A Systematic Literature Review for Blockchain-Based Healthcare Implementations
Abstract
1. Introduction
| Ref: | Authors, Year | Research Questions/Objectives | Followed Systematic Methodology i.e., PRISMA Guidelines | Reviewing Answers Similar or Close to Proposed Questions | Identified Strengths and Weaknesses | Identified/Reported Interventions or Developments | Bias or Quality Assessment |
|---|---|---|---|---|---|---|---|
| [15] | Emeka Chukwu et al, 2020 | Yes | Yes | No | No | Yes | No |
| [16] | R. Saranya et al., 2023 | No | No | No | No | No | No |
| [17] | Reval Prabhu et al., 2023 | Yes | Yes | No | No | No | No |
| [18] | Shashank Chauhan et al., 2022 | No | No | No | Yes | No | No |
| [19] | Shweta Mittal et al., 2024 | No | No | No | No | No | No |
| [20] | Hanaa Fatoum et al., 2021 | No | No | No | No | No | No |
| [21] | Saumya Upadhyay et al., 2024 | No | Yes | No | Yes | Yes | No |
| [22] | Sarthak Dhingra et al., 2024 | Yes | No | No | Yes | Yes | No |
| [23] | Kianoush Kiania et al., 2023 | Yes | No | No | No | No | No |
| [24] | M. Kassab et al.,2021 | Yes | No | No | Yes | Yes | Yes |
| [25] | Shubhangi V Urkude et al., 2023 | No | Yes | No | No | No | No |
| [26] | Ammara Karim Noon et al., 2021 | Yes | No | No | No | Yes | No |
| [27] | Vazirani et al.,2019 | Yes | Yes | No | No | Yes | Yes |
| [28] | Huma Saeed et al., 2022 | Yes | Yes | No | No | Yes | No |
| [14] | Elangovan et al., 2022 | No | Yes | No | Yes | Yes | Yes |
| [29] | Valeria Merlo et al., 2023 | No | Yes | No | Yes | Yes | No |
| [30] | Sobiya Arsheen et al., 2021. | No | No | No | No | No | No |
| [31] | Alaa, Haddad et al., 2022 | Yes | Yes | No | Yes | Yes | No |
| Proposed SLR | Yes | Yes | Yes | Yes | Yes | Yes |
- Identify and describe recent (past 5 years) research trends on how (the use of) BC technology reshaped healthcare applications.
- Explain existing healthcare systems where BC applications are practically implemented to achieve an appropriate solution to real-world problems or digital transformation.
- Report on BC-based design and development methods applied for implementation which demonstrated the robustness and validity to achieve efficient results for healthcare applications.
- To elaborate on the strengths and weaknesses that enable or limit various BC-based healthcare applications and interventions based on evidence strengths.
- Report both qualitative and quantitative data for BC-based implementations, their data analysis or research methods, healthcare datasets, and their evaluation metrics that show validated outcomes to present and lead future research prospects in BC-based healthcare applications.
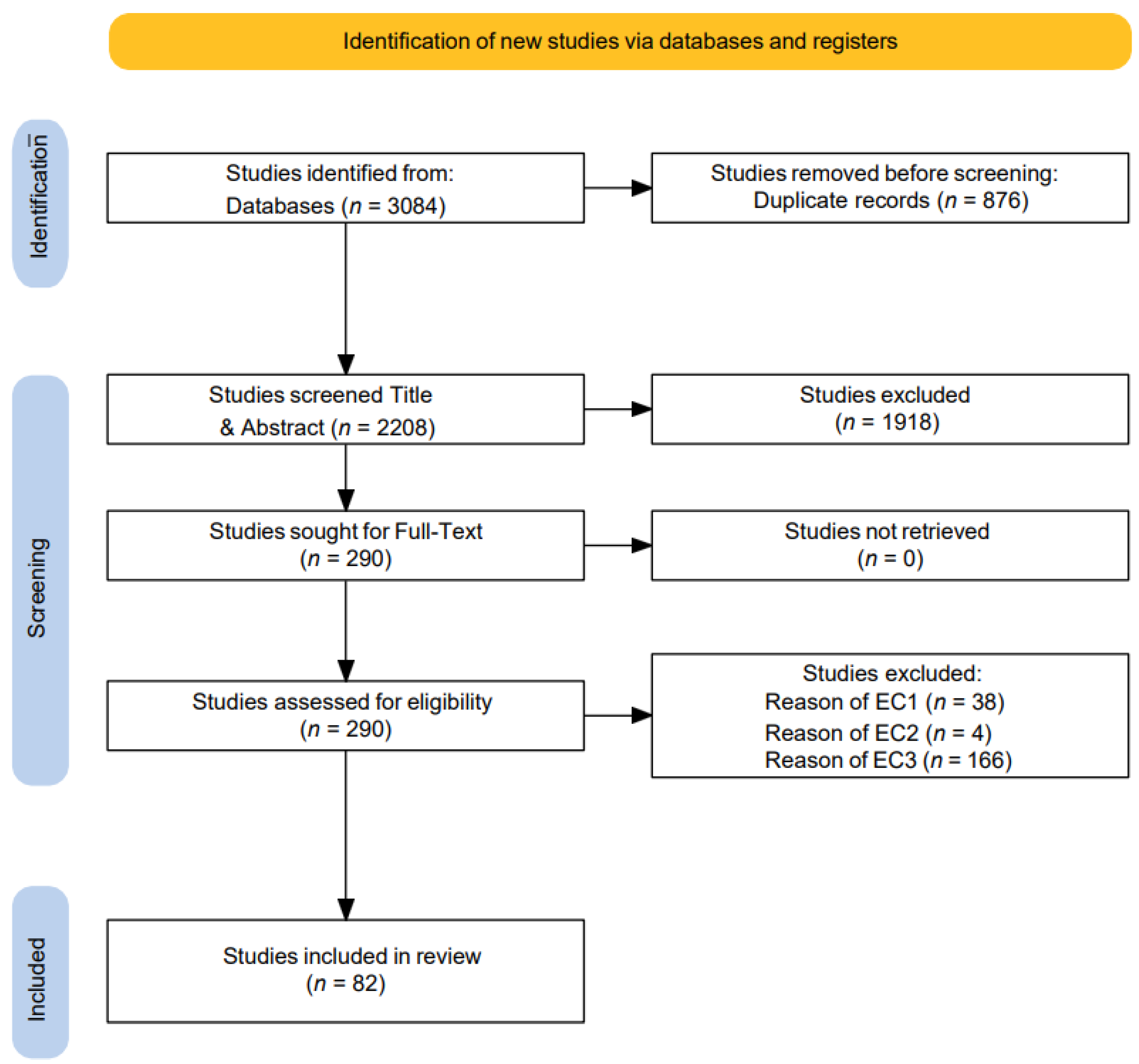
2. Methods
2.1. Search Strategy
2.2. Selection of Studies
2.3. Bias/Quality Assessment and Critical Appraisal
2.4. Data Extraction and Synthesis
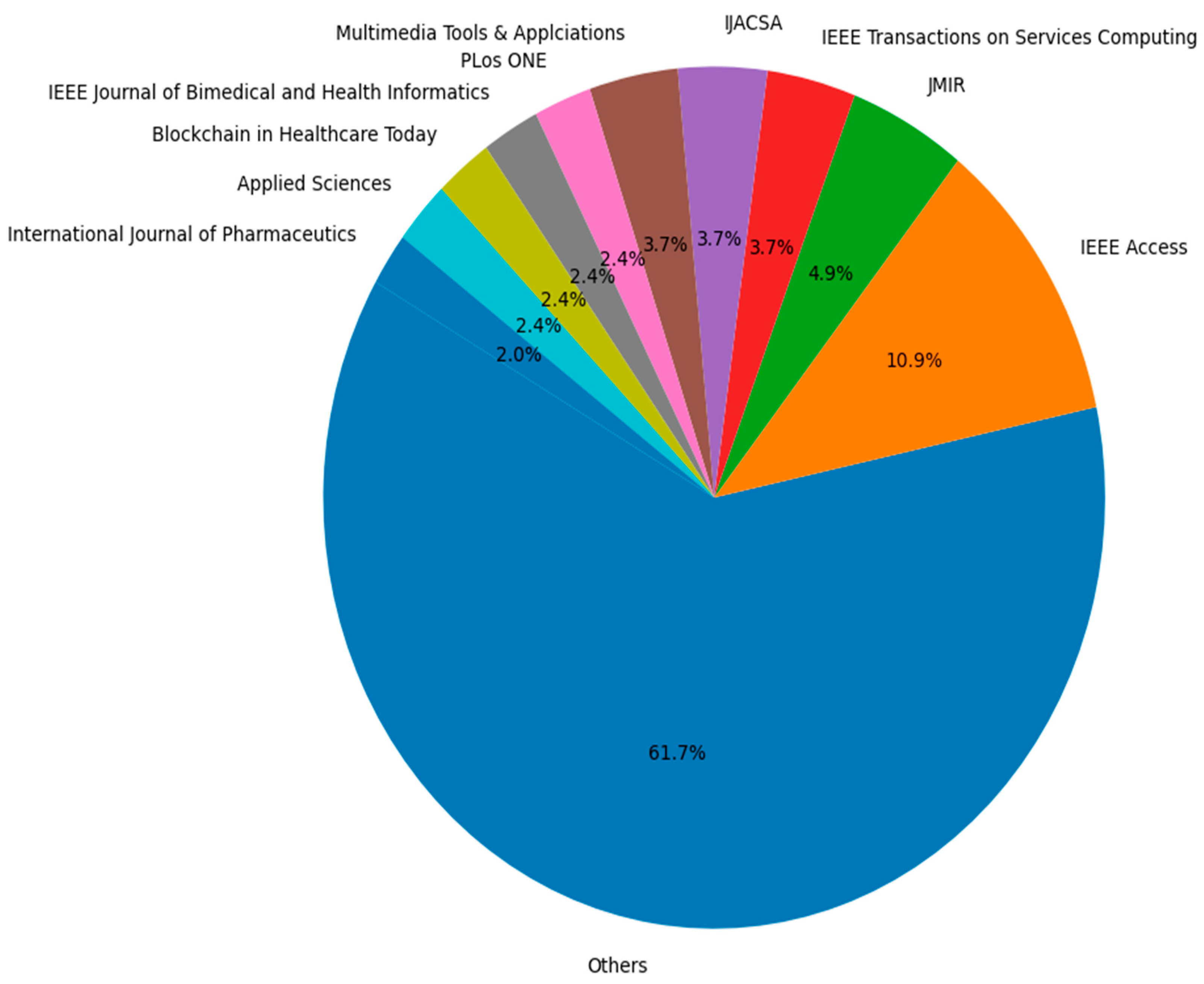
3. Results
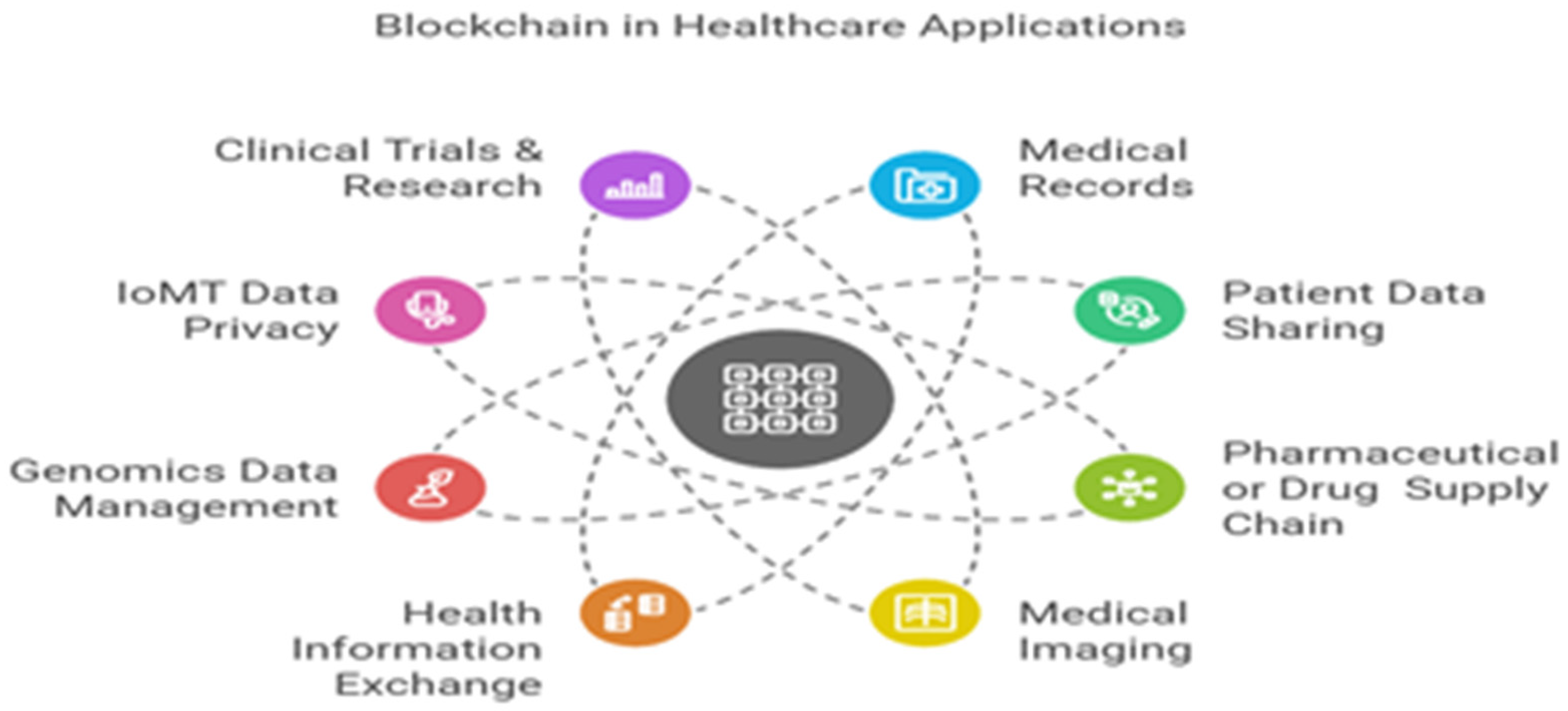
- Medical records: BC is widely leveraged in electronic, medical, and personal health records (EHR, EMR, and PHR) implementation, integration, and management to enable access control, privacy, high security, and seamless and timely sharing of the sophisticated volumes of patient data. Of 82 included studies, 39 (31.98%) studies were found to have been implemented and published on this avenue to facilitate prominence problems and likewise fragmented EHRs, security risks, data inaccessibility, unauthorized access, and data leakage and even loss [31]. The EHR, EMR, and PHR are digital organizations that collect, manage, and store patients’ medical, personal, and health information, providing a comprehensive and holistic view of their healthcare journey. They are the cornerstone for modern healthcare systems because they integrate diverse datasets, enhance care coordination, and enable data-driven decision-making. Their management also becomes paramount while dealing with fragmented records and unlawful access. BC ensures secure patient-centric control over records by utilizing framework implementations such as Hyperledger Fabric and Ethereum, which improve data accessibility, privacy, and interoperability [41,42,43].
- Patient data sharing: In patient data sharing, BC tackled the issue of inefficient and insecure sharing mechanisms. Traditional systems often fail to provide patients with control over their data, leading to privacy concerns. BC-enabled solutions such as HealthChain [38] utilize proxy re-encryption and smart contracts to allow patients to dynamically share their data with specific stakeholders (e.g., providers, researchers) while maintaining privacy. This approach has shown improved efficiency and transparency, particularly in multi-institutional data exchanges [38,44,45]. Future applications include integrating AI with BC for personalized and secure patient care analytics.
- Pharmaceutical or drug supply chains: The pharmaceutical supply chain benefited significantly from BC’s ability to ensure transparency and traceability. Counterfeit drugs pose a major risk to public health, and BC systems such as Hyperledger Fabric for the drug supply chain address this issue by creating immutable records of drug transactions. One study showed a 100% success rate in counterfeit detection and a 95% reduction in supply chain fraud. Additionally, compliance with regulatory standards such as DSCSA is streamlined through BC’s auditable and tamper-proof nature [46,47,48].
