Electroacupuncture for Temporomandibular Disorders: A Systematic Review of Randomized Controlled Trials
Abstract
:1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Data Sources and Searches
2.3. Study Selection
2.3.1. Types of Studies
2.3.2. Participants
2.3.3. Types of Interventions
2.3.4. Types of Comparisons
2.3.5. Types of Outcome Measures
2.4. Data Extraction
2.5. Assessment of Risk of Bias (ROB)
2.6. Data Analyses
3. Results
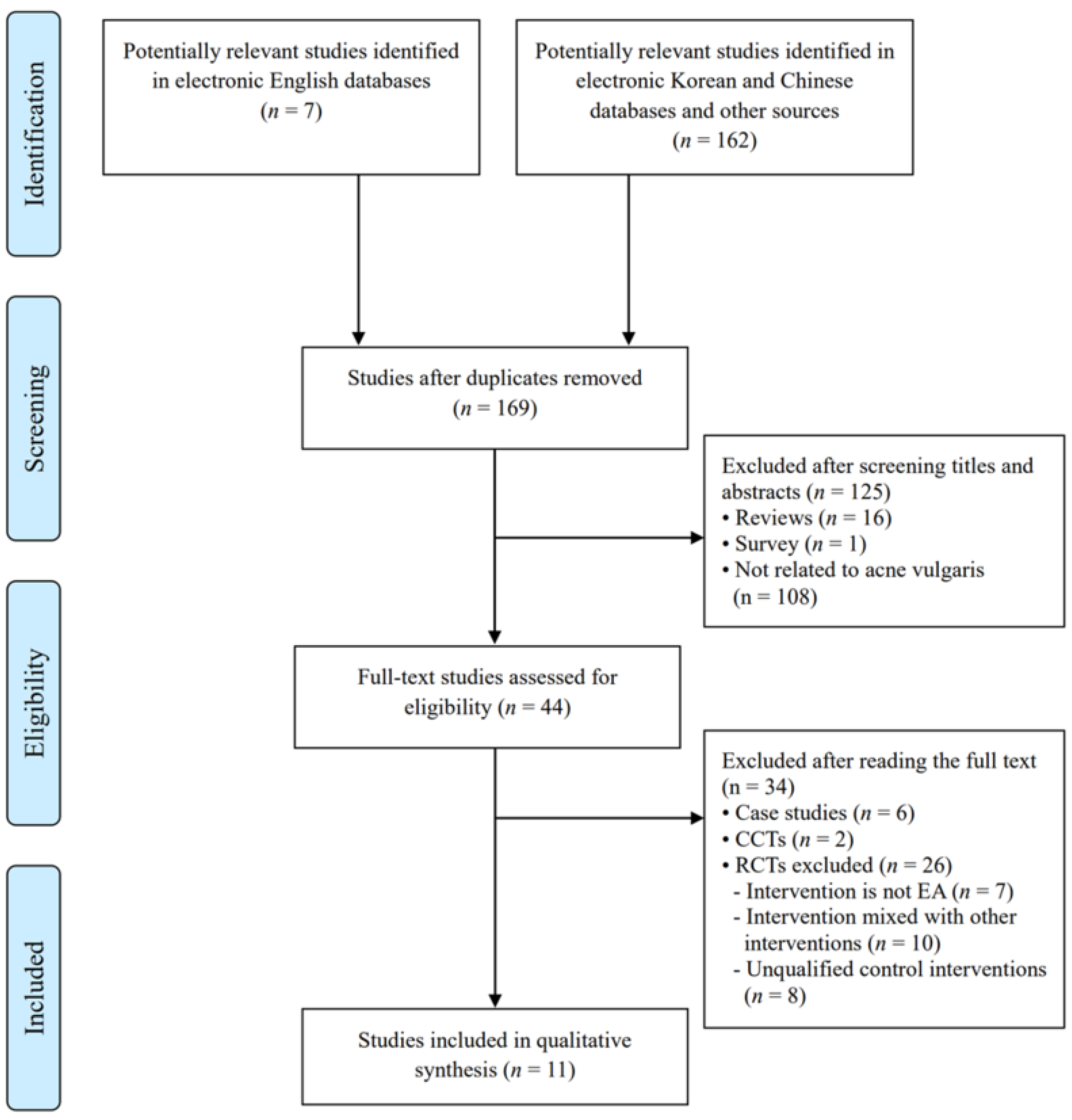
3.1. Study Selection and Description
3.2. Participants
3.3. Intervention
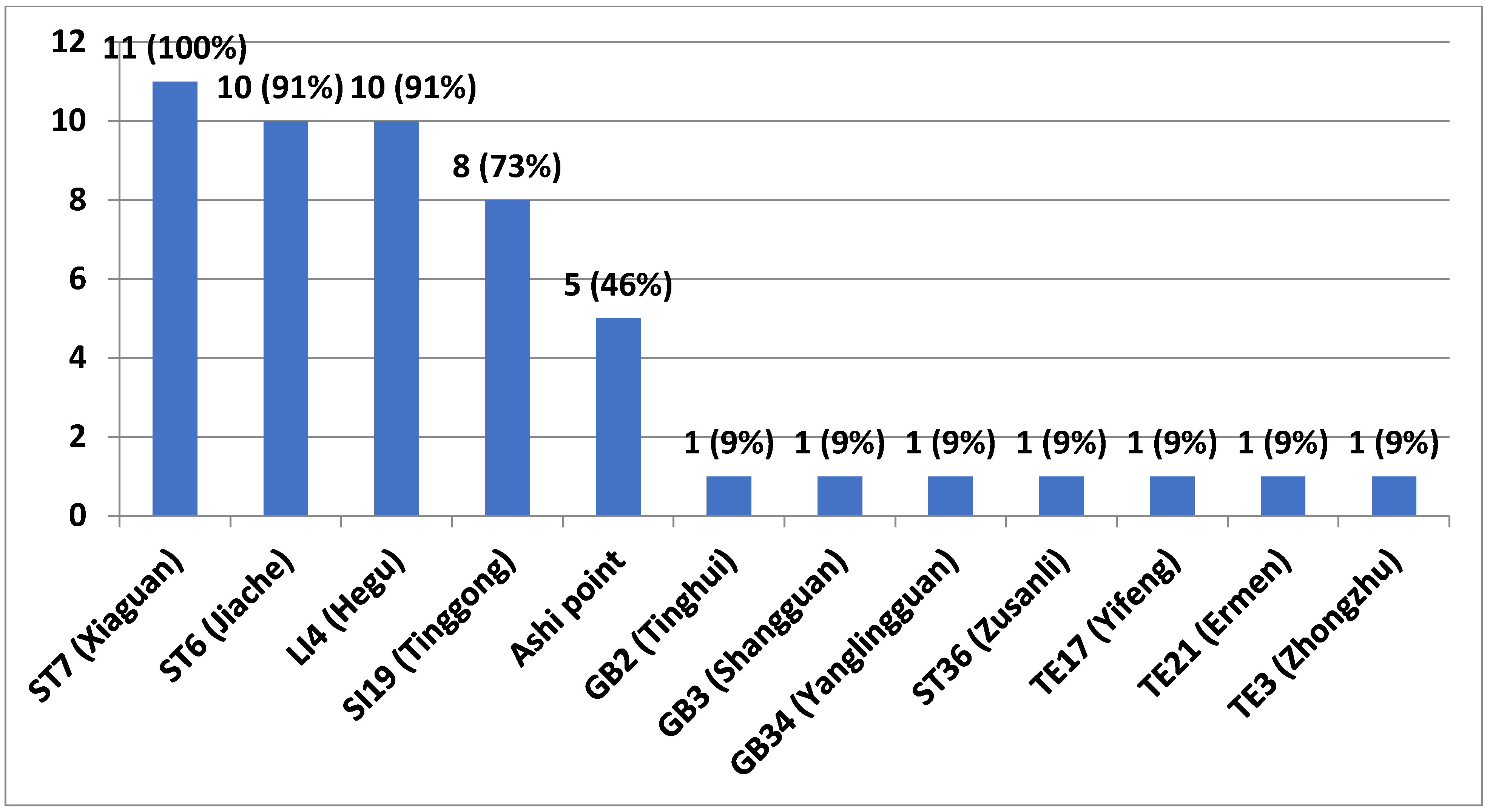
3.3.1. EA Points
3.3.2. Needle Type (Diameter, Length)
3.3.3. Depth of Insertion
3.3.4. Angle of Insertion
3.3.5. Needle Retention Time
3.3.6. Frequency of Electric Stimulation
3.4. Outcomes
3.4.1. EA versus Block Therapy
3.4.2. EA versus EA plus Microwave
3.4.3. EA plus Ultrashort Wave versus Ultrashort Wave Only
3.4.4. EA versus EA plus Ultrashort Wave
3.4.5. EA versus Physiotherapy
3.4.6. EA versus EA plus Massage Therapy
3.4.7. EA versus Acupuncture
3.4.8. EA versus EA plus Extracorporeal Shock Wave
3.5. Adverse Events
3.6. Assessment for ROB
3.7. Publication Bias
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wadhwa, S.; Kapila, S. TMJ disorders: Future innovations in diagnostics and therapeutics. J. Dent. Educ. 2008, 72, 930–947. [Google Scholar] [CrossRef] [PubMed]
- Ouanounou, A.; Goldberg, M.; Haas, D.A. Pharmacotherapy in temporomandibular disorders: A review. J. Can. Dent. 2017, 83, h7. [Google Scholar]
- Graff-Radford, S.B.; Abbott, J.J. Temporomandibular disorders and headache. Oral. Maxillofac. Surg. Clin. N. Am. 2016, 28, 335–349. [Google Scholar] [CrossRef]
- Dym, H.; Israel, H. Diagnosis and treatment of temporomandibular disorders. Dent. Clin. N. Am. 2012, 56, 149–161. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R. Executive summary of the diagnostic criteria for temporomandibular disorder(DC/TMD) for clinical and research applications. J. Am. Dent Assoc. 2016, 147, 438–445. [Google Scholar] [CrossRef] [Green Version]
- Tanaka, E.; Detamore, M.S.; Mercuri, L.G. Degenerative disorders of the temporomandibular joint: Etiology, diagnosis, and treatment. J. Dent. Res. 2008, 87, 296–307. [Google Scholar] [CrossRef]
- Kalladka, M.; Quek, S.; Heir, G.; Eliav, E.; Mupparapu, M.; Viswanath, A. Temporomandibular joint osteoarthritis: Diagnosis and long-term conservative management: A topic review. J. Indian Prosthodont. Soc. 2014, 14, 6–15. [Google Scholar] [CrossRef]
