1. Introduction
Constipation is defined as a state in which feces cannot be defecated in sufficient quantity and with comfort [
1]. In general, constipation is diagnosed based on symptoms according to the Rome IV diagnostic criteria [
2]. To define constipation, two or more of the following symptoms should be present: straining at stool, lumpy or hard stool, sensation of incomplete evacuation, sensation of anorectal obstruction or blockage, need for manual maneuvers, and fewer than three bowel movements per week. The pathophysiology of constipation includes impairment of colonic transit function (i.e., slow transit constipation) and defecation disorders, such as difficult defecation, incomplete evacuation, and rectal hyposensitivity [
3,
4].
The prevalence of constipation in the elderly population is as high as 30% compared with that in younger populations [
5,
6,
7]. Japan has become a super-aging society with increasing number of elderly people with cerebrovascular diseases and dementia. It could be considered that the number of elderly people who could not complain of subjective symptoms or who have difficulty with communication are increasing.
Generally, in hospitals, nurses assess constipation in older people who have difficulty communicating their constipation symptoms accurately, based on the hardness of stool and bowel movement frequency, and choose bowel-related nursing care, such as laxative or suppository administration or digital disimpaction [
8]. However, in home-care settings, constipation may be difficult to assess in older people by observing feces because visiting nurses cannot always observe the feces directly. Several problems such as diarrhea can be caused by administration of laxatives to patients who are not constipated [
9], and administration of suppositories to patients without rectal fecal retention is inappropriate [
1]. Furthermore, digital disimpaction should not be performed in patients without fecal impaction [
10] because of its invasiveness and risk of rectal mucosa damage [
