Assessing the Need and Demand for a Community Emergency Paramedic Strategy in the Ambulance Rescue System of Hamburg, Germany
Abstract
1. Introduction
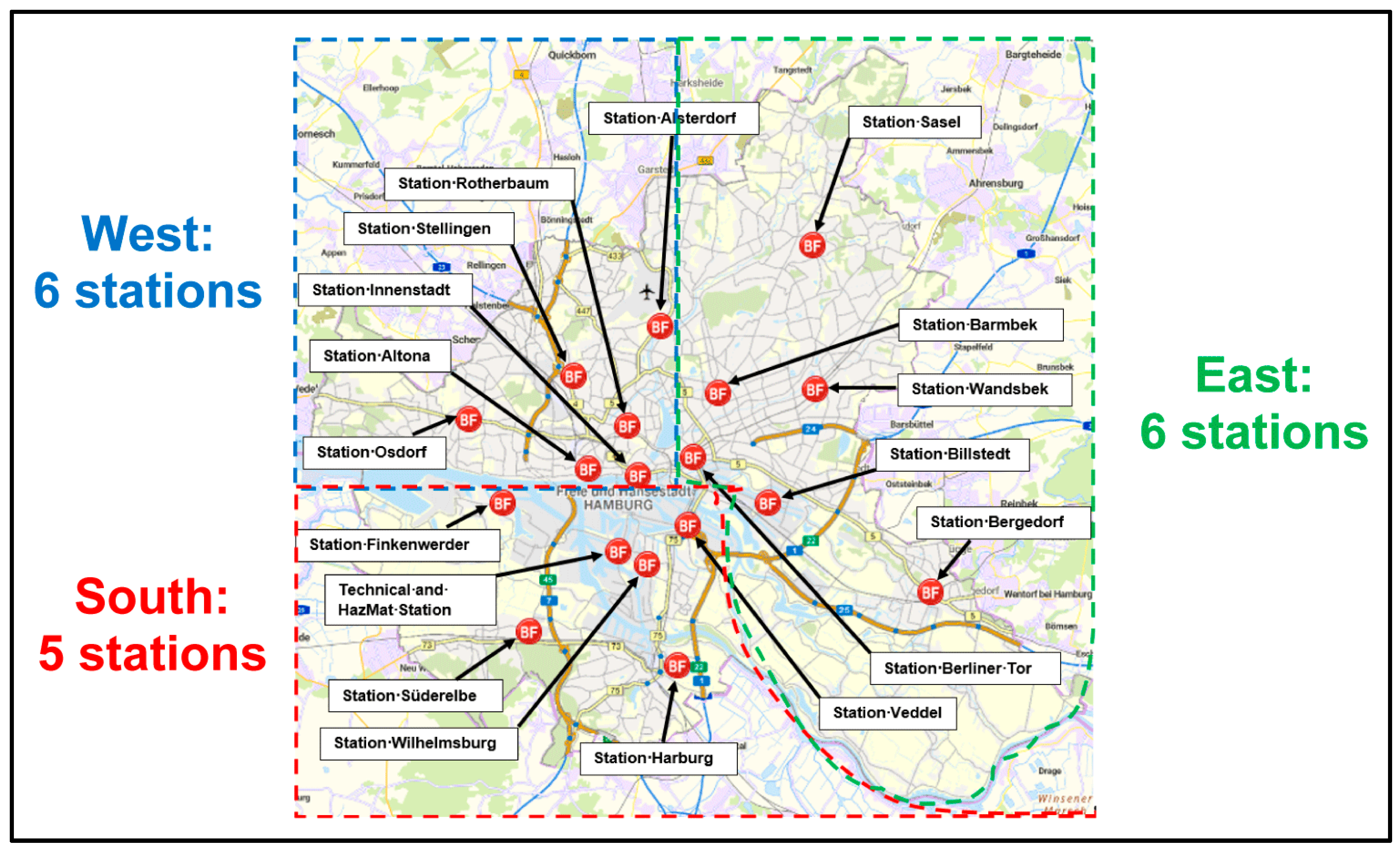
1.1. The Ambulance Rescue System in the City of Hamburg, Germany
1.2. The General Potential of CEP Systems
1.3. The Potential of a CEP System for the City of Hamburg, Germany
- Can a station-level analysis for the 17 major rescue stations identify areas with the greatest potential for non-time-critical CEP interventions?
- Which time-of-day or seasonal factors significantly influence non-critical call patterns?
- How could these insights inform policymakers about resource allocation?
- Does an uneven distribution of call volume (high-demand vs. low-demand areas) require tailored CEP strategies, especially at peak times?