- Medical imaging: BC introduced decentralized solutions for medical imaging, addressing privacy concerns and the high storage costs associated with large imaging files such as MRIs and CT scans. The patient-centric medical image management study used Ethereum and inter-planetary file systems to store medical images securely and cost-effectively. This decentralized approach ensures that imaging data are accessible only to authorized users, enhancing patient trust and reducing reliance on centralized repositories [49,50].
- Health information exchange: Interoperability and data ownership are significant challenges in health information exchange (HIE). BC solutions compliant with standards such as HL7 FHIR enable secure and seamless data exchange between healthcare institutions. The patient-centric health information exchange framework study demonstrated how BC improves interoperability while empowering patients with control over their data. This system significantly reduces redundancies and enhances the scalability of large-scale health information systems up to large transactions [51]. An Ethereum-based implementation of health data exchange [52] showed their chain effectiveness, namely EdgeMediChain, evaluated for execution time with a reduction of nearly 84.75% for 2000 concurrent transactions, claiming higher throughput compared to a traditional BC and scalable ledger storage with a linear growth rate implemented by other BC-based frameworks [53]. The authors implemented a smart contract for patient-centered data control using public key cryptography on simulated data, providing enhanced patient data ownership, scalability, and security.
- Genomics data management: Given the sensitivity of genomic information, privacy and ownership are critical concerns in genomics data management. BC applications, such as non-fungible token (NFT)-based systems for genomic data sharing, allow for privacy-preserving collaboration in genomic research and mutation of diseases. The BC for genomic data auditing study showcased how immutable audit trails enable researchers to securely query genomic datasets while ensuring compliance with data ownership policies [54]. It additionally [55] demonstrated that the evolution of genomic logs ledger via the platform (MultiChain 1 to 2) returned a 30–40% increase in insertion logs efficiency, showing a creative and efficient technique for storing and querying genomic log file data.
- Internet of Medical Things (IoMT) data privacy: The IoMT devices and remote networks are major contributors that generate massive amounts of real-time data from sensors and wearable devices, and nowadays, these are on rapid adoption and deployment [56]. They are mostly used for remote patient health monitoring by a healthcare provider, and this mode raises concerns about data security and privacy. BC frameworks integrated with lightweight cryptographic protocols addressed these challenges by enabling secure data sharing in IoMT environments. The IoMT-enabled EHR privacy management [57] demonstrated real-time data protection with reduced latency and high throughput, making BC a viable solution for IoT-heavy healthcare systems, while [58] proposed a multiple authority BC-based attribute-based encryption EHR access control scheme to solve the data security and access control for IoMTs environment through four smart contracts.
- Clinical trials research: BC has the potential to enhance the accountability, audibility, and transparency of medical researchers and practitioners in the areas of managing trials, subject consents, and clinical trials themselves. By preserving the immutable logs of patient consent data, authorities could readily regulate the quality of clinical trials, ensuring that it corresponds with the citizen’s law and complies with an informed agreement. It is particularly crucial to save from many prevalent forms of clinical fraud, medication abuse, and falsified informed consent forms. It also entails changing records and fabricating patient permission, suggesting that trial subjects’ authentication is crucial to preventing them. Here, BC leverages smart contracts to avoid and even help reinforce that kind of arrangement in a way that prevents physicians from accessing patient data without a key by the conclusion. Therefore, [59] proposes a proof-of-concept protocol that utilizes BC to timestamp every stage of patient consent collecting, archiving, and historicizing the consent through cryptographic validation in a visible and safely unfalsifiable manner. These healthcare avenues demonstrate the wide range of applicability and the transformative potential of BC-leveraged solutions such as decentralized, holistic, predictive (EHR, EMR, and PHR) systems, improving patient data sharing interoperability, drug traceability counterfeiting, and so on. All applications we explored addressed significant pain points extensively to contribute to broader challenges such as large-scale scalability, integration with legacy systems, health data management, preservation of privacy, and cost efficiency. Our research contributes to the growing body of pragmatic evidence supporting BC’s role in enhancing healthcare security, transparency, privacy, interoperability, data management, and patient centricity, but is not limited to this. We summarized some BC-based applications in informed healthcare avenues in Table 4.