- Joseph, R.; Rahena, A.; Hassan, N.; Hilton, G.; Wickham, J.; Ibaragi, S. Epidemiology of temporomandibular disorder in the general population: A systematic review. Adv. Dent. Oral. Health 2019, 10, 1–13. [Google Scholar]
- Gonçalves, D.A.; Dal Fabbro, A.L.; Campos, J.A.; Bigal, M.; Speciali, J.G. Symptoms of temporomandibular disorders in the population: An epidemiological study. J. Orofac. Pain 2010, 24, 270–278. [Google Scholar] [PubMed]
- Dalewski, B.; Kaminska, A.; Bialkowska, K.; Jakubowska, A.; Sobolewska, E. Association of estrogen receptor 1 and tumor necrosis factor α polymorphisms with temporomandibular joint anterior disc displacement without reduction. Dis. Markers 2020, 2020, 6351817. [Google Scholar] [CrossRef] [PubMed]
- Harper, D.E.; Schrepf, A.; Clauw, D.J. Pain mechanisms and centralized pain in temporomandibular disorders. J. Dent. Res. 2016, 95, 1102–1108. [Google Scholar] [CrossRef] [Green Version]
- Gauer, R.L.; Semidey, M.J. Diagnosis and treatment of temporomandibular disorders. Am. Fam. Physician 2015, 91, 378–386. [Google Scholar] [PubMed]
- Dalewski, B.; Kaminska, A.; Szydlowski, M.; Kozak, M.; Sobolewska, E. Comparison of early effectiveness of three different intervention methods in patients with chronic orofacial pain: A randomized controlled clinical trial. Pain Res. Manag. 2019, 2019, 7954291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Durham, J.; Newton-John, T.R.O.; Zakrzewska, J.M. Temporomandibular disorders. BMJ 2015, 350, h1154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raphael, K.G.; Klausner, J.J.; Nayak, S.; Marbach, J.J. Complementary and alternative therapy use by patients with fascial temporomandibular disorders. J. Orofac. Pain 2003, 17, 36–41. [Google Scholar]
- DeBar, L.L.; Vuckovic, N.; Schneider, J.; Ritenbaugh, C. Use of complementary and alternative medicine for temporomandibular disorders. J. Orofac. Pain 2003, 17, 224–236. [Google Scholar]
- Fernandes, A.C.; Duarte Moura, D.M.; Da Silva, L.G.D.; De Almeida, E.O.; Barbosa, G.A.S. Acupuncture in temporomandibular disorder myofascial pain treatment: A systematic review. J. Oral. Facial. Pain Headache 2017, 31, 225–232. [Google Scholar] [CrossRef]
- Vier, C.; Almeida, M.B.; Neves, M.L.; dos Santos, A.R.S.; Bracht, M.A. The effectiveness of dry needling for patients with orofacial pain associated with temporomandibular dysfunction: A systematic review and meta-analysis. Braz. J. Phys. Ther. 2019, 23, 3–11. [Google Scholar] [CrossRef]
