Abstract
Pregnancy and childbirth can have far-reaching effects on women’s pelvic floor health. It is important to educate pregnant women about pelvic floor health and potential birth-related pelvic floor (PF) changes as part of continuous midwifery care. This scoping review aims to identify the current state of research on knowledge and knowledge gaps in pregnant women regarding the PF and PF dysfunction (PFD) in order to derive conclusions and recommendations for midwifery care and midwifery science. This review follows the Arksey and O’Malley framework and the PRISMA Statement. The literature search was conducted on databases PubMed, CINAHL, and Web of Science using various search terms and defined inclusion criteria. Eleven articles were included. The results show a considerable context-related knowledge deficit among pregnant women, with a high prevalence of PFDs such as urinary incontinence (UI), fecal incontinence (FI), or prolapse symptoms (POP). All contributions emphasize the importance of improved specific education and health advice regarding the PF and PFD for pregnant women to close knowledge gaps and promote sustainable PF health. Demands are made on the professional group ‘midwife’, which emphasize the importance of specific and target group-appropriate educational concepts on the subject of the PF and PFD.
1. Introduction
Pregnancy, childbirth, and the postpartum period are significant events in a woman’s life that are accompanied by profound physiological, psychological, and emotional changes. In addition to these changes, women are exposed to increased health risks, including a higher likelihood of developing pelvic floor dysfunction (PFD) such as urinary incontinence (UI), fecal incontinence (FI), or pelvic organ prolapse (POP) [1,2]. The prevalence of urinary incontinence during pregnancy is considerable; in the first trimester, 8–10% of women are affected, rising to 23–32% by the time of delivery. After birth, the prevalence remains high; up to 36% report UI after 6–13 weeks, 31% after 6 months, and even 51% after one year postpartum [3,4]. Even long-term data indicate a persistent burden; around 38% of women report UI 20 years after giving birth [5]. Existing or persistent urinary incontinence during pregnancy and in the early postpartum period has been identified as a significant risk factor for long-term incontinence up to 12 years later [6]. PFDs can have a significant impact on women’s quality of life. The associated consequences include mental illnesses such as depression and anxiety, sexual dysfunction, limited social participation, and restrictions on physical activity [7]. Due to the intimate and often shameful nature of the subject, many affected women are reluctant to ask questions or seek support. Insufficient information from healthcare professionals or midwives contributes to postpartum PFD being seen as a normal and expected outcome of labour, leading to underdiagnosis and inadequate treatment [8,9]. Particularly concerning is that pregnant women know little about the proven preventative effects of pelvic floor muscle training (PFMT). Structured and supervised PFMT, which includes alternating contraction and relaxation of the pelvic floor muscles and pelvic floor awareness exercises, has been shown to be effective in reducing the risk of postpartum UI and FI, particularly in continent pregnant women [10,11]. Nonetheless, adherence to regular PFMT during pregnancy remains low [10,12,13]. This underlines the importance of sensitising pregnant women to the health of the pelvic floor and possible changes in pelvic floor function (PFF) caused by pregnancy or childbirth. It also emphasises the need to provide them with comprehensive information about prevention strategies and how to implement them in everyday life. In Germany, midwives play a central role in promoting pelvic floor health during pregnancy and in the postnatal period. Counselling and guidance on protecting and strengthening the pelvic floor are among the core tasks of midwives, who therefore bear a great responsibility for maintaining perineal health [14,15]. Effective and targeted counselling requires knowing what pregnant women know—or do not know—about the anatomy and function of the pelvic floor and about possible pregnancy-related PFDs.
The aim of this review is therefore to examine the current state of research on the knowledge and health literacy of pregnant women in relation to pelvic floor anatomy, function, and dysfunction. By identifying existing knowledge and gaps, this review provides recommendations for midwifery science and the development of appropriate counselling and education strategies.
