The Role of Hospital Transfer in Reexamination Computed Tomography Scans: A Nationwide Cohort Study of Gastric Cancer Patients Undergoing Surgery
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Collection
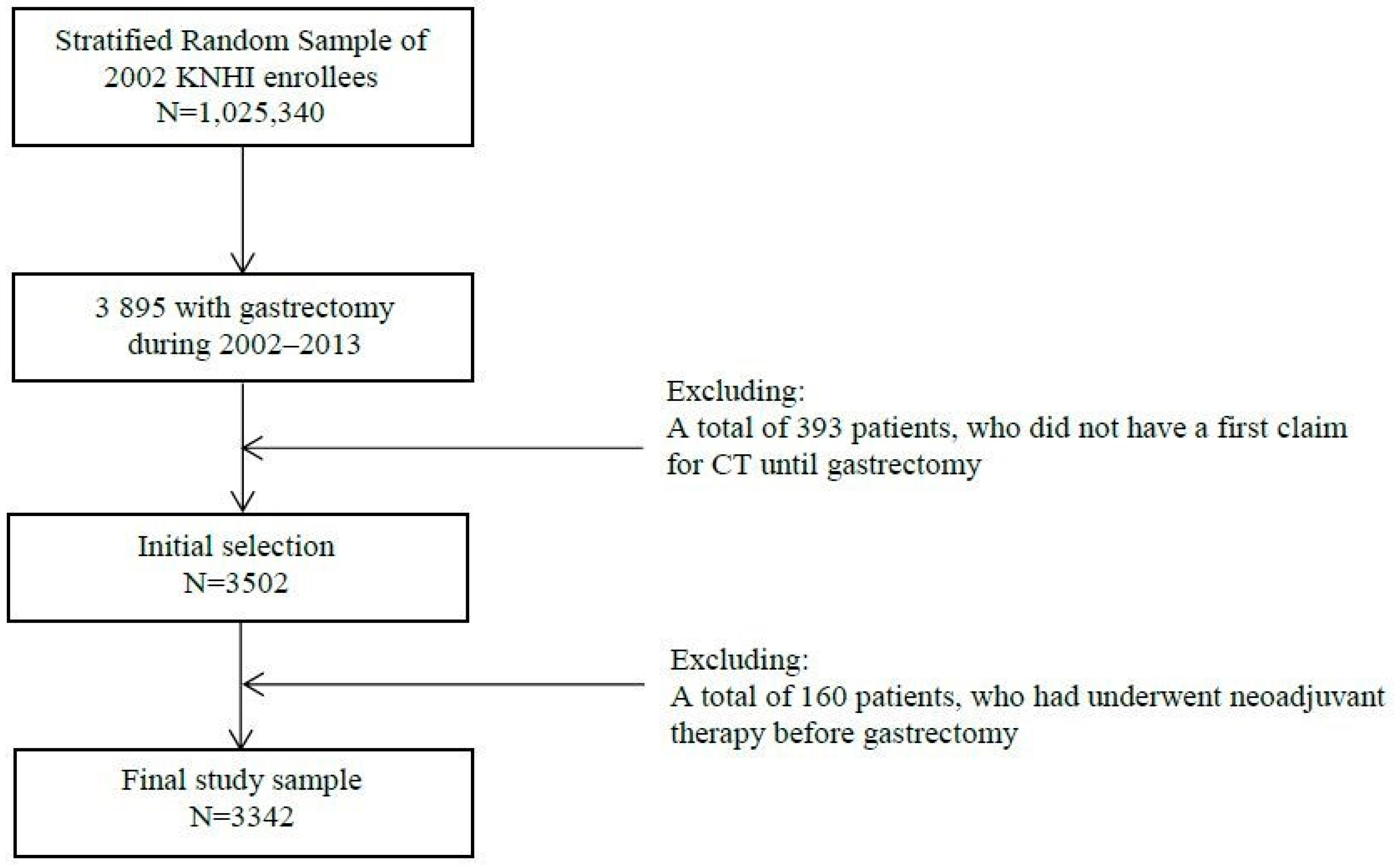
2.2. Description of the Study Cohort
2.3. Initial and Reexamination CT Scans
2.4. Statistical Analysis
3. Results
3.1. Demographic Characteristics
