Role of Equanimity on the Mediation Model of Neuroticism, Perceived Stress and Depressive Symptoms
Abstract
1. Introduction
2. Materials and Methods
Study Population and Procedure
3. Measurements
3.1. 10-Item Perceived Stress Scale (PSS-10)
3.2. Neuroticism Inventory (NI)
3.3. Core Symptom Index (CSI)
3.4. Equanimity Scale (SBI-E)
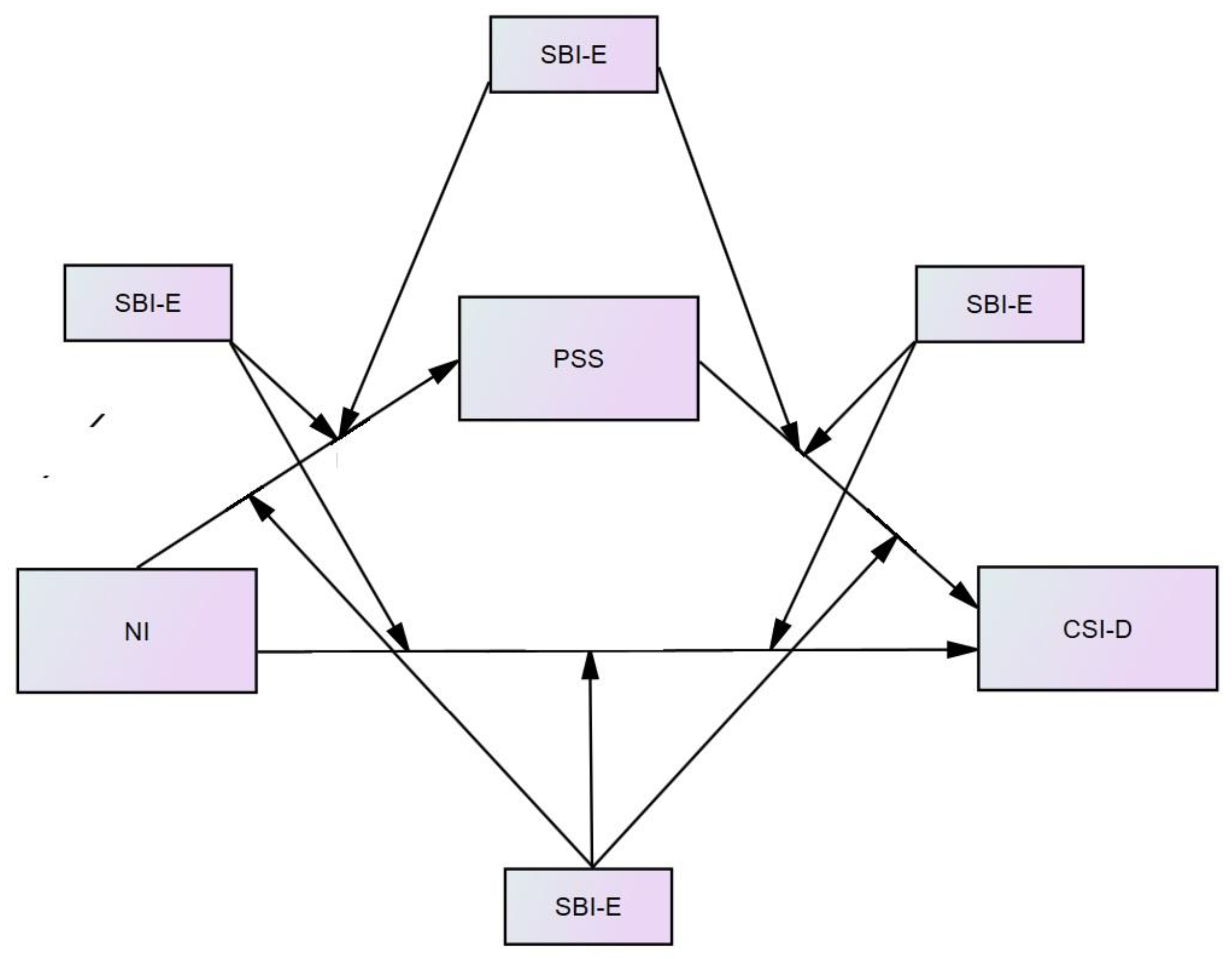
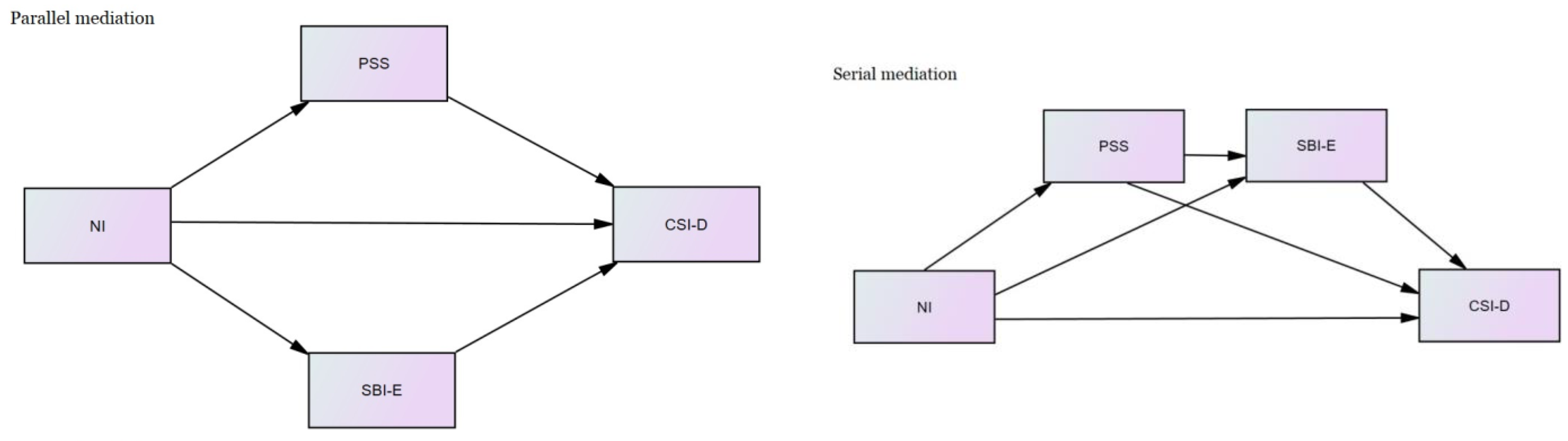
4. Statistical Analysis
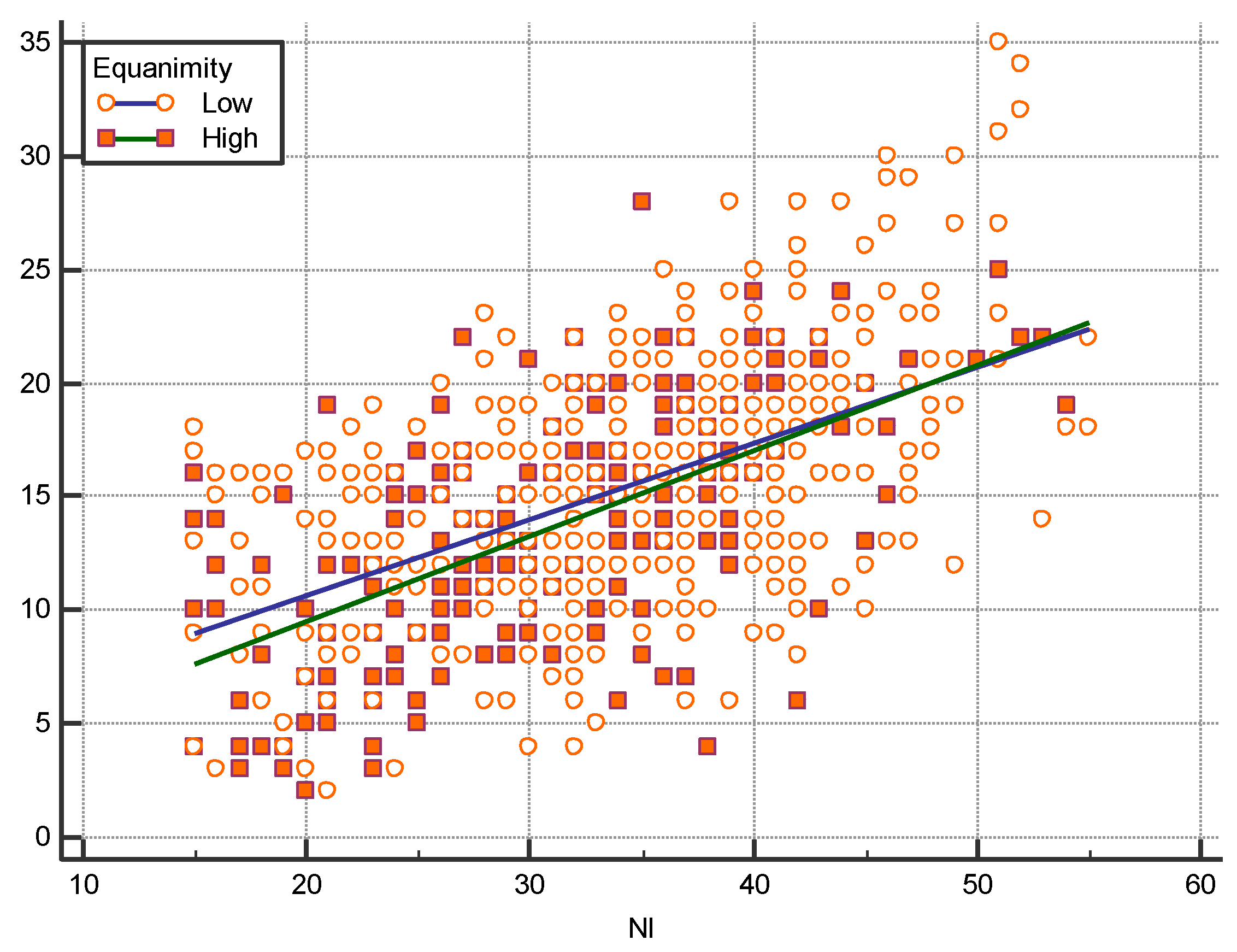
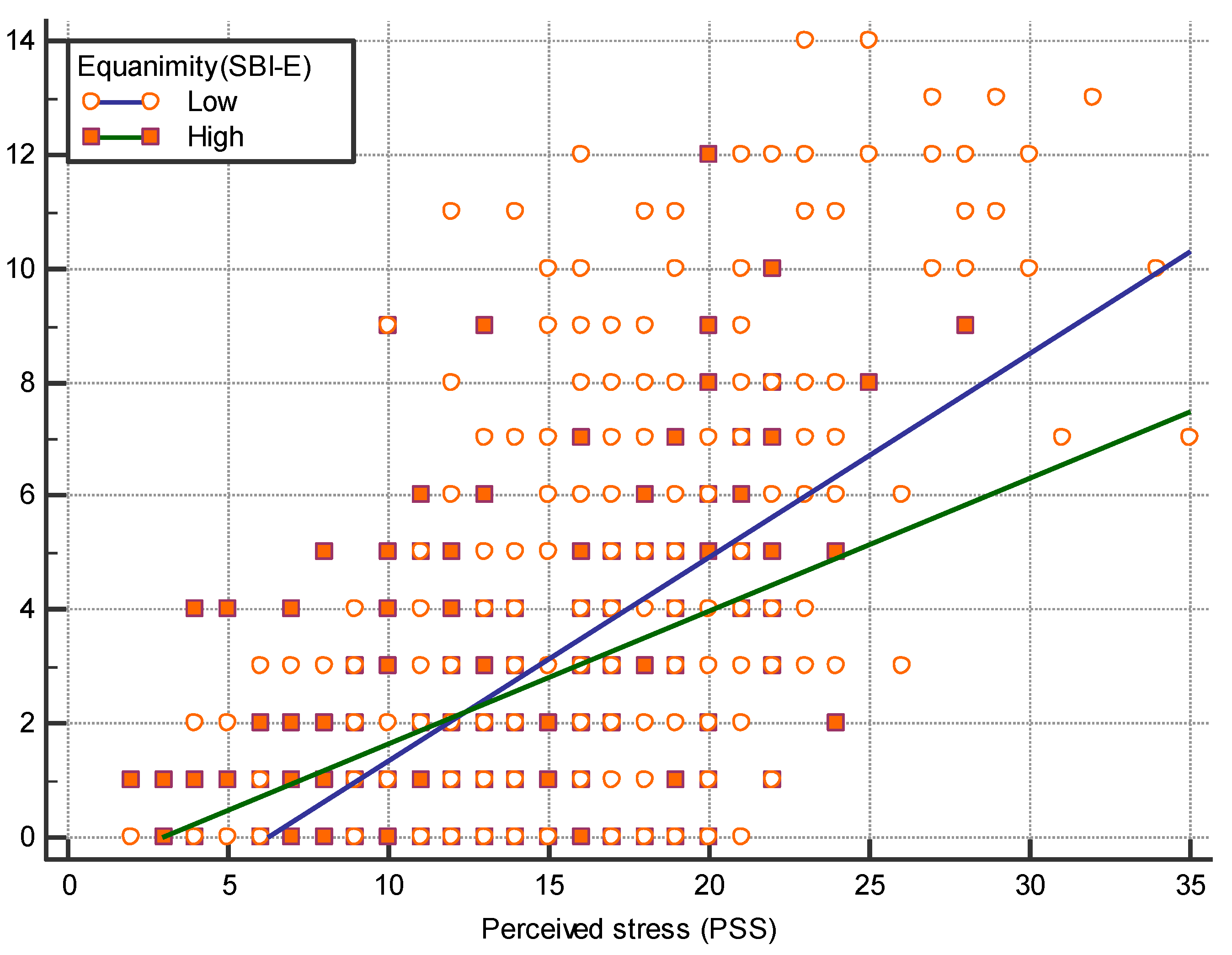
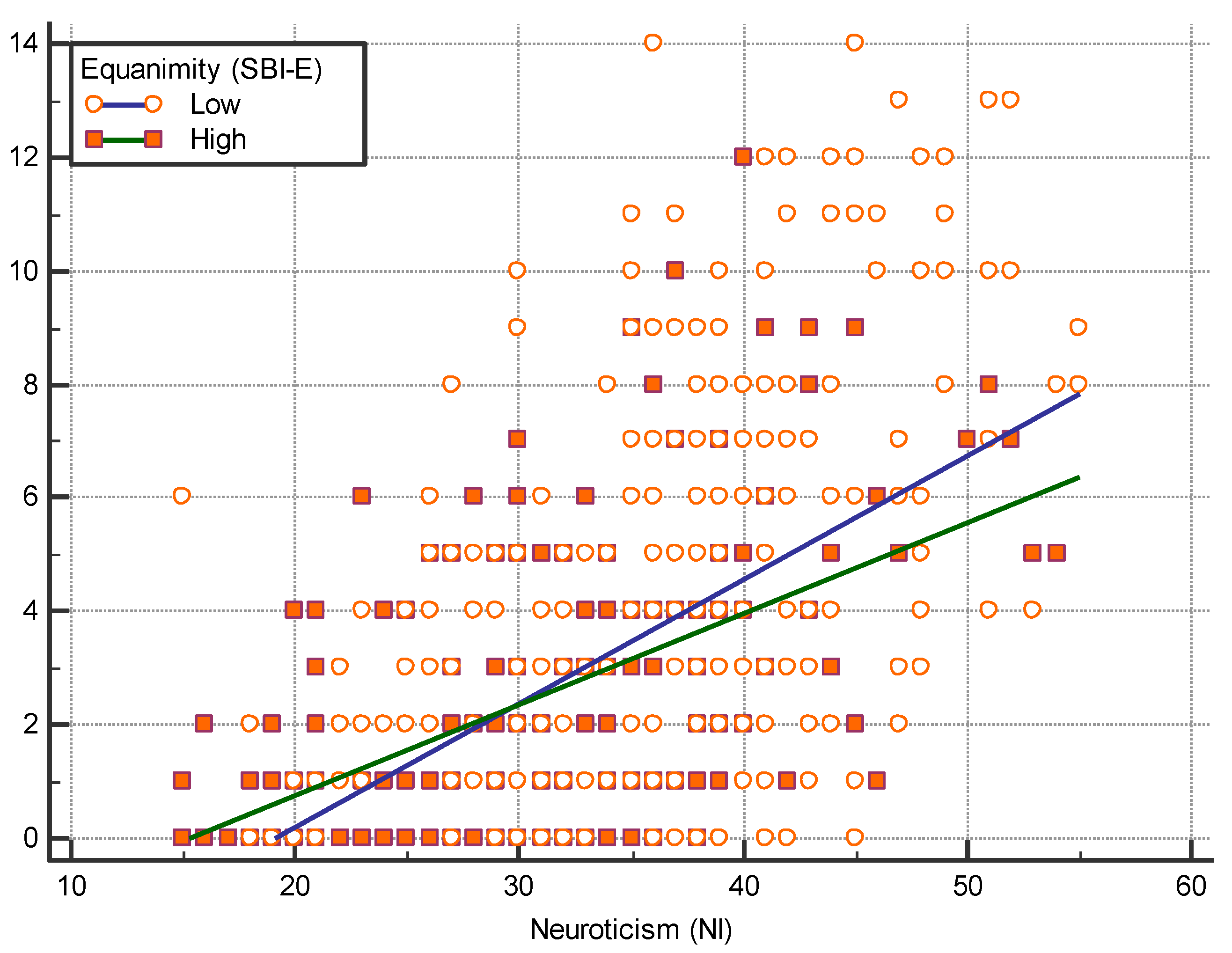
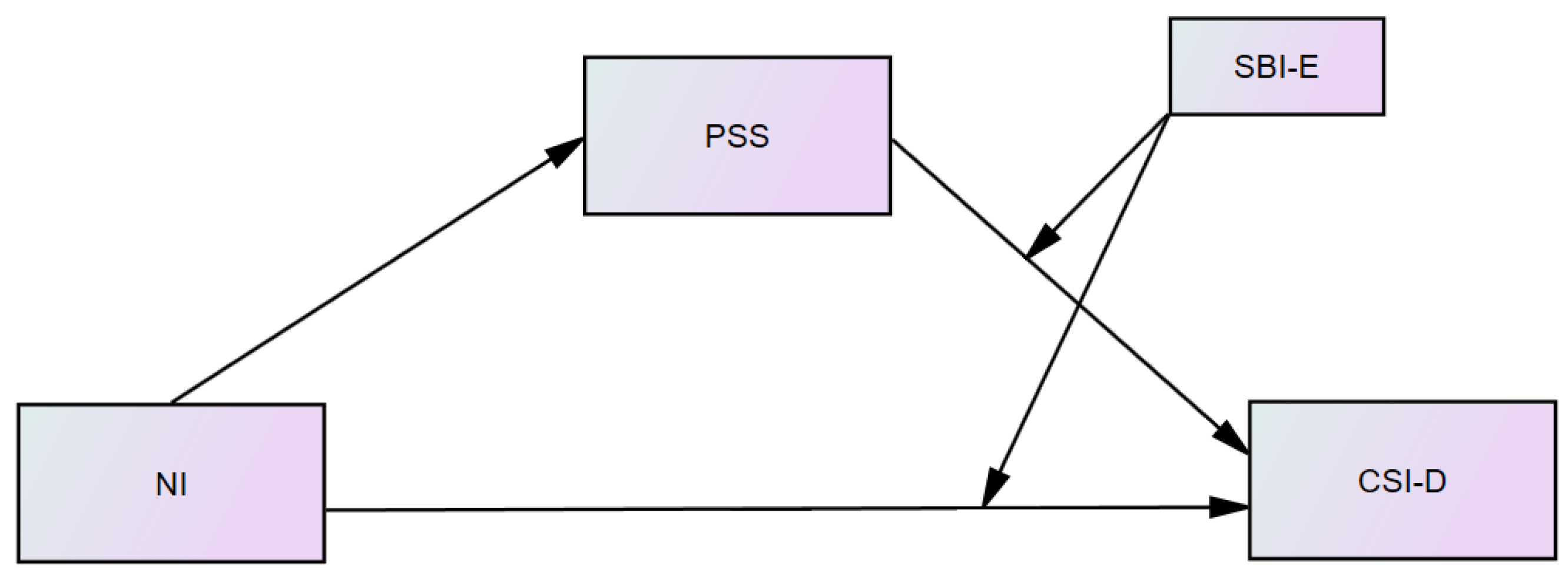
5. Results
6. Discussion
Strengths and Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Francis, L.J.; Brown, L.B.; Philipchalk, R. The development of an abbreviated form of the revised Eysenck personality questionnaire (EPQR-A): Its use among students in England, Canada, the U.S.A. and Australia. Personal. Individ. Differ. 1992, 13, 443–449. [Google Scholar] [CrossRef]
- Liu, Y.; Zhang, N.; Bao, G.; Huang, Y.; Ji, B.; Wu, Y.; Liu, C.; Li, G. Predictors of depressive symptoms in college students: A systematic review and meta-analysis of cohort studies. J. Affect. Disord. 2019, 244, 196–208. [Google Scholar] [CrossRef] [PubMed]
- Xia, J.; He, Q.; Li, Y.; Xie, D.; Zhu, S.; Chen, J.; Shen, Y.; Zhang, N.; Wei, Y.; Chen, C.; et al. The relationship between neuroticism, major depressive disorder and comorbid disorders in Chinese women. J. Affect. Disord. 2011, 135, 100–105. [Google Scholar] [CrossRef] [PubMed]
- McCrae, R.R.; Costa, P.T. The Five-Factor Theory of Personality: Theoretical Perspective; Guilford Press: New York, NY, USA, 1996. [Google Scholar]
- Abbasi, M.; Mirderikvand, F.; Adavi, H.; Hojati, M. The Relationship Between Personality Traits (Neuroticism and Extraversion) and Self-Efficacy With Aging Depression. Yektaweb J. 2018, 12, 458–466. [Google Scholar] [CrossRef]
- Wongpakaran, N.; Wongpakaran, T.; van Reekum, R. Social inhibition as a mediator of neuroticism and depression in the elderly. BMC Geriatr. 2012, 12, 41. [Google Scholar] [CrossRef] [PubMed]
- McCrae, R.R.; Terracciano, A. Universal features of personality traits from the observer’s perspective: Data from 50 cultures. J. Pers. Soc. Psychol. 2005, 88, 547–561. [Google Scholar] [CrossRef]
- Kadimpati, S.; Zale, E.L.; Hooten, M.W.; Ditre, J.W.; Warner, D.O. Associations between Neuroticism and Depression in Relation to Catastrophizing and Pain-Related Anxiety in Chronic Pain Patients. PLoS ONE 2015, 10, e0126351. [Google Scholar]