| Healthcare Avenues | Applications | Problems | Leveraging Blockchain | References |
|---|---|---|---|---|
| Medical records (EHRs, EMRs and PHRs) | Privacy-preservation EHRs/EMRs | Fragmented EHRs, security risks, data inaccessibility, incomplete view, data leakage, and unauthorized access. | Enhances data accessibility, privacy, access control, and provides a holistic view of patient history. | [42,44,68,69,72,73,74] |
| Patient-centric EHRs/EMRs/PHR | Data loss, lack of patient control due to centralized EMRs, tempering, communication gaps among hospitals, and inefficient clinical data retrieval systems for patients. | Provides data immutability and integrity through various conventional consensus algorithms and hash functions, and also enables decentralized control over electronic medical records (EMRs). | [41,43,75,76,77,78,79,80,81,82,83,84,85] | |
| Interoperability of EHR/EMR | Cross-chain interoperability, application-level interoperability, and delays in seamless data exchange. Lack of standardization. | Distributed and decentralized translation layer and integrating HL7 FHIR resources, achieved application and semantic, cross-chain interoperability solution allowing BC networks to inter-communicate, share data, and make requests. | [50,86,87,88,89,90,91,92,93,94] | |
| Patient consent, access control and full- patient control EHRs | Patients’ intractability led to difficult communication and increased procedural costs, limits in developing a better understanding and consent-based patient’ traceability of their data. Medical records theft due to the centralized system. Personal data leakages and monetization. | Enables improved cryptographic primitive multiple access control, attribute-based and semi-policy hiding, and dynamic permission changing based on partial ciphertext simultaneously. | [47,95,96,97,98,99,100] | |
| BINDAAS: BC-based deep-learning as a service | Privacy, scalability, and predictive challenges in EHR data | Secure and predictive EHR management using BC. | [101] | |
| Patient data sharing | HealthChain | Information security, interoperability, data integrity, identity validation, and scalability. | Presents patients and providers with access to consistent and comprehensive medical records. | [38] |
| System for the promotion of traceability and ownership of health data | Privacy risks and inefficiency in data sharing. | Secures access and privacy in patient data sharing with BC technology. | [102] | |
| MedShare | information isolation, centralized health servers, distributed denial of service (DDoS) attacks, and the single point of failure. | Efficient patient data sharing with fine-grained access control and constant size attribute-based encryption (ABE) scheme. | [60] | |
| Redact-chain for health | Data modification and deletion on BC and centralized patient systems undermines single point of failure and robustness. | Redact-Chain integrated with distributed trapdoor scheme introduces a fine-grained data editing scheme for institutions to effectively edit and manage data on the BC, thereby circumventing the issue of a single point of failure. | [103] | |
| Pharmaceutical or drug supply chain | Model for storing pharmaceutical supply chain data | Trust, relying on third party, and storing large data. | Completeness, cost-effectiveness, privacy, and confidentiality ensured and efficient information queries. | [46] |
| Medledger | Counterfeit drugs having serious side effects, online, Internet-based pharmacies hazards safety and security. | Provides efficient and safe transaction records, with high integrity, reliability, and security, and reduces the likelihood of meddling with stored data. | [104] | |
| Counterfeit drug prevention pharma supply chain, PharmaChain and BRUINchain | Counterfeit fake drugs and lack of drug traceability. | Provides traceability, tracking, verification and effectively forestalls any medication being scanned, expiration detection, fake and counterfeit detection; as with reduced paperwork. | [61,62,105] | |
| Healthcare chain network | Prescription drug abuse and doctor shopping. | Tracking prescriptions by decentralization and audibility, encryption ensured anti-fraud and anti-forgery measures to prevent prescription abuse. | [106] | |
| Secure pharmaceutical supply chain | Time delays in the supply chain and lack of security. | Timestamping, authentication, process coordination, non-repudiation, commercial transactions, and security for transactions and storage. | [107] | |
| Medical imaging | PCMIMS—patient-centric medical image management system, and PCRIM—patient-centric test report and image management system | High operational costs and storage space requirements, security, and privacy of large medical images. | Efficient validated large patient-centric medical image processing and requesting, decentralized storage, and privacy of medical imaging data. | [49,67] |
| Health information exchange (HIE) | Patient-centric health information exchange framework | Data ownership issues, interoperability challenges. | Facilitates interoperability and ownership of patient data. | [51], |
| MedChain | Trustworthiness of a third-party, inefficient sharing data streams from IoT and sensors. | Higher efficiency and satisfy the security requirements in data sharing efficient scheme. | [64] | |
| MedHypChain | Infected patients overwhelmed the inadequate medical services and lack of interoperability. | Achieved confidentiality, anonymity, traceability, and unforgeability through an identity-based broadcast group encryption scheme. | [65] | |
| MEXchange | Security, privacy, and costs, with focus on privacy issues caused by analyzing senders and receivers of transactions in HIE. | Ring signature and stealth address implementation mitigating privacy and security issues among healthcare stakeholders. | [53] | |
| EdgeMediChain | HIE systems unable to adapt the expanding volume of body sensor data and their vulnerabilities against attacks. | BC and edge computing facilitate providing an integrated healthcare ecosystem in terms of scalability, security, and privacy to execute up to 2000 concurrent transactions. | [52] | |
| BaaS-HIE | Lagged (EHRs/EMRs) adoption due to confidentiality, interoperability, integrity, and privacy. | Offering decentralized and fine-grained accessibility mechanism for the patient and the doctor in a given healthcare system. | [66] | |
| Genomics data management | Privacy and Ownership Protection System for Genomics [POPS-G] | Privacy and security of gnomic data during analysis and maintenance for mutation of disease. | Provides BC-NFT genomics data handling system for secure, efficient, and simple while preserving privacy and ownership of merging genomic data with EHRs. | [54] |
| Genomics audit logging (MultiChain) | Time or space-efficient structure and mechanism of storing/retrieving genomic data access logs on MultiChain | presented creative and efficient techniques for storing and querying genomic log file data in MultiChain. | [55] | |
| IoMT data privacy | MediVault | Security risks associated with the current digital healthcare data, accessing data by malicious parties. | Provide safe storage of healthcare data in digital form, secure access for authenticated entities and secure, simple, and efficient with a limited computation overhead. | [57] |
| Multiple authorities attribute-based encryption for EHR access control scheme | Security risks of sharing patients’ EHRs, prevailing problems such as difficulties in sharing EHRs between different hospitals and patients’ inability to grasp the usage of their medical devices. | Ensures trust of multiple authorities, secret sharing and smart contracts-based keys for multiple administrative attributes for a single point of failure reduces communication computation overhead on user data. Ciphertext encryption ensured the security of EHRs and IoMTs. | [58] | |
| IoMT-enabled EHR privacy management | Unauthorized access and privacy risks for IoT and wearable device data. | Ensures secure real-time data sharing for wearable and IoT devices using lightweight protocols. | [77] | |
| Clinical trials and research | BC-based patient consent management | Inefficient and non-transparent consent management systems. | Transparent and efficient consent processes for patients. | [108] |
| Aspect | Strengths | Weaknesses | References |
|---|---|---|---|
| Data security and privacy | Multi-attribute encryption techniques, consensus mechanisms ensure highly secure storage and data transmission and immutable records to reduce tampering risks. | Privacy and security imbalance, especially compliance of GDPR remains a big challenge. | [38,41,42,70,72,93,109,110] |
| Transparency and traceability | Immutable records build trust. Transparency through smart contracts for patient consent mechanisms to improve decision-making. | Inefficiency and ethical barriers (e.g., data monetization concerns) invoke complicated prevalent adoption. | [25,28,46,47,48,84,88,108] |
| Decentralized control | Eliminates single points of failure. Empowers individuals (e.g., patients) with data control. | User adoption is hindered by technical complexity and a lack of understanding among stakeholders. | [41,43,61,74,91,95,101,105] |
| Interoperability | Integration with HL7 FHIR standards enables seamless data sharing and reduces redundancies. | Integration with legacy systems and IoT devices is challenging. | [41,51,64,67,71,73,77,97] |
| Efficiency | Smart contracts streamline processes and consent management and data sharing. | High costs (e.g., gas fees in public BC) hinder implementation. | [38,44,45,67,95,96,111] |
| Regulatory compliance | Redactable BC supports detailed audit trails and GDPR compliance, enhancing transparency. | Variations in regulations and ethical concerns limit cross-border implementations. | [25,28,47,48,70,72,84,88] |
| Scalability | N/A | High computational and storage demands, along with latency issues, and limited scalability. | [49,50,73,110] |
| Cryptography | N/A | Proxy re-encryption and attribute-based encryption methods demand high computational resources. | [45,109,112,113] |
| Applications | Blockchain Design and Development Methods (Blockchain Type, Network, Storage, Smart Contract, and Encryption) | Contribution to Present Healthcare | Future Prospects | References |
|---|---|---|---|---|
| Patient-centric EHRs/EMRs/PHR | Permissioned BC, Hyperledger Fabric, multiple smart contracts, IPFS, and asymmetric key cryptography | Enhanced data accessibility, privacy, and interoperability. | Real-time, interoperable global EHR systems integrated with IoMT and body sensors. | [41,43,75] |
| HealthChain | Ethereum, smart contracts, Proxy Re-encryption (PRE) | Improved consent management and secure sharing. | AI-driven data analytics for personalized healthcare solutions. | [38] |
| Pharmaceutical or drug supply chain | Permissioned BC Hyperledger Fabric, Smart Contract, IPFS, Digital Signatures encryption | Verified drug traceability, fraud detection, accuracy, and drug counterfeit prevention. | Automated supply chain auditing and global compliance integration. | [46,61,107] |
| PCMIMS and PCRIM | Public BC, Ethereum, IPFS, Smart Contract Asymmetric Encryption | Decentralized storage reduces costs and enhances access. | AI-enabled imaging analysis integrated with secure BC records. | [49,67] |
| Patient-centric health information exchange | Mixed-BC Hyperledger Fabric, HL7-FHIR compliance, Smart Contract | Improved interoperability and ownership of patient data with full access to treatment. | Seamless cross-chain healthcare information exchange to deliver high-quality treatment. | [51,114] |
| POPS-G and MultiChain | MultiChain, Ethereum, NFT Metamask storage, Smart Contract, genetic encryption | Secure sharing and controlled access for sensitive genomic data for desease mutation. | Global genomic research collaboration with robust privacy controls. | [54,55] |
