Educational Attainment | ||
| <High school | 13.85% (0.01) | 9.39% (0.01) |
| High school or some college | 34.60% (0.02) | 55.42% (0.01) |
| ≥College | 51.55% (0.02) | 35.19% (0.02) |
| Modifiable lifestyle behaviors mean or % (se) | ||
| Physical Activity | ||
| Sedentary | 24.20% (0.01) | 21.29% (0.01) |
| Insufficient | 44.73% (0.45) | 34.62% (0.01) |
| Moderate | 15.75% (0.16) | 17.00% (0.01) |
| High | 15.12% (0.15) | 27.08% (0.01) |
| Tobacco Use | ||
| Current user | 9.30% (0.01) | 19.33% (0.01) |
| Former or never user | 90.70% (0.01) | 80.67% (0.01) |
| Alcohol Use | ||
| Lifetime abstainer | 31.11% (0.01) | 9.68% (0.01) |
| Former drinker | 10.84% (0.01) | 13.81% (0.01) |
| Non-excessive current drinker | 53.44% (0.02) | 66.77% (0.02) |
| Excessive current drinker | 4.61% (0.01) | 9.75% (0.01) |
| Men, % (95% CI) | Women, % (95% CI) | |||||
|---|---|---|---|---|---|---|
| BMI | <23 (under or Normal Weight) | 23–27.4 (Overweight) | ≥27.5 (Obese) | <23 (under or Normal Weight) | 23–27.4 (Overweight) | ≥ 27.5 (Obese) |
| MetS | 5.32 (2.36–8.29) | 38.23 (34.21–42.25) | 77.68 (72.30–83.07) | 18.61 (14.36–22.85) | 47.82 (41.94–53.71) | 67.73 (59.91–75.55) |
| Central obesity | 6.78 (3.66–9.91) | 53.99 (49.49–58.50) | 97.82 (95.98–99.66) | 35.93 (31.00–40.87) | 88.55 (84.52–92.57) | 99.96 (n/a) |
| Raised triglycerides | 32.85 (26.47–39.24) | 56.96 (53.50–60.42) | 70.35 (64.46–76.24) | 27.82 (23.56–32.08) | 48.22 (42.69–53.75) | 57.24 (49.75–64.74) |
| Reduced HDL cholesterol | 19.72 (14.56–24.88) | 39.27 (35.37–43.17) | 55.12 (48.61–61.63) | 27.26 (22.96–31.56) | 41.22 (36.18–46.27) | 59.46 (50.48–68.44) |
| Raised blood pressure | 31.76 (26.01–37.51) | 35.85 (31.39–40.31) | 56.53 (50.53–62.52) | 30.02 (26.11–33.94) | 33.94 (29.28–38.61) | 40.73 (35.18–46.28) |
| Raised fasting plasma glucose | 49.84 (42.44–57.23) | 59.88 (54.19–65.56) | 72.40 (65.24–79.56) | 33.56 (27.17–39.95) | 41.94 (34.30–49.58) | 60.57 (51.64–69.51) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, L.; Yang, W.J.; Spence, C.B.; Bhimla, A.; Ma, G.X. Lean Yet Unhealthy: Asian American Adults Had Higher Risks for Metabolic Syndrome than Non-Hispanic White Adults with the Same Body Mass Index: Evidence from NHANES 2011–2016. Healthcare 2021, 9, 1518. https://doi.org/10.3390/healthcare9111518
Zhu L, Yang WJ, Spence CB, Bhimla A, Ma GX. Lean Yet Unhealthy: Asian American Adults Had Higher Risks for Metabolic Syndrome than Non-Hispanic White Adults with the Same Body Mass Index: Evidence from NHANES 2011–2016. Healthcare. 2021; 9(11):1518. https://doi.org/10.3390/healthcare9111518
Chicago/Turabian StyleZhu, Lin, Wei J. Yang, Cody B. Spence, Aisha Bhimla, and Grace X. Ma. 2021. "Lean Yet Unhealthy: Asian American Adults Had Higher Risks for Metabolic Syndrome than Non-Hispanic White Adults with the Same Body Mass Index: Evidence from NHANES 2011–2016" Healthcare 9, no. 11: 1518. https://doi.org/10.3390/healthcare9111518
APA StyleZhu, L., Yang, W. J., Spence, C. B., Bhimla, A., & Ma, G. X. (2021). Lean Yet Unhealthy: Asian American Adults Had Higher Risks for Metabolic Syndrome than Non-Hispanic White Adults with the Same Body Mass Index: Evidence from NHANES 2011–2016. Healthcare, 9(11), 1518. https://doi.org/10.3390/healthcare9111518