2. Materials and Methods
2.1. Purpose of the Case Study
2.2. Data of the Case Study
2.3. Statistical and Policy Analyses Performed
3. Results
3.1. Descriptive Analysis Including Statistical Tests, Clustering Methods and Regression Models
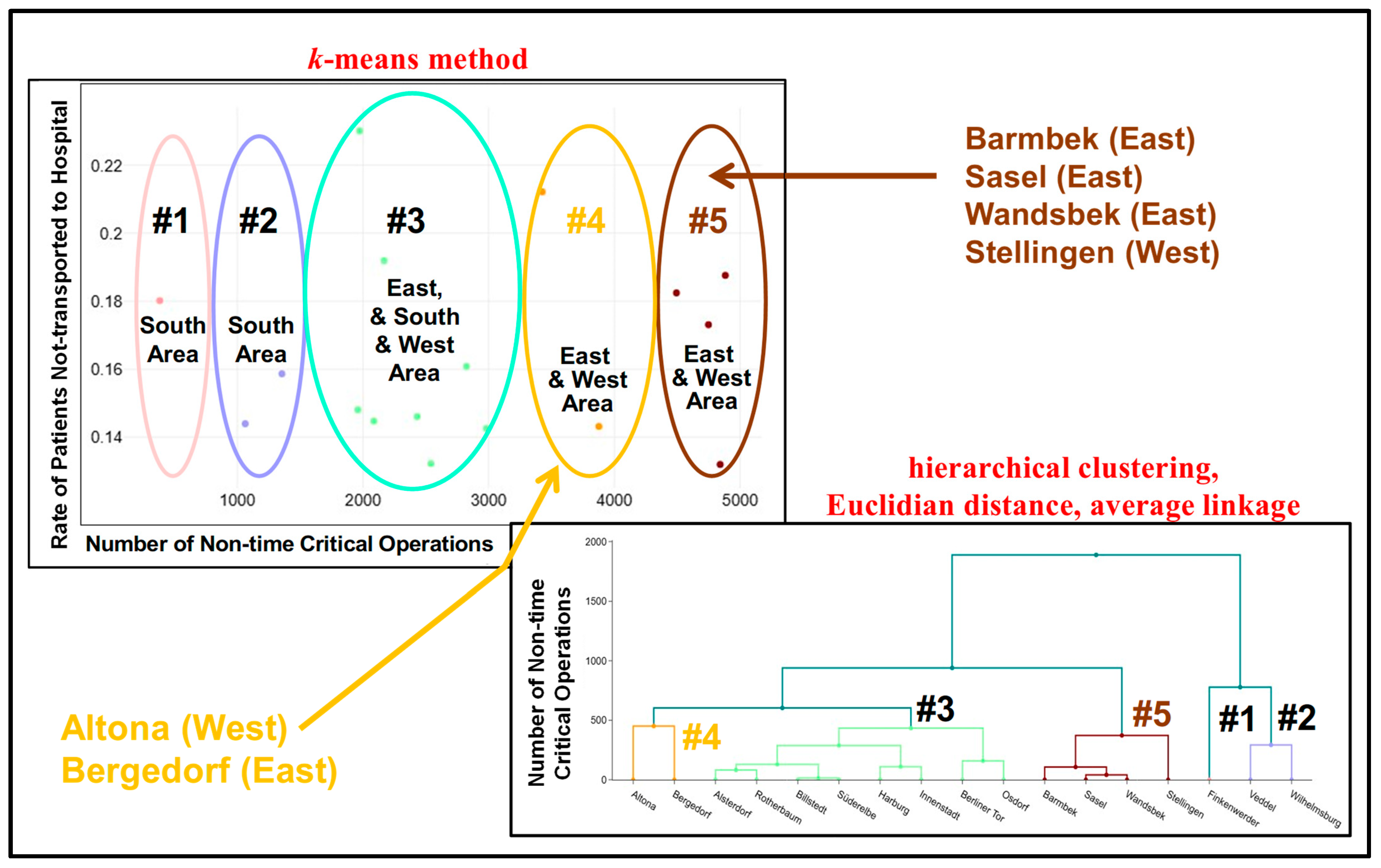
3.1.1. Area and Station Effects
3.1.2. Weekly Effects
3.1.3. Weekday Effects
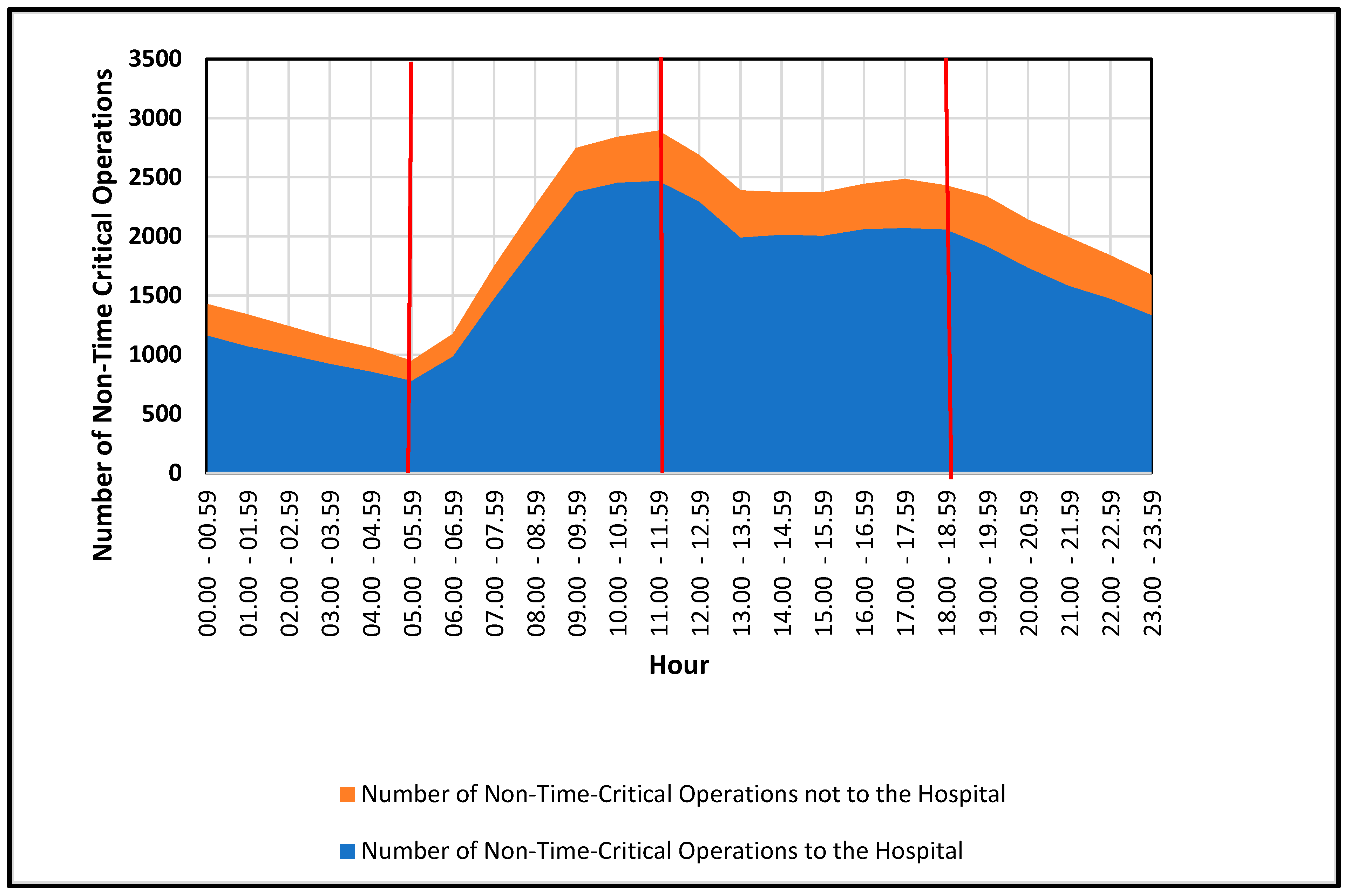
3.1.4. Time of the Day Effects
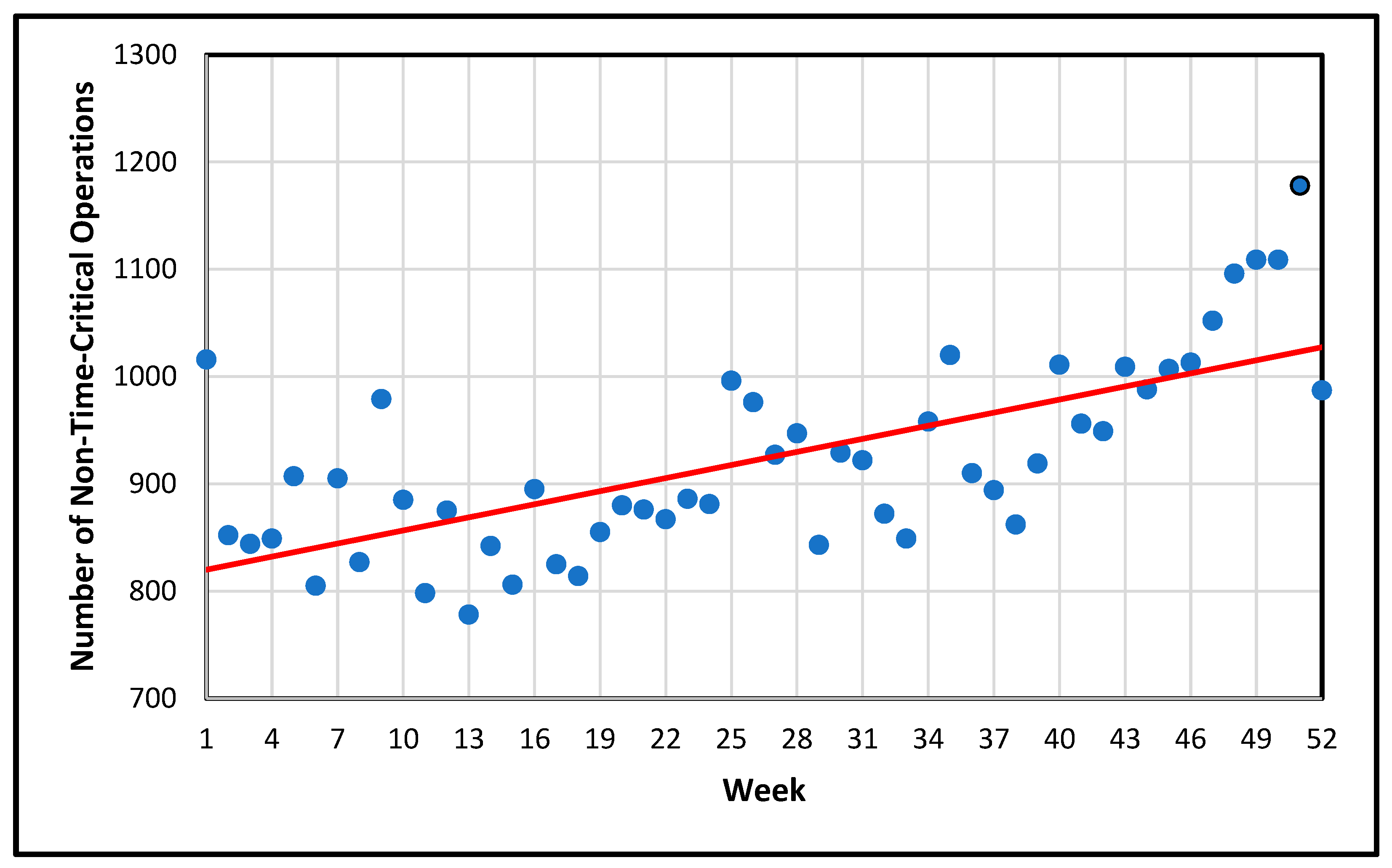
3.1.5. Time Series Effects
Overview of the Prophet Model
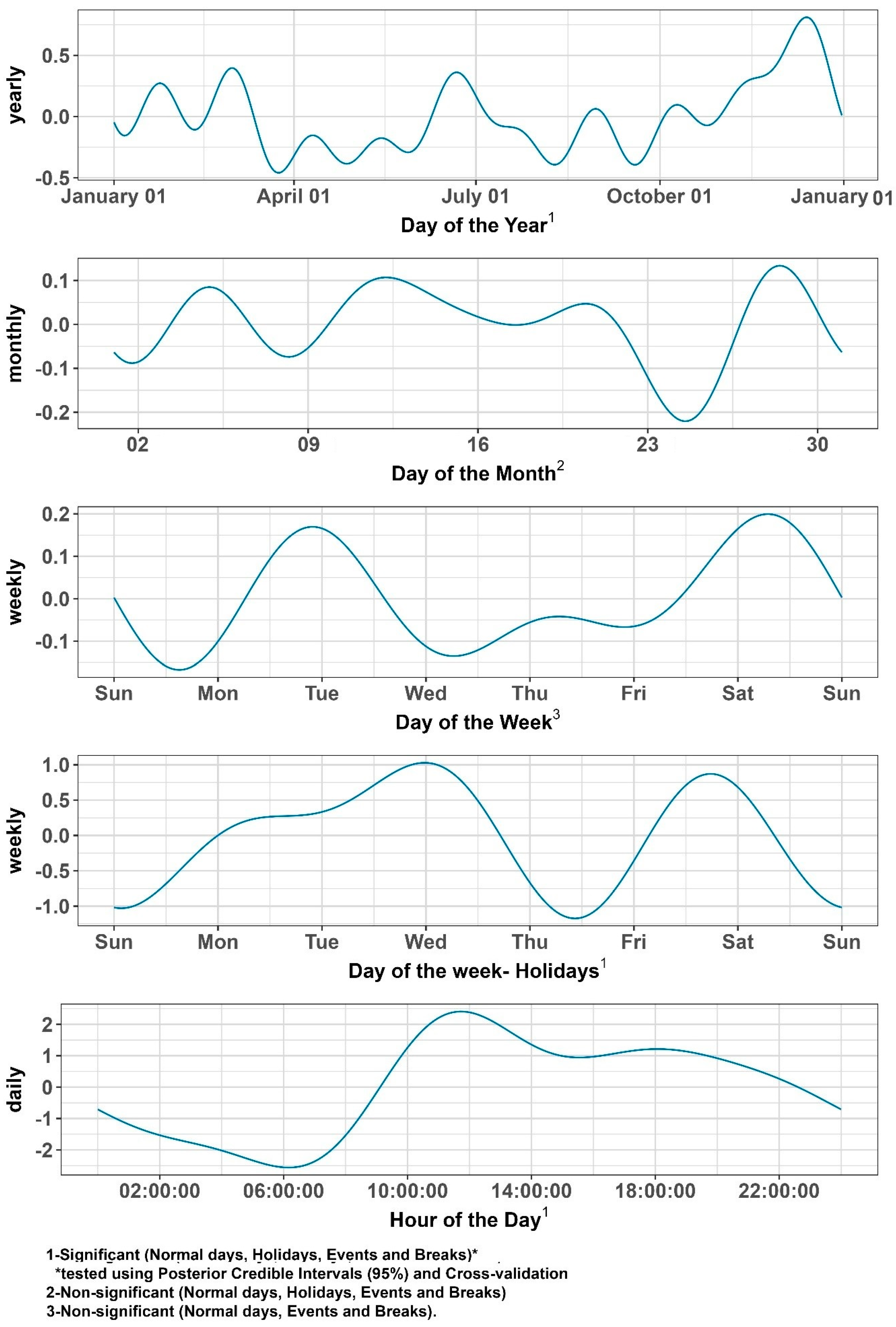
- g(t), trend: To capture any trend effects, the Prophet model uses a piecewise linear specification that accommodates “changepoints” (dates when the slope changes), thus capturing gradual or abrupt shifts in call volume over the year. For the most part, there is no long-term increase or decrease in call volume. The trend is slightly positive, but that is due to the increase in end-of-year seasonality and is therefore non-informative.
- s(t), seasonality: To capture the multiple seasonalities needed for this analysis, the Prophet model utilizes Fourier series. Each series reflects a different cycle: daily (24 h), weekly, monthly and yearly.
- h(t), holiday or event effects: Known holidays, major events and school breaks were entered as time-limited regressors. This allows the Prophet model to estimate specific localized changes in call volumes.
- t, residual error.
Fourier Decomposition of Seasonalities
Bayesian Estimation and Posterior Credible Intervals
(Time Series) Cross-Validation
- Train on data up to a cut-off date.
- Forecast the next horizon (e.g., 14 or 30 days).
