Effects of Sling-Based Thoracic Active Exercise on Pain and Function and Quality of Life in Female Patients with Neck Pain: A Randomized Controlled Trial
Abstract
1. Introduction
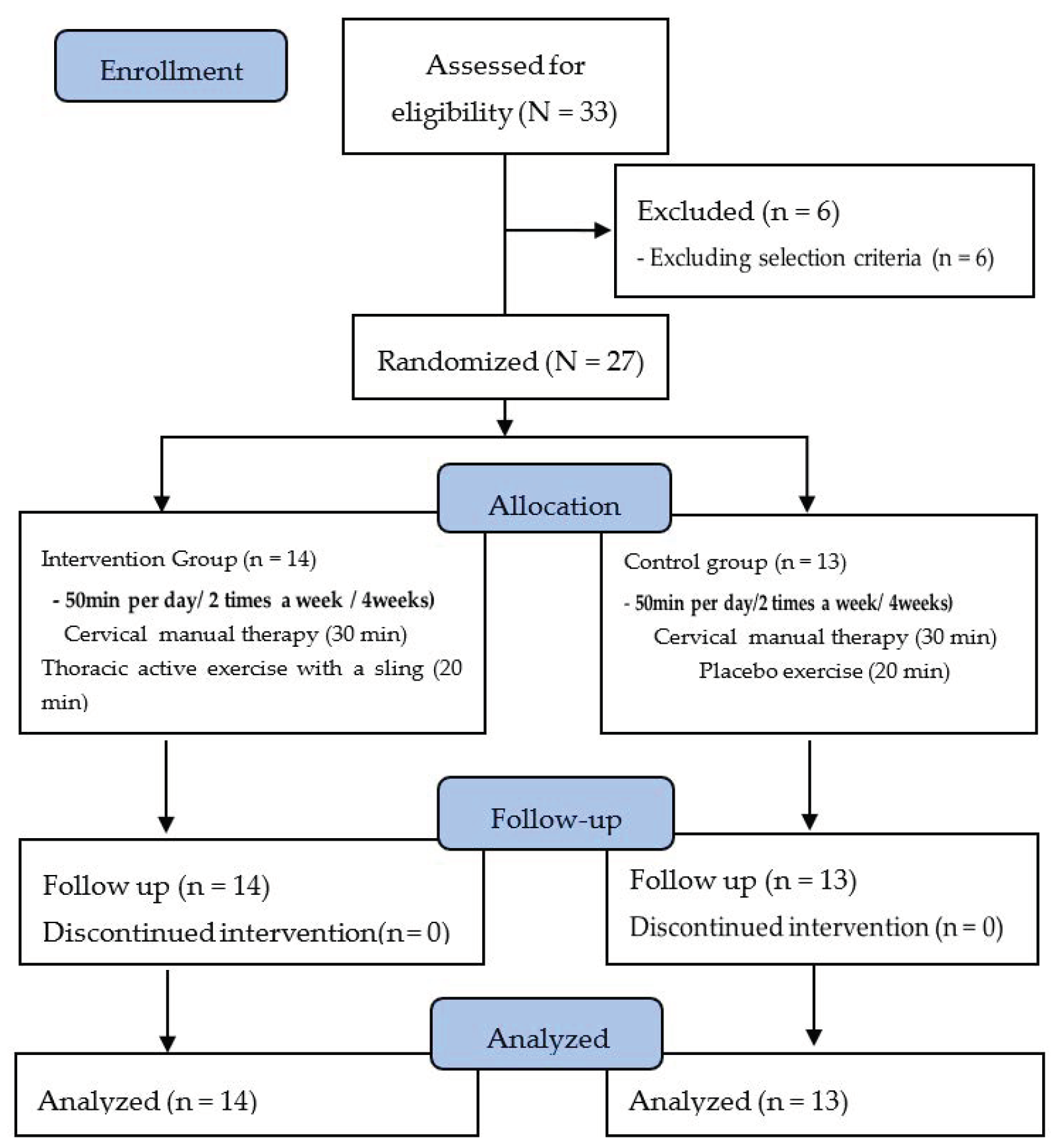
2. Materials and Methods
2.1. Participants
2.2. Experimental Procedures
2.2.1. Thoracic Active Exercise with a Sling
2.2.2. Manual Therapy
2.2.3. Placebo Exercise
2.3. Outcome Measurements
2.4. Statistical Analysis
3. Results
3.1. Pain
3.2. Function
3.3. Quality of Life
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Korea National Statistical Office. Available online: http://www.kostat.go.kr/portal/eng/index.action (accessed on 8 August 2019).