| MediVault | Ehtereum BC, NFT using (IPFS) and FireBase, Smart Contract, asymmetric encryption, and Multi-Authority Signature Scheme | Secure and efficient real-time data sharing for IoMT and IoT devices. | Expansion to smart city healthcare systems leveraging IoT. | [56,57] |
| MedShare and Redact-Chain for health | Ethereum and redactable Blockchian, IPFS, multiple smart contracts, searchable attribute encryptions, and SHA-256 | Transparent and efficient consent mechanisms with boolean search empower patients’ data-controlled sharing with complete view and data editing. | Universal patient-controlled data platforms with editable exchange. | [60,103] |
| Blockchain-Based Healthcare Application | Data Analysis Performed | Evaluation Metrics (Quantitative Results) | Data Analysis Technique/Models | Datasets | References |
|---|---|---|---|---|---|
| PatientDataChain | Real-world PHRs (1144 trasanction) analyzed for data exchange and scalability. | Privacy: 98% with security compliance; scalability: up to 10 k TPS. | Latency and throughput testing, cryptographic model testing | 100 real-world PHR records over 1144 transactions | [94] |
| BRUINchain | Real-world pharmacy data analyzed for traceability and regulatory compliance. | Traceability:100% success in counterfeit detection; scalability: 2 k TPS. | Traceability analysis using BC logs | Real-world pharmaceutical data | [62] |
| Structural EHRs standard based on the HL7 FHIR | Real-time FHIR simulation of 3 models. | Gas cost: 1.8 billion gas units, gas transactions: 10,000 concurrent. | Hybrid off-chain and on-chain approach, the second model implements a full on-chain | Synthetic dataset with 10,000 patients’ personal information records | [90] |
| [POPS-G] | Genomic access logs analyzed for query time and space efficiency. | Query time: ∼200 ms per request; space efficiency: reduced storage by 35%. | Query benchmarking and space utilization analysis | Real-world genomic data | [54,67] |
| BC for Decentralized Patient Records | Cross-border EHRs evaluated for privacy and security. | Privacy: 96% GDPR compliance; security: no unauthorized access in 10 k tests. | Compliance testing and security event simulation | Real-world international EHR datasets | [73] |
| Pharmaceuticals Traceability using BC | Real-world drug data analyzed for counterfeit detection and fraud prevention. | Traceability: 100% fraud detection; fraud prevention: 95% reduction in cases. | BC transaction analysis and fraud detection modeling | Real-world pharmaceutical data | [84] |
| BC Technology in Healthcare Systems utilizing Machine learning Techniques | Machine learning techniques and BC test net analysis. | Model accuracy: 97.236%. | SHA-256 Secure hashing, Naive Bayes classification algorithm | Real health dataset with 81 symptoms list of patients | [115] |
4. Discussions and Limitations
- Pragmatic evolution: The analyzed findings show the steady progression of BC-based implementations gained a lot of development focus with new creative ideas that help researchers to initiate multi-sphere practicability. The viability of pragmatic shift is being established and evaluated hereof in terms of qualitative recommendations, providing insights into academic, constructive, and quantitative outcomes as measurable metrics in the following perspectives.
- Health data management: Based on our findings, we can say that more academics are paying attention to data management and medical records. The use of BC technology for medical data management has been supported by previous studies [41,43,75,76,77,78,79,80,81,82,83,84,85]. Furthermore, BC can help construct an HIE to manage such EHRs, EMRs, and PHRs [47,95,96] by merging heterogeneous types of data [56,111]. Based on the SLR, we identify three primary enhanced facets of ongoing research in this field.
- Enhanced data security: Previous research about data security implications of this technology in healthcare focused on handling the privacy of data by maintaining data access permission. However, the to an advanced implemented the identity-based proxy re-encryption (IB-PRE) algorithm used by [42,109] to share EHRs in a private, secure, and safe manner over the various security risks such as amateur-level attacks and data breaches by hackers, their technique involves a proxy node retrieves requested data from IPFS, which performs re-encryption and returns re-encrypted data to the requester to ensure user privacy and data integrity.
- Privacy preservation: Data prevention from unauthorized access with maintaining data confidentiality to guarantee data safety are two other major issues covered in our research on the BC’s role in health data management. Most of the included studies concentrated on stopping unauthorized access [42] and preserved privacy through a framework for EHR management. To accomplish this goal, several studies have been put forth, such as the use of redactable BC [72], federated learning technique [71], ring signature and stealth address [53], and consortium BC [73].
- Access control: Multiple studies discussed access control as a key element to health data management which guarantees that sensitive patient data are only available to authorized users or systems while upholding legal requirements and privacy. According to our results, refs [58,95] implemented BC-based multiple attribute-based encryption for access control schemes for EHR for patient data sharing in hospitals among multiple authorized entities and achieved trust among them using secret sharing by deploying smart contracts for attributes. Thus, we also observed a few integrated studies such as [45] implemented BC and an AI-based decentralized access control model to enable secure healthcare interoperability and IoT access control implementation for sharing EHR data [47].
- Advanced novel patient-centric frameworks: Our included studies also comprise new novel frameworks, models have been implemented and trained by the novel patient-centric architectural framework [75], and trusted artificial intelligence for patient data sharing [59] affirms the patient-centric design of a decentralized healthcare management systems over traditional EHR-based systems who plagued data loss risks, security, and immutability consensus over patient health records. Their models ensure patients with authentic immutable medical histories with predictive capabilities by adding an additional layer of BC novelty and AI capabilities synergy.
- Advanced interoperability and cross-chain communication: Interoperability in healthcare involves the secure, seamless exchange of patient data and information across disparate systems, stakeholders, and applications. Our results show a wider contribution of BC as a decentralized and transparent nature, and offer promising solutions to address interoperability challenges. Consider the HIE system based on FHIR, BigchainDB, and GraphQL approach [97], on-chain and off-chain healthcare data system [70], Redact-Chain for Health [103], new scheme BaaS-HIE [66], Appx-Chain: application-level interoperability [86] enabled health data exchange to use the FHIR, HL7, GraphQL, REST, and semantic approaches to observe more effective and efficient architectural solutions that can be used to achieve interoperability between health information systems for organizational use.
- Integration with AI, ML, DL, IoT, FL, and edge computing: BC uses found synergized in healthcare as it enters the fourth stage in development with the intensifying integration of AI [45,98]. Machine learning [115], deep learning [101], federated learning [71,110], IoT [47,48,116], edge computing [52], and cloud computing [51] have all actively been synergized through BC design and development architecture. Researchers are using these technologies to evaluate that BC can enhance the transparency, traceability, and explainability of AI-driven healthcare distributed systems having predictive training capabilities of data intelligence, decision making, and epidemiology [51]. Moreover, leveraging edge computing, a hybrid edge BC-based framework [52] was implemented to facilitate the necessary requirements for a health- care ecosystem in terms of scalability, security, as well as privacy.
- Decentralized governance: Furthermore, studies centered on using BC-based implementation in supporting providers of healthcare services with governance tasks, e.g., self-sovereign identity for patient-centric healthcare [117] and fusion identity management into global healthcare [118]. To eliminate a third party and single point of failure, ref. [89] focused on enabling trusted parties only to ensure access to private data. This research centered on how the BC development methods boosted efficiency and added trust, value to established models, and new structures to end governance management.
- Drug traceability and fraud detection for drug counterfeiting: The advent of threatening patient safety led to data integrity and financial losses. BC offered transformative solutions to enhance maximum drug transparency and traceability [104], detect fraud effectively [61], enhance prescription fraud avoidance [105], and enhance automatic claim resolution [108], which have all been implemented having a measured provenance for BC in the healthcare supply chain. It further enables all parties to verify the authenticity of a drug’s origin and analyze traceability using BC logs for compliance with regulatory standards; BRUINChain achieved traceability as a 100% success in counterfeit detection; and scalability: 2 k TPS [62]. Moreover, ref. [107] implemented a pharmaceutical supply chain using BC in IoT cloud systems, where IoT devices and smart labels (e.g., QR codes, RFID tags) can be linked to BC systems to log real-time data about the location, temperature, and handling conditions of drugs.
- Large-scale solutions: Large volumes of data are being produced by desperate healthcare systems, necessitating secure, scalable, and effective management solutions. ABC implementations [42,108,113] explained promising decentralized medical record self-management systems, with an extent of scalability and transaction throughput attempted with low fees. Additionally, large-scale medical imaging applications PCMIMS [49] and PCRIM [67] validated large patient-centric medical image processing, requesting, and test report management systems through BC schemes. Their results show the decentralized storage and privacy of medical imaging data in a controlled and managed way with patient consent. However, our research witnessed a prominent gap in privacy mismanagement and data tempering while dealing with large-scale implementation. So, we explored Layer-2 solutions to offer a practical means of moving beyond these restrictions, allowing for more practical applications. The benefit of Layer 2: rollups can help update patient data effectively without putting a strain on the main chain so that data records are accessed more quickly while preserving their privacy and integrity.
- Applications in precision medicine: Advancing in the use of genetic, environmental safety, and lifestyle health data, precision medicine seeks to customize medical care to each patient’s unique traits. BC provides a strong back for tackling important precision medicine issues such as data security, interoperability, and patient consent. The only two implementations, i.e., 2% from included studies of this SLR, observed the implementation of genomic data management, such as NFT-enabled privacy, ownership genomics protection systems [54], and decentralized genomics audit logging [55]. Their results demonstrate the feasible ledger for genomic query log data yielded with 30–40% increase in insertion efficiency and privacy-preserved genomic data management. However, the secure sharing of genomic data becomes a paramount concern for further research.