3.2. Multivariate Logistic Regression for Reexamination CT Scans
3.3. Subgroup Analysis for Transferred Patients Only
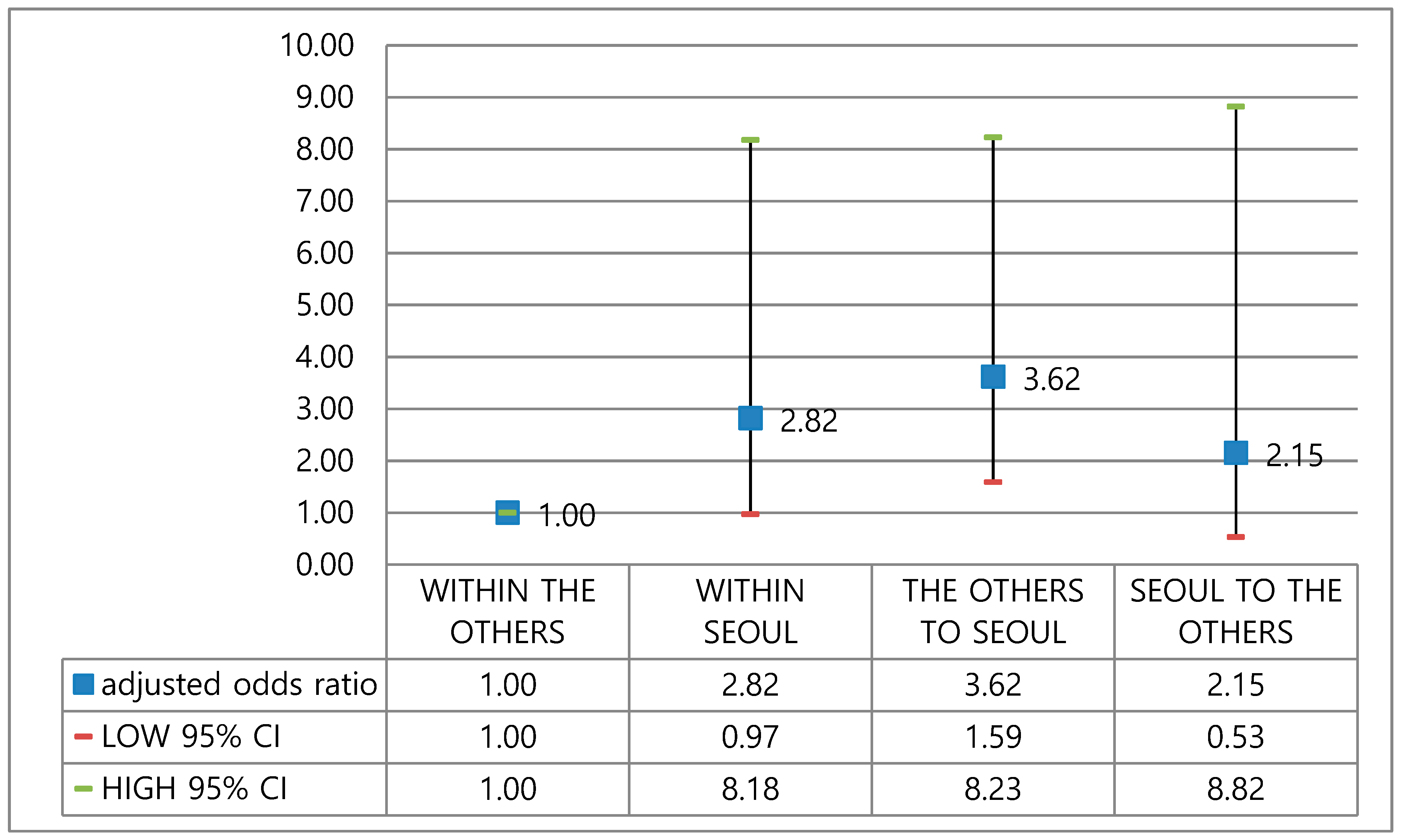
3.4. Subgroup Analysis: Transfer between General Hospitals
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ministry of Health and Welfare. New Health Plan 2020; Ministry of Health and Welfare: Seoul, Korea, 2011.