- Falla, D.; Jull, G.; Rusell, T.; Vicenzino, B.; Hodges, P. Effect of neck exercise on sitting posture in patients with chronic neck pain. Phys. Ther. 2007, 87, 408–417. [Google Scholar] [CrossRef] [PubMed]
- Fejer, R.; Kyvik, K.O.; Hartvigsen, J. The prevalence of neck pain in the world population: A systematic critical review of the literature. Eur. Spine J. 2006, 15, 834–848. [Google Scholar] [CrossRef]
- Health Insurance Review & Assessment. Available online: https://www.hira.or.kr/main.do (accessed on 8 August 2020).
- Cleland, J.A.; Flynn, T.W.; Childs, J.D.; Eberhart, S. The audible pop from thoracic spine thrust manipulation and its relation to short-term outcomes in patients with neck pain. J. Man. Manip. Ther. 2007, 15, 143–154. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pernold, G.; Mortimer, M.; Wiktorin, C.; Tornqvist, E.W.; Vingard, E. Musculoskeletal Intervention Center-Norrtaije Study Group. Neck/shoulder disorders in a general population. Natural course and influence of physical exercise: A 5-year follow-up. Spine 2005, 30, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Anderson, V.C.; Carlson, C.; Shatin, D. Outcomes of spinal cord stimulation: Patient validation. Neuromodulation 2001, 4, 11–17. [Google Scholar] [CrossRef]
- Yun, J.H.; Kang, J.M.; Kim, K.S.; Kim, S.H.; Kim, T.H.; Park, Y.W.; Sung, Y.K.; Sohn, J.H.; Song, B.J.; Uhm, W.S.; et al. Health-related quality of life in Korean patients with chronic diseases. J. Korean Rheum. Assoc. 2004, 11, 263–274. [Google Scholar]
- Jo, K.S. Occupational Health, 1st ed.; Soomoonsa: Paju city, Kyunggi-do, Korea, 1991. [Google Scholar]
- Bopp, M.J.; Houston, D.K.; Lenchik, L.; Easter, L.; Kritchevsky, S.B.; Nicklas, B.J. Lean mass loss is associated with low protein intake during dietary-induced weight loss in postmenopausal women. J. Am. Diet. Assoc. 2008, 108, 1216–1220. [Google Scholar] [CrossRef]
- Guss, D.A.; Jacoby, I.J. Longus colli tendinitis causing acute neck pain. J. Emerg. Med. 2002, 22, 211–212. [Google Scholar] [PubMed]
- Taimela, S.; Takala, E.P.; Asklöf, T.; Seppälä, K.; Parviainen, S. Active treatment of chronic neck pain: A prospective randomized intervention. Spine 2000, 25, 1021–1027. [Google Scholar] [CrossRef]
- Viljanen, M.; Malmivaara, A.; Uitti, J.; Rinne, M.; Palmroos, P.; Laippala, P. Effectiveness of dynamic muscle training, relaxation training, or ordinary activity for chronic neck pain: Randomised controlled trial. BMJ 2003, 327, 475. [Google Scholar] [CrossRef] [PubMed]
- Graham, N.; Gross, A.R.; Carlesso, L.C.; Santaguida, P.L.; Macdermid, J.C.; Walton, D.; Ho, E.; ICON. An ICON Overview on Physical Modalities for Neck Pain and Associated Disorders. Open Orthop. J. 2013, 7, 440–460. [Google Scholar] [CrossRef]
- Miller, J.; Gross, A.; D’Sylva, J.; Burnie, S.J.; Goldsmith, C.H.; Graham, N.; Haines, T.; Brønfort, G.; Hoving, J.L. Manual therapy and exercise for neck pain: A systematic review. Man. Ther. 2010, 15, 334–354. [Google Scholar] [CrossRef] [PubMed]