2. Methods
This form of scoping review is suitable for the existing research question, as this is a relatively new field of research within midwifery science, and existing evidence is to be presented and structured [16]. This paper followed the basic work by Arksey and O’Malley [17], the explanations by Levac et al. [18], the PRISMA 2020 Statement [19,20,21,22], and further recommendations by von Elm et al. [16]. The priori protocol was not registered. Two researchers were involved in the following steps and phases. The following steps were derived and completed: phase 1, identifying the research question; phase 2, identifying relevant studies; phase 3, selecting the studies; phase 4, charting the data; and finally, phase 5, collecting, summarizing, and reporting the results [16,17,18].
Phase 1: Identification of the research question
The research question was formulated according to the PCC framework, which stands for population, concept, and context [16]. The aspects included are listed in Table 1. The resulting research question is: ‘What do pregnant women know about their pelvic floor and the impact of pregnancy on potential pelvic floor dysfunction?’ The aim of the review is to map the available evidence to gain an overview of the following questions:

Table 1.
PCC framework.
- What ideas do pregnant women have about PF anatomy and PFF?
- What basic knowledge is available on PFD in the context of pregnancy and birth?
- What is the level of knowledge on the prevention of PFD or on measures to restore PF health in the case of pregnancy-associated PFD?
- What factors promote an improvement in the level of knowledge of pregnant women regarding the PF and possible pregnancy-associated PFDs?
- Which medical services are sought by pregnant women with PFDs?
Phase 2: Identifying relevant studies
A comprehensive search strategy was used to identify the relevant literature. Using specific keywords and search terms, placeholders, and Boolean operators ‘OR/AND’ as well as truncation (*) in the word stem “pregnancy”, various databases were searched for topic-specific articles. The literature search was carried out in consultation and in cooperation with the Medical Library of the University Hospital Tuebingen. The three large and medically relevant databases PubMed (Medline), CINAHL, and Web of Science were selected. Table 2 shows the search strategies described with the corresponding search terms:

Table 2.
Search strategy.
Phase 3: Study selection
The first step in selecting relevant studies was to remove duplicates and short meeting abstracts after importing all the studies searched for into a Microsoft Excel file. The remaining studies were imported into the EndNote 21 software. The articles were then checked for suitability of the title and abstract. After excluding articles that did not fit the research question, the remaining articles were checked for suitability by means of full-text screening and examination of inclusion criteria for the final inclusion of the relevant study articles in this scoping review. The literature search and selection took place between July and August 2024 and was carried out by two independent researchers. The inclusion or exclusion of various articles was discussed in personal conversations and discursive consensus. In order to obtain a comprehensive overview of the topic of this literature review, literature from January 2004 to 31. July 2024 was included. The type of study was not restricted to implementing a search strategy that was as sensitive as possible. Publications in English and German were considered. Associated inclusion criteria are shown in Table 3.

Table 3.
Inclusion criteria.
Type of Sources
A critical appraisal of studies is not intended in a scoping review [16,18]. The scoping review approach chosen here allows for the exploration of research questions even in areas where only limited literature is available. A formal critical appraisal might otherwise exclude studies that offer valuable insights relevant to the research question. Thus, all types of studies focusing on the knowledge of pregnant women on the PF and PFD were included. A national and international overview is provided by German and English language publications from the last 20 years that were included in the screening process. Data were only extracted if a German or English translation of the full text was available. Short articles, such as published poster presentations, were not included. Furthermore, studies that investigated the knowledge of the PF or PFD in non-pregnant women were not included. Further exclusion criteria were publications before January 2004, exclusive research subject pelvic floor muscle training during pregnancy or postpartum with or without forms of incontinence, and sexual behaviour during pregnancy. Although a sensitive search was conducted from 2004 onwards, relevant publications were available between 2016 and 2024.
Phase 4: Charting the data
The data extraction was based on the objective and research question of this scoping review, which led to a descriptive summary of the results. The following characteristics were extracted from the literature and summarized in a Table: author, year, title, country, objective, population, methods (Table 4), and relevant outcomes and recommendations (Table 5).