- Wu, J.Y.; Zhang, C.; Xu, Y.P.; Yu, Y.Y.; Peng, L.; Leng, W.D.; Niu, Y.M.; Deng, M.H. Acupuncture therapy in the management of the clinical outcomes for temporomandibular disorders: A PRISMA-compliant meta-analysis. Medicine 2017, 96, e6064. [Google Scholar] [CrossRef]
- Noordergraaf, A.; Silage, D. Electroacupuncture. IEEE Trans. Biomed. Eng. 1973, 20, 364–366. [Google Scholar] [CrossRef]
- Chassot, M.; Dussan-Sarria, J.A.; Sehn, F.C.; Deitos, A.; de Souza, A.; Vercelino, R.; Torres, I.L.C.; Fregni, F.; Caumo, W. Electroacupuncture analgesia is associated with increased serum brain-derived neurotrophic factor in chronic tension-type headache: A randomized, sham controlled, crossover trial. BMC Complement. Altern. Med. 2015, 15, 144. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V.; Flemyng, E. Cochrane Handbook for Systematic Reviews of Interventions; version 6.1 (updated September 2020). Cochrane. 2020. Available online: www.training.cochrane.org/handbook (accessed on 11 June 2021).
- Liu, M. 62 cases of temporomandibular joint syndrome treated with super short wave combined with electric needle and ultrashort wave. Shanghai J. Acupunct. Moxibustion 2007, 26, 27. [Google Scholar]
- Wang, D.; Kap, S.; Hu, Q. Comparative analysis on the effect of electric needle and local seal method in disorder of mouth joints. Hebei Med. J. 2009, 31, 2496–2497. [Google Scholar]
- Jia, N. Twenty-one patients with jaw joint disorder were treated by electric needle combined with microwave. J. Tradit. Chin. Med. 2010, 42, 49–50. [Google Scholar]
- Liu, Y.; Guan, Y.; Zhang, L. Twenty-six patients with temporal and maxillary joint disorders treated by combined audio super short wave TDP. Aerosp. Med. 2010, 21, 933. [Google Scholar]
- Bu, L.X.; Chen, T.; Chen, X.; Jing, H.; Li, N.Y. Clinical observation of acupuncture and massage therapy for temporomandibular joint disorders. Shanghai Kou Qiang Yi Xue 2011, 20, 292–295. [Google Scholar] [PubMed]
- Li, Y.; Ho, Y.L. Analysis on the effect of closed treatment for the function disorder of temporomandibular joints. China Foreign Med. Treat. 2011, 31, 91. [Google Scholar]
- Chen, C.Y. Treatment of 32 cases of temporomandibular joint disorder with electric needle combined with microwave. Chin. Community Dr. 2012, 14, 211–212. [Google Scholar]
- Zhang, D.; Yu, X. Treatment of temporomandibular joint dysfunction syndrome by electroacupuncture. Hebei J. TCM 2014, 36, 399–400. [Google Scholar]
- Han, P.J.; Guo, K.F.; Sun, L.; Gao, Y. Effect of electroacupuncture combined external shock wave in treatment of temporomandibular joint disorder syndrome. Chin. Manip. Rehabil. Med. 2018, 9, 26–28. [Google Scholar]
- Hu, Y. Treatment of temporal and maxillary joint disorders by electro-needle combined with ultrashort. Tradit. Chin. Med. Res. 2018, 31, 47–49. [Google Scholar]
- Ye, H. Effect of ultrashort wave combined with electric needle in the treatment of temporomandibular joint disorder. J. Clin. Med. 2019, 6, 76–78. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hwang, J.H.; Jung, H.W. TA pharmacopuncture as a primary and independent treatment for frequent sprains occurring over 9 months in a patient with needle sickness. Medicine 2018, 97, e13123. [Google Scholar] [CrossRef]
- Hu, W.L.; Chang, C.H.; Hung, Y.C.; Tseng, Y.J.; Hung, I.L.; Hsu, S.F. Laser acupuncture therapy in patients with treatment-resistant temporomandibular disorders. PLoS ONE 2014, 9, e110528. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Q.B.; Zhou, Y.; Zhong, H.Z.; Liu, Y. Effect of stretching combined with ultrashort wave diathermy on joint function and its possible mechanism in a rabbit knee contracture model. Am. J. Phys. Med. Rehabil. 2018, 97, 357–363. [Google Scholar] [CrossRef]
- Tengfei, F.; William, C.L.; Feng, Z.; Zhang, J. Role of shortwave and microwave diathermy in peripheral neuropathy. J. Int. Med. Res. 2019, 47, 3569–3579. [Google Scholar]
- Nelson, N.L.; Churilla, J.R. Massage therapy for pain and function in patients with arthritis: A systematic review of randomized controlled trials. Am. J. Phys. Med. Rehabil. 2017, 96, 665–672. [Google Scholar] [CrossRef]
- Wang, C.J. Extracorporeal shockwave therapy in musculoskeletal disorders. J. Orthop. Surg. Res. 2012, 8, 11. [Google Scholar] [CrossRef] [Green Version]
- France, S.; Bown, J.; Nowosilskyj, M.; Mott, M.; Rand, S.; Walters, J.L. Evidence for the use of dry needling and physiotherapy in the management of cervicogenic or tension-type headache: A systematic review. Cephalalgia 2014, 34, 994–1003. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, L.A.; de Oliveira, R.G.; Guimarães, J.P.; Carvalho, A.C.P.; De Paula, M.V.Q. Laser acupuncture in patients with temporomandibular dysfunction: A randomized controlled trial. Lasers Med. Sci. 2013, 28, 1549–1558. [Google Scholar] [CrossRef]
- Rosted, P. Practical recommendations for the use of acupuncture in the treatment of temporomandibular disorders based on the outcome of published controlled studies. Oral. Dis. 2001, 7, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.M.; Kain, Z.N.; White, P. Acupuncture analgesia: I. The scientific basis. Anesth. Analg. 2008, 106, 602–610. [Google Scholar] [CrossRef] [PubMed]
- Cantwell, S.L. Traditional Chinese veterinary medicine: The mechanism and management of acupuncture for chronic pain. Top. Companion Anim. Med. 2010, 25, 53–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MacPherson, H.; Altman, D.G.; Hammerschlag, R.; Li, Y.; Wu, Y.; White, A.; Moher, D. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): Extending the CONSORT statement. PLoS Med. 2010, 7, e1000261. [Google Scholar] [CrossRef] [Green Version]
- Petticrew, M.; Roberts, H. Systematic Reviews in the Social Sciences: A Practical Guide; Blackwell Publishing: Malden, MA, USA, 2006. [Google Scholar]

| Author, Year | Sample Size (m/f) | Experimental Group (No. of Participants Analyzed/Randomized) | Control Group (No. of Participants Analyzed/Randomized) | Outcome Measures | Main Results | AE |
|---|---|---|---|---|---|---|
| Liu (2007) [24] | 62 (11/51) | EA (31/31) | EA + Ultrashort wave a1 (31/31) | TER for TMD | Negative i | n.r. |
| Wang (2009) [25] | 96 (46/50) | EA (48/48) | Block therapy (38/48) b1 | TER for TMD | Positive h | n.r. |
| Jia (2010) [26] | 35 (15/20) | EA (14/14) | EA + Microwave (21/21) c1 | TER for TMD | Negative h | n.r. |
| Liu (2010) [27] | 51 (28/23) | EA (26/26) | Physiotherapy (25/25) d | TER for TMD | Negative i | n.r. |
| Bu(2011) [28] | 96 (30/66) | EA (48/48) | EA + Massage therapy (48/48) e | (1) TER for TMD | (1) Negative h | n.r. |
| (2) TER for myofascial pain | (2) Negative h | |||||
| (3) TER for external pterygoid muscle spasm | (3) Negative h | |||||
| Li (2011) [29] | 54 (12/42) | EA (27/27) | Block therapy (27/27) b2 | TER for TMD | Negative h | n.r. |
| Chen (2012) [30] | 64 (25/39) | EA (32/32) | EA + Microwave (32/32) c2 | TER for TMD | Negative h | n.r. |
| Zhang (2014) [31] | 60 (26/34) | EA (30/30) | Acupuncture (30/30) f | (1) VAS | (1) Positive h | n.r |
| (2) TER for TMD | (2) Positive h | |||||
| Han (2018) [32] | 40 (23/17) | EA (20/20) | EA+ Extracorporeal Shock Wave (20/20) g | (1) VAS | (1) Negative h | n.r. |
| (2) TER for TMD | (2) Negative h | |||||
| (3) Maximum opening degree | (3) Negative h | |||||
| (4) Fricton’s TMJ Dysfunction Index | (4) Negative h | |||||
| Hu (2018) [33] | 69 (28/41) | EA + Ultrashort wave (35/35) | Ultrashort wave (34/34) a2 | (1) TER for TMD | (1) Positive h | n.r. |
| (2) Relapse rate (after 3 months) | (2) Positive h | |||||
| Ye (2019) [34] | 40 (19/21) | EA + Ultrashort wave (20/20) | Ultrashort wave (20/20) a3 | (1) VAS | (1) Positive i | n.r. |
| (2) Painless opening degree | (2) Positive i |
| Author, Year | Regimen | Acupuncture Points | Type of Needle (Diameter, Length) | Depth of Insertion | Angle of Insertion | Needle Retention Time | Frequency of Electric Stimulation | Co-Interventions |
|---|---|---|---|---|---|---|---|---|
| Liu (2007) [24] | 20 sessions (20 days) | ST7, ST6, SI19, LI4 | 0.35 mm, 40 mm | n.r. | 90° | 30 min | 2 Hz | Ultrashort wave |
| Wang (2009) [25] | 14 sessions (14 days) | ST7, ST6, LI4, Ashi point * | 0.25 mm, 40 mm | n.r. | n.r. | 30 min | n.r | None |
| Jia (2010) [26] | 10 sessions (once a day for 10 days) | ST7, ST6, LI4, Ashi point * | 0.25 mm, 40 mm | ST7: 25–30 mm Etc: n.r. | ST7: 90° Etc: n.r. | 30 min | 50 Hz | Microwave |
| Liu (2010) [27] | 10 sessions (10 days) | LI4, ST7, ST6, SI19 | n.r., 40 mm | n.r. | n.r. | 15–20 min | n.r. | None |
| Bu(2011) [28] | 40 sessions (40 days) | GB3, ST7, ST6, SI19, LI4 | 0.32 mm, 40 mm | n.r. | n.r. | 20 min | 1.2 Hz | Massage therapy |
| Li (2011) [29] | 5 sessions (every other day for 10 days) | TE21, ST6, ST7, LI4, GB2, SI19 | n.r., 40 mm | 0.5–1.5 inch | n.r. | 20 min | n.r. | None |
| Chen (2012) [30] | 10 sessions (10 days) | ST7, ST6, LI4, Ashi point * | 0.25 mm, 40 mm | ST7: 25–30 mm Etc: n.r. | ST7: 90° Etc: n.r. | 30 min | 50 Hz | Microwave |
| Zhang (2014) [31] | 20 sessions (once a day for 20 days) | TE3, ST7, SI19 | 0.30 mm, 25 mm | ST7, SI19 | n.r | 20 min | 20 Hz | None |
| Han (2018) [32] | 10 sessions (5 times a week for 2 wks) | SI19, ST7, ST6, LI4, Ashi point | 0.32 mm, 40 mm | n.r. | n.r. | 30 min | 1.2 Hz | Extra corporeal Shock Wave |
| Hu (2018) [33] | 14 sessions (14 days) | SI19, TE17, ST7, ST6, LI4, GB34, Ashi point * | 0.25 mm, 25 mm/40 mm | n.r. | n.r. | 30 min | 1.45 Hz | Ultrashort wave |
| Ye (2019) [34] | 10 sessions (5 times a week for 2 wks) | SI19, ST7, ST6, LI4, ST36 | 0.25 × 25 mm | n.r. | n.r. | 30 min | Low frequency | Ultrashort wave |
| Author, Year | Scale of TER | Symptoms Included in the TER Evaluation | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pain | Discomfort | Tenderness | Functional Activity | Opening Disorder | Mastication Disorder | Clicking with Function | Recurrence | ||
| Liu (2007) [24] | 3-point scale | o | x | x | x | o | x | o | x |
| Liu (2010) [27] | 3-point scale | o | x | x | x | o | x | o | x |
| Wang (2009) [25] | 3-point scale | o | x | x | x | o | x | x | o |
| Jia (2010) [26] | 5-point scale | x | x | o | o | o | o | o | x |
| Hu (2018) [32] | 5-point scale | x | x | o | o | o | o | o | x |
| Bu(2011) [28] | 4-point scale | o | x | o | x | o | x | x | o |
| Li (2011) [29] | 5-point scale | o | o | x | x | o | x | o | o |
| Chen (2012) [30] | 5-point scale | x | x | o | o | o | o | o | x |
| Zhang (2014) [31] | 3-point scale | o | x | o | x | o | x | x | x |
| Han (2018) [32] | 5-point scale | o | x | o | x | o | o | o | x |
| First Author, Year | Selection Bias | Performance Bias | Detection Bias | Attrition Bias | Reporting Bias | |
|---|---|---|---|---|---|---|
| Random Sequence Generation | Allocation Concealment | Blinding of Participants | Blinding of Outcome Assessment | Incomplete Outcome Data | Selective Reporting | |
| Liu (2007) [24] | H | U | H | L | L | U |
| Wang (2009) [25] | U | U | H | U | L | U |
| Jia (2010) [26] | U | U | H | U | L | U |
| Liu (2010) [27] | U | U | H | U | L | U |
| Bu (2011) [28] | U | U | H | U | L | U |
| Li (2011) [29] | U | U | H | U | L | U |
| Chen (2012) [30] | U | U | H | U | L | U |
| Zhang (2014) [31] | U | U | H | U | L | U |
| Han (2018) [32] | U | U | H | U | L | U |
| Hu (2018) [33] | L | U | H | U | L | U |
| Ye (2019) [34] | H | U | H | U | L | U |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sung, S.-H.; Kim, D.; Park, M.; Hwang, S.-I.; Yoon, Y.-J.; Park, J.-K.; Sung, H.-K. Electroacupuncture for Temporomandibular Disorders: A Systematic Review of Randomized Controlled Trials. Healthcare 2021, 9, 1497. https://doi.org/10.3390/healthcare9111497
Sung S-H, Kim D, Park M, Hwang S-I, Yoon Y-J, Park J-K, Sung H-K. Electroacupuncture for Temporomandibular Disorders: A Systematic Review of Randomized Controlled Trials. Healthcare. 2021; 9(11):1497. https://doi.org/10.3390/healthcare9111497
Chicago/Turabian StyleSung, Soo-Hyun, Dongsu Kim, Minjung Park, Su-In Hwang, Young-Jin Yoon, Jang-Kyung Park, and Hyun-Kyung Sung. 2021. "Electroacupuncture for Temporomandibular Disorders: A Systematic Review of Randomized Controlled Trials" Healthcare 9, no. 11: 1497. https://doi.org/10.3390/healthcare9111497
APA StyleSung, S.-H., Kim, D., Park, M., Hwang, S.-I., Yoon, Y.-J., Park, J.-K., & Sung, H.-K. (2021). Electroacupuncture for Temporomandibular Disorders: A Systematic Review of Randomized Controlled Trials. Healthcare, 9(11), 1497. https://doi.org/10.3390/healthcare9111497