- Liu, C.; Chen, L.; Chen, S. Influence of Neuroticism on Depressive Symptoms Among Chinese Adolescents: The Mediation Effects of Cognitive Emotion Regulation Strategies. Front. Psychiatry 2020, 11, 420. [Google Scholar] [CrossRef]
- Wongpakaran, T.; Wongpakaran, N.; Sirithepthawee, U.; Pratoomsri, W.; Burapakajornpong, N.; Rangseekajee, P.; Bookkamana, P.; Temboonkiat, A. Interpersonal problems among psychiatric outpatients and non-clinical samples. Singap. Med. J. 2012, 53, 481–487. [Google Scholar]
- Kendler, K.S.; Kuhn, J.; Prescott, C.A. The Interrelationship of Neuroticism, Sex, and Stressful Life Events in the Prediction of Episodes of Major Depression. Am. J. Psychiatry 2004, 161, 631–636. [Google Scholar] [CrossRef]
- Kim, S.E.; Kim, H.N.; Cho, J.; Kwon, M.J.; Chang, Y.; Ryu, S.; Shin, H.; Kim, H.L. Direct and Indirect Effects of Five Factor Personality and Gender on Depressive Symptoms Mediated by Perceived Stress. PLoS ONE 2016, 11, e0154140. [Google Scholar]
- Banjongrewadee, M.; Wongpakaran, N.; Wongpakaran, T.; Pipanmekaporn, T.; Punjasawadwong, Y.; Mueankwan, S. The role of perceived stress and cognitive function on the relationship between neuroticism and depression among the elderly: A structural equation model approach. BMC Psychiatry 2020, 20, 25. [Google Scholar] [CrossRef] [PubMed]
- Gramstad, T.O.; Gjestad, R.; Haver, B. Personality traits predict job stress, depression and anxiety among junior physicians. BMC Med. Educ. 2013, 13, 150. [Google Scholar] [CrossRef] [PubMed]
- Pereira-Morales, A.; Adan, A.; Forero, D. Perceived Stress as a Mediator of the Relationship between Neuroticism and Depression and Anxiety Symptoms. Curr. Psychol. 2019, 38, 66–74. [Google Scholar] [CrossRef]
- Pizzagalli, D.A.; Bogdan, R.; Ratner, K.G.; Jahn, A.L. Increased perceived stress is associated with blunted hedonic capacity: Potential implications for depression research. Behav. Res. Ther. 2007, 45, 2742–2753. [Google Scholar] [CrossRef]
- Vasunilashorn, S.; Glei, D.A.; Weinstein, M.; Goldman, N. Perceived stress and mortality in a Taiwanese older adult population. Stress 2013, 16, 600–606. [Google Scholar] [CrossRef]
- Zannas, A.S.; McQuoid, D.R.; Steffens, D.C.; Chrousos, G.P.; Taylor, W.D. Stressful life events, perceived stress, and 12-month course of geriatric depression: Direct effects and moderation by the 5-HTTLPR and COMT Val158Met polymorphisms. Stress 2012, 15, 425–434. [Google Scholar] [CrossRef][Green Version]