- Regulatory compliance and adherence: BC’s architecture inherently has a permissions layer to ensure that transactions are secure, authenticated, and verifiable. It further holds the potential to strengthen patient-centricity [85], cross-chain interoperability [48], and data security [93] in the healthcare industry. However, for this implementation to be successful, regulatory compliance frameworks such as the General Data Protection Regulation (GDPR), Electronic Identification, Authentication, and Trust Services (eIDAS), and Health Insurance Portability and Accountability Act (HIPAA) must be complied [114]. Here, the authors implemented a Smart Patient Consent Management model for HIE and achieved excellent traceability, openness, and dependability for sharing patient data in research institutions and hospitals complied with GDPR. Additionally, many BC-based implementations aligned their work with regulations such as GDPR and HIPAA while exploring innovations such as regulatory sandboxes and decentralized governance models. In this context, our research explored the European Blockchain Sandbox [119], which is a promising controlled environment where BC solutions are actively researched, tested, and developed within the framework of EU regulations. It facilitates innovation, collaboration, and compatibility while ensuring compliance with the GDPR, eIDAS, or other applicable laws. This initiative allows stakeholders, including startups, enterprises, and regulators, to collaborate and address challenges in BC adoption.
5. Conclusions
6. Challenges and Future Research Direction
- Data security and privacy: Genomic data are highly sensitive, constructed, and valuable; its accessibility and sharing yields risk of breach enabling a prime target for cyber attacks. So, ensuring adherence to regulations such as GDPR, HIPAA, or local laws can be complex, and maintaining data ownership control, anonymity, privacy, and secure genomic data sharing for meaningful access and research poses a significant challenge.
- Lack of standardization and interoperability: Diverse data formats, structures, and a lack of standardization in healthcare or genomic data across platforms hinder seamless sharing. Differences in privacy regulations across regions also create barriers to sharing data internationally besides cross-border data exchange. Integrating genomic data with other healthcare datasets (e.g., EHRs) for holistic analysis requires robust standards and protocols.
- Ethics and consent management: Patient consent for data usage is often overlooked, and managing clear, comprehensive agreement is essential to obtaining a code of ethics. Data ownership is another persistent challenge that leads to undefined ownership of genomic data—patients, researchers, or institutions. Additionally, potential misuse appears as risks of genetic discrimination or unauthorized use of data for purposes away from initial consent.
- Scalability and performance: Genomic datasets are massive structures, and large data volume-based iterations require high storage and computational power. Their real-time access, supporting efficient live queries for research and treatment decisions, is challenging.
- Trust and transparency: Patients and even healthcare stakeholders may not fully understand the benefits and risks of secure genomic data sharing. This lack of awareness hinders its adoption and calls transparency into question. Further, there is a trust deficit related to patients’ being reluctant to share their data due to fears of misuse, less transparency, or breaches. Cultural sensitivity is challenging in genomic research and data sharing must respect cultural and societal norms around genetic information.
- Cost and resources: Infrastructure setup costs in massive amounts, and maintaining operative secure storage, back-end servers, BC networks, and data processing systems can be expensive too. These high costs may limit access, generate inequity to personalized medicine, and exacerbate health inequities.
- BC integration technical challenges: Integrating limitations for BC’s on-chain storage capabilities are insufficient for large-scale genomic datasets, necessitating off-chain decentralized storage such as IPFS. Additionally, the time required for BC transactions might delay critical data retrieval, yielding low latency. Energy consumption is another hurdle for BC systems, especially those using proof of work (PoW), which might be resource intensive.
- Data integrity and authenticity: Ensuring verification issues such as shared data remain unaltered and originate from a trusted legitimate source is critical. Implementing auditability mechanisms to track data usage without compromising privacy is complex.
- Collaboration challenges: Coordination among stakeholders is unavailable, which means researchers, healthcare providers, and policymakers often operate in silos, which leads to complicating collaborative efforts. Negotiating agreements between institutions for genomic data sharing can delay research and there are no such data sharing agreements due to this challenge.
- AI and genomics dilemmas: At any stage, using AI to analyze genomic data can lead to biases in the algorithm, especially if the training datasets are not representative. Understanding AI decision-making processes in genomics interpretation remains a challenge to appraise transparency issues. This is the unique challenge that our research identified, and to address, this we build a novel model for BC-based secure sharing of genomic data using hybrid cryptography, SSI, and encryption techniques. Additionally, our progressive research and development aims to adopt innovative solutions for the pressing need for tailored AI, BC, and large language models (LLMs) solutions that fully address, tame, and advance the specific challenges posed by regional healthcare infrastructures and centers [120,121]. BC applications must be designed to accommodate local variations in data formats, privacy laws, and technological readiness. This adaptability is critical to successfully implement BC in diverse health centers and settings.
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Healthcare IT Market: Global Opportunity Analysis and Industry Forecast, 2021–2030. Technical Report, Allied Market Research. 2021. Available online: https://www.alliedmarketresearch.com/healthcare-information-technology-market (accessed on 20 January 2025).
- Zhang, P.; White, J.; Schmidt, D.C.; Lenz, G.; Rosenbloom, S.T. FHIRChain: Applying Blockchain to Securely and Scalably Share Clinical Data. Comput. Struct. Biotechnol. J. 2018, 16, 267–278. [Google Scholar] [CrossRef] [PubMed]
- Office of the National Coordinator for Health Information Technology. US Core Data for Interoperability (USCDI). 2023. Available online: https://www.healthit.gov/isp/united-states-core-data-interoperability-uscdi (accessed on 20 January 2025).
- Casado-Vara, R.; Corchado, J. Blockchain for Democratic Voting: How Blockchain Could Cast Off Voter Fraud. Orient. J. Comput. Sci. Technol. 2018, 11, 1–9. [Google Scholar] [CrossRef]
- Casado-Vara, R.; Corchado, J. Distributed e-health wide-world accounting ledger via blockchain. J. Intell. Fuzzy Syst. 2019, 36, 2381–2386. [Google Scholar] [CrossRef]
- Jaoude, J.A.; Saade, R.G. Blockchain applications–usage in different domains. IEEE Access 2019, 7, 45360–45381. [Google Scholar] [CrossRef]
- Kitchenham, B.; Brereton, O.P.; Budgen, D.; Turner, M.; Bailey, J.; Linkman, S. Systematic literature reviews in software engineering–a systematic literature review. Inf. Softw. Technol. 2009, 51, 7–15. [Google Scholar] [CrossRef]
- Peck, M.E. Blockchain world—Do you need a blockchain? This chart will tell you if the technology can solve your problem. IEEE Spectr. 2017, 54, 38–60. [Google Scholar] [CrossRef]
- Chen, Z.; Gu, J.; Yan, H. HAE: A hybrid cryptographic algorithm for blockchain medical scenario applications. Appl. Sci. 2023, 13, 12163. [Google Scholar] [CrossRef]
- Jaoude, J.A. Blockchain, consent and prosent for medical research. J. Med. Ethics 2019, 45, 54–60. [Google Scholar]
- Tehrani, K.D.; Deravi, M.M. Fraud detection in insurance claims using machine learning and blockchain. J. Comput. Sci. 2023, 39, 1124–1135. [Google Scholar]
- Jin, H.; Li, B.; Jakovljevic, M. How China controls the Covid-19 epidemic through public health expenditure and policy? J. Med. Econ. 2022, 25, 437–449. [Google Scholar] [CrossRef]
- Allaire, J. Blockchain technology: Real-world use cases and future opportunities. IEEE Trans. Ind. Inform. 2022, 16, 4832–4839. [Google Scholar]
- Elangovan, D.; Long, C.S.; Bakrin, F.S.; Tan, C.S.; Goh, K.W.; Yeoh, S.F.; Loy, M.J.; Hussain, Z.; Lee, K.S.; Idris, A.C.; et al. The use of blockchain technology in the healthcare sector: Systematic review. JMIR Med. Inform. 2022, 10, e17278. [Google Scholar] [CrossRef] [PubMed]
- Chukwu, E.; Garg, L. A systematic review of blockchain in healthcare: Frameworks, prototypes, and implementations. IEEE Access 2020, 8, 21196–21214. [Google Scholar] [CrossRef]
- Saranya, R.; Murugan, A. A systematic review of enabling blockchain in healthcare system: Analysis, current status, challenges and future direction. Mater. Today Proc. 2023, 80, 3010–3015. [Google Scholar] [CrossRef]
- Puneeth, P.R.P.; Parthasarathy, G. A survey on security and interoperability of electronic health records sharing using blockchain technology. Acta Inform. Pragensia 2023, 12, 160–178. [Google Scholar] [CrossRef]
- Chauhan, S.; Tanwar, H.K.S. Application of blockchain technology in healthcare: A systematic review. In Proceedings of the 2022 International Conference on Applied Artificial Intelligence and Computing (ICAAIC), Salem, India, 9–11 May 2022; pp. 1–5. [Google Scholar]
- Mittal, S.; Ghosh, M. Applications of blockchain in healthcare domain: A comprehensive survey. In Proceedings of the 2024 11th International Conference on Computing for Sustainable Global Development (INDIACom), New Delhi, India, 28 February–1 March 2024; pp. 1015–1022. [Google Scholar]
- Fatoum, H.; Hanna, S.; Halamka, J.D.; Sicker, D.C.; Spangenberg, P.; Hashmi, S.K. Blockchain integration with digital technology and the future of healthcare ecosystems: Systematic review. J. Med. Internet Res. 2021, 23, e19846. [Google Scholar] [CrossRef]
- Upadhyay, S.; Agarwal, S.; Chaudhary, A.; Singh, P.; Sharma, R. Blockchain in healthcare systems: A systematic review. In Proceedings of the 2024 2nd International Conference on Disruptive Technologies (ICDT), Greater Noida, India, 15–16 March 2024; pp. 140–147. [Google Scholar]
- Dhingra, S.; Raut, R.; Naik, K.; Muduli, K. Blockchain technology applications in healthcare supply chains–A review. IEEE Access 2024, 12, 12345–12356. [Google Scholar] [CrossRef]
- Kiania, K.; Jameii, S.M.; Rahmani, A.M. Blockchain-based privacy and security preserving in electronic health: A systematic review. Multimed. Tools Appl. 2023, 82, 28493–28519. [Google Scholar] [CrossRef]
- Kassab, M.; DeFranco, J.; Malas, T.; Laplante, P.; Destefanis, G.; Neto, V.V.G. Exploring research in blockchain for healthcare and a roadmap for the future. IEEE Trans. Emerg. Top. Comput. 2019, 9, 1835–1852. [Google Scholar] [CrossRef]
- Urkude, S.V.; Saravanan, D. Exploring the blockchain applications in healthcare sector: A systematic literature review. In Proceedings of the 2023 3rd International Conference on Innovative Mechanisms for Industry Applications (ICIMIA), Bengaluru, India, 21–23 December 2023; pp. 240–247. [Google Scholar]
- Noon, A.K.; Aziz, O.; Zahra, I.; Anwar, M. Implementation of blockchain in healthcare: A systematic review. In Proceedings of the 2021 International Conference on Innovative Computing (ICIC), Lahore, Pakistan, 9–10 November 2021; pp. 1–10. [Google Scholar]
- Vazirani, A.A.; O’Donoghue, O.; Brindley, D.; Meinert, E. Implementing blockchains for efficient healthcare: Systematic review. J. Med. Internet Res. 2019, 21, e12439. [Google Scholar] [CrossRef]
- Saeed, H.; Malik, H.; Bashir, U.; Ahmad, A.; Riaz, S.; Ilyas, M.; Bukhari, W.A.; Khan, M.I.A. Blockchain technology in healthcare: A systematic review. PLoS ONE 2022, 17, e0266462. [Google Scholar] [CrossRef] [PubMed]
- Merlo, V.; Pio, G.; Giusto, F.; Bilancia, M. On the exploitation of the blockchain technology in the healthcare sector: A systematic review. Expert Syst. Appl. 2023, 213, 118897. [Google Scholar] [CrossRef]
- Arsheen, S.; Ahmad, K. SLR: A systematic literature review on blockchain applications in healthcare. In Proceedings of the 2021 International Conference on Information Science and Communications Technologies (ICISCT), Tashkent, Uzbekistan, 3–5 November 2021; pp. 1–6. [Google Scholar]
- Haddad, A.; Habaebi, M.H.; Islam, M.R.; Hasbullah, N.F.; Zabidi, S.A. Systematic review on AI-blockchain based e-healthcare records management systems. IEEE Access 2022, 10, 94583–94615. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Rethlefsen, M.L.; Kirtley, S.; Waffenschmidt, S.; Ayala, A.P.; Moher, D.; Page, M.J.; Koffel, J.B.; PRISMA-S Group. PRISMA-S: An extension to the PRISMA statement for reporting literature searches in systematic reviews. Syst. Rev. 2021, 10, 39. [Google Scholar] [CrossRef]
- Lockwood, C.; Munn, Z.; Porritt, K. Qualitative research synthesis: Methodological guidance for systematic reviewers utilizing meta-aggregation. Int. J. Evid. -Based Healthc. 2015, 13, 179–187. [Google Scholar] [CrossRef]
- Clarivate Analytics. EndNote 21; Clarivate Analytics: London, UK, 2025; Available online: https://endnote.com/ (accessed on 5 February 2025).