11]. Therefore, to accurately assess constipation, a new objective assessment method for nurses to observe feces and evaluate constipation in home-care settings is needed.
Some objective assessment methods to observe feces in the body already exist, such as colon transit time examination (CTT), computed tomography (CT), and magnetic resonance imaging (MRI) [
3,
7]. Although CTT can evaluate the movement of feces, it cannot evaluate fecal properties and volume in real time. CT and MRI can evaluate fecal properties and volume; however, these methods are invasive because of radiation exposure or longer examination time. Moreover, the assessment methods as described above cannot be used for assessment by nurses in home-care settings.
In this study, transabdominal ultrasonography (US) was evaluated as an assessment method that nurses can use in home-care settings, as a US is easily portable and enables noninvasive observation of feces in real time [
12,
13]. Rectal US has already been used to evaluate the presence or absence of feces and fecal volume in children [
14,
15]. Moreover, colonic US can be used for qualitative assessment of feces in adults [
13]. However, to our knowledge, previous studies have not clarified the relationship between the patterns of fecal distribution changes and constipation symptoms in the colorectum in elderly people. It is necessary to clarify the actual condition in facilities where feces can be directly observed.
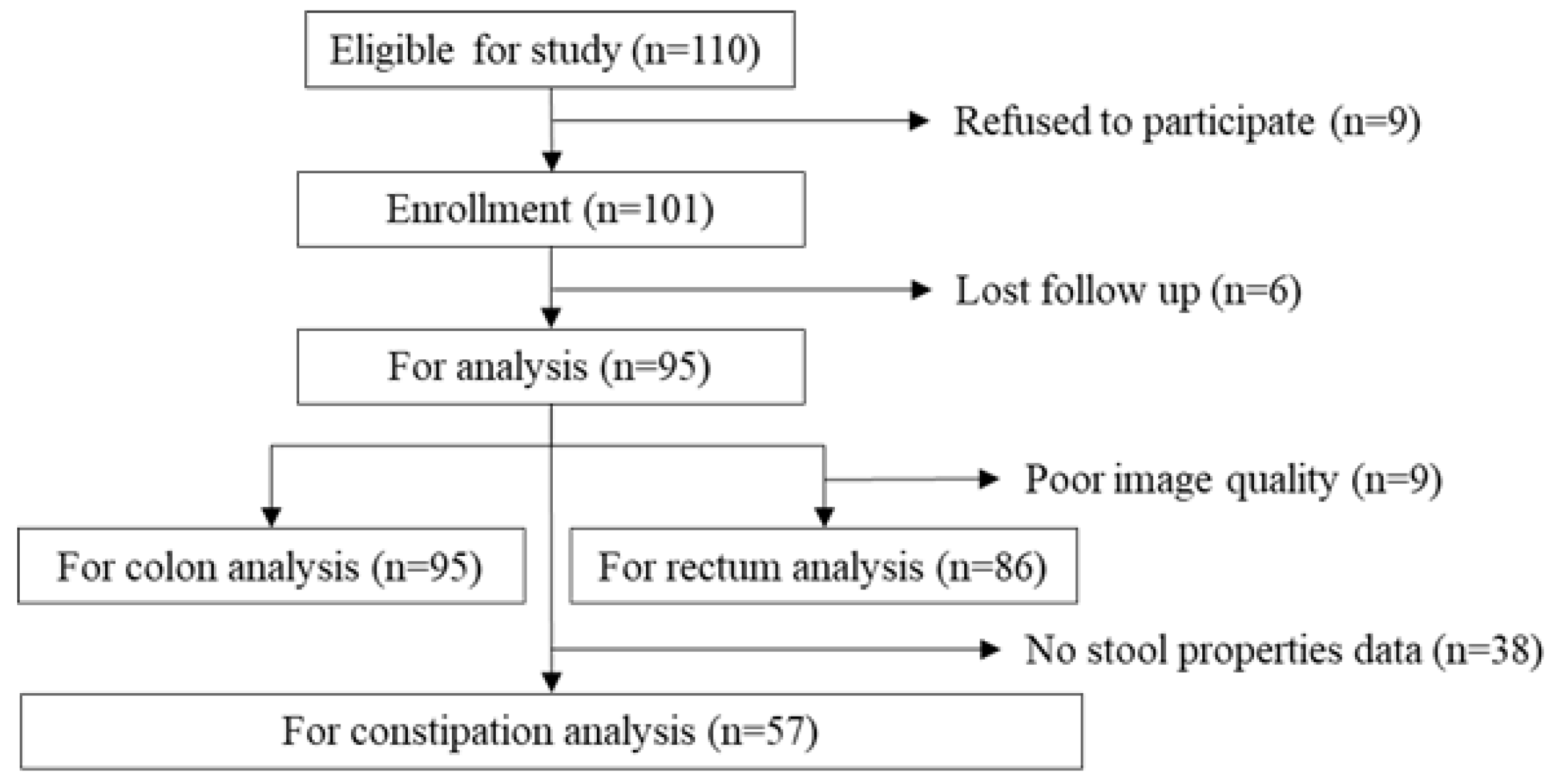
The aims of this study were to continuously observe fecal distribution changes using colorectal US and to clarify the relationship between patterns of fecal distribution changes and constipation symptoms in older people with physical and cognitive impairment at long-term care facilities.
4. Discussion
This study aimed to firstly investigate the usefulness of US for continuous observation of the patterns of fecal distribution changes in older people with physical and cognitive impairment, because US has been generally only used for the diagnosis of colorectal disease.