- Compare predictions to actual values using the RMSE (root mean squared error).
- Roll the cut-off forward and repeat.
Summary of the Area- and Time-Related Effects Found
- Yearly Seasonality: Informative and “significant” for all data subsets (normal days, holidays, events, school breaks). All 95% posterior credible intervals show an effect different from 0 and including them gives a much better performance when using cross-validation compared to the alternative model (one without). This shows a robust yearly pattern, with higher volumes typically around the semester break, mid-summer and pre-Christmas.
- Monthly Seasonality: Not informative under any treatment. The posterior intervals included zero, offering no consistent monthly effect. Including a monthly effect did not increase the model’s performance in terms of RMSE.
- Weekly Seasonality: Informative only when we explicitly model weeks with holidays. For normal days, breaks and event weeks, the weekly pattern was non-informative (credible intervals included zero, and the performance did not increase when doing CV).
- Daily Seasonality (24 h cycle): Informative across all categories, showing a pronounced morning-to-afternoon peak and lower overnight volumes. When comparing different treatments, the main difference among holidays, events and breaks compared to normal days is that the trend is slightly shifted left or right, which indicates an on average earlier or later start of day. The overall shape of the trend, however, remains the same.
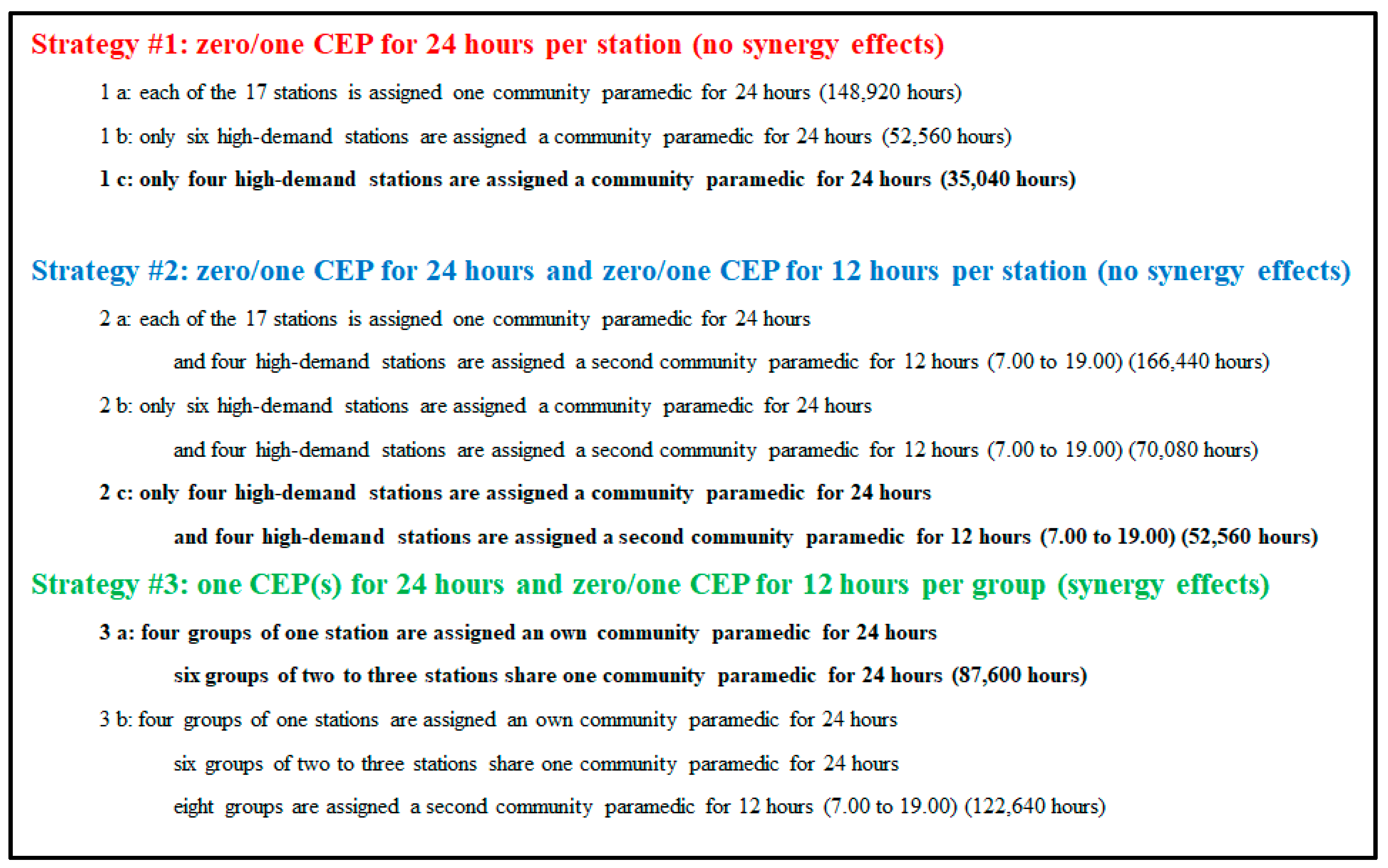
3.2. Allocation Strategies for the Community Emergency Paramedics Concept in the City of Hamburg
3.2.1. CEP Strategy #1
3.2.2. CEP Strategy #2
3.2.3. CEP Strategy #3
- Group #1: Stations Süderelbe and Finkenwerder (South area):
- one shared CEP for 24 h between these stations [a, b]
- Group #2: Stations Harburg, Veddel and Wilhelmsburg (South area):
- one shared CEP for 24 h among these stations [a, b]
- Group #3: Stations Billstedt and Bergedorf (East area):
- one shared CEP for 24 h between these stations [a, b]
- Group #4: Stations Innenstadt and Berliner Tor (East area):
- one shared CEP for 24 h between these stations [a, b]
- Group #5: Stations Altona and Osdorf (West area):
- one shared CEP for 24 h between these stations [a, b]
- Group #6: Station Rotherbaum (East area):
- one CEP for 24 h for this station alone
- Group #7: Stations Stellingen and Alsterdorf (West area):
- one shared CEP for 24 h between these stations [a, b]
- one second shared CEP from 7.00–19.00 between these stations [b]
- Groups #8, #9, and #10: Station Barmbek, Sasel and Wandsbek (East area):
- one CEP for 24 h for each of the groups [a, b]
- one second non-shared CEP from 7.00–19.00 for each of the groups [b]
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Heath, C.; Sommerfield, A.; Ungern-Sternberg, B. Resilience strategies to manage psychological distress among healthcare workers during the COVID-19 pandemic: A narrative review. Anaesthesia 2020, 75, 1364–1371. [Google Scholar] [CrossRef]
- Haldane, V.; Morgan, G. From resilient to transilient health systems: The deep transformation of health systems in response to the COVID-19 pandemic. Health Policy Plan. 2021, 36, 134–135. [Google Scholar] [CrossRef] [PubMed]
- Haldane, V.; De Foo, C.; Abdalla, S.M.; Jung, A.S.; Tan, M.; Wu, S.; Chua, A.; Verma, M.; Shrestha, P.; Singh, S.; et al. Health systems resilience in managing the COVID-19 pandemic: Lessons from 28 countries. Nat. Med. 2021, 27, 964–980. [Google Scholar] [CrossRef] [PubMed]
- Iyengar, K.; Mabrouk, A.; Jain, V.K.; Venkatesan, A.; Vaishya, R. Learning opportunities from COVID-19 and future effects on health care system. Diabetes Metab. Syndr. 2020, 14, 943–946. [Google Scholar] [CrossRef] [PubMed]
- Ridde, V.; Gautier, L.; Dagenais, C.; Chabrol, F.; Hou, R.; Bonnet, E.; David, P.M.; Cloos, P.; Duhoux, A.; Lucet, J.-C.; et al. Learning from public health and hospital resilience to the SARS-CoV-2 pandemic: Protocol for a multiple case study (Brazil, Canada, China, France, Japan, and Mali). Health Res. Policy Syst. 2021, 19, 76. [Google Scholar] [CrossRef]
- Behrens, D.A.; Rauner, M.S.; Sommersguter-Reichmann, M. Why Resilience in Health Care Systems is More than Coping with Disasters: Implications for Health Care Policy. Schmalenbach J. Bus. Res. 2022, 74, 465–495. [Google Scholar] [CrossRef]
- Swyter, B. Optimierung des Ressourcenmanagements im Rettungsdienst: Gemeindenotfallsanitäter als innovative Lösung zur Bewältigung nicht-zeitkritischer Einsätze in der Freien und Hansestadt Hamburg. Master’s Thesis, University of Vienna, Vienna, Austria, 12 July 2023. [Google Scholar]
- Wagner, B. Der Hamburger Rettungsdienst und Seine Geschichte: 160 Jahre Zwischen Behörde und Ehrenamt; Diplomica Verlag: Hamburg, Germany, 2013. [Google Scholar]