- Vicenzino, B.; Collins, D.; Wright, A. The initial effects of a cervical spine manipulative physiotherapy treatment on the pain and dysfunction of lateral epicondylalgia. Pain 1996, 68, 69–74. [Google Scholar] [CrossRef]
- Blanpied, P.R.; Gross, A.R.; Elliott, J.M.; Devaney, L.L.; Clewley, D.; Walton, D.M.; Sparks, C.; Robertson, E.K. Neck Pain: Revision 2017. J. Orthop. Sports Phys. Ther. 2017, 47, 1–83. [Google Scholar] [CrossRef]
- Lau, H.M.; Wing Chiu, T.T.; Lam, T.H. The effectiveness of thoracic manipulation on patients with chronic mechanical neck pain—A randomized controlled trial. Man. Ther. 2011, 16, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Krauss, J.; Creighton, D.; Ely, J.D.; Podlewska-Ely, J. The immediate effects of upper thoracic translatoric spinal manipulation on cervical pain and range of motion: A randomized clinical trial. J. Man. Manip. Ther. 2008, 16, 93–99. [Google Scholar] [CrossRef]
- Gross, A.R.; Hoving, J.L.; Haines, T.A.; Goldsmith, C.H.; Kay, T.; Aker, P.; Bronfort, G. Cervical overview group, Manipulation and mobilisation for mechanical neck disorders. Cochrane Database Syst. Rev. 2004, 1, CD004249. [Google Scholar]
- Sarig-Bahat, H. Evidence for exercise therapy in mechanical neck disorders. Man. Ther. 2003, 8, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Vikne, J.; Oedegaard, A.; Laerum, E.; Ihlebaek, C.; Kirkesola, G. A randomized study of new sling exercise treatment vs traditional physiotherapy for patients with chronic whiplash-associated disorders with unsettled compensation claims. J. Rehabil. Med. 2007, 39, 252–259. [Google Scholar] [CrossRef][Green Version]
- Harter, R.A. Clinical rationale for closed kinetic chain activities in functional testing and rehabilitation of ankle pathologies. J. Sport Rehabil. 1996, 5, 13–24. [Google Scholar]
- Verhagen, A.P.; Karels, C.; Bierma-Zeinstra, S.M.A.; Feleus, A.; Dahaghin, S.; Burdorf, A.; Koes, B.W. Exercise proves effective in a systematic review of work-related complaints of the arm, neck, or shoulder. J. Clin. Epidemiol. 2007, 60, 110–117. [Google Scholar]
- Chang, W.D.; Huang, W.S.; Lee, C.L.; Lin, H.Y.; Lai, P.T. Effects of open and closed kinetic chains of sling exercise therapy on the muscle activity of the vastus medialis oblique and vastus lateralis. J. Phys. Ther. Sci. 2014, 26, 1363–1366. [Google Scholar] [CrossRef] [PubMed]
- Dannelly, B.D.; Otey, S.C.; Croy, T.; Harrison, B.; Rynders, C.A.; Hertel, J.N.; Weltman, A. The effectiveness of traditional and sling exercise strength training in women. J. Strength Cond. Res. 2011, 25, 464–471. [Google Scholar] [CrossRef]
- Lin, K.Y.; Tsai, Y.J.; Hsu, P.Y.; Tsai, C.S.; Kuo, Y.L. Effects of Sling Exercise for Neck Pain: A Systematic Review and Meta-Analysis. Phys. Ther. 2021, 101, pzab120. [Google Scholar] [CrossRef] [PubMed]