- Wongpakaran, T.; Wongpakaran, N.; Pinyopornpanish, M.; Srisutasanavong, U.; Lueboonthavatchai, P.; Nivataphand, R.; Apisiridej, N.; Petchsuwan, D.; Saisavoey, N.; Wannarit, K.; et al. Baseline characteristics of depressive disorders in Thai outpatients: Findings from the Thai Study of Affective Disorders. Neuropsychiatr. Dis. Treat. 2014, 10, 217–223. [Google Scholar] [CrossRef][Green Version]
- Rocke, K.; Roopchand, X. Predictors for depression and perceived stress among a small island developing state university population. Psychol. Health Med. 2020, 26, 1108–1117. [Google Scholar] [CrossRef]
- Owczarek, J.E.; Lion, K.M.; Radwan-Oczko, M. The impact of stress, anxiety and depression on stomatognathic system of physiotherapy and dentistry first-year students. Brain Behav. 2020, 10, e01797. [Google Scholar] [CrossRef]
- Mrklas, K.; Shalaby, R.; Hrabok, M.; Gusnowski, A.; Vuong, W.; Surood, S.; Urichuk, L.; Li, D.; Li, X.M.; Greenshaw, A.J.; et al. Prevalence of Perceived Stress, Anxiety, Depression, and Obsessive-Compulsive Symptoms in Health Care Workers and Other Workers in Alberta During the COVID-19 Pandemic: Cross-Sectional Survey. JMIR Ment. Health 2020, 7, e22408. [Google Scholar] [CrossRef] [PubMed]
- Rietschel, L.; Zhu, G.; Kirschbaum, C.; Strohmaier, J.; Wüst, S.; Rietschel, M.; Martin, N.G. Perceived Stress has Genetic Influences Distinct from Neuroticism and Depression. Behav. Genet. 2014, 44, 639–645. [Google Scholar] [CrossRef] [PubMed]
- Ebstrup, J.F.; Eplov, L.F.; Pisinger, C.; Jørgensen, T. Association between the Five Factor personality traits and perceived stress: Is the effect mediated by general self-efficacy? Anxiety Stress Coping 2011, 24, 407–419. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.A.; Naragon-Gainey, K. Evaluation of the unique and specific contributions of dimensions of the triple vulnerability model to the prediction of DSM-IV anxiety and mood disorder constructs. Behav. Ther. 2013, 44, 277–292. [Google Scholar] [CrossRef]
- Hayward, R.D.; Taylor, W.D.; Smoski, M.J.; Steffens, D.C.; Payne, M.E. Association of five-factor model personality domains and facets with presence, onset, and treatment outcomes of major depression in older adults. Am. J. Geriatr. Psychiatry 2013, 21, 88–96. [Google Scholar] [CrossRef]
- van der Wal, R.A.; Bucx, M.J.; Hendriks, J.C.; Scheffer, G.J.; Prins, J.B. Psychological distress, burnout and personality traits in Dutch anaesthesiologists: A survey. Eur. J. Anaesthesiol. 2016, 33, 179–186. [Google Scholar] [CrossRef]