- Yang, B.M. Medical technology and inequity in health care: The case of Korea. Health Policy Plann. 1993, 8, 385–393. [Google Scholar] [CrossRef] [PubMed]
- OECD/WHO. Health at a Glance: Asia/Pacific 2018: Measuring Progress toward Universal Health Coverage; OECD Publishing: Paris, France, 2018. [Google Scholar] [CrossRef]
- Summers, R.M. Progress in fully automated abdominal CT interpretation. AJR Am. J. Roentgenol. 2016, 207, 67–79. [Google Scholar] [CrossRef] [PubMed]
- Richmond, C. Sir Godfrey Hounsfield. BMJ 2004, 329, 687. [Google Scholar] [CrossRef]
- Lee, S. Current status and policy options for high-tech medical devices in Korea: Vertical and horizontal synchronization of health policy. J. Korean Med. Assoc. 2012, 55, 950–958. [Google Scholar] [CrossRef][Green Version]
- Lee, S.; Oh, Y.; Song, H.; Kim, E.; Cho, S.; Baek, J. The Present Condition of Supply and Demand for Healthcare Resources and Management Policy Implications; Korea Institute for Health and Social Affairs: Seoul, Korea, 2003. [Google Scholar]
- Han, K.H.; Koh, S.K.; Jung, S.H. High-Price Medical Technologies in South Korea. Korean J. Hosp. Manag. 2007, 19, 479–485. [Google Scholar]
- Choi, Y.J.; Cho, S.J. Development of Fee Schedule for High-Tech Medical Imaging Devices; Health Insurance Review Agency: Seoul, Korea, 2012. [Google Scholar]
- Shen, L.; Shan, Y.S.; Hu, H.M.; Price, T.J.; Sirohi, B.; Yeh, K.H.; Yang, Y.H.; Sano, T.; Yang, H.K.; Zhang, X.; et al. Management of gastric cancer in Asia: Resource-stratified guidelines. Lancet Oncol. 2013, 14, e535–e547. [Google Scholar] [CrossRef]
- Nishida, T.; Blay, J.Y.; Hirota, S.; Kitagawa, Y.; Kang, Y.K. The standard diagnosis, treatment, and follow-up of gastrointestinal stromal tumors based on guidelines. Gastric Cancer 2016, 19, 3–14. [Google Scholar] [CrossRef]
- Oh, C.M.; Won, Y.J.; Jung, K.W.; Kong, H.J.; Cho, H.; Lee, J.K.; Lee, D.H.; Lee, K.H. Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2013. Cancer Res. Treat. 2016, 48, 436–450. [Google Scholar] [CrossRef]
- Kim, N.Y.; Oh, J.S.; Choi, Y.; Shin, J.; Park, E.C. Relationship between socioeconomic status and accessibility for endoscopic resection among gastric cancer patients: Using National Health Insurance Cohort in Korea: Poverty and endoscopic resection. Gastric Cancer 2017, 20, 61–69. [Google Scholar] [CrossRef]
- Shin, D.W.; Cho, B.; Guallar, E. Korean National Health Insurance Database. JAMA Intern. Med. 2016, 176, 138. [Google Scholar] [CrossRef]
- Lee, J.; Lee, J.S.; Park, S.H.; Shin, S.A.; Kim, K. Cohort Profile: The National Health Insurance Service–National Sample Cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 2016, 46, e15. [Google Scholar] [CrossRef] [PubMed]