- Halvorsen, F.H. Neurac1 seminer workbook. Redcord AS. Thorac. Mobilization Exerc. Proced. 2014, 3, 5–7. [Google Scholar]
- Ylinen, J.; Kautiainen, H.; Wirén, K.; Häkkinen, A. Stretching exercises vs manual therapy in treatment of chronic neck pain: A randomized, controlled cross-over trial. J. Rehabil. Med. 2007, 39, 126–132. [Google Scholar] [CrossRef]
- Tunks, E.; Crook, J.; Norman, G.; Kalaher, S. Tender points in fibromyalgia. Pain 1988, 34, 11–19. [Google Scholar] [CrossRef]
- Farrar, J.T.; Young, J.P.Y., Jr.; LaMoreaux, L.; Werth, J.L.; Poole, M.R. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001, 94, 149–158. [Google Scholar] [CrossRef]
- Yip, C.H.; Chiu, T.T.; Poon, A.T. The relationship between head posture and severity and disability of patients with neck pain. Man. Ther. 2008, 13, 148–154. [Google Scholar] [CrossRef]
- Raine, S.; Twomey, L.T. Head and shoulder posture variations in 160 asymptomatic women and men. Arch. Phys. Med. Rehabil. 1997, 78, 1215–1223. [Google Scholar] [CrossRef]
- Young, I.A.; Cleland, J.A.; Michener, L.A.; Brown, C. Reliability, construct validity, and responsiveness of the neck disability index, patient-specific functional scale, and numeric pain rating scale in patients with cervical radiculopathy. Am. J. Phys. Med. Rehabil. 2010, 89, 831–839. [Google Scholar] [CrossRef]
- Vernon, H.; Mior, S. The Neck Disability Index: A study of reliability and validity. J. Manip. Physiol. Ther. 1991, 14, 409–415. [Google Scholar]
- Han, C.W.; Lee, E.J.; Iwaya, T.; Kataoka, H.; Kohzuki, M. Development of the Korean version of Short-Form 36-Item Health Survey: Health related QOL of healthy elderly people and elderly patients in Korea. Tohoku J. Exp. Med. 2004, 203, 189–194. [Google Scholar] [PubMed]
- Edmondston, S.J.; Chan, H.Y.; Ngai, G.C.W.; Warren, M.L.R.; Williams, J.M.; Glennon, S.; Netto, K. Postural neck pain: An investigation of habitual sitting posture, perception of ′good″ posture and cervicothoracic kinaesthesia. Man. Ther. 2007, 12, 363–371. [Google Scholar] [CrossRef]
- Norlander, S.; Nordgren, B. Clinical symptoms related to musculoskeletal neck-shoulder pain and mobility in the cervico-thoracic spine. Scand. J. Rehabil. Med. 1998, 30, 243–251. [Google Scholar] [PubMed]
- Celenay, S.T.; Kaya, D.O.; Akbayrak, T. Cervical and scapulothoracic stabilization exercises with and without connective tissue massage for chronic mechanical neck pain: A prospective, randomised controlled trial. Man. Ther. 2016, 21, 144–150. [Google Scholar]
- Masaracchio, M.; Cleland, J.; Hellman, M.; Hagins, M. Short-term combined effects of thoracic spine thrust manipulation and cervical spine nonthrust manipulation in individuals with mechanical neck pain: A randomized clinical trial. J. Orthop. Sports Phys. Ther. 2013, 43, 118–127. [Google Scholar] [CrossRef]
- Kendall, F.P.; McCreary, E.K.; Provance, P.G. Muscle Testing and Function with Posture and Pain, 5th ed.; Lippincott Williams & Wilkins: Philadephia, PA, USA, 2005. [Google Scholar]