Table 4.
Analyzed studies.

Table 5.
Important results and derived recommendations.
Phase 5: Collecting, summarizing, and reporting the results
At this point, information was extracted from eleven studies conducted in nine different countries. The research question specified in Step 1 could be answered on the basis of the study characteristics defined in Step 4. In this way, important findings can be presented with regard to the research question of this literature review.
3. Results
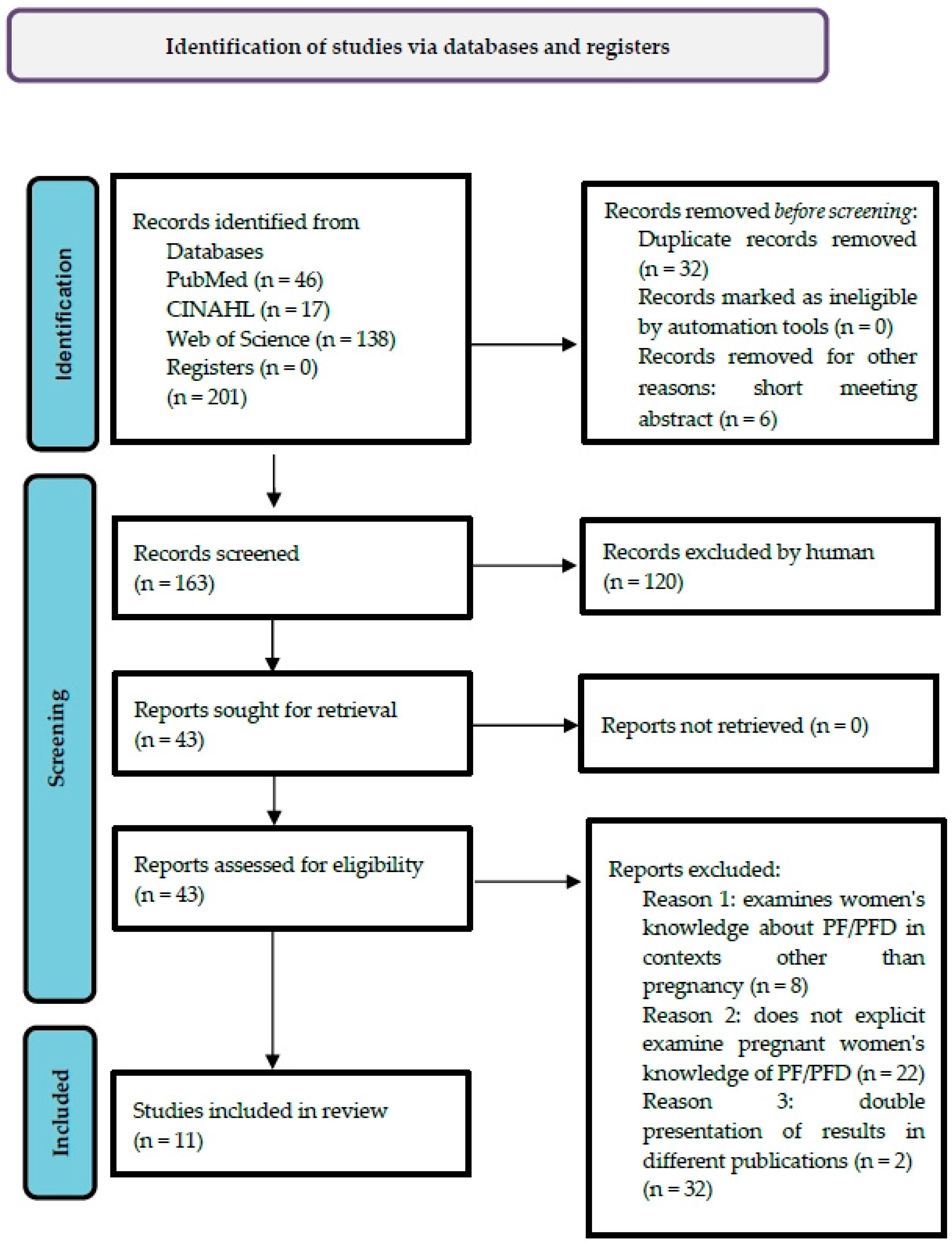
The literature search identified 201 relevant records in three databases, of which 32 duplicates and 6 short meeting abstracts were removed. After reviewing n = 163 records for title and abstract, n = 43 remaining articles were identified for subsequent full-text screening for the inclusion criteria presented. This was followed by the exclusion of n = 32 articles that did not meet the inclusion criteria. Thus, n = 11 articles were included in this literature review. The search process is illustrated in the PRISMA flow diagram [22] (Figure 1):
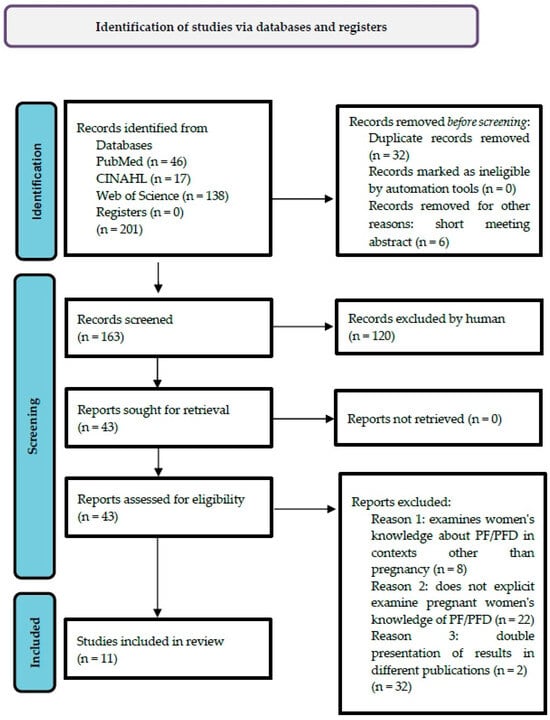
Figure 1.
PRISMA Flow Diagram.
3.1. Characteristics of Included Sources of Evidence
All sources were scientific publications in scientific journals. The included articles were published between 2016 and 2024 and were from nine different countries [23,24,25,26,27,28,29,30,31,32,33]. Two each of the eleven integrated studies originated from the USA and Turkey. In addition, one study each from the UK, Australia, Malaysia, Singapore, Israel, Brazil, and Ethiopia was integrated. What all the studies had in common was that they investigated pregnant women’s knowledge of PF, PFF, and PFD. Ten of the eleven studies were conducted in a quantitative design, of which two were multicentre-cross-sectional surveys [23,24] and eight were cross-sectional surveys [25,26,27,28,29,30,31,32]. Seven