- Maciejewski, P.K.; Prigerson, H.G.; Mazure, C.M. Self-efficacy as a mediator between stressful life events and depressive symptoms. Differences based on history of prior depression. Br. J. Psychiatry 2000, 176, 373–378. [Google Scholar] [CrossRef]
- Wang, Y.; Yao, L.; Liu, L.; Yang, X.; Wu, H.; Wang, J.; Wang, L. The mediating role of self-efficacy in the relationship between Big five personality and depressive symptoms among Chinese unemployed population: A cross-sectional study. BMC Psychiatry 2014, 14, 61. [Google Scholar] [CrossRef]
- Gong, Y.; Shi, J.; Ding, H.; Zhang, M.; Kang, C.; Wang, K.; Yu, Y.; Wei, J.; Wang, S.; Shao, N.; et al. Personality traits and depressive symptoms: The moderating and mediating effects of resilience in Chinese adolescents. J. Affect. Disord. 2020, 265, 611–617. [Google Scholar] [CrossRef]
- An, Y.; Fu, G.; Yuan, G.; Zhang, Q.; Xu, W. Dispositional mindfulness mediates the relations between neuroticism and posttraumatic stress disorder and depression in Chinese adolescents after a tornado. Clin. Child. Psychol. Psychiatry 2019, 24, 482–493. [Google Scholar] [CrossRef]
- Giluk, T.L. Mindfulness, Big Five personality, and affect: A meta-analysis. Personal. Individ. Differ. 2009, 47, 805–811. [Google Scholar] [CrossRef]
- Thavaro, V. Handbook of Meditation Practice, 2nd ed.; Chuanpim: Bangkok, Thailand, 1982. [Google Scholar]
- The Path of Purification (Visuddhimagga). Available online: https://www.accesstoinsight.org/lib/authors/nanamoli/PathofPurification2011.pdf (accessed on 25 August 2021).
- Maurer, B.T. Evaluating the patient with a measure of equanimity. JAAPA 2009, 22, 56. [Google Scholar] [CrossRef]
- Sokol, D. Aequanimitas. Br. Med. J. 2007, 335, 1049. [Google Scholar] [CrossRef]
- Ostafin, B.; Robinson, M.; Meier, B. Introduction: The Science of Mindfulness and Self-Regulation. In Handbook of Mindfulness And Self-Regulation; Springer Science + Business Media: Berlin/Heidelberg, Germany, 2015; pp. 1–6. [Google Scholar]
- Kalra, S.; Priya, G.; Grewal, E.; Aye, T.T.; Waraich, B.K.; SweLatt, T.; Khun, T.; Phanvarine, M.; Sutta, S.; Kaush, U.; et al. Lessons for the Health-care Practitioner from Buddhism. Indian J. Endocrinol. Metab. 2018, 22, 812–817. [Google Scholar] [CrossRef] [PubMed]