- Falla, D.L.; Jull, G.A.; Hodges, P.W. Patients with neck pain demonstrate reduced electromyographic activity of the deep cervical flexor muscles during performance of the craniocervical flexion test. Spine 2004, 29, 2108–2114. [Google Scholar] [CrossRef] [PubMed]
- Harman, K.; Hubley-Kozey, C.L.; Butler, H. Effectiveness of an exercise program to improve forward head posture in normal adults: A randomized, controlled 10-week trial. J. Man. Manip. Ther. 2005, 13, 163–176. [Google Scholar] [CrossRef]
- Yang, L.; Lei, Z.J.; Jiang, J.L.; Zhang, L.M.; He, C.Q. Sichuan da xue xue bao. Yi xue ban. J. Sichuan Univ. 2014, 45, 129–133. [Google Scholar]
- Szeto, G.P.; Straker, L.; Raine, S. A field comparison of neck and shoulder postures in symptomatic and asymptomatic office workers. Appl. Ergon. 2002, 33, 75–84. [Google Scholar] [CrossRef]
- Cho, J.; Lee, E.; Lee, S. Upper thoracic spine mobilization and mobility exercise versus upper cervical spine mobilization and stabilization exercise in individuals with forward head posture: A randomized clinical trial. BMC Musculoskelet. Disord. 2017, 18, 525. [Google Scholar] [CrossRef] [PubMed]
- Wirth, B.; Amstalden, M.; Perk, M.; Boutellier, U.; Humphreys, B.K. Respiratory dysfunction in patients with chronic neck pain—Influence of thoracic spine and chest mobility. Man. Ther. 2014, 19, 440–444. [Google Scholar]
- Garrett, T.R.; Youdas, J.W.; Madson, T.J. Reliability of measuring forward head posture in a clinical setting. J. Orthop. Sports Phys. Ther. 1993, 17, 155–160. [Google Scholar] [CrossRef]
- Arsh, A.; Darain, H.; Iqbal, M.; Rahman, M.U.; Ullah, I.; Khalid, S. Effectiveness of manual therapy to the cervical spine with and without manual therapy to the upper thoracic spine in the management of non-specific neck pain; A randomized controlled trial. J. Pak. Med. Assoc. 2020, 70, 399–403. [Google Scholar] [PubMed]
- Wegner, S.; Jull, G.; O’Leary, S.; Johnston, V. The effect of a scapular postural correction strategy on trapezius activity in patients with neck pain. Man. Ther. 2010, 15, 562–566. [Google Scholar] [CrossRef]
- Mekhora, K.; Liston, C.B.; Nanthavanij, S.; Cole, J.H. The effect of ergonomic intervention on discomfort in computer users with tension neck syndrome. Int. J. Ind. Ergon. 2000, 26, 367–379. [Google Scholar]
- Nicholas, M.K. Mental disorders in people with chronic pain: An international perspective. Pain 2007, 129, 231–232. [Google Scholar] [CrossRef]
- Matcham, F.; Norton, S.; Steer, S.; Hotopf, M. Usefulness of the SF-36 Health Survey in screening for depressive and anxiety disorders in rheumatoid arthritis. BMC Musculoskelet. Disord. 2016, 17, 224. [Google Scholar]
- WHO. Mental Health Aspects of Women’s Reproductive Health: A Global Review of the Literature. 2009. Available online: https://digitallibrary.un.org/record/653457?ln=en (accessed on 18 August 2012).