out of ten studies [23,25,26,29,30,31,32] used the validated 24-item Prolapse and Incontinence Knowledge Questionnaire (PIKQ) with outcome measures of knowledge in UI and POP as the baseline instrument. This provides three response options for items in each assigned subscale. The correct answer ‘Agree’ is scored as 1, the answers ‘Disagree’ and ‘Not sure’ are scored as 0. A score of at least 10 out of 12 on the UI subscale and 6 out of 12 on the POP subscale is considered good knowledge competence [34]. In two studies, the additional instrument of the validated Pelvic Floor Distress Inventory-20-Questionnaire (PFDI-20) was used with outcome measures for the diagnosis and severity of PFD, such as UI, POP, and FI [23,25]. Here too, a total score (0 to 300 points) from 20 questions in 3 dimensions (UI/POP/FI) reflects the individual burden of PFD. The higher the score, the higher the individual symptomatic burden [35]. One study used a self-designed validated questionnaire based on the PIKQ [24]. Two further studies supplemented the PIKQ with additional questions [30,31]. One study [29] used the validated Urinary Incontinence Attitude Scale (UIAS) [36] as a second instrument, which measures attitudes towards UI. Another study utilized a specially designed, validated, and piloted questionnaire with items that measured awareness of PFMs and knowledge of PFMs and PFMTs, and explored the role of PFMs as a key function in the prevention of UI [27]. Another study utilized a specially designed, validated, and piloted questionnaire with outcome measures regarding knowledge of PFD (UI/POP/FI) and how they relate to pregnancy and childbirth [28]. Only one study was conducted using a qualitative design. The focus here was on conducting a semi-structured interview on knowledge about the PF and the reproductive system, as well as a graphic representation of this by the study participants [33].