In healthy adults, rectal fecal retention was observed only when they had a desire to defecate [
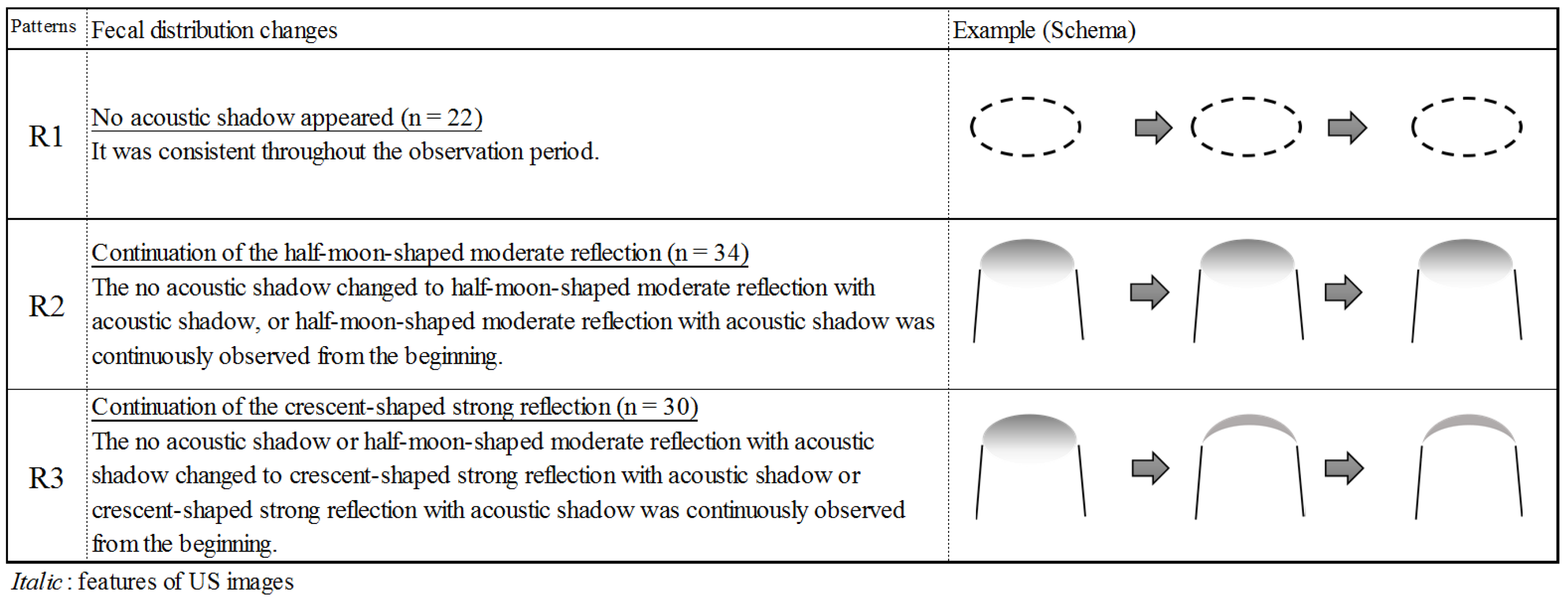
22]. However, in this study, rectal patterns of R2 or R3 were recognized as fecal retention [
15] in approximately 70% of all patients. Further, the rectal fecal retention pattern was significantly associated with severe cognitive impairment and defecation on the bed. Thus, older people with physical and cognitive impairment tend to have fecal retention in the rectum (anorectal dysfunction). This indicates that abnormal patterns of fecal distribution changes existed. The older people may feel uncomfortable due to continuous fecal retention in the rectum. Elderly people with physical and cognitive impairment tend to have a higher rectal perception threshold than younger people [