- Dahmen, J.; Brettschneider, P.; Poloczek, S.; Pommerenke, C.; Wollenhaupt, L.; Breuer, L. Warum wird der Notruf 112 gewählt?—Befragung zum Notrufverhalten der Berliner Bevölkerung. Notfall+ Rettungsmed. 2024, 27, 42–50. [Google Scholar] [CrossRef]
- Seeger, I.; Klausen, A.; Thate, S.; Flake, F.; Peters, O.; Rempe, W.; Peter, M.; Scheinichen, F.; Günther, U.; Röhrig, R.; et al. Gemeindenotfallsanitäter als innovatives Einsatzmittel in der Notfallversorgung—Erste Ergebnisse einer Beobachtungsstudie. Notfall Rettungsmed. 2021, 24, 194–202. [Google Scholar] [CrossRef]
- Bradley, P. Taking Healthcare to the Patient: Transforming NHS Ambulance Services; Department of Health: London, UK, 2005. [Google Scholar]
- Hänninen, J.; Kouvonen, A.; Sumanen, H. Patients Seeking Retreatment after Community emergency paramedic Assessment and Treatment: Piloting a Community emergency paramedic Unit Program in Southwest Finland. Nurs. Rep. 2020, 10, 66–74. [Google Scholar] [CrossRef]
- Agarwal, G.; Angeles, R.; Pirrie, M.; McLeod, B.; Marzanek, F.; Parascandalo, J.; Thabane, L. Reducing 9-1-1 emergency medical service calls by implementing a community emergency paramedicine program for vulnerable older adults in public housing in Canada: A multi-site cluster randomized controlled trial. Prehosp. Emerg. Care 2019, 23, 718–729. [Google Scholar] [CrossRef]
- Rural Health Information Hub. Mobile Integrated Healthcare Network (MIHN). Available online: https://www.ruralhealthinfo.org/project-examples/1119 (accessed on 15 June 2024).
- Hoikka, M.; Silfvast, T.; Ala-Kokko, T.I. A high proportion of prehospital emergency patients are not transported by ambulance: A retrospective cohort study in Northern Finland. Acta Anaesthesiol. Scand. 2017, 61, 549–556. [Google Scholar] [CrossRef] [PubMed]
- Gregg, A.; Tutek, J.; Leatherwood, M.D.; Crawford, W.; Friend, R.; Crowther, M.; McKinney, R. Systematic review of community paramedicine and EMS mobile integrated health care interventions in the United States. Popul. Health Manag. 2019, 22, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Thurman, W.A.; Moczygemba, L.R.; Tormey, K.; Hudzik, A.; Welton-Arndt, L.; Okoh, C. A scoping review of community paramedicine: Evidence and implications for interprofessional practice. J. Interprof. Care 2021, 35, 229–239. [Google Scholar] [CrossRef]
- Lauer, D.; Bandlow, S.; Rathje, M.; Seidl, A.; Karutz, H. Veränderungen und Entwicklungen in der präklinischen Notfallversorgung: Zentrale Herausforderungen für das Rettungsdienstmanagement [Changes and developments in emergency medical services: Key challenges for rescue management]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2022, 65, 987–995. [Google Scholar] [CrossRef]
- Redelsteiner, C. Community Care. Eine Systementlastung für den Rettungsdienst. Rettungsdienst 2023, 46, 28–32. [Google Scholar]
- Redelsteiner, C. Die eigene professionelle Altersversorgung sichern-der Rettungsdienst als mobiler Sozial-und Gesundheitsdienstleister. Notfall Rettungsmed. 2024, 27, 517–520. [Google Scholar] [CrossRef]
- Passet, H.; Richter, S. Projekt NotSan-Erkunder. Einsatzkräfte für das Frankfurter Bahnhofsviertel. Rettungsdienst 2023, 46, 34–37. [Google Scholar]
- Blum, M.; Redelsteiner, C.; Konertz, M.; Danneberg, S. Projekt HanseSani in Bremen: Wenn der Rettungsdienst zu “einfachen“ Einsätzen gerufen wird. Rettungsdienst 2023, 46, 38–41. [Google Scholar]
- Günther, A.; Schmid, S.; Bruns, A.; Kleinschmidt, T.; Bartkiewicz, T.; Harding, U. Ambulante Kontakte mit dem Rettungsdienst. Notfall Rettungsmed. 2017, 20, 477–485. [Google Scholar] [CrossRef]
- Dittrich, T.; Lippert, H. Die Reform der Notfallversorgung—Kann der Gemeinde-Notfallsanitäter zur Problemlösung beitragen? GesundheitsRecht 2023, 22, 15–19. [Google Scholar] [CrossRef]
- Seeger, I.; Klausen, A.D.; Günther, U.; Bienzeisler, J.; Schnack, H.; Lubasch, J.S. Reasons for non-participation in a patient survey in the context of prehospital emergency medical care by community emergency paramedics—A retrospective observational study. Z. Evidenz Fortbild. Qual. Gesundheitswesen 2024, 187, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Auricchio, A.; Gianquintieri, L.; Burkart, R.; Benvenuti, C.; Muschietti, S.; Peluso, S.; Mira, A.; Moccetti, T.; Caputo, M.L. Real-life time and distance covered by lay first responders alerted by means of smartphone-application: Implications for early initiation of cardiopulmonary resuscitation and access to automatic external defibrillators. Resuscitation 2019, 141, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Wanner, G.; Burch, K. EMS Community Paramedicine and Mobile Integrated Health. StatPearls. 2024. Available online: https://www.statpearls.com/point-of-care/158738 (accessed on 15 June 2024).