- Kwok, J.Y.Y.; Kwan, J.C.Y.; Auyeung, M.; Mok, V.C.T.; Lau, C.K.Y.; Choi, K.C.; Chan, H.Y.L. Effects of Mindfulness Yoga vs Stretching and Resistance Training Exercises on Anxiety and Depression for People With Parkinson Disease: A Randomized Clinical Trial. JAMA Neurol. 2019, 76, 755–763. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Wongpakaran, N.; Wongpakaran, T. The Thai version of the PSS-10: An Investigation of its psychometric properties. Biopsychosoc. Med. 2010, 4, 6. [Google Scholar] [CrossRef] [PubMed]
- Wongpakaran, T.; Wongpakaran, N. The Effect of Neuroticism on Academic Performance and Quality of Life in Third-Year Medical Students, Chiang Mai University; Chaing Mai University: Chaing Mai, Thailand, 2013. [Google Scholar]
- Wongpakaran, N.; Wongpakaran, T.; Lertkachatarn, S.; Sirirak, T.; Kuntawong, P. Core Symptom Index (CSI): Testing for bifactor model and differential item functioning. Int. Psychogeriatr. 2019, 31, 1769–1779. [Google Scholar] [CrossRef] [PubMed]
- Wongpakaran, N.; Wongpakaran, T.; Kuntawong, P. Development and Validation of the inner Strength-Based Inventory (SBI). Ment. Health Relig. Cult. 2020, 23, 263–273. [Google Scholar]
- Shen, C.; Wang, M.P.; Ho, H.C.Y.; Wan, A.; Stewart, S.M.; Viswanath, K.; Chan, S.S.C.; Lam, T.H. Test–retest reliability and validity of a single-item Self-reported Family Happiness Scale in Hong Kong Chinese: Findings from Hong Kong Jockey Club FAMILY Project. Qual. Life Res. 2019, 28, 535–543. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process. Analysis: A Regression-Based Approach, 2nd ed.; Guilford Press: New York, NY, USA, 2018. [Google Scholar]
- Preacher, K.J.; Hayes, A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Method 2008, 40, 879–891. [Google Scholar] [CrossRef] [PubMed]
- D’Lima, G.M.; Pearson, M.R.; Kelley, M.L. Protective behavioral strategies as a mediator and moderator of the relationship between self-regulation and alcohol-related consequences in first-year college students. Psychol. Addict. Behav. 2012, 26, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Ding, H.; Han, J.; Zhang, M.; Wang, K.; Gong, J.; Yang, S. Moderating and mediating effects of resilience between childhood trauma and depressive symptoms in Chinese children. J. Affect. Disord. 2017, 211, 130–135. [Google Scholar] [CrossRef]
- van den Hurk, P.A.M.; Wingens, T.; Giommi, F.; Barendregt, H.P.; Speckens, A.E.M.; van Schie, H.T. On the Relationship Between the Practice of Mindfulness Meditation and Personality-an Exploratory Analysis of the Mediating Role of Mindfulness Skills. Mindfulness 2011, 2, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Sivaramappa, B.; Deshpande, S.; Kumar, P.V.G.; Nagendra, H.R. Effect of anapanasati meditation on anxiety: A randomized control trial. Ann. Neurosci. 2019, 26, 32–36. [Google Scholar] [CrossRef]