23], decreased rectal sensitivity and increased rectal compliance can contribute to fecal retention by decreasing the frequency and intensity of the desire to defecate [
4]. Moreover, having a correct posture is crucial for appropriate defecation [
24].
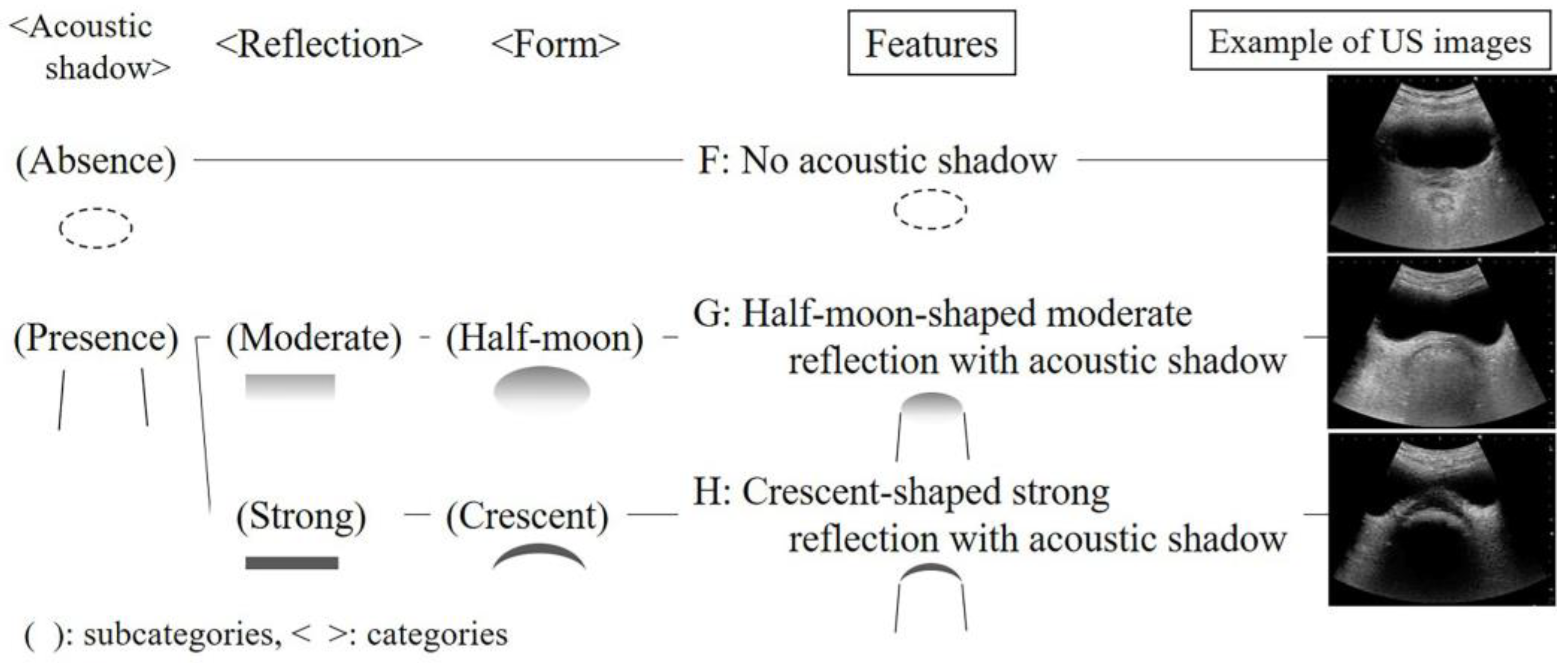
In this study, a new US finding was the R2 pattern, which indicated soft stool in approximately 80% of patients. The R3 pattern indicated hard stool in approximately 90% of patients and was significantly associated with severe cognitive impairment. The hardness of stool correlates with the length of bowel movement frequency [
16]. As cognitive impaired patients have difficulty in perceiving the rectal fecal retention, or reporting a desire to defecate, feces should be stagnated, and the frequency in bowel movements should be longer. Therefore, rectal fecal properties should be assessed in patients with severe cognitive impairment using rectal US as hard stool is likely to be retained in the rectum. This can be assessed through the crescent-shaped strong reflection with an acoustic shadow.