- Lindbergh, V.G.; Filho, I.D.M.B. Trends in Blockchain Applied to Healthcare. In Proceedings of the 2024 IEEE 12th International Conference on Healthcare Informatics (ICHI), Orlando, FL, USA, 3–6 June 2024; pp. 531–533. [Google Scholar] [CrossRef]
- Hylock, R.H.; Zeng, X. A blockchain framework for patient-centered health records and exchange (HealthChain): Evaluation and proof-of-concept study. J. Med. Internet Res. 2019, 21, e13592. [Google Scholar] [CrossRef]
- Chelladurai, M.U.; Pandian, S.; Ramasamy, K. A blockchain based patient-centric electronic health record storage and integrity management for e-Health systems. Health Policy Technol. 2021, 10, 100513. [Google Scholar] [CrossRef]
- Kasyapa, M.S.; Vanmathi, C. Blockchain integration in healthcare: A comprehensive investigation of use cases, performance issues, and mitigation strategies. Front. Digit. Health 2024, 6, 1359858. [Google Scholar] [CrossRef]
- Agbo, C.C.; Mahmoud, Q.H.; Eklund, J.M. Blockchain technology in healthcare: A systematic review. Healthcare 2019, 7, 56. [Google Scholar] [CrossRef] [PubMed]
- Jakhar, A.K.; Singh, M.; Sharma, R.; Viriyasitavat, W.; Dhiman, G.; Goel, S. A blockchain-based privacy-preserving and access-control framework for electronic health records management. Multimed. Tools Appl. 2024, 83, 84195–84229. [Google Scholar] [CrossRef]
- Ndzimakhwe, M.; Telukdarie, A.; Munien, I.; Vermeulen, A.; Chude-Okonkwo, U.K.; Philbin, S.P. A Framework for User-Focused Electronic Health Record System Leveraging Hyperledger Fabric. Information 2023, 14, 51. [Google Scholar] [CrossRef]
- Subramanian, H. A Decentralized Marketplace for Patient-Generated Health Data: Design Science Approach. J. Med. Internet Res. 2023, 25, e42743. [Google Scholar] [CrossRef]
- Rana, S.K.; Nisar, K.; Ibrahim, A.A.A.; Rana, A.K.; Goyal, N.; Chawla, P. Blockchain Technology and Artificial Intelligence Based Decentralized Access Control Model to Enable Secure Interoperability for Healthcare. Sustainability 2022, 14, 9471. [Google Scholar] [CrossRef]
- Tahmasbzadeh, A.; Kabirirad, S. A Blockchain-Based Approach for Data Storage in Drug Supply Chain. In Proceedings of the 2023 9th International Conference on Web Research (ICWR), Tehran, Iran, 3–4 May 2023; pp. 335–341. [Google Scholar] [CrossRef]
- Ilyas, I.B.; Kumar, A.; Ali, S.M.; Lei, H. Blockchain-enabled IoT access control model for sharing electronic healthcare data. Multimed. Tools Appl. 2024, 84, 8127–8148. [Google Scholar] [CrossRef]
- Puneeth, R.P.; Parthasarathy, G. Seamless Data Exchange: Advancing Healthcare with Cross-Chain Interoperability in Blockchain for Electronic Health Records. Int. J. Adv. Comput. Sci. Appl. 2023, 14, 280–289. [Google Scholar] [CrossRef]
- Aljaloud, A. A Framework for Patient-Centric Medical Image Management using Blockchain Technology. Int. J. Adv. Comput. Sci. Appl. 2023, 14, 747–757. [Google Scholar] [CrossRef]
- Puranik, A.; Akkihal, A.V.; Honnavalli, P.B.; Eswaran, S. CoreMedi: Secure Medical Records Sharing Using Blockchain Technology. In Proceedings of the 2022 International Conference on Data Analytics for Business and Industry, ICDABI 2022, Sakhir, Bahrain, 25–26 October 2022; pp. 33–37. [Google Scholar] [CrossRef]
- Zhuang, Y.; Sheets, L.R.; Chen, Y.W.; Shae, Z.Y.; Tsai, J.J.P.; Shyu, C.R. A patient-centric health information exchange framework using blockchain technology. IEEE J. Biomed. Health Inform. 2020, 24, 2169–2176. [Google Scholar] [CrossRef]
- Akkaoui, R.; Hei, X.; Cheng, W. EdgeMediChain: A Hybrid Edge Blockchain-Based Framework for Health Data Exchange. IEEE Access 2020, 8, 113467–113486. [Google Scholar] [CrossRef]
- Lee, D.; Song, M. MEXchange: A Privacy-Preserving Blockchain-Based Framework for Health Information Exchange Using Ring Signature and Stealth Address. IEEE Access 2021, 9, 158122–158139. [Google Scholar] [CrossRef]
- Dakshayini, M.; Kavalleswari, A.; Suhasini, H.S. Blockchain-NFT Enabled Privacy and Ownership Protection System for Genomics [POPS-G]. In Proceedings of the International Conference on Emerging Technologies in Computer Science for Interdisciplinary Applications, ICETCS 2024, Bengaluru, India, 22–23 April 2024. [Google Scholar] [CrossRef]
- Pattengale, N.D.; Hudson, C.M. Decentralized genomics audit logging via permissioned blockchain ledgering. BMC Med. Genom. 2020, 13, 102. [Google Scholar] [CrossRef] [PubMed]
- Biswas, S.; Sharif, K.; Li, F.; Latif, Z.; Kanhere, S.S.; Mohanty, S.P. Interoperability and Synchronization Management of Blockchain-Based Decentralized e-Health Systems. IEEE Trans. Eng. Manag. 2020, 67, 1363–1376. [Google Scholar] [CrossRef]
- Blockchain Enabled MediVault for Healthcare System. Available online: https://www.researchgate.net/publication/381517166_Blockchain_enabled_MediVault_for_healthcare_system (accessed on 5 February 2025).
- Yang, X.; Zhang, C. Blockchain-Based Multiple Authorities Attribute-Based Encryption for EHR Access Control Scheme. Appl. Sci. 2022, 12, 10812. [Google Scholar] [CrossRef]
- Jennath, H.S.; Anoop, V.S.; Asharaf, S. Blockchain for healthcare: Securing patient data and enabling trusted artificial intelligence. Int. J. Interact. Multimed. Artif. Intell. 2020, 6, 15–23. [Google Scholar] [CrossRef]
- Wang, M.; Guo, Y.; Zhang, C.; Wang, C.; Huang, H.; Jia, X. MedShare: A Privacy-Preserving Medical Data Sharing System by Using Blockchain. IEEE Trans. Serv. Comput. 2023, 16, 438–451. [Google Scholar] [CrossRef]
- SS, G.; Dhali, A.; Tahlil, T.; MM, A.; ABMS, A. PharmaChain: Blockchain-based drug supply chain provenance verification system. Heliyon 2023, 9, e17957. [Google Scholar] [CrossRef]
- The Last Mile: DSCSA Solution Through Blockchain Technology: Drug Tracking, Tracing, and Verification at the Last Mile of the Pharmaceutical Supply Chain with BRUINchain. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC9907423/ (accessed on 26 December 2024).