- Zeng, X.; Li, M.; Zhang, B.; Liu, X. Revision of the Philadelphia Mindfulness Scale for measuring awareness and equanimity in Goenka’s Vipassana meditation with Chinese Buddhists. J. Relig. Health 2015, 54, 623–637. [Google Scholar] [CrossRef]
- Desbordes, G.; Gard, T.; Hoge, E.A.; Hölzel, B.K.; Kerr, C.; Lazar, S.W.; Olendzki, A.; Vago, D.R. Moving beyond Mindfulness: Defining Equanimity as an Outcome Measure in Meditation and Contemplative Research. Mindfulness 2014, 2014, 356–372. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. Mindfulness-based interventions in context: Past, present, and future. Clin. Psychol. Sci. 2003, 10, 144–156. [Google Scholar] [CrossRef]
- Juneau, C.; Pellerin, N.; Trives, E.; Ricard, M.; Shankland, R.; Dambrun, M. Reliability and validity of an equanimity questionnaire: The two-factor equanimity scale (EQUA-S). PeerJ 2020, 8, e9405. [Google Scholar] [CrossRef]
- Dennison, P. The Human Default Consciousness and Its Disruption: Insights From an EEG Study of Buddhist Jhāna Meditation. Front. Hum. Neurosci. 2019, 13, 178. [Google Scholar] [CrossRef]
- Majjhimanikāyo Mūlapaṇṇāsapāḷi. Available online: https://84000.org/ (accessed on 25 August 2021).
- Grol-Prokopczyk, H. Thai and American doctors on medical ethics: Religion, regulation, and moral reasoning across borders. Soc. Sci. Med. 2013, 76, 92–100. [Google Scholar] [CrossRef]
- Upasen, R.; Thanasilp, S. Death acceptance from a Thai Buddhist perspective: A qualitative study. Eur. J. Oncol. Nurs. 2020, 49, 101833. [Google Scholar] [CrossRef] [PubMed]
- Nyklíček, I.; van Beugen, S.; Denollet, J. Effects of mindfulness-based stress reduction on distressed (type D) personality traits: A randomized controlled trial. J. Behav. Med. 2013, 36, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Mahāvaggo Paṭisambhidāmaggapāḷi. Available online: https://www.84000.org (accessed on 25 August 2021).
| Variable | Value | |
|---|---|---|
| Sex | n (%) | |
| Female | 478 (74.2) | |
| Male | 166 (25.8) | |
| Age | M ± SD | 28.28 ± 10.6 |
| Marital status | n (%) | |
| Single/divorced/widowed | 519 (80.6) | |
| Married | 125 (19.4) | |
| Monthly income | n (%) | |
| Less than 20,000 THB | 405 (62.9) | |
| 20,000 and more | 239 (37.1) | |
| Education | n (%) | |
| Less than Bachelor | 67 (10.4) | |