- D’Hoore, W.; Bouckaert, A.; Tilquin, C. Practical considerations on the use of the charlson comorbidity index with administrative data bases. J. Clin. Epidemiol. 1996, 49, 1429–1433. [Google Scholar] [CrossRef]
- D’Hoore, W.; Sicotte, C.; Tilquin, C. Risk Adjustment in Outcome Assessment: The Charlson Comorbidity Index. Methods Inf. Med. 1993, 32, 382–387. [Google Scholar] [CrossRef] [PubMed]
- Fukuya, T.; Honda, H.; Hayashi, T.; Kaneko, K.; Tateshi, Y.; Ro, T.; Maehara, Y.; Tanaka, M.; Tsuneyoshi, M.; Masuda, K. Lymph-node metastases: Efficacy for detection with helical CT in patients with gastric cancer. Radiology 1995, 197, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Hur, J.; Park, M.S.; Lee, J.H.; Lim, J.S.; Yu, J.S.; Hong, Y.J.; Kim, K.W. Diagnostic accuracy of multidetector row computed tomography in T-and N staging of gastric cancer with histopathologic correlation. J. Comput. Assist Tomogr. 2006, 30, 372–377. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.W.; Lee, D.H.; Lee, S.H.; Park, Y.S.; Hwang, J.H.; Kim, J.W.; Jung, S.H.; Kim, N.Y.; Kim, Y.H.; Lee, K.H.; et al. Preoperative staging of gastric cancer by endoscopic ultrasonography and multidetector-row computed tomography. J. Gastroenterol. Hepatol. 2010, 25, 512–518. [Google Scholar] [CrossRef]
- Botet, J.F.; Lightdale, C.J.; Zauber, A.G.; Gerdes, H.; Winawer, S.J.; Urmacher, C.; Brennan, M.F. Preoperative staging of gastric cancer: Comparison of endoscopic US and dynamic CT. Radiology 1991, 181, 426–432. [Google Scholar] [CrossRef]
- Lee, J.M.; Jung, S.E. Imaging diagnosis of gastric cancer: CT scan. J. Korean Radiol. Soc. 2002, 46, 511–519. [Google Scholar] [CrossRef]
- Kim, K.S.; Lee, Y.J. Developments and General Features of National Health Insurance in Korea. Soc. Work Public Health 2010, 25, 142–157. [Google Scholar] [CrossRef]
- Shreibati, J.B.; Baker, L.C.; Hlatky, M.A. Association of Coronary CT Angiography or Stress Testing With Subsequent Utilization and Spending Among Medicare Beneficiaries. JAMA 2011, 306, 2128–2136. [Google Scholar] [CrossRef]
- Kim, L.; Kim, J.A.; Kim, S. A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples. Epidemiol. Health 2014, 36, e2014008. [Google Scholar] [CrossRef] [PubMed]
- Health Insurance Review and Assessment. The Reading Fee for External Medical Images; Health Insurance Review and Assessment: Seoul, Korea, 2003. [Google Scholar]
- Kwon, S. Payment system reform for health care providers in Korea. Health Policy Plann. 2003, 18, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Medicare Improvements for Patients and Providers Act of 2008. Section 135: Imaging Provisions. Available online: https://www.govinfo.gov/content/pkg/PLAW-110publ275/pdf/PLAW-110publ275.pdf (accessed on 15 November 2019).