- Benchoufi, M.; Porcher, R.; Ravaud, P. Blockchain protocols in clinical trials: Transparency and traceability of consent. F1000Research 2017, 6, 66. [Google Scholar] [CrossRef]
- Shen, B.; Guo, J.; Yang, Y. MedChain: Efficient healthcare data sharing via blockchain. Appl. Sci. 2019, 9, 1207. [Google Scholar] [CrossRef]
- Kumar, M.; Chand, S. MedHypChain: A patient-centered interoperability hyperledger-based medical healthcare system: Regulation in COVID-19 pandemic. J. Netw. Comput. Appl. 2021, 179, 102975. [Google Scholar] [CrossRef]
- Buzachis, A.; Celesti, A.; Fazio, M.; Villari, M. On the Design of a Blockchain-as-a-Service-Based Health Information Exchange (BaaS-HIE) System for Patient Monitoring. In Proceedings of the IEEE Symposium on Computers and Communications, Barcelona, Spain, 29 June–3 July 2019. [Google Scholar] [CrossRef]
- Mohsan, S.A.H.; Razzaq, A.; Ghayyur, S.A.K.; Alkahtani, H.K.; Al-Kahtani, N.; Mostafa, S.M. Decentralized Patient-Centric Report and Medical Image Management System Based on Blockchain Technology and the Inter-Planetary File System. Int. J. Environ. Res. Public Health 2022, 19, 14641. [Google Scholar] [CrossRef] [PubMed]
- Chenthara, S.; Ahmed, K.; Wang, H.; Whittaker, F.; Chen, Z. Healthchain: A novel framework on privacy preservation of electronic health records using blockchain technology. PLoS ONE 2020, 15, e0243043. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.; Zhang, X. Integrating blockchain and ZK-ROLLUP for efficient healthcare data privacy protection system via IPFS. Sci. Rep. 2024, 14, 11746. [Google Scholar] [CrossRef]
- Miyachi, K.; Mackey, T.K. hOCBS: A privacy-preserving blockchain framework for healthcare data leveraging an on-chain and off-chain system design. Inf. Process. Manag. 2021, 58, 102535. [Google Scholar] [CrossRef]
- Guduri, M.; Chakraborty, C.; Maheswari, U.; Margala, M. Blockchain-Based Federated Learning Technique for Privacy Preservation and Security of Smart Electronic Health Records. IEEE Trans. Consum. Electron. 2024, 70, 2608–2617. [Google Scholar] [CrossRef]
- Xu, S.; Ning, J.; Li, X.; Yuan, J.; Huang, X.; Deng, R.H. A Privacy-Preserving and Redactable Healthcare Blockchain System. IEEE Trans. Serv. Comput. 2024, 17, 364–377. [Google Scholar] [CrossRef]
- Zhang, X.; Xi, P.; Liu, W.; Peng, S. EMRShareChain: A Privacy-Preserving EMR Sharing System Model Based on the Consortium Blockchain. In Bioinformatics Research and Applications. ISBRA 2022; Lecture Notes in Computer Science; Springer: Cham, Switzerland, 2022; pp. 343–355. [Google Scholar] [CrossRef]
- Lee, J.S.; Chew, C.J.; Liu, J.Y.; Chen, Y.C.; Tsai, K.Y. Medical blockchain: Data sharing and privacy preserving of EHR based on smart contract. J. Inf. Secur. Appl. 2022, 65, 103117. [Google Scholar] [CrossRef]
- Singh, A.P.; Singh, A.P.; Pradhan, N.R.; Luhach, A.K.; Agnihotri, S.; Jhanjhi, N.Z.; Verma, S.; Ghosh, U.; Roy, D.S. A Novel Patient-Centric Architectural Framework for Blockchain-Enabled Healthcare Applications. IEEE Trans. Ind. Inform. 2021, 17, 5779–5789. [Google Scholar] [CrossRef]
- Madine, M.M.; Battah, A.A.; Yaqoob, I.; Salah, K.; Jayaraman, R.; Al-Hammadi, Y.; Pesic, S.; Ellahham, S. Blockchain for Giving Patients Control over Their Medical Records. IEEE Access 2020, 8, 193102–193115. [Google Scholar] [CrossRef]
- da Silva Costa, T.B.; Shinoda, L.; Moreno, R.A.; Krieger, J.E.; Gutierrez, M. Blockchain-Based Architecture Design for Personal Health Record: Development and Usability Study. J. Med. Internet Res. 2022, 24, e35013. [Google Scholar] [CrossRef]
- Kaur, J.; Rani, R.; Kalra, N. A Blockchain-based Framework for Privacy Preservation of Electronic Health Records (EHRs). Trans. Emerg. Telecommun. Technol. 2022, 33, e4507. [Google Scholar] [CrossRef]
- Naresh, V.S.; Reddi, S.; Allavarpu, V.V.L.D. Blockchain-based patient centric health care communication system. Int. J. Commun. Syst. 2021, 34, e4749. [Google Scholar] [CrossRef]
- Reen, G.S.; Mohandas, M.; Venkatesan, S. Decentralized patient centric e-Health record management system using blockchain and IPFS. In Proceedings of the 2019 IEEE Conference on Information and Communication Technology, CICT 2019, Allahabad, India, 6–8 December 2019. [Google Scholar] [CrossRef]
- Haddad, A.; Habaebi, M.H.; Elsheikh, E.A.; Islam, M.R.; Zabidi, S.A.; Suliman, F.E.M. E2EE enhanced patient-centric blockchain-based system for EHR management. PLoS ONE 2024, 19, e0301371. [Google Scholar] [CrossRef] [PubMed]
- Vyas, J.D.; Han, M.; Li, L.; Pouriyeh, S.; He, J.S. Integrating blockchain technology into healthcare. In Proceedings of the ACMSE ‘20: Proceedings of the 2020 ACM Southeast Conference, Tampa, FL, USA, 2–4 April 2020; pp. 197–203. [Google Scholar] [CrossRef]
- George, M.; Chacko, A.M. MediTrans—Patient-centric interoperability through blockchain. Int. J. Netw. Manag. 2022, 32, e2187. [Google Scholar] [CrossRef]
- Toshniwal, B.; Podili, P.; Reddy, R.J.; Kataoka, K. PACEX: PAtient-Centric EMR eXchange in Healthcare Systems using Blockchain. In Proceedings of the 2019 IEEE 10th Annual Information Technology, Electronics and Mobile Communication Conference, IEMCON 2019, Vancouver, BC, Canada, 17–19 October 2019; pp. 954–960. [Google Scholar] [CrossRef]
- Rai, B.K.; Fatima, S.; Satyarth, K. Patient-Centric Multichain Healthcare Record. Int. J. e-Health Med. Commun. 2022, 13, 1–14. [Google Scholar] [CrossRef]
- Madine, M.; Salah, K.; Jayaraman, R.; Al-Hammadi, Y.; Arshad, J.; Yaqoob, I. AppxChain: Application-level interoperability for blockchain networks. IEEE Access 2021, 9, 87777–87791. [Google Scholar] [CrossRef]
- Rahman, A.U.; Mohammed, A.; Abdullah, A.; Abdullah, A.; Al, J.A.; Hassan, A.; Aghiad, B.; Nehad, I.; Khalid, A.; Tahir, I.; et al. Blockchain Empowered Interoperable Framework for Smart Healthcare. Math. Model. Eng. Probl. 2024, 11, 1330–1340. [Google Scholar] [CrossRef]
- Carter, G.; Shahriar, H.; Sneha, S. Blockchain-based interoperable electronic health record sharing framework. In Proceedings of the 2019 IEEE 43rd Annual Computer Software and Applications Conference (COMPSAC), Milwaukee, WI, USA, 15–19 July 2019; pp. 452–457. [Google Scholar] [CrossRef]
- Nargis, T.; Vivek, S.; Thomas, A.C.; Shenoy, S.U. Decentralized Record Encryption Authentication and Management System (DREAMS) for Healthcare. In Proceedings of the 2023 International Conference on Network, Multimedia and Information Technology, NMITCON 2023, Bengaluru, India, 1–2 September 2023. [Google Scholar] [CrossRef]
- Pulmano, C.; Fernandez, P. Developing a Structural Standard for Smart Contract Electronic Health Records Based on the HL7 Fast Healthcare Interoperability Resources. In Proceedings of the International Conference on Information and Communication Technologies for Ageing Well and e-Health, ICT4AWE—Proceedings, Angers, France, 28–30 April 2024; pp. 169–175. [Google Scholar] [CrossRef]
- Pasha, M.J.; Baseer, K.K.; Vasavi, N.; Sreenivasulu, K.; Nadeem, S.M.; Reddy, A.C.O. Ethereum Blockchain-Based Design and Implementation of Electronic Records for Home Care. In Proceedings of the 2nd IEEE International Conference on Networking and Communications 2024, ICNWC 2024, Chennai, India, 2–4 April 2024. [Google Scholar] [CrossRef]
- Zaabar, B.; Cheikhrouhou, O.; Jamil, F.; Ammi, M.; Abid, M. HealthBlock: A secure blockchain-based healthcare data management system. Comput. Netw. 2021, 200, 108500. [Google Scholar] [CrossRef]
- Abouali, M.; Sharma, K.; Saadawi, T. Patient Full Control over Secured Medical Records Transfer Framework Based on Blockchain. In Proceedings of the International Conference on Electrical Engineering and Informatics, Virtually, 19–20 October 2022; pp. 43–48. [Google Scholar] [CrossRef]
- Cernian, A.; Tiganoaia, B.; Sacala, I.S.; Pavel, A.; Iftemi, A. Patientdatachain: A blockchain-based approach to integrate personal health records. Sensors 2020, 20, 6538. [Google Scholar] [CrossRef]
- Yuan, W.X.; Yan, B.; Li, W.; Hao, L.Y.; Yang, H.M. Blockchain-based medical health record access control scheme with efficient protection mechanism and patient control. Multimed. Tools Appl. 2023, 82, 16279–16300. [Google Scholar] [CrossRef]
- Sun, J.; Yao, X.; Wang, S.; Wu, Y. Blockchain-Based Secure Storage and Access Scheme for Electronic Medical Records in IPFS. IEEE Access 2020, 8, 59389–59401. [Google Scholar] [CrossRef]
- Li, F.; Liu, K.; Zhang, L.; Huang, S.; Wu, Q. EHRChain: A Blockchain-Based EHR System Using Attribute-Based and Homomorphic Cryptosystem. IEEE Trans. Serv. Comput. 2022, 15, 2755–2765. [Google Scholar] [CrossRef]
- Zhan, W.; Chen, C.L.; Weng, W.; Tsaur, W.J.; Lim, Z.Y.; Deng, Y.Y. Incentive EMR Sharing System Based on Consortium Blockchain and IPFS. Healthcare 2022, 10, 1840. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Wu, H.; Wang, L. Patients-controlled secure and privacy-preserving EHRs sharing scheme based on consortium blockchain. In Proceedings of the 2019 IEEE Global Communications Conference (GLOBECOM), Waikoloa, HI, USA, 9–13 December 2019. [Google Scholar] [CrossRef]