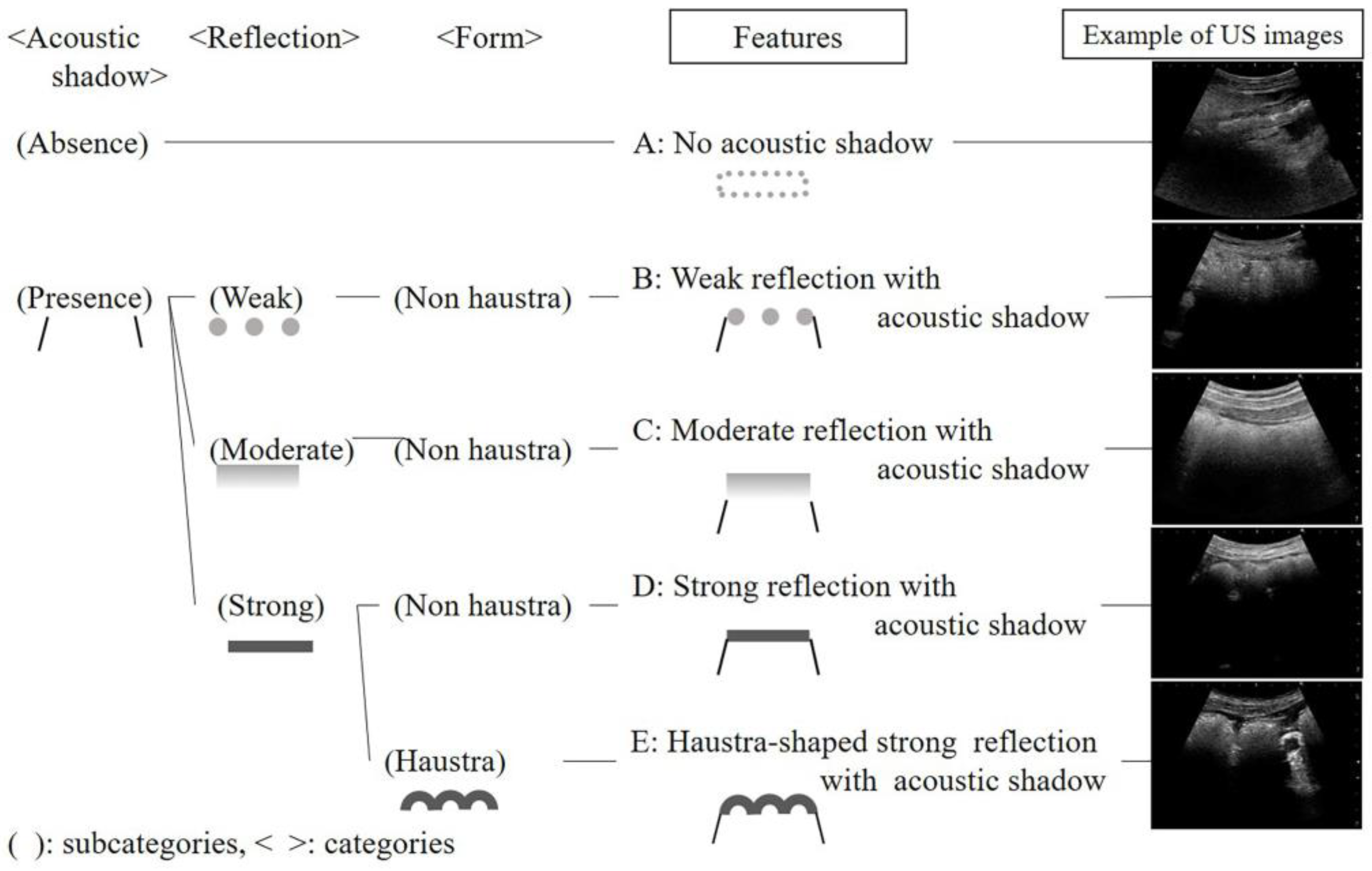
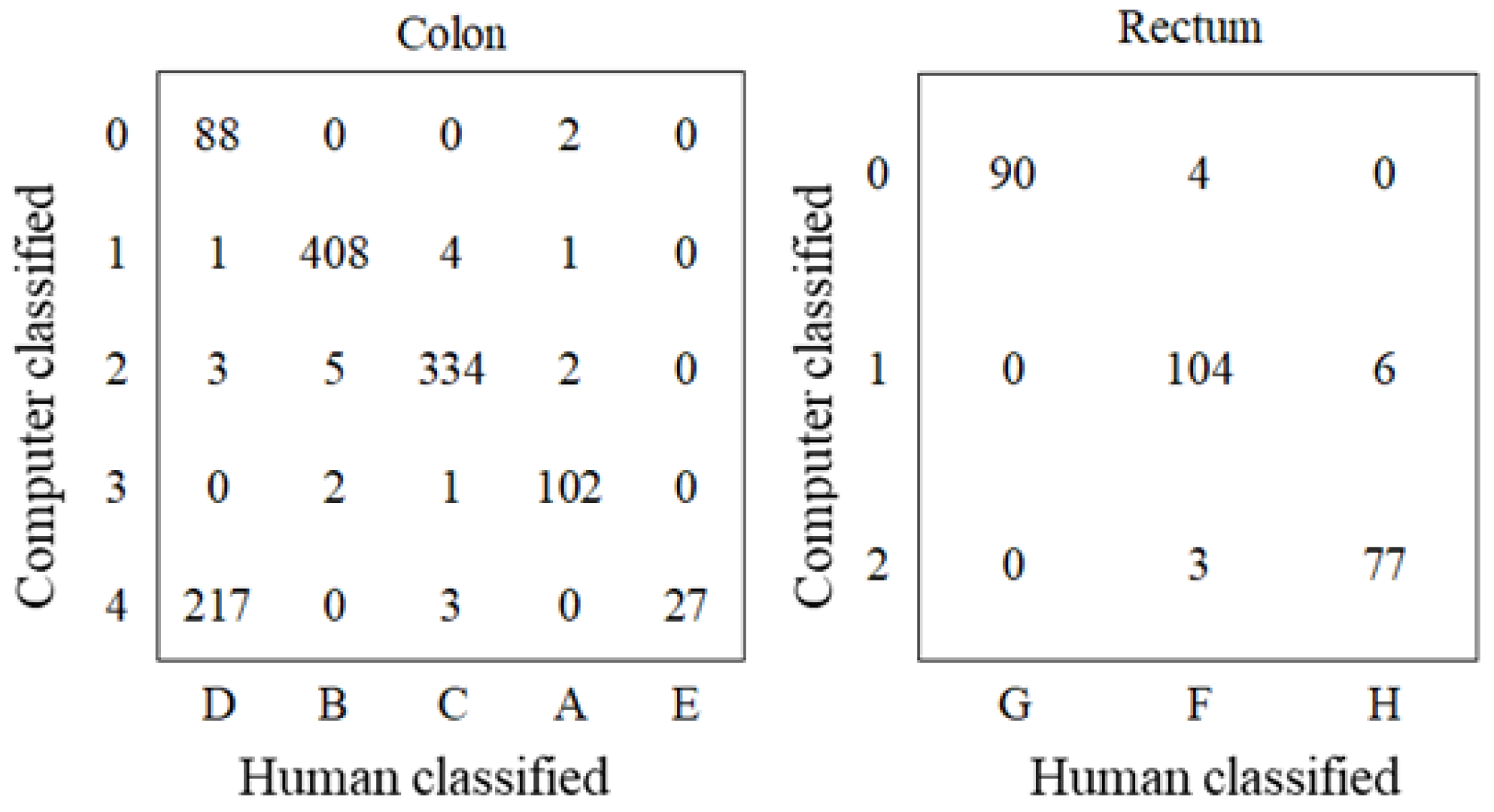
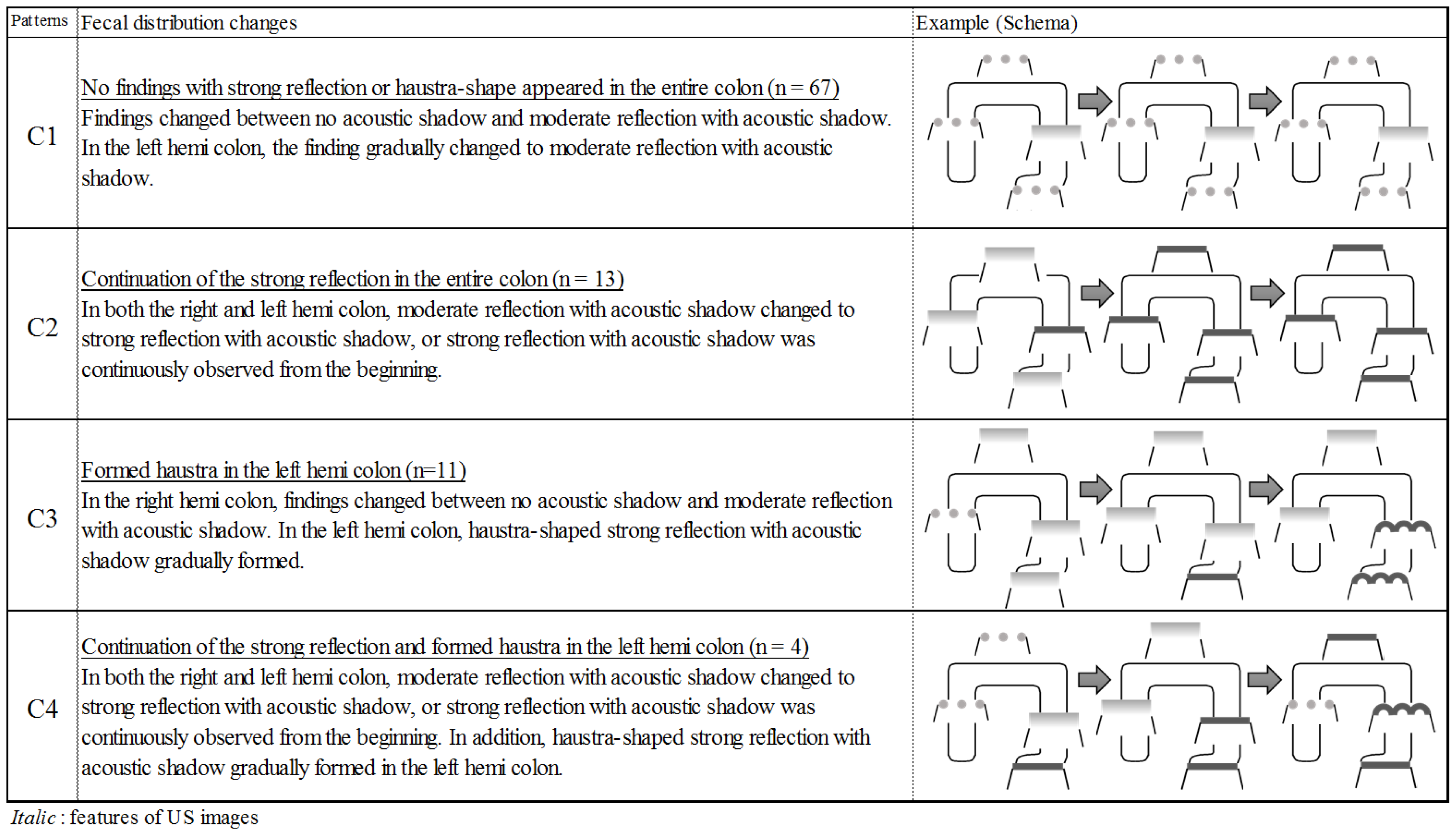
A clustering method in the text mining was used for internal validation of qualitative analysis. This method is commonly used in information science areas for automatic categorization. The method is capable of validating generated features as another evaluator. The human-detected features were well matched with the computer-detected features except in one category. Features D (strong reflection with acoustic shadow) and E (haustra-shaped strong reflection with acoustic shadow) were similar because descriptions of both features included almost the same words, and the difference was in only a few words related to haustra. Thus, the computer