- Leszczyński, P.K.; Sobolewska, P.; Muraczyńska, B.; Gryz, P.; Kwapisz, A. Impact of COVID-19 pandemic on quality of health services provided by emergency medical services and emergency departments in the opinion of patients: Pilot study. Int. J. Environ. Res. Public Health 2022, 19, 1232. [Google Scholar] [CrossRef] [PubMed]
- Kruskal, W.H.; Wallis, W.A. Use of Ranks in One-Criterion Variance Analysis. J. Am. Stat. Assoc. 1952, 47, 583–621. [Google Scholar] [CrossRef]
- Bonferroni, C. Teoria statistica delle classi e calcolo delle probabilita. Pubbl. Ist. Super. Sci. Econ. Commericiali Firenze 1936, 8, 3–62. [Google Scholar]
- Dunn, O.J. Multiple comparisons among means. J. Am. Stat. Assoc. 1961, 56, 52–64. [Google Scholar] [CrossRef]
- Durbin, J.; Watson, G.S. Testing for Serial Correlation in Least Squares Regression. I. In Breakthroughs in Statistics: Methodology and Distribution; Springer: New York, NY, USA, 1992; pp. 237–259. [Google Scholar]
- Durbin, J.; Watson, G.S. Testing for Serial Correlation in Least Squares Regression. II. In Breakthroughs in Statistics: Methodology and Distribution; Springer: New York, NY, USA, 1992; pp. 260–266. [Google Scholar]
- Spearman, C. The proof and measurement of association between two things. Am. J. Psychol. 1987, 100, 441–471. [Google Scholar] [CrossRef]
- Sokal, R.R.; Michener, C.D. A statistical method for evaluating systematic relationships. Univ. Kans. Sci. Bull. 1958, 38, 1409–1438. [Google Scholar]
- Taylor, S.J.; Letham, B. Forecasting at scale. Am. Stat. 2018, 72, 37–45. [Google Scholar] [CrossRef]
- Fourier, J.B.J. Théorie Analytique de la Chaleur; Gauthier-Villars: Paris, France, 1888; Volume 1. [Google Scholar]
- Betancourt, M. A conceptual introduction to Hamiltonian Monte Carlo. arXiv 2017, arXiv:1701.02434. [Google Scholar]
- Gelman, A.; Carlin, J.B.; Stern, H.S.; Dunson, D.B.; Vehtari, A.; Rubin, D.B. Bayesian Data Analysis, 3rd ed.; Chapman & Hall/CRC: Boca Raton, FL, USA, 2013. [Google Scholar]
- World Health Organization. With the International Public Health Emergency Ending, WHO/Europe Launches Its Transition Plan for COVID-19. Available online: https://www.who.int/europe/news/item/12-06-2023-with-the-international-public-health-emergency-ending--who-europe-launches-its-transition-plan-for-covid-19 (accessed on 3 June 2024).
- Burns, R.B. The Human Impact of the COVID-19 Pandemic: A Review of International Research; Springer Nature Singapore Pte Ltd.: Singapore, 2023. [Google Scholar]
- Khalil-Khan, A.; Khan, M.A. The Impact of COVID-19 on Primary Care: A Scoping Review. Cureus 2023, 15, e33241. [Google Scholar] [CrossRef] [PubMed]
- Torrance, N.; MacIver, E.; Adams, N.N.; Skåtun, D.; Scott, N.; Kennedy, C.; Douglas, F.; Hernandez-Santiago, V.; Grant, A. Lived experience of work and long COVID in healthcare staff. Occup. Med. 2024, 74, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Schmiedel, R.; Behrendt, H.; Betzler, E. Bedarfsplanung im Rettungsdienst, 1st ed.; Springer: Berlin, Germany, 2004; pp. 73–167. [Google Scholar]
- Hunink, M.M.; Weinstein, M.C.; Wittenberg, E.; Drummond, M.F.; Pliskin, J.S.; Wong, J.B.; Glasziou, P.P. Decision Making in Health and Medicine: Integrating Evidence and Values; Cambridge University Press: Cambridge, UK, 2014. [Google Scholar]
- Brailsford, S.C.; Harper, P.R.; Patel, B.; Pitt, M. An analysis of the academic literature on simulation and modelling in health care. J. Simul. 2009, 3, 130–140. [Google Scholar] [CrossRef]
- Brailsford, S.C.; Carter, M.W.; Jacobson, S.H. Five decades of healthcare simulation. In Proceedings of the 2017 Winter Simulation Conference (WSC), Las Vegas, NV, USA, 3–6 December 2017; pp. 365–384. [Google Scholar] [CrossRef]
- Tolk, A.; Harper, A.; Mustafee, N. Hybrid models as transdisciplinary research enablers. Eur. J. Oper. Res. 2021, 291, 1075–1090. [Google Scholar] [CrossRef] [PubMed]
- Masmoudi, M.; Jarboui, B.; Siarry, P. (Eds.) Operations Research and Simulation in Healthcare; Springer International Publishing: Cham, Switzerland, 2021. [Google Scholar]
- Wang, L.; Demeulemeester, E. Simulation optimization in healthcare resource planning: A literature review. Iise Trans. 2023, 55, 985–1007. [Google Scholar] [CrossRef]
- Aringhieri, R.; Bruni, M.E.; Khodaparasti, S.; van Essen, J.T. Emergency medical services and beyond: Addressing new challenges through a wide literature review. Comput. Oper. Res. 2017, 78, 349–368. [Google Scholar] [CrossRef]
- Reuter-Oppermann, M.; van den Berg, P.L.; Vile, J.L. Logistics for emergency medical service systems. Health Syst. 2017, 6, 187–208. [Google Scholar] [CrossRef]
- Aringhieri, R.; Hirsch, P.; Rauner, M.S.; Reuter-Oppermanns, M.; Sommersguter-Reichmann, M. Operations research applied to health services (ORAHS) in Europe: General trends and ORAHS 2020 conference in Vienna, Austria. Cent. Eur. J. Oper. Res. 2022, 30, 1–18. [Google Scholar] [CrossRef]
- Matinrad, N.; Reuter-Oppermann, M. A review on initiatives for the management of daily medical emergencies prior to the arrival of emergency medical services. Cent. Eur. J. Oper. Res. 2022, 30, 251–302. [Google Scholar] [CrossRef]
- Neira-Rodado, D.; Escobar-Velasquez, J.W.; McClean, S. Ambulances Deployment Problems: Categorization, Evolution and Dynamic Problems Review. ISPRS Int. J. Geo-Inf. 2022, 11, 109. [Google Scholar] [CrossRef]
- Klein, T.L.; Thielen, C. Improving patient transport in hospitals: A literature review of operations research methods. arXiv 2024, arXiv:2404.03282. [Google Scholar] [CrossRef]
| Variable | Type | Number [Range] |
|---|---|---|
| Stations | Categorial | 17 [1 = Altona,…, 17 = Wandsbek] |
| Months | Ordinal | 12 [1 = January,…, 12 = December] |
| Weeks | Ordinal | 52 [1…52] |
| Day of the Year | Numeric [Time Series] | 365 [t0 = 1 January, …, t364 = 31 December] |
| Days of the Week | Ordinal | 1 [1 = Monday,…, 7 = Saturday] |
| Hours of the Day | Ordinal | 24 [1 = “0.00–0.59”,…, 24 = “23.00–23.59”] |
| Breaks | Binary | [1 = true, 0 = false] |
| Events | Binary | [1 = true, 0 = false] |
| Holidays | Binary | [1 = true, 0 = false] |
| Station | Abbrevation Station | Area | Population Size | Area Size in km2 | Population Density Per km2 |
|---|---|---|---|---|---|
| Altona | Alo | West | 70,791 | 11.42 | 6199.41 |
| Alsterdorf | Als | West | 152,952 | 41.88 | 3652.06 |
| Barmbek | Bar | East | 170,752 | 25.265 | 6761.12 |
| Bergedorf | Beg | East | 114,212 | 129.25 | 883.68 |
| Berliner Tor | Bet | East | 78,123 | 13.37 | 5841.85 |
| Billstedt | Bil | East | 56,125 | 57.38 | 978.19 |
| Finkenwerder | Fin | South | 12,846 | 56.18 | 228.64 |
| Harburg | Har | South | 109,213 | 47.08 | 2319.73 |
| Innenstadt | Inn | West | 21,607 | 6.87 | 3145.58 |
| Osdorf | Osd | West | 204,793 | 57.69 | 3550.01 |
| Rotherbaum | Rot | West | 109,294 | 11.01 | 9928.60 |
| Sasel | Sas | East | 169,192 | 86.42 | 1957.72 |
| Stellingen | Ste | West | 272,006 | 49.08 | 5542.67 |
| Süderelbe | Sue | South | 58,611 | 59.26 | 989.07 |
| Veddel | Ved | South | 22,271 | 24.72 | 901.11 |
| Wandsbek | Wan | East | 123,594 | 45.39 | 2722.76 |
| Wilhelmsburg | Wil | South | 51,689 | 26.60 | 1942.90 |
| Average in East Area | East | 51,689 | 47.08 | 1276.29 | |
| Average in South Area | South | 118,666 | 59.51 | 3190.87 | |
| Average in West Area | West | 138,574 | 29.66 | 5336.39 | |
| Average per Station | 105,769 | 44.05 | 3385.00 | ||
| Hamburg Area (Total) | 1,798,071 | 748.85 | 2401.10 |
| Station | Area | Number of Non-Time-Critical Operations | ||||
|---|---|---|---|---|---|---|
| Total Number | With Transportation to Hospital | Without Transportation to Hospital | ||||
| Number | % | Number | % | |||
| Altona | West | 3877 | 3322 | 85.68% | 555 | 16.71% |
| Alsterdorf | West | 2168 | 1752 | 80.81% | 416 | 23.74% |
| Barmbek | East | 4749 | 3927 | 82.69% | 822 | 20.93% |
| Bergedorf | East | 3426 | 2699 | 78.78% | 727 | 26.94% |
| Berliner Tor | East | 2823 | 2369 | 83.92% | 454 | 19.16% |
| Billstedt | East | 1973 | 1519 | 76.99% | 454 | 29.89% |
| Finkenwerder | South | 383 | 314 | 81.98% | 69 | 21.97% |
| Harburg | South | 2431 | 2076 | 85.40% | 355 | 17.10% |
| Innenstadt | West | 2541 | 2205 | 86.78% | 336 | 15.24% |
| Osdorf | West | 2982 | 2557 | 85.75% | 425 | 16.62% |
| Rotherbaum | West | 2086 | 1784 | 85.52% | 302 | 16.93% |
| Sasel | East | 4842 | 4203 | 86.80% | 639 | 15.20% |
| Stellingen | West | 4494 | 3674 | 81.75% | 820 | 22.32% |
| Süderelbe | South | 1959 | 1669 | 85.20% | 290 | 17.38% |
| Veddel | South | 1063 | 910 | 85.61% | 153 | 16.81% |
| Wandsbek | East | 4883 | 3967 | 81.24% | 916 | 23.09% |
| Wilhelmsburg | South | 1355 | 1140 | 84.13% | 215 | 18.86% |
| Average per Station | 2825.59 | 2358.06 | 83.47% | 467.53 | 19.93% | |
| Average in East Area | 22,696 | 18,684 | 82.32% | 4012 | 17.68% | |
| Average in South Area | 7191 | 6109 | 84.95% | 1082 | 15.05% | |
| Average in West Area | 18,148 | 15,294 | 84.27% | 2854 | 15.73% | |
| Total | 292,856 (100%) | 48,035 (16.40%) | 40,087 (13.68%) | 100% | 7948 (2.71%) | 100% |
| Weekday | Number of Non-Time-Critical Operations | Percentage of Non-Time-Critical Operations |
|---|---|---|
| Monday | 7125 | 14.83% |
| Tuesday | 6959 | 14.49% |
| Wednesday | 6599 | 13.74% |
| Thursday | 6833 | 14.23% |
| Friday | 6812 | 14.18% |
| Saturday | 6973 | 14.52% |
| Sunday | 6734 | 14.02% |
| Average per day | 6862.14 | 14.29% |
| Total | 48.035 | 100.00% |
| Hourly Time Slot | Average Rate of Non-Time-Critical Operations | Operation Time (in Minutes) | Average Demand (in Minutes) | Number of Community Paramedics | Supply (in Minutes) | Average Workload [Demand/Supply] (%) |
|---|---|---|---|---|---|---|
| 00.00–00.59 | 0.3534 | 60 | 21.21 | 1 | 60 | 35.34% |
| 01.00–01.59 | 0.3370 | 60 | 20.21 | 1 | 60 | 33.70% |
| 02.00–02.59 | 0.3233 | 60 | 19.40 | 1 | 60 | 32.33% |
| 03.00–03.59 | 0.2301 | 60 | 13.81 | 1 | 60 | 23.01% |
| 04.00–04.59 | 0.2767 | 60 | 16.60 | 1 | 60 | 27.67% |
| 05.00–05.59 | 0.2356 | 60 | 14.14 | 1 | 60 | 23.56% |
| 06.00–06.59 | 0.3452 | 60 | 20.71 | 1 | 60 | 34.52% |
| 07.00–07.59 | 0.4740 | 60 | 28.44 | 1 | 60 | 47.40% |
| 08.00–08.59 | 0.6548 | 60 | 39.29 | 1 | 60 | 65.48% |
| 09.00–09.59 | 0.7562 | 60 | 45.37 | 1 | 60 | 75.62% |
| 10.00–10.59 | 0.8877 | 60 | 53.26 | 1 | 60 | 88.77% (*) |
| 11.00–11.59 | 0.8301 | 60 | 49.81 | 1 | 60 | 83.01% |
| 12.00–12.59 | 0.7616 | 60 | 45.70 | 1 | 60 | 76.16% |
| 13.00–13.59 | 0.7397 | 60 | 44.38 | 1 | 60 | 73.97% |
| 14.00–14.59 | 0.7178 | 60 | 43.07 | 1 | 60 | 71.78% |
| 15.00–15.59 | 0.6110 | 60 | 36.66 | 1 | 60 | 61.10% |
| 16.00–16.59 | 0.7699 | 60 | 46.19 | 1 | 60 | 76.99% |
| 17.00–17.59 | 0.7178 | 60 | 43.07 | 1 | 60 | 71.78% |
| 18.00–18.59 | 0.6247 | 60 | 37.48 | 1 | 60 | 62.47% |
| 19.00–19.59 | 0.6575 | 60 | 39.45 | 1 | 60 | 65.75% |
| 20.00–20.59 | 0.5945 | 60 | 35.67 | 1 | 60 | 59.45% |
| 21.00–21.59 | 0.5534 | 60 | 33.21 | 1 | 60 | 55.34% |
| 22.00–22.59 | 0.4466 | 60 | 26.80 | 1 | 60 | 44.66% |
| 23.00–23.59 | 0.4685 | 60 | 28.11 | 1 | 60 | 46.85% |
| Total | 0.5569 (average) | 1400 (sum) | 1 | 1440 (sum) | 55.70% (average) |
| Station | Average Hourly Workload Strategy #1 in 2019 | Feasibility 2019 | Feasibility 2021 |
|---|---|---|---|
| Altona [b] | 44.26% | sufficient | sufficient |
| Alsterdorf [a] | 24.75% | sufficient | sufficient |
| Barmbek [b, c] | 54.19% | sufficient | 6 time slots over 85% and 1 time slot over 100% |
| Bergedorf [b] | 39.09% | sufficient | sufficient |
| Berliner Tor [a] | 32.23% | sufficient | sufficient |
| Billstedt [a] | 22.51% | sufficient | sufficient |
| Finkenwerder [a] | 4.37% | sufficient | sufficient |
| Harburg [a] | 27.73% | sufficient | sufficient |
| Innenstadt [a] | 28.98% | sufficient | sufficient |
| Osdorf [a] | 34.03% | sufficient | sufficient |
| Rotherbaum [a] | 23.79% | sufficient | sufficient |
| Sasel [b, c] | 55.26% | 1 time slot over 85% | 1 time slot over 85% and 3 time slots over 100% |
| Stellingen [b, c] | 51.27% | sufficient | 3 time slots over 85% |
| Süderelbe [a] | 22.35% | sufficient | sufficient |
| Veddel [a] | 12.13% | sufficient | sufficient |
| Wandsbek [b, c] * | 55.70% | 1 time slot over 85% | 6 time slots over 85% and 2 time slots over 100% |
| Wilhelmsburg [b, c] | 15.47% | sufficient | sufficient |
| Groups | Average Hourly Workload Strategy #3 [a] (Feasibility in 2019 and 2021) | Average Hourly Workload Strategy #3 [b] (Feasibility in 2019 and 2021) |
|---|---|---|
| (1) Süderelbe and Finkenwerder | 26.72% | - |
| (2) Harburg, Veddel and Wilhelmsburg | 55.33% (2019: 1 > 85%; 2021: 3 > 85%, 1 > 100%) | 38.08% |
| (3) Billstedt and Bergedorf | 61.60% (2021: 8 > 85%; 2 > 100%) | 40.45% (2021: 1 > 85%) |
| (4) Innenstadt and Berliner Tor | 61.21% (2021: 10 > 85%) | 43.83% (2021: 1 > 85%) |
| (5) Altona and Osdorf | 78.29% (2019: 10 > 85%, 2 > 100%; 2021: 3 > 85%, 13 > 100%) | 55.09% (2019: 1 > 85; 2021: 3 >85%; 2 > 100%) |
| (6) Rotherbaum | 23.79% | - |
| (7) Stellingen and Alsterdorf | 76.02% (2019: 11 > 85%; 2021: 3 > 85%,12 > 100;) | 52.08% (2019: 1; 2021: 2 > 85%; 1 > 100%) |
| (8) Barmbek | 54.19% (2021: 6 > 85%; 1 > 100%) | 36.55% |
| (9) Sasel | 55.26% (2019: 1 > 85%; 2021: 3 > 85%; 3 > 100%) | 37.28% |
| (10) Wandsbek | 55.70% (2019: 1 > 85%; 2021: 6 > 85%; 2 > 100%) | 37.89% |
| CEP Strategy | Number of 24 h Community Paramedics (Area Coverage Rate) | Number of 12 h Community Paramedics | Number of Staff Hours Per Day | Number of Staff Hours Per Year * | Feasibility in 2021 |
|---|---|---|---|---|---|
| Strategy #1 [a]: one 24 h CEP for each station | 17 (100%) | 0 | 408 | 148,920 | four high-demand stations |
| Strategy #1 [b]: one 24 h CEP for the six higher-demand stations | 6 (35.3%) | 0 | 144 | 52,560 | four high-demand stations |
| Strategy #1 [c]: one 24 h CEP for the four high-demand stations | 4 (23.5%) | 0 | 96 | 35,040 | four high-demand stations |
| Strategy #2 [a]: one 24 h CEP for each station and a second 12 h one for four higher-demand stations | 17 (100%) | 4 | 456 | 166,440 | |
| Strategy #2 [b]: one 24 h CEP for six higher-demand stations and a second 12 h one for the four high-demand stations | 6 (35.3%) | 4 | 192 | 70,080 | |
| Strategy #2 [c]: one 24 h CEP for four high-demand stations and a second 12 h one for the four high-demand stations | 4 (23.5%) | 4 | 144 | 52,560 | |
| Strategy #3 [a]: one shared 24 h CEP for each group (ten groups including 17 stations) | 10 (100%) | 0 | 240 | 87,600 | high feasibility for eight groups |
| Strategy #3[b]: one shared 24 h CEP for each group and a second 12 h one for the eight higher-demand groups (ten groups including 17 stations) | 10 (100%) | 8 | 336 | 122,640 | Slight feasibility for two groups and intermediate feasibility for two groups |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rauner, M.S.; Swyter, B.; Velev, S. Assessing the Need and Demand for a Community Emergency Paramedic Strategy in the Ambulance Rescue System of Hamburg, Germany. Healthcare 2025, 13, 979. https://doi.org/10.3390/healthcare13090979
Rauner MS, Swyter B, Velev S. Assessing the Need and Demand for a Community Emergency Paramedic Strategy in the Ambulance Rescue System of Hamburg, Germany. Healthcare. 2025; 13(9):979. https://doi.org/10.3390/healthcare13090979
Chicago/Turabian StyleRauner, Marion Sabine, Benjamin Swyter, and Stefan Velev. 2025. "Assessing the Need and Demand for a Community Emergency Paramedic Strategy in the Ambulance Rescue System of Hamburg, Germany" Healthcare 13, no. 9: 979. https://doi.org/10.3390/healthcare13090979
APA StyleRauner, M. S., Swyter, B., & Velev, S. (2025). Assessing the Need and Demand for a Community Emergency Paramedic Strategy in the Ambulance Rescue System of Hamburg, Germany. Healthcare, 13(9), 979. https://doi.org/10.3390/healthcare13090979