- Granot, M.; Yarnitsky, D.; Itskovitz-Eldor, J.; Granovsky, Y.; Peer, E.; Zimmer, E.Z. Pain perception in women with dysmenorrhea. Obstet. Gynecol. 2001, 98, 407–411. [Google Scholar]

| Week | Weekly Training | Times |
|---|---|---|
| 1 Week | Flexion-Extension, Lateral Flexion Therapist’s Joint Exercise Guide (Passive Joint Mobilization) | 15 times, 3 set |
| 2 Week | Flexion-Extension, Lateral Flexion Therapist’s Joint Exercise Guide (Passive Joint Mobilization 50%) | |
| 3 Week | Flexion-Extension, Lateral Flexion (Passive Joint Mobilization 30%) | |
| 4 Week | Flexion-Extension, Lateral Flexion (Passive Joint Mobilization 15%) |
| Technique | Manual Therapy | Time |
|---|---|---|
| Passive stretching | periphery of the cervical spine (upper trapezius, pectoralis major, pectoralis minor, etc.) | 5 min |
| Soft tissue relaxation | upper trapezius, suboccipital muscle, cervical flexor, rhomboid muscle, central trapezius, scalenes, sternocleidomastoid muscle, pectoralis major, and pectoralis minor | 15 min |
| Joint mobilization | cervical vertebrae | 5 min |
| Passive stretching | cervical vertebrae (scalenes, nuchal ligament, etc.) | 5 min |
| STAET Group (n = 14) | Control Group (n = 13) | t(p) | |
|---|---|---|---|
| Age(year) | 43.21(7.96) | 46.77(9.10) | −1.082(0.290) |
| Height(cm) | 158.86(3.84) | 159.69(3.54) | −0.586(0.563) |
| Weight(kg) | 57.00(4.00) | 54.15(3.00) | 2.079(0.048) |
| BMI | 22.63(2.07) | 21.28(1.80) | 1.801(0.084) |
| Parameters | STAET Group (n = 14) | Control Group (n = 13) | t(p) | |
|---|---|---|---|---|
| Splenius capitis (Right) | Pre | 19.96(3.95) | 20.04(4.93) | −0.047(0.963) |
| Post | 36.34(5.53) | 31.35(5.89) | ||
| Pre-post | −16.38(5.43) | −11.32(5.32) | −2.447(0.022) * | |
| t(p) | −11.290(0.000) * | −7.665(0.000) * | ||
| Splenius capitis (Left) | Pre | 20.13(4.26) | 19.18(4.48) | 0.561(0.579) |
| Post | 34.86(4.67) | 29.95(5.90) | ||
| Pre-post | −14.73(4.59) | −10.77(4.26) | −2.319(0.029) * | |
| t(p) | −12.014(0.000) * | −9.117(0.000) * | ||
| Upper trapezius (Right) | Pre | 21.59(4.28) | 21.97(6.38) | −0.185(0.855) |
| Post | 37.61(4.51) | 30.56(6.61) | ||
| Pre-post | −16.02(4.63) | −8.59(4.37) | −4.278(0.000) * | |
| t(p) | −12.939(0.000) * | −7.090(0.000) * | ||
| Upper trapezius (Left) | Pre | 19.34(5.14) | 21.00(3.53) | 0.968(0.342) |
| Post | 36.79(5.46) | 29.75(4.47) | ||
| Pre-post | −17.45(4.39) | −8.75(4.73) | −4.958(0.000) * | |
| t(p) | −14.881(0.000) * | −6.676(0.000) * | ||
| Middle trapezius (Right) | Pre | 23.68(6.29) | 28.64(7.11) | −1.9220.066) |
| Post | 43.65(8.05) | 33.52(7.25) | ||
| Pre-post | −19.97(8.63) | −4.88(3.56) | −6.012(0.000) * | |
| t(p) | −8.658(0.000) * | −4.5943(0.000) * | ||
| Middle trapezius (Left) | Pre | 23.81(5.55) | 28.27(5.26) | −2.137(0.043) |
| Post | 42.96(6.46) | 33.06(5.64) | ||