could not distinguish well between the two features, which led to failure of detecting feature D. The consistency between human and computer feature detection indicated that the detected features might be valid.
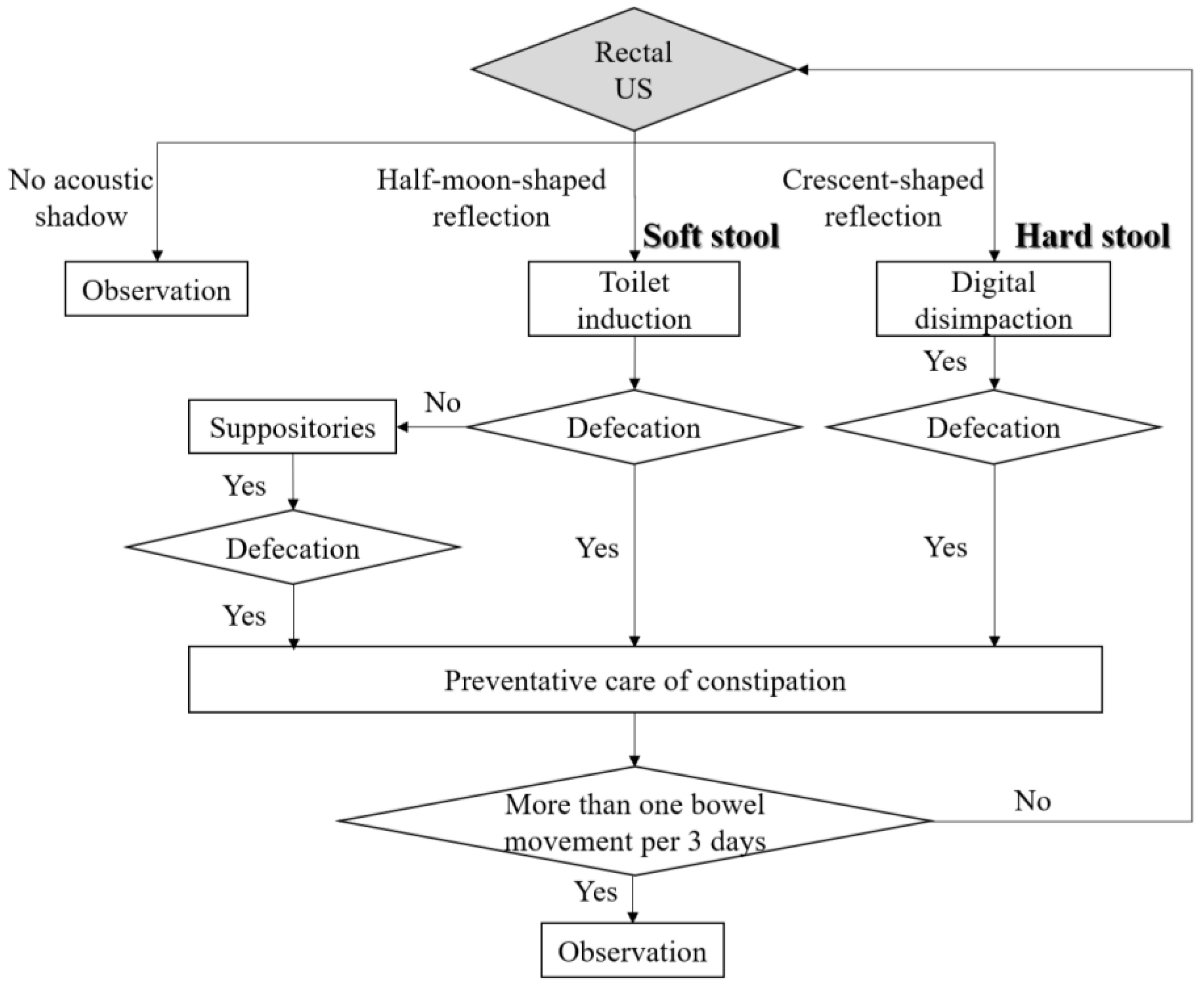
As a result of this study, nurses should assess constipation by US in older people with severe cognitive impairment and select appropriate bowel-related nursing care. Based on the results of this study, we propose a bowel-related nursing care algorithm using US for older people with physical and cognitive impairment (
Figure 7). First, US should be performed to detect crescent-shaped strong reflection findings in the rectum because fecal impaction must be relieved [
24]. Next, if rectal US detects a half-moon-shaped moderate reflection, nurses should select appropriate bowel-related nursing care, such as toilet induction, to promote