- Oliveira, M.T.D.; Reis, L.H.A.; Verginadis, Y.; Mattos, D.M.F.; Olabarriaga, S.D. SmartAccess: Attribute-Based Access Control System for Medical Records Based on Smart Contracts. IEEE Access 2022, 10, 117836–117854. [Google Scholar] [CrossRef]
- Bhattacharya, P.; Tanwar, S.; Bodkhe, U.; Tyagi, S.; Kumar, N. BinDaaS: Blockchain-Based Deep-Learning as-a-Service in Healthcare 4.0 Applications. IEEE Trans. Netw. Sci. Eng. 2021, 8, 1242–1255. [Google Scholar] [CrossRef]
- Pinto, R.P.; Silva, B.M.C.; Inacio, P.R.M. A System for the Promotion of Traceability and Ownership of Health Data Using Blockchain. IEEE Access 2022, 10, 92760–92773. [Google Scholar] [CrossRef]
- Hu, J.; Huang, K.; Bian, G.; Cui, Y. Redact-Chain for Health: A Scheme Based on Redactable Blockchain for Managing Shared Healthcare Data. Electronics 2023, 12, 4240. [Google Scholar] [CrossRef]
- Uddin, M. Blockchain Medledger: Hyperledger fabric enabled drug traceability system for counterfeit drugs in pharmaceutical industry. Int. J. Pharm. 2021, 597, 120235. [Google Scholar] [CrossRef]
- Jha, R.K.; Alam, P.; Priyadarshi, N.; Ghazi, M.A.; Bhargavi, M.S. Counterfeit Drug Prevention in Pharma Supply Chain using Blockchain Technology. In Proceedings of the 2023 3rd International Conference on Intelligent Communication and Computational Techniques (ICCT), Jaipur, India, 19–20 January 2023; pp. 1–6. [Google Scholar] [CrossRef]
- Mani, V.; Prakash, M. Healthcare Chain Network Framework for Monitoring and Verifying Pharmaceutical Supply Chain. In Proceedings of the ECS Transactions, Atlanta, GA, USA, 9–13 October 2022; pp. 3233–3244. [Google Scholar] [CrossRef]
- Mangala, N.; Naveen, D.R.; Reddy, B.E.; Buyya, R.; Venugopal, K.R.; Iyengar, S.S.; Patnaik, L.M. Secure pharmaceutical supply chain using blockchain in IoT cloud systems. Internet Things 2024, 26, 101215. [Google Scholar] [CrossRef]
- Naik, K.V.; Murari, T.V.; Manoj, T. A Blockchain Based Patient Consent Management Technique for Electronic Health Record Sharing. In Proceedings of the 7th IEEE International Conference on Recent Advances and Innovations in Engineering (ICRAIE), Mangalore, India, 1–3 December 2022; pp. 214–219. [Google Scholar] [CrossRef]
- Kaur, J.; Rani, R.; Kalra, N. Attribute-Based Access Control Scheme for Secure Storage and Sharing of EHRs Using Blockchain and IPFS. Cluster Computing 2024, 27, 1579–1591. [Google Scholar] [CrossRef]
- Mukherjee, A.; Halder, R.; Chandra, J.; Shrivastava, S. HealthChain: A Blockchain-aided Federated Healthcare Management System. In Proceedings of the 2023 IEEE International Conference on Blockchain and Cryptocurrency, ICBC 2023, Dubai, United Arab Emirates, 1–5 May 2023. [Google Scholar] [CrossRef]
- Kastowo, D.; Utami, E.; Muhammad, A.H. FHIR, BigchainDB, and GraphQL approach for interoperability between heterogeneous Health Information System. In Proceedings of the ICOIACT 2022—5th International Conference on Information and Communications Technology: A New Way to Make AI Useful for Everyone in the New Normal Era, Virtually, 24–25 August 2022; pp. 272–277. [Google Scholar] [CrossRef]
- Marry, P.; Yenumula, K.; Katakam, A.; Bollepally, A.; Athaluri, A. Blockchain based Smart Healthcare System. In Proceedings of the International Conference on Sustainable Computing and Smart Systems, ICSCSS 2023, Coimbatore, India, 14–16 June 2023; pp. 1480–1484. [Google Scholar] [CrossRef]
- Saidi, H.; Labraoui, N.; Ari, A.A.A.; Maglaras, L.A.; Emati, J.H.M. DSMAC: Privacy-Aware Decentralized Self-Management of Data Access Control Based on Blockchain for Health Data. IEEE Access 2022, 10, 101011–101028. [Google Scholar] [CrossRef]
- Rohini, K.R.; Rajakumar, P.S.; Geetha, S. Smart Patient Consent Management Model for Health Information Exchange Based on Blockchain Technology. J. Comput. Sci. 2024, 20, 730–741. [Google Scholar] [CrossRef]
- Patil, S.R. Implementing Blockchain Technology in Healthcare Systems utilizing Machine learning Techniques. In Proceedings of the 2022 IEEE North Karnataka Subsection Flagship International Conference, NKCon 2022, Vijayapura, India, 20–21 November 2022. [Google Scholar] [CrossRef]
- Gohar, A.N.; Abdelmawgoud, S.A.; Farhan, M.S. A Patient-Centric Healthcare Framework Reference Architecture for Better Semantic Interoperability Based on Blockchain, Cloud, and IoT. IEEE Access 2022, 10, 92137–92157. [Google Scholar] [CrossRef]
- Harrell, D.T.; Usman, M.; Hanson, L.; Abdul-Moheeth, M.; Desai, I.; Shriram, J.; de Oliveira, E.; Bautista, J.R.; Meyer, E.T.; Khurshid, A. Technical Design and Development of a Self-Sovereign Identity Management Platform for Patient-Centric Health Care Using Blockchain Technology. Blockchain Health Today 2022, 5, 196. [Google Scholar] [CrossRef]
- Abdeen, M.A.R.; Ali, T.; Khan, Y.; Yagoub, M.C.E. Fusing identity management, HL7 and blockchain into a global healthcare record sharing architecture. Int. J. Adv. Comput. Sci. Appl. 2019, 10, 630–636. [Google Scholar] [CrossRef]
- Commission, E. European Blockchain Regulatory Sandbox. 2024. Available online: https://digital-finance-platform.ec.europa.eu/cross-border-services/ebsi (accessed on 26 December 2024).
- Shammi, S.A.; Ghosh, P.; Sutradhar, A.; Shamrat, F.J.M.; Moni, M.A.; De Oliveira, T.E.A. Advances in Artificial Intelligence and Blockchain Technologies for Early Detection of Human Diseases. IEEE Trans. Comput. Soc. Syst. 2024, in press. [Google Scholar] [CrossRef]
- Sun, L.; Liu, D.; Wang, M.; Han, Y.; Zhang, Y.; Zhou, B.; Ren, Y. Taming Unleashed Large Language Models with Blockchain for Massive Personalized Reliable Healthcare. IEEE J. Biomed. Health Inform. 2025, in press. [Google Scholar] [CrossRef]


| Research Questions: | Rationale: |
|---|---|
| RQ1: What is the current state of BC technology research in healthcare? | This is a rapidly developing research area, so it would be relevant to obtain an impression of the research published over the past five years, their venues, and origin. |
| RQ2: Which fundamental healthcare avenues used BC technology to solve issues raised by earlier studies? | BC technology revolutionizes new healthcare applications, but studies highlighted many new ventures in the infancy of many healthcare areas. So, it becomes paramount to explain its fundamentals and ways to solve healthcare challenges raised by developments explored by our research. |
| RQ3: What are the strengths and weaknesses catered from BC-based healthcare implementations? | BC-based healthcare implementations offer significant advantages, but they also invoke new methodological limitations. So, an overview of the strengths and weaknesses derived from current research takes a clear picture for real-world uses. |
| RQ4: How do BC-based applications, their applied research methods, data analysis, and evaluation metrics correlatively contribute to present and possible future prospects for healthcare development? | Understanding methods, data sources, and respective evaluation emphasizes implementation. So, this part aims to explain BC design development methods, data analysis, and evaluation metrics by reporting those developments that analyzed data as qualitative or quantitative evidence. Here, we also report effective outcomes from the insights of evaluation matrices. |
| Inclusion Criteria (IC): | Exclusion Criteria (EC): |
|---|---|
| IC1: Original peer-reviewed research articles such as primary research articles and concept articles that specifically address the applications of BC in healthcare core avenues. | EC1: Review articles and secondary analyses of previously published articles that do not bring any new information, book chapters, proceedings from symposiums, commentaries, or articles in magazines. |
| IC2: English language studies published between July 2019 and July 2024 (last five years). | EC2: Duplicated studies. |
| IC3: Availability of complete texts in search machines. | EC3: Exclude based on bias/quality assessment criteria. |
| IC4: Proposed implementations or developments adequately address BC methods and techniques in core healthcare avenues. | EC4: Studies that only propose design, system, model, or framework for BC in healthcare applications without implementation or intervention. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shaikh, M.; Memon, S.A.; Ebrahimi, A.; Wiil, U.K. A Systematic Literature Review for Blockchain-Based Healthcare Implementations. Healthcare 2025, 13, 1087. https://doi.org/10.3390/healthcare13091087
Shaikh M, Memon SA, Ebrahimi A, Wiil UK. A Systematic Literature Review for Blockchain-Based Healthcare Implementations. Healthcare. 2025; 13(9):1087. https://doi.org/10.3390/healthcare13091087
Chicago/Turabian StyleShaikh, Mutiullah, Shafique Ahmed Memon, Ali Ebrahimi, and Uffe Kock Wiil. 2025. "A Systematic Literature Review for Blockchain-Based Healthcare Implementations" Healthcare 13, no. 9: 1087. https://doi.org/10.3390/healthcare13091087
APA StyleShaikh, M., Memon, S. A., Ebrahimi, A., & Wiil, U. K. (2025). A Systematic Literature Review for Blockchain-Based Healthcare Implementations. Healthcare, 13(9), 1087. https://doi.org/10.3390/healthcare13091087