- Lau, L.S. The Australian National Quality Program in Diagnostic Imaging and Interventional Radiology. J. AM Coll Radiol. 2007, 4, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Jho, W. Challenges for e-governance: Protests from civil society on the protection of privacy in e-government in Korea. Int. Rev. Adm. Sci. 2005, 71, 151–166. [Google Scholar] [CrossRef]
- Hann, I.H.; Hui, K.L.; Lee, S.Y.T.; Png, I.P.L. Overcoming Online Information Privacy Concerns: An Information-Processing Theory Approach. J. Manag. Inf. Syst. 2007, 24, 13–42. [Google Scholar] [CrossRef]
- Christiansen, C. X-ray contrast media-an overview. Toxicology 2005, 209, 185–187. [Google Scholar] [CrossRef]
- Song, S.Y. Future direction of nanomedicine in gastrointestinal cancer. Korean J. Gastroenterol. 2007, 49, 271–279. [Google Scholar]

| Variable | Reexamination CT Scan | Total | p-Value | |||
|---|---|---|---|---|---|---|
| NO | YES | |||||
| N | % | N | % | |||
| Age Group | ||||||
| 29 or below | 19 | 76.0 | 6 | 24.0 | 25 | 0.001 |
| 30 to 39 | 106 | 67.9 | 50 | 32.1 | 156 | |
| 40 to 49 | 352 | 69.8 | 152 | 30.2 | 504 | |
| 50 to 59 | 537 | 65.2 | 286 | 34.8 | 823 | |
| 60 to 69 | 673 | 66.3 | 342 | 33.7 | 1015 | |
| 70 to 79 | 440 | 61.2 | 279 | 38.8 | 719 | |
| 80 or above | 50 | 50.0 | 50 | 50.0 | 100 | |
| Sex | ||||||
| Male | 1430 | 63.6 | 820 | 36.4 | 2250 | 0.006 |
| Female | 747 | 68.4 | 345 | 31.6 | 1092 | |
| Health Coverage Type | ||||||
| National Health Insurance | 2104 | 65.2 | 1125 | 34.8 | 3229 | 0.903 |
| Medical aid | 73 | 64.6 | 40 | 35.4 | 113 | |
| Residential Area | ||||||
| Rural | 784 | 65.4 | 414 | 34.6 | 1198 | 0.784 |
| City | 1393 | 65.0 | 751 | 35.0 | 2144 | |
| Premium Level | ||||||
| Low | 334 | 64.6 | 183 | 35.4 | 517 | 0.942 |
| Middle | 664 | 65.5 | 350 | 34.5 | 1014 | |
| High | 1179 | 65.1 | 632 | 34.9 | 1811 | |
| Transfer (1st ct ≠ Surgery) | ||||||
| No | 2070 | 77.7 | 593 | 22.3 | 2663 | <0.001 |
| Yes | 107 | 15.8 | 572 | 84.2 | 679 | |
| Gastrectomy Type | ||||||
| Total | 400 | 54.5 | 334 | 45.5 | 734 | <0.001 |
| Subtotal/Partial | 1777 | 68.1 | 831 | 31.9 | 2608 | |
| Charlson Comorbidities Index | ||||||
| Mean | SD | Mean | SD | |||
| Score | 1.3 | 1.1 | 1.5 | 1.3 | <0.001 | |
| Hospital Type, Taking the Initial ct | ||||||
| Clinic | 23 | 29.9 | 54 | 70.1 | 77 | <0.001 |
| Hospital | 25 | 19.4 | 104 | 80.6 | 129 | |
| General hospital | 2129 | 67.9 | 1007 | 32.1 | 3136 | |
| Hospital Provinces *, Taking the Initial ct | ||||||
| Capital | 940 | 71.9 | 367 | 28.1 | 1307 | <0.001 |
| Metropolitan | 627 | 65.4 | 331 | 34.6 | 958 | |
| Other rural provinces | 610 | 56.6 | 467 | 43.4 | 1077 | |
| Total | 2177 | 65.1 | 1165 | 34.9 | 3342 | |
| Variable | OR | Low CI | High CI |
|---|---|---|---|
| Age Group | |||
| 29 or below | 0.88 | 0.29 | 2.68 |
| 30 to 39 | 0.95 | 0.58 | 1.54 |
| 40 to 49 | 1.00 | ||
| 50 to 59 | 1.24 | 0.93 | 1.66 |