| Pre-post | −19.14(6.71) | −4.79(3.65) | −6.82(0.000) * | |
| t(p) | −10.676(0.000) * | −4.736(0.000) * | ||
| Parameters | STAET Group (n = 14) | Control Group (n = 13) | t(p) | |
|---|---|---|---|---|
| NPRS (Point) | Pre | 7.64(0.84) | 7.38(1.04) | 0.710(0.484) |
| Post | 3.43(0.76) | 4.08(0.76) | ||
| Pre-post | 4.21(1.12) | 3.31(1.25) | 1.986(0.058) | |
| t(p) | 14.057(0.000) * | 9.536(0.000) * | ||
| Parameters | STAET Group (n = 14) | Control Group (n = 13) | t(p) | |
|---|---|---|---|---|
| CVA (°) | Pre | 59.84(3.00) | 59.19(2.17) | −0.639(0.529) |
| Post | 63.16(2.42) | 60.03(2.06) | ||
| Pre-post | −3.31(1.08) | −0.84(0.77) | −8.088(0.000) * | |
| t(p) | −11.492(0.000) * | −3.919(0.002) | ||
| NDI (Point) | Pre | 17.50(2.93) | 16.62(3.15) | 0.6754(0.458) |
| Post | 9.57(1.65) | 12.15(2.15) | ||
| Pre-post | 7.93(2.30) | 4.46(1.81) | 4.328(0.000) * | |
| t(p) | 12.883(0.000) * | 8.897(0.000) * | ||
| Parameters | STAET Group (n = 14) | Control Group (n =13) | t(p) | |
|---|---|---|---|---|
| PCS (Point) | Pre | 40.22(12.13) | 48.65(11.61) | −1.845(0.077) |
| Post | 70.37(11.45) | 57.79(12.57) | ||
| Pre-post | −30.15(12.46) | −9.13(5.53) | −5.732(0.000) * | |
| t(p) | −9.055(0.000) * | −5.957(0.000) * | ||
| MCS (Point) | Pre | 43.12(10.99) | 50.32(11.36) | −1.674(0.107) |
| Post | 67.46(9.73) | 56.44(14.23) | ||
| Pre-post | −24.34(8.43) | −6.12(6.42) | −6.284(0.000) * | |
| t(p) | −10.810(0.000) * | −3.440(0.005) | ||
| GH (Point) | Pre | 41.67(10.37) | 49.49(10.41) | −1.953(0.062) |
| Post | 68.92(7.01) | 57.11(12.73) | ||
| Pre-post | −27.25(7.75) | −7.63(4.93) | −7.779(0.000) * | |
| t(p) | −13.156(0.000) * | −5.582(0.000) * | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, G.-W.; An, J.; Kim, S.-W.; Lee, B.-H. Effects of Sling-Based Thoracic Active Exercise on Pain and Function and Quality of Life in Female Patients with Neck Pain: A Randomized Controlled Trial. Healthcare 2021, 9, 1514. https://doi.org/10.3390/healthcare9111514
Park G-W, An J, Kim S-W, Lee B-H. Effects of Sling-Based Thoracic Active Exercise on Pain and Function and Quality of Life in Female Patients with Neck Pain: A Randomized Controlled Trial. Healthcare. 2021; 9(11):1514. https://doi.org/10.3390/healthcare9111514
Chicago/Turabian StylePark, Gun-Woo, Jungae An, Sang-Woo Kim, and Byoung-Hee Lee. 2021. "Effects of Sling-Based Thoracic Active Exercise on Pain and Function and Quality of Life in Female Patients with Neck Pain: A Randomized Controlled Trial" Healthcare 9, no. 11: 1514. https://doi.org/10.3390/healthcare9111514
APA StylePark, G.-W., An, J., Kim, S.-W., & Lee, B.-H. (2021). Effects of Sling-Based Thoracic Active Exercise on Pain and Function and Quality of Life in Female Patients with Neck Pain: A Randomized Controlled Trial. Healthcare, 9(11), 1514. https://doi.org/10.3390/healthcare9111514