3.2. Literature Synthesis
The detailed study description and its results within the literature synthesis are listed in Table 4 and Table 5. The results (Table 5) represent the key aspects with regard to the knowledge of pregnant women in the context of the PF and PFD, which illustrate the challenges and opportunities for midwifery science.
The following section summarizes the findings of the included studies based on the initially formulated aspects of the research question and addresses both commonalities and discrepancies among the studies.
3.2.1. Knowledge and Ideas About Pelvic Floor Anatomy and Pelvic Floor Functions
Three studies show that pregnant women have little knowledge of PF anatomy and the functions of the various PFMs [27,31,33]. While anatomical structures of the reproductive system, including the uterus, fallopian tubes, and ovaries, are known, the PMF as part of the female body is difficult to visualize and comprehend due to its hidden structure [33]. For example, Hill et al. found that only 5.4% of the study population were able to describe the correct PF anatomy. Only 54% of the study participants knew that the PFMs run around the bladder opening, and a further 20% were unable to categorize the function of the PFMs [27]. Toprak Celenay et al. show similar results with regard to knowledge of PFM functionality; approximately one third of the study population was unable to establish a link between intact PFM function and PF health [31]. Kammers et al. showed that the pregnant women involved had a good visualization of the anatomical structures of the organs of the female reproductive system, but the PFMs were judged to be difficult to comprehend. These appear to be hidden as muscular structures and are associated with the sexual experience of women, which is generally taboo, but especially during pregnancy [33].
3.2.2. Basic Knowledge of Pelvic Floor Dysfunctions (UI, POP, FI) in the Context of Pregnancy and Birth
Overall, pregnant women’s knowledge of PFDs such as UI and POP is low [23,24,25,26,27,28,29,30,31,32]. This also applies to FI [24,28]. UI during pregnancy sometimes appears to be considered ‘normal’ by women [27,29], and UI or POP is also categorized as unproblematic or not necessarily requiring treatment [31]. Although the general level of knowledge with regard to PFD can be categorized as low, it is apparent that there is more knowledge about the pathogenesis and perception of UI compared to POP [24,26,28,31,32] or POP and FI [24,28]. Geynisman-Tan et al. reported a mean knowledge score on UI of 7.9 out of 12 points (66% ± 12) and on POP of 4.9 out of 12 points (41% ± 17) [26]. Liu et al. showed an increased knowledge of UI (46.2 ± 0.3%), followed by FI (39.8% ± 0.3) and POP (35.3% ± 0.3) [28]. O’Neill et al. reported that knowledge of UI (63%) was the highest, followed by POP (36%) and FI (35%) [24]. Toprak Celenay et al. also showed an increased knowledge of UI followed by POP. The mean PIKQ-UI score was 6; the mean PIKQ-POP score was 5 out of 12 points [31]. Similarly, Yohay et al. showed an average higher knowledge of UI (7.65 ± 2.8) compared to POP (5.32 ± 2) [32].
Individual studies investigated participants’ knowledge of whether the occurrence of PFD postpartum was associated with vaginal birth [23,26,29]. This only appears to be the case to a limited extent. Geynisman-Tan et al. showed that only 62.5% of respondents knew that multiple childbearing was a higher risk for UI, compared to only 43% of respondents who knew that the same was true for an increased risk of POP [26]. Similarly, the study