| Bachelor | 456 (70.8) | |
| Master and higher | 121 (18.8) | |
| Clinical variables | M ± SD | |
| NI score | 33.40 ± 9.0 | |
| CSI-D score | 3.05 ± 3.09 | |
| PSS score | 15.08 ± 6.0 | |
| SBI-E score | 3.81 ± 0.8 | |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1.Sex, female | ||||||||
| 2.Age | 0.009 | |||||||
| 3.Marital, no partner | 0.053 | 0.602 ** | ||||||
| 4.Education, bachelor | 0.197 * | 0.267 ** | 0.288 ** | |||||
| 5.Monthly income, <700 US | −0.194 * | 0.668 ** | 0.453 ** | 0.485 ** | ||||
| 6. NI score | 0.030 | 0.002 | 0.012 | −0.066 | 0.029 | |||
| 7. CSI-D score | −0.026 | −0.166 ** | −0.168 ** | −0.062 | −0.090 * | 0.578 ** | ||
| 8. PSS score | 0.004 | −0.062 | −0.001 | −0.062 | −0.054 | 0.599 ** | 0.611 ** | |
| 9. SBI-E score | 0.217 ** | 0.128 ** | 0.098 * | 0.110 ** | 0.053 | −0.305 ** | −0.355 ** | −0.307 ** |
| Outcome: CSI-Dep | Product of Coefficients | p-Value | Bootstrapping Bias-Corrected 95%CI | |||
|---|---|---|---|---|---|---|
| Point Estimate | SE | Lower Limit | Upper Limit | |||
| Model 1 (R2 = 0.326) (Single regression model) | Total effect | 0.571 | 0.024 | 0.000 | 0.531 | 0.608 |
| Direct effect | ||||||
| - NI | 0.571 | 0.024 | 0.000 | 0.531 | 0.608 | |
| Mediator: - | ||||||
| Total indirect | - | - | - | - | - | |
| Model 2 (R2 = 0.414) (Mediation model) | Total effect | 0.571 | 0.024 | 0.000 | 0.531 | 0.608 |
| Direct effect | ||||||
| Predictor-NI | 0.366 | 0.033 | 0.000 | 0.313 | 0.422 | |
| Mediator: PSS | 0.361 | 0.036 | 0.000 | 0.301 | 0.418 | |
| Total indirect | 0.205 | 0.024 | 0.000 | 0.167 | 0.245 | |
| Indirect effect | ||||||
| - via PSS | 0.205 | 0.024 | 0.000 | 0.167 | 0.245 | |
| Model 3 (R2 = 0.348) (Mediation model) | Total effect | 0.571 | 0.024 | 0.000 | 0.531 | 0.608 |
| Direct effect | ||||||
| - NI | 0.528 | 0.026 | 0.000 | 0.484 | 0.568 | |
| Mediator: SBI-E | −0.156 | 0.033 | 0.000 | −0.210 | −0.102 | |
| Total indirect | 0.043 | 0.011 | 0.000 | 0.028 | 0.063 | |
| Indirect effect | ||||||
| - via SBI-E | 0.043 | 0.026 | 0.000 | 0.028 | 0.063 | |
| Model 4 (R2 = 0.429) (Parallel mediation model) | Total effect | 0.571 | 0.024 | 0.000 | 0.531 | 0.608 |
| Direct effect | ||||||
| - NI | 0.340 | 0.033 | 0.000 | 0.287 | 0.397 | |
| Mediator: PSS | 0.346 | 0.036 | 0.000 | 0.285 | 0.403 | |
| Mediator: SBI-E | −0.125 | 0.031 | 0.000 | −0.177 | −0.073 | |
| Total indirect | 0.231 | 0.024 | 0.000 | 0.192 | 0.273 | |
| Indirect | ||||||
| - via PSS | 0.196 | 0.024 | 0.000 | 0.159 | 0.237 | |
| - via SBI-E | 0.026 | 0.009 | 0.004 | 0.014 | 0.044 | |
| - via PSS + SBI-E | 0.008 | 0.004 | 0.031 | 0.003 | 0.017 | |
| Model 5 (R2 = 0.429) (Serial mediation model) | Total effect | 0.571 | 0.024 | 0.000 | 0.528 | 0.604 |
| Direct effect | ||||||
| -NI | 0.340 | 0.034 | 0.000 | 0.287 | 0.397 | |
| Mediator: PSS | 0.346 | 0.036 | 0.000 | 0.285 | 0.403 | |
| Mediator: SBI-E | −0.125 | 0.031 | 0.000 | −0.177 | −0.073 | |
| Total indirect | 0.231 | 0.024 | 0.000 | 0.191 | 0.274 | |
| Indirect | ||||||
| - via PSS | 0.196 | 0.025 | 0.000 | 0.156 | 0.237 | |
| - via SBI-E | 0.026 | 0.009 | 0.004 | 0.014 | 0.044 | |
| - via PSS + SBI-E | 0.008 | 0.004 | 0.034 | 0.004 | 0.015 | |
| Outcome: CSI-Dep | Product of Coefficients | p-Value | Bootstrapping Bias-Corrected 95%CI | |||
|---|---|---|---|---|---|---|
| Point Estimate | SE | Lower Limit | Upper Limit | |||
| Model 15 (R2 = 0.646) | Total effect | 1.035 | 0.161 | 0.000 | 0.784 | 1.323 |
| Direct effect | ||||||
| - NI | 0.651 | 0.059 | 0.001 | 0.651 | 1.009 | |
| Mediator: PSS | 0.676 | 0.095 | 0.000 | 0.474 | 0.785 | |
| SBI-E | 0.427 | 0.098 | 0.000 | 0.286 | 0.608 | |
| Moderator1: SBI-E *Neuro | −0.418 | 0.189 | 0.027 | −0.559 | −0.178 | |
| Moderator2: SBI-E *PSS | −0.413 | 0.119 | 0.001 | −0.418 | −0.130 | |
| Total indirect | 0.384 | 0.059 | 0.000 | 0.277 | 0.464 | |
| Indirect effect | ||||||
| - via PSS | 0.384 | 0.059 | 0.000 | 0.277 | 0.464 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wongpakaran, N.; Wongpakaran, T.; Wedding, D.; Mirnics, Z.; Kövi, Z. Role of Equanimity on the Mediation Model of Neuroticism, Perceived Stress and Depressive Symptoms. Healthcare 2021, 9, 1300. https://doi.org/10.3390/healthcare9101300
Wongpakaran N, Wongpakaran T, Wedding D, Mirnics Z, Kövi Z. Role of Equanimity on the Mediation Model of Neuroticism, Perceived Stress and Depressive Symptoms. Healthcare. 2021; 9(10):1300. https://doi.org/10.3390/healthcare9101300
Chicago/Turabian StyleWongpakaran, Nahathai, Tinakon Wongpakaran, Danny Wedding, Zsuzsanna Mirnics, and Zsuzsanna Kövi. 2021. "Role of Equanimity on the Mediation Model of Neuroticism, Perceived Stress and Depressive Symptoms" Healthcare 9, no. 10: 1300. https://doi.org/10.3390/healthcare9101300
APA StyleWongpakaran, N., Wongpakaran, T., Wedding, D., Mirnics, Z., & Kövi, Z. (2021). Role of Equanimity on the Mediation Model of Neuroticism, Perceived Stress and Depressive Symptoms. Healthcare, 9(10), 1300. https://doi.org/10.3390/healthcare9101300