defecation. After defecation, nurses should perform preventative care of constipation. Introducing this algorithm using US, it may be possible to assess fecal retention of hard stool in the rectum in older people without digital disimpaction. It contributes to patient’s comfort, because of noninvasive assessment in real time. Further studies are warranted to determine whether this algorithm can be particularly applied to patients with physical and cognitive impairment in home-care settings. Furthermore, we believe that US can solve nurses’ dilemma in bowel-related nursing care to patients who cannot communicate their desire to defecate.
Generally, US depends on operator skill and technique. However, this study has additional finding that nurses who were not familiar to US operation could detect easily the rectal fecal retention using US, according to this study process. The screening technique is as follows: first, US could be performed by applying the convex probe onto the suprapubic rim and further inclining the probe approximately 15° toward the head side to identify the rectum, as point-of-care US [
25]. Moreover, US is considered as a relatively low-cost equipment, which requires lesser electricity and cost-effective echo jelly. Therefore, US can be used as a feasible assessment tool by nurses.
There are some limitations to this study. First, patients who have not defecated for 3 days had undergone routine care with administration of a suppository at the research hospitals. Thus, the results of this study may not be applicable at acute care hospitals. Second, the sample size of patients who could be observed of fecal properties was small. However, in this study, US was useful to objectively evaluate constipation in older people with physical and cognitive impairment.