Implementation of a Family Skills Programme in Internally Displaced People Camps in Kachin State, Myanmar
Abstract
1. Introduction
1.1. Child Wellbeing and Caregiver Support for Displaced Populations
1.2. Family Skill Programmes
1.3. Aims and Objectives
1.4. Country Context
2. Materials and Methods
2.1. Programme Intervention
2.2. Trial Design, Sampling, Eligibility Criteria, and Sample Size
- Jaw Masat IDP Camp: This camp was established with IDP from Aung Lawt, Tanai township, and was in Jaw Masat village, Myitkyina township, Kachin state, Myanmar. The camp had a total of 137 households with 657 residents. The residents were primarily farmers, and they faced difficulties in finding job opportunities in Myitkyina. They often travelled to faraway hills and mountains to cultivate crops, particularly rice. They returned to the IDP camp once a month to receive food from the World Food Programme (WFP), and some only returned every two or three months. Most parents stayed in the camp from February to May, while the children usually attended school during the government academic year.
- Trinity IDP camp: This camp was established in 2018 as a result of air strikes due to a clash between the Myanmar military and the Kachin Independence Army that affected 27 villages. It consisted 198 households, including 52 non-camp households, with a total population of 965. Sixty percent of parents had left the IDP camp to work in the hills and mountains for sustenance, returning only once a month to queue for the food provided by the WFP at the camp.
- Njan Dung IDP camp: This camp was established in 2011 due to a clash between the Myanmar military and the Kachin Independence Army. It was located in Njang Dung ward, Myitkyina township, Kachin State, Myanmar. The residents of the camps were from over 10 villages, with a significant proportion from Gara Yang village in Waimaw township. The camp hosted 73 households with over 300 residents. Approximately half of the parents worked as daily laborers within the camp vicinity, while the remaining travelled to distant locations for work, including up to the borders of China.
- Ziun IDP camp: This IDP camp was located in Alay Kone ward, Myitkyina township, and was established in 2011 due to a clash between the military and the Kachin Independence Army. Its residents were from 15 villages and comprised over 120 households and 600 residents. Most parents worked as daily labourers around/within the town, remaining close to their children in the camp.
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Recruitment, Follow-Up, and Erroneous Data
3.2. Demographics of Study Participants
3.3. Parenting and Family Adjustment Skills (PAFAS)
3.4. Strengths and Difficulties Questionnaire (SDQ)
3.5. Child and Youth Resilience Measure (CYRM-R)
4. Discussion
4.1. Overall Effect of the Strong Families Programme
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Betancourt, T.S.; Newnham, E.A.; Layne, C.M.; Kim, S.; Steinberg, A.M.; Ellis, H.; Birman, D. Trauma history and psychopathology in war-afected refugee children referred for trauma-related mental health services in the United States. J. Trauma. Stress 2012, 25, 682–690. [Google Scholar] [CrossRef] [PubMed]
- El-Khani, A.; Ulph, F.; Peters, S.; Calam, R. Syria: The challenges of parenting in refugee situations of immediate displacement. Intervention 2016, 14, 99–113. [Google Scholar] [CrossRef]
- Miller, K.E.; Koppenol-Gonzalez, G.V.; Arnous, M.; Tossyeh, F.; Chen, A.; Nahas, N.; Jordans, M.J.D. Supporting Syrian families displaced by armed confict: A pilot randomized controlled trial of the Caregiver Support Intervention. Child Abus. Negl. 2020, 106, 104512. [Google Scholar] [CrossRef] [PubMed]
- Blackmore, R.; Gray, K.M.; Boyle, J.A.; Fazel, M.; Ranasinha, S.; Fitzgerald, G.; Misso, M.; Gibson-Helm, M. Systematic review and meta-analysis: The prevalence of mental illness in child and adolescent refugees and asylum seekers. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 705–714. [Google Scholar] [CrossRef]
- Cluver, L.; Perks, B.; Rakotomalala, S.; Maalouf, W. Ukraine’s children: Use evidence to support child protection in emergencies. BMJ 2022, 376, o781. [Google Scholar] [CrossRef] [PubMed]
- Eltanamly, H.; Leijten, P.; Jak, S.; Overbeek, G. Parenting in times of war: A metaanalysis and qualitative synthesis of war exposure, parenting, and child adjustment. Trauma Violence Abus. 2021, 22, 147–160. [Google Scholar] [CrossRef]
- El-Khani, A.; Ulph, F.; Peters, S.; Calam, R. Syria: Refugee parents’ experiences and need for parenting support in camps and humanitarian settings. Vulnerable Child. Youth Stud. 2018, 13, 19–29. [Google Scholar] [CrossRef]
- Merry, L.; Pelaez, S.; Edwards, N.C. Refugees, asylumseekers and undocumented migrants and the experience of parenthood: A synthesis of the qualitative literature. Glob. Health 2017, 13, 75. [Google Scholar] [CrossRef]
- Osman, F.; Klingberg-Allvin, M.; Flacking, R.; Schön, U.-K. Parenthood in transition—Somali-born parents’ experiences of and needs for parenting support programmes. BMC Int. Health Hum. Rights 2016, 16, 7. [Google Scholar] [CrossRef]
- WHO. Violence Prevention: The Evidence. Preventing Violence Through the Development of Safe, Stable and Nurturing Relationships Between Children and Their Parents and Caregivers; WHO: Geneva, Switzerland, 2009. [Google Scholar]
- Barry, M.M. Promoting positive mental health: Theoretical frameworks for practice. Int. J. Ment. Health Promot. 2001, 3, 25–34. [Google Scholar]
- Forgatch, M.S.; Patterson, G.R.; Degarmo, D.S.; Beldavs, Z.G. Testing the Oregon delinquency model with 9-year followup of the Oregon Divorce Study. Dev. Psychopathol. 2009, 21, 637–660. [Google Scholar] [CrossRef] [PubMed]
- Gewirtz, A.H. A call for theoretically informed and empirically validated military family interventions. J. Fam. Theory Rev. 2018, 10, 587–601. [Google Scholar] [CrossRef] [PubMed]
- UNODC; WHO. International Standards on Drug Use Prevention, 2nd ed.; UNODC and WHO: Vienna, Austria, 2018. [Google Scholar]
- WHO; CDC; End Violence Against Children; PAHO; PEPFAR; Together for Girls; UNICEF; UNODC; USAID; The World Bank. INSPIRE: Seven Strategies for Ending Violence Against Children; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Wessels, I.; Mikton, C.; Ward, C.L.; Kilbane, T.; Alves, R.; Campello, G.; Dubowitz, H.; Hutchings, J.; Jones, L.; Lynch, M.; et al. Preventing Violence: Evaluating Outcomes of Parenting Programmes; WHO: Geneva, Switzerland, 2013. [Google Scholar]
- WHO; UNICEF. Helping Adolescents Thrive Toolkit: Strategies to Promote and Protect Adolescent Mental Health and Reduce Self-Harm and Other Risk Behaviours; WHO, UNICEF: Geneva, Switzerland, 2021. [Google Scholar]
- Mejia, A.; Calam, R.; Sanders, M.R. A pilot randomized controlled trial of a brief parenting intervention in low-resource settings in Panama. Prev. Sci. 2015, 16, 707–717. [Google Scholar] [CrossRef] [PubMed]
- Murphy, K.M.; Rodrigues, K.; Costigan, J.; Annan, J. Raising children in conflict: An integrative model of parenting in war. Peace Confl. J. Peace Psychol. 2017, 23, 46–52. [Google Scholar] [CrossRef]
- Mejia, A.; Emsley, R.; Fichera, E.; Maalouf, W.; Segrott, J.; Calam, R. Protecting Adolescents in Low- And Middle-Income Countries from Interpersonal Violence (PRO YOUTH TRIAL): Study Protocol for a Cluster Randomized Controlled Trial of the Strengthening Families Programme 10–14 (“Familias Fuertes”) in Panama. Trials 2018, 19, 320–340. [Google Scholar] [CrossRef]
- Gillespie, S.; Banegas, J.; Maxwell, J.; Chan, A.C.Y.; Darawshy, N.A.-S.; Wasil, A.R.; Marsalis, S.; Gewirtz, A. Parenting interventions for refugees and forcibly displaced families: A systematic review. Clin. Child Fam. Psychol. Rev. 2022, 25, 395–412. [Google Scholar] [CrossRef]
- Gonçalves Júnior, J.; de Amorim, L.M.; Neto, M.L.R.; Uchida, R.R.; de Moura, A.T.M.S.; Lima, N.N.R. The impact of “the war that drags on” in Ukraine for the health of children and adolescents: Old problems in a new conflict? Child Abus. Negl. 2022, 128, 105602. [Google Scholar] [CrossRef]
- Campello, G.; Heikkila, H.; Maalouf, W. International Standards on Drug Use Prevention: Tools to Support Policy Makers Globally to Implement an Evidence-based Prevention Response; Cambridge University Press: Cambridge, UK, 2016; pp. 134–160. [Google Scholar]
- Sandler, I. Quality and ecology of adversity as common mechanisms of risk and resilience. Am. J. Community Psychol. 2001, 29, 19–61. [Google Scholar] [CrossRef]
- Haar, K.; El-Khani, A.; Mostashari, G.; Hafezi, M.; Malek, A.; Maalouf, W. Impact of a brief family skills training programme (“Strong Families”) on parenting skills, child Psychosocial functioning, and resilience in Iran: A multisite controlled trial. Int. J. Environ. Res. Public Health 2021, 18, 11137. [Google Scholar] [CrossRef]
- Haar, K.; El-Khani, A.; Molgaard, V.; Maalouf, W. Strong families: A new family skills training programme for challenged and humanitarian settings: A single-arm intervention tested in Afghanistan. BMC Public Health 2020, 20, 634. [Google Scholar] [CrossRef]
- El-Khani, A.; Haar, K.; Stojanovic, M.; Maalouf, W. Assessing the Feasibility of Providing a Family Skills Intervention, “Strong Families”, for Refugee Families Residing in Reception Centers in Serbia. Int. J. Environ. Res. Public Health 2021, 18, 4530. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Sports. Myanmar Integrated Biological and Behavioural Surveillance Survey and Population Size Estimates among People Who Inject Drugs; 2014. Available online: https://pr-myanmar.org/sites/pr-myanmar.org/files/publication_docs/myanmar_pwid_ibbs_pse_report_300516.pdf (accessed on 30 April 2025).
- United Nations Office for the Coordination of Humanitarian Affairs. Myanmar. 2022. Available online: https://www.unocha.org/myanmar (accessed on 11 October 2024).
- United Nations Office for the Coordination of Humanitarian Affairs (OCHA). Myanmar Humanitarian Update No. 24 | 3 December 2024; OCHA: Geneva, Switzerland, 2022. [Google Scholar]
- UNODC Myanmar (United Nations, Myanmar). Baseline Assessment on Drug Use Among IDP Camps and Surrounding Communities in Three Selected Townships in Kachin State. Unpublished internal document. 2021. [Google Scholar]
- UNODC Myanmar (United Nations, Myanmar). Situation Assessment on Drug Use Prevention Program in Three Selected Townships in Kachin State. Unpublished internal document. 2020. [Google Scholar]
- Goodman, R. The Strengths and Difficulties Questionnaire: A Research Note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef] [PubMed]
- SDQ Info. Scoring the Strengths & Difficulties Questionnaire for Age 4–17 or 18+ In Scoring the SDQ; 2016. Available online: https://www.sdqinfo.org/py/sdqinfo/c0.py (accessed on 11 October 2024).
- Mon, M.-M.; Liabsuetrakul, T. Identification of psychological behaviours among children having parental HIV infection and their determinants in Myanmar: A comparative study with neighbourhood peers. Vulnerable Child. Youth Stud. 2017, 12, 33–45. [Google Scholar] [CrossRef]
- Mon, M.; Saw, S.; Nu-Oo, Y.; San, K.; Myint, W.; Aye, S.; Nge, P. Threat of HIV/AIDS in children: Social, education and health consequences among HIV orphans and vulnerable children in Myanmar. WHO South East Asia J. Public Health 2013, 2, 41–46. [Google Scholar] [CrossRef]
- Khan, N.Z.; Shilpi, A.B.; Sultana, R.; Sarker, S.; Razia, S.; Roy, B.; Arif, A.; Ahmed, M.U.; Saha, S.C.; McConachie, H. Displaced Rohingya children at high risk for mental health problems: Findings from refugee camps within Bangladesh. Child Care Health Dev. 2019, 45, 28–35. [Google Scholar] [CrossRef]
- Sanders, M.R.; Morawska, A.; Haslam, D.M.; Filus, A.; Fletcher, R. Parenting and Family Adjustment Scales (PAFAS): Validation of a brief parent-report measure for use in assessment of parenting skills and family relationships. Child Psychiatry Hum. Dev. 2014, 45, 255–272. [Google Scholar] [CrossRef]
- Jefferies, P.; McGarrigle, L.; Ungar, M. The CYRM-R: A Rasch-Validated Revision of the Child and Youth Resilience Measure. J. Evid.-Based Soc. Work 2019, 16, 70–92. [Google Scholar] [CrossRef]
- Panter-Brick, C.; Hadfield, K.; Dajani, R.; Eggerman, M.; Ager, A.; Ungar, M. Resilience in Context: A Brief and Culturally Grounded Measure for Syrian Refugee and Jordanian Host-Community Adolescents. Child Dev. 2018, 89, 1803–1820. [Google Scholar] [CrossRef]
- Resilience Research Centre. CYRM and ARM User Manual; Resilience Research Centre, Dalhousie University: Halifax, NS, USA, 2018. [Google Scholar]
- Jakobsen, J.C.; Gluud, C.; Wetterslev, J.; Winkel, P. When and how should multiple imputation be used for handling missing data in randomised clinical trials—A practical guide with flowcharts. BMC Med. Res. Methodol. 2017, 17, 162. [Google Scholar] [CrossRef]
 significant difference between t1 and t2,
significant difference between t1 and t2,  significant difference between t2 and t3,
significant difference between t2 and t3,  significant difference between t1 and t3.
significant difference between t1 and t3.
 significant difference between t1 and t2,
significant difference between t1 and t2,  significant difference between t2 and t3,
significant difference between t2 and t3,  significant difference between t1 and t3.
significant difference between t1 and t3.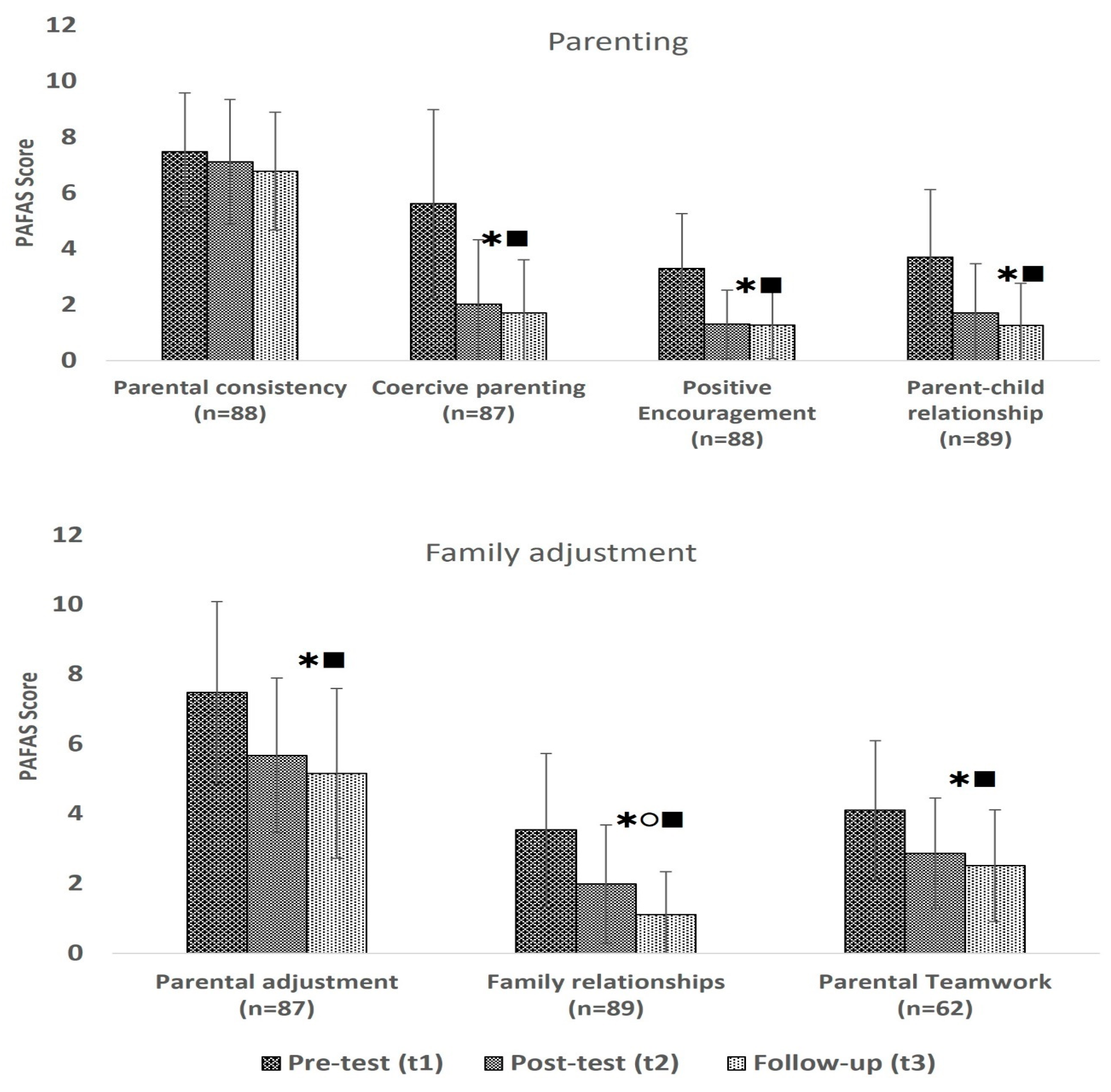
 significant difference between t1 and t2,
significant difference between t1 and t2,  significant difference between t2 and t3,
significant difference between t2 and t3,  significant difference between t1 and t3.
significant difference between t1 and t3.
 significant difference between t1 and t2,
significant difference between t1 and t2,  significant difference between t2 and t3,
significant difference between t2 and t3,  significant difference between t1 and t3.
significant difference between t1 and t3.
 significant difference between t1 and t2,
significant difference between t1 and t2,  significant difference between t1 and t3.
significant difference between t1 and t3.
 significant difference between t1 and t2,
significant difference between t1 and t2,  significant difference between t1 and t3.
significant difference between t1 and t3.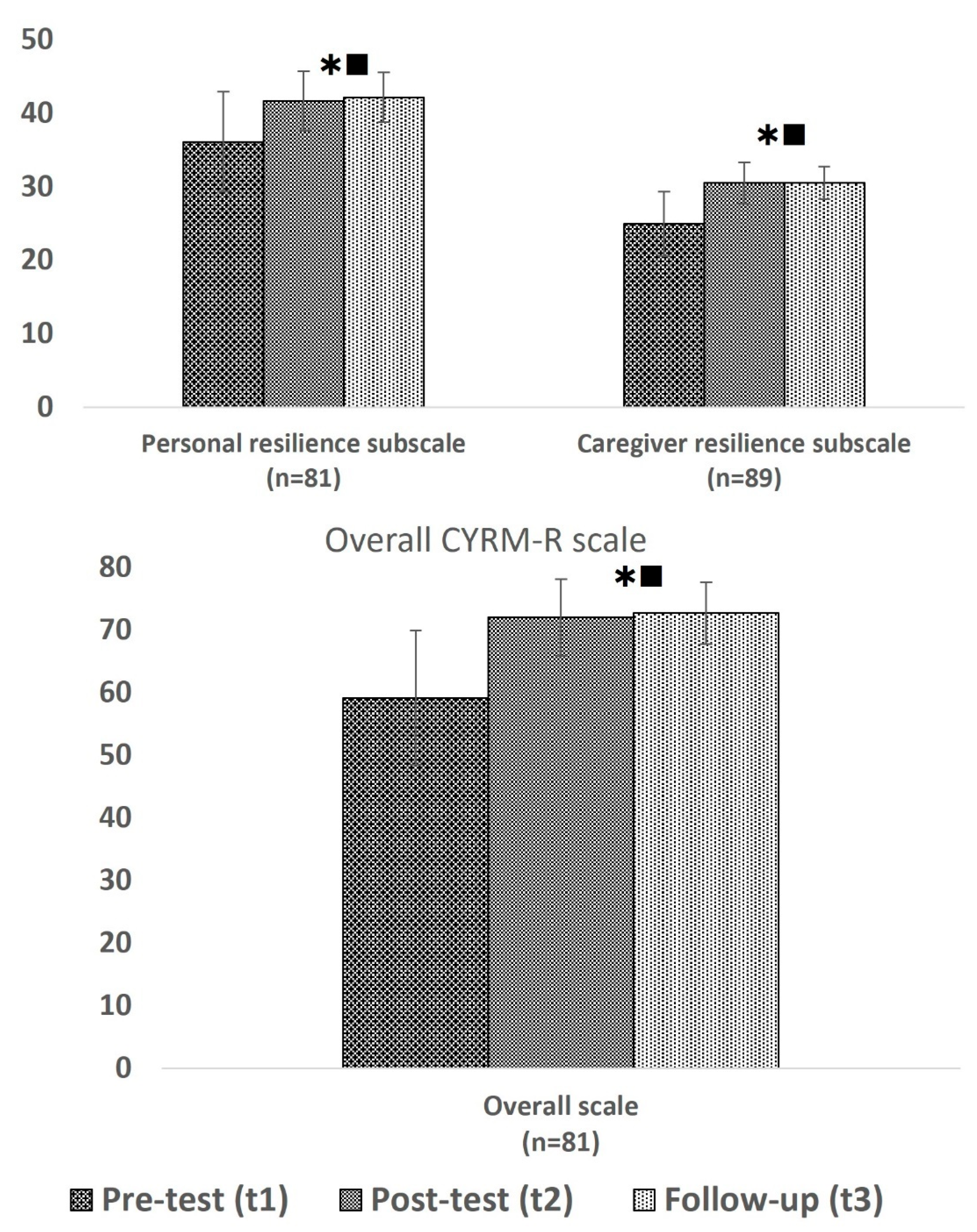
| Week 1 | Week 2 | Week 3 | ||
|---|---|---|---|---|
| Caregiver pre-session Understanding Strengths and Stresses | Caregiver session 1 Using Love and Limits | In parallel | Caregiver session 2 Teaching children what is right | In parallel |
| Child session 1 Learning about stress | Child session 2 Following rules and appreciating caregivers | |||
| Family session 1 Learning about each other | Family session 2 Supporting values and dreams | |||
| IDP Camp | Pre-Intervention t1 | Post-Intervention t2 | Follow-Up t3 |
|---|---|---|---|
| Jaw Masat n = 40 | 40 100% | 39 98% | 39 98% |
| Njang Dung n = 10 | 10 100% | 8 80% | 10 100% |
| Trinity n = 40 | 40 100% | 34 85% | 38 95% |
| Ziun n = 10 | 10 100% | 10 100% | 10 100% |
| Total n = 100 | 100 100% | 91 91% | 97 97% |
| Caregiver Demographics | Total (n = 100) | Female Caregiver (n = 96) | Male Caregiver (n = 4) | p-Value | Chi2, t-Test | |
|---|---|---|---|---|---|---|
| Mean (SD); n (%) | Mean (SD); n (%) | Mean (SD); n (%) | ||||
| Age (in years) | 41.0 (10.28) | 40.8 (10.19) | 45.8 (12.84) | 0.352 | t98 = −0.935 | |
| Marital status | Married | 80 (80%) | 77 (80%) | 3 (75%) | 0.858 | Χ2 = 0.766 |
| Divorced/separated | 5 (5%) | 5 (5%) | - | |||
| Single | 2 (2%) | 2 (2%) | - | |||
| Widow | 13 (13%) | 12 (13%) | 1 (25%) | |||
| Education | Primary school or less | 60 (60%) | 58 (60%) | 2 (50%) | <0.001 | Χ2 = 24.315 |
| Some high school | 37 (37%) | 36 (38%) | 1 (25%) | |||
| Completed high school | 1 (1%) | - | 1 (25%) | |||
| University degree | 2 (2%) | 2 (2%) | - | |||
| Partner’s education | Primary school or less | 59 (69%) | 57 (79%) | 2 (67%) | 0.972 | Χ2 = 0.056 |
| Some high school | 25 (29%) | 24 (29%) | 1 (33%) | |||
| Completed high school | 1 (1%) | 1 (1%) | - | |||
| Work status | Full time | 4 (4%) | 4 (4%) | - | 0.759 | Χ2 = 1.872 |
| Part time | 8 (8%) | 8 (8%) | - | |||
| Not working but looking for a job | 5 (5%) | 5 (5%) | - | |||
| Home based paid work | 14 (14%) | 14 (15%) | - | |||
| Not working | 69 (69%) | 65 (68%) | 4 (100%) | |||
| If working, what kind of work | Voluntary work (unpaid) | 3 (20%) | 3 (20%) | - | n/a | n/a |
| Voluntary work (paid salary monthly but counting daily basis) | 1 (7%) | 1 (7%) | - | |||
| Cash for Work (daily basis labour) | 7 (47%) | 7 (47%) | - | |||
| Others | 4 (27%) | 4 (27%) | - | |||
| Partner’s work status | Full time | 34 (42%) | 33 (42%) | 1 (33%) | 0.723 | Χ2 = 1.327 |
| Part time | 31 (38%) | 29 (37%) | 2 (67%) | |||
| Not working but looking for a job | 2 (3%) | 2 (3%) | - | |||
| Not working | 14 (17%) | 14 (18%) | - | |||
| If the partner is working, what kind of work | Voluntary work (unpaid) | 2 (3%) | 2 (3%) | - | 0.495 | Χ2 = 2.390 |
| Voluntary work (paid salary monthly but counting daily basis) | 6 (9%) | 5 (8%) | 1 (33%) | |||
| Cash for work (daily basis labour) | 37 (57%) | 36 (58%) | 1 (33%) | |||
| Others | 20 (31%) | 19 (31%) | 1 (33%) | |||
| Current difficulties in the family (Multiple answer question) | Insufficient food | 77 (79%) | 74 (79%) | 3 (75%) | ||
| Lack of job opportunities | 34 (35%) | 32 (34%) | 2 (50%) | |||
| Insufficient drinking water | 9 (9%) | 9 (10%) | - | |||
| Quarrelling with partner | 3 (3%) | 3 (3%) | - | |||
| Other (no income, education, lack of school fees, struggling alone, caring for chronic patients, poor health, lack of healthcare, narrow space, disabled child, unable to afford children’s needs, etc.) | 48 (49%) | 47 (50%) | 1 (25%) | |||
| Experienced war or armed conflict in the past | Yes | 99 (99%) | 95 (99%) | 4 (100%) | 0.837 | Χ2 = 0.042 |
| No | 1 (1%) | 1 (1%) | - | |||
| Number of children | 3.0 (1.33) | 3.0 (1.35) | 2.8 (0.50) | 0.669 | t98 = −0.428 | |
| Child demographics | Total (n = 100) | Girls (n = 54) | Boys (n = 46) | p-value | Chi2, t-test | |
| Age of child taking part in the programme (in years) | 12.1 (2.37) | 11.8 (2.26) | 12.4 (2.48) | 0.245 | t98 = 1.170 | |
| Relationship of the caregiver to the child | Mother | 84 (84%) | 46 (55%) | 38 (45%) | 0.025 | Χ2 = 12.871 |
| Father | 4 (4%) | - | 4 (100%) | |||
| Grandmother | 6 (6%) | 5 (83%) | 1 (17%) | |||
| Sister | 3 (3%) | - | 3 (100%) | |||
| Stepmother | 1 (1%) | 1 (100%) | - | |||
| Other | 2 (2%) | 2 (100%) | - | |||
| Pre-Test Family Scores | Pre-Test Mean (SD) | Post-Test Mean (SD) | Follow-Up Mean (SD) | Two-Way Mixed ANOVA F(dftime, dferror); p-Value | Repeated-Measures ANOVA F(dftime, dferror); p-Value | Post Hoc Tests | |
|---|---|---|---|---|---|---|---|
| PARENTING | |||||||
| Parental Consistency | ≥9 (n = 31) | 9.77 (0.92) | 6.65 (2.21) | 7.45 (1.91) | F(3.821,162.389) = 16.503; p < 0.001 | F(2,60) = 24.999; p < 0.001 |  |
| 7–8 (n = 29) | 7.34 (0.48) | 8.10 (2.14) | 6.72 (2.21) | F(2,56) = 4.379; p = 0.017 | |||
| ≤6 (n = 28) | 5.07 (1.05) | 6.64 (2.08) | 6.11 (2.06) | F(2,54) = 6.149; p = 0.004 |  | ||
| Coercive Parenting | ≥7 (n = 34) | 9.18 (1.59) | 3.00 (2.89) | 2.15 (1.83) | F(4,168) = 33.055; p < 0.001 | F(2,66) = 112.546; p < 0.001 |  |
| 4–6 (n = 28) | 4.89 (0.83) | 1.39 (1.66) | 1.93 (2.02) | F(2,54) = 44.419; p < 0.001 |  | ||
| ≤3 (n = 25) | 1.60 (1.19) | 1.44 (1.47) | 0.92 (1.68) | ||||
| Positive Encouragement | ≥4 (n = 38) | 5.38 (1.16) | 1.38 (1.26) | 1.41 (1.28) | F(3.795,161.272) = 36.106; p < 0.001 | F(2,66) = 135.037; p < 0.001 |  |
| 3 (n = 25) | 3.00 (0) | 1.45 (1.34) | 1.73 (1.39) | F(2,42) = 12.903; p < 0.001 |  | ||
| ≤2 (n = 35) | 1.31 (0.74) | 1.13 (1.13) | 0.84 (0.81) | ||||
| Parent–child Relationship | ≥5 (n = 31) | 6.32 (1.51) | 2.13 (1.93) | 1.19 (1.60) | F(4,172) = 31.134; p < 0.001 | F(2,60) = 77.938; p < 0.001 |  |
| 3–4 (n = 30) | 3.50 (0.51) | 1.47 (1.43) | 1.40 (1.57) | F(2,58) = 31.312; p < 0.001 |  | ||
| ≤2 (n = 28) | 1.04 (0.92) | 1.54 (1.88) | 1.18 (1.42) | ||||
| FAMILY ADJUSTMENT | |||||||
| Parental Adjustment | ≥9 (n = 29) | 10.48 (1.27) | 6.28 (2.05) | 5.48 (2.59) | F(4,168) = 17.563; p < 0.001 | F(2,56) = 50.008; p < 0.001 |  |
| 7–8 (n = 24) | 7.42 (0.50) | 5.71 (1.90) | 5.33 (2.22) | F(2,46) = 12.827; p < 0.001 |  | ||
| ≤6 (n = 34) | 4.97 (1.36) | 5.15 (2.45) | 4.76 (2.45) | ||||
| Family relationships | ≥5 (n = 27) | 6.15 (1.59) | 2.07 (2.04) | 1.30 (1.44) | F(3.787,162.848) = 23.158; p < 0.001 | F(2,52) = 50.185; p < 0.001 |  |
| 3–4 (n = 31) | 3.45 (0.51) | 2.32 (1.68) | 1.29 (1.31) | F(1.534,46.016) = 27.555; p < 0.001 |  | ||
| ≤2 (n = 31) | 1.35 (2.19) | 1.58 (1.31) | 0.77 (1.09) | F(2,60) = 4.786; p = 0.012 |  | ||
| Parental teamwork | ≥5 (n = 28) | 5.86 (1.04) | 3.11 (1.45) | 2.57 (1.53) | F(4,118) = 16.540; p < 0.001 | F(2,54) = 62.948; p < 0.001 |  |
| 3–4 (n = 20) | 3.65 (0.49) | 3.00 (1.86) | 2.70 (1.53) | ||||
| ≤2 (n = 14) | 1.29 (0.73) | 2.21 (1.31) | 2.14 (1.92) | ||||
 significant difference between t1 and t2,
significant difference between t1 and t2,  significant difference between t2 and t3,
significant difference between t2 and t3,  significant difference between t1 and t3.
significant difference between t1 and t3.| Total Difficulty Score | B | 95% CI for B | SE B | β | R2 | ΔR2 | |
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Model | 0.119 | 0.099 * | |||||
| Constant | 23.29 * | 17.456 | 29.125 | 2.935 | |||
| Age of the child | −0.613 * | −1.002 | −0.223 | 0.196 | −0.319 | ||
| Sex of the child | −1.654 | −3.487 | 0.180 | 0.922 | −0.183 | ||
| SDQ | Pre-Test Mean (SD) | Post-Test Mean (SD) | Follow-Up Mean (SD) | Two-Way Mixed ANOVA F(dftime, dferror); p-Value | Repeated-Measures ANOVA F(dftime, dferror); p-Value | Post Hoc Tests |
|---|---|---|---|---|---|---|
| Total Difficulty Scores in Children with 17 or Pre-Test More Points (High and Very High) | ||||||
| Boys (n = 10) | 19.5 (2.27) | 10.5 (7.29) | 6.5 (3.78) | F(2,30) = 0.230; p = 0.796 | F(2,18) = 18.359; p < 0.001 |  |
| Girls (n = 7) | 19.9 (3.02) | 10.0 (7.83) | 8.6 (8.06) | F(2,12) = 6.500; p = 0.012 |  | |
 significant difference between t1 and t2,
significant difference between t1 and t2,  significant difference between t1 and t3.
significant difference between t1 and t3.| Pre-Test Family Scores | Pre-Test Mean (SD) | Post-Test Mean (SD) | Follow-Up Mean (SD) | Two-Way Mixed ANOVA F(dftime, dferror); p-Value | Repeated-Measures ANOVA F(dftime, dferror); p-Value | Post Hoc Tests | |
|---|---|---|---|---|---|---|---|
| Total CYRM-R scale | 17–55 (n = 28) | 46.89 (5.59) | 71.0 (5.48) | 71.96 (5.80) | F(4,156) = 44.06; p < 0.001 | F(2,54) = 174.885; p < 0.001 |  |
| 56–65 (n = 26) | 60.69 (2.62) | 71.69 (6.89) | 73.27 (3.94) | F(1.495,37.384) = 49.986; p < 0.001 |  | ||
| 66–85 (n = 27) | 70.59 (3.52) | 73.59 (5.92) | 73.15 (4.99) | F(2,52) = 3.816; p = 0.028 | |||
| Personal resilience subscale | 10–31 (n = 26) | 26.08 (3.79) | 40.5 (4.07) | 42.0 (3.51) | F(4,156) = 34.935; p < 0.001 | F(2,50) = 124.339; p < 0.001 |  |
| 32–37 (n = 26) | 34.5 (1.68) | 41.58 (3.91) | 41.96 (3.21) | F(1.659,41.486) = 45.156; p < 0.001 |  | ||
| 38–50 (n = 29) | 40.93 (2.91) | 42.79 (3.99) | 42.48 (3.46) | n.s. | |||
| Caregiver resilience subscale | 7–22 (n = 30) | 19.97 (2.16) | 30.57 (2.54) | 30.17 (2.78) | F(4,172) = 46.731; p < 0.001 | F(2,58) = 214.782; p < 0.001 |  |
| 23–27 (n = 27) | 25.04 (1.37) | 30.15 (2.90) | 30.56 (1.76) | F(1.733,45,053) = 55.485; p < 0.001 |  | ||
| 28–35 (n = 32) | 29.53 (1.54) | 30.72 (3.02) | 30.91 (1.99) | F(1.721,53.353) = 4.172; p = 0.026 |  |
 significant difference between t1 and t2,
significant difference between t1 and t2,  significant difference between t1 and t3.
significant difference between t1 and t3.Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haar, K.; El-Khani, A.; Hawng, H.; Brang, T.T.; Mar, W.; Lynn, Z.K.K.; Maalouf, W. Implementation of a Family Skills Programme in Internally Displaced People Camps in Kachin State, Myanmar. Healthcare 2025, 13, 1090. https://doi.org/10.3390/healthcare13091090
Haar K, El-Khani A, Hawng H, Brang TT, Mar W, Lynn ZKK, Maalouf W. Implementation of a Family Skills Programme in Internally Displaced People Camps in Kachin State, Myanmar. Healthcare. 2025; 13(9):1090. https://doi.org/10.3390/healthcare13091090
Chicago/Turabian StyleHaar, Karin, Aala El-Khani, Hkawng Hawng, Tun Tun Brang, Win Mar, Zin Ko Ko Lynn, and Wadih Maalouf. 2025. "Implementation of a Family Skills Programme in Internally Displaced People Camps in Kachin State, Myanmar" Healthcare 13, no. 9: 1090. https://doi.org/10.3390/healthcare13091090
APA StyleHaar, K., El-Khani, A., Hawng, H., Brang, T. T., Mar, W., Lynn, Z. K. K., & Maalouf, W. (2025). Implementation of a Family Skills Programme in Internally Displaced People Camps in Kachin State, Myanmar. Healthcare, 13(9), 1090. https://doi.org/10.3390/healthcare13091090