| 60 to 69 | 1.31 | 0.98 | 1.74 |
| 70 to 79 | 1.56 | 1.15 | 2.12 |
| 80 or above | 2.52 | 1.51 | 4.20 |
| Sex | |||
| Male | 1.00 | ||
| Female | 0.83 | 0.69 | 1.01 |
| Health coverage type | |||
| National health insurance | 1.00 | ||
| Medical aid | 0.93 | 0.55 | 1.55 |
| Residential area | |||
| Rural | 1.00 | ||
| City | 1.28 | 1.06 | 1.54 |
| Premium level | |||
| Low | 1.00 | ||
| Middle | 0.94 | 0.70 | 1.25 |
| High | 0.83 | 0.63 | 1.09 |
| Transfer * | |||
| No | 1.00 | ||
| Yes | 23.87 | 18.15 | 31.39 |
| Gastrectomy type | |||
| Total | 1.90 | 1.55 | 2.33 |
| Subtotal/Partial | 1.00 | ||
| Charlson comorbidities index | |||
| Per point | 1.05 | 0.97 | 1.14 |
| Hospital type, taking the initial ct | |||
| Clinic | 0.45 | 0.26 | 0.80 |
| Hospital | 1.40 | 0.79 | 2.46 |
| General hospital | 1.00 | ||
| Hospital provinces, taking the initial ct | |||
| Capital (seoul) | 1.00 | ||
| Metropolitan (busan, daegu, gwangju, daejeon, ulsan, and incheon) | 0.45 | 0.26 | 0.80 |
| Other rural provinces | 1.40 | 0.79 | 2.46 |
| Year | |||
| Per one year | 1.15 | 1.12 | 1.19 |
| Variable | OR | Low CI | High CI | p-Value |
|---|---|---|---|---|
| Transfer route | ||||
| General to general hospital | 1.00 | |||
| Clinic and hospital to general hospital | 0.65 | 0.32 | 1.33 | 0.2426 |
| Number of beds, initial ct hospital | ||||
| Per 100 beds | 0.88 | 0.83 | 0.94 | <0.001 |
| Number of beds, surgery hospital | ||||
| Per 100 beds | 1.29 | 1.20 | 1.36 | <0.001 |
| VARIABLE | OR | Low CI | High CI | p-Value |
|---|---|---|---|---|
| Number of beds, initial ct hospital | ||||
| Per 100 beds | 0.91 | 0.88 | 0.95 | <0.001 |
| Number of beds, surgery hospital | ||||
| Per 100 beds | 1.10 | 1.06 | 1.13 | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, J.; Choi, Y.J.; Choi, Y.; Lee, S.G.; Kim, J.M. The Role of Hospital Transfer in Reexamination Computed Tomography Scans: A Nationwide Cohort Study of Gastric Cancer Patients Undergoing Surgery. Healthcare 2020, 8, 2. https://doi.org/10.3390/healthcare8010002
Shin J, Choi YJ, Choi Y, Lee SG, Kim JM. The Role of Hospital Transfer in Reexamination Computed Tomography Scans: A Nationwide Cohort Study of Gastric Cancer Patients Undergoing Surgery. Healthcare. 2020; 8(1):2. https://doi.org/10.3390/healthcare8010002
Chicago/Turabian StyleShin, Jaeyong, Yoon Jung Choi, Young Choi, Sang Gyu Lee, and Ji Man Kim. 2020. "The Role of Hospital Transfer in Reexamination Computed Tomography Scans: A Nationwide Cohort Study of Gastric Cancer Patients Undergoing Surgery" Healthcare 8, no. 1: 2. https://doi.org/10.3390/healthcare8010002
APA StyleShin, J., Choi, Y. J., Choi, Y., Lee, S. G., & Kim, J. M. (2020). The Role of Hospital Transfer in Reexamination Computed Tomography Scans: A Nationwide Cohort Study of Gastric Cancer Patients Undergoing Surgery. Healthcare, 8(1), 2. https://doi.org/10.3390/healthcare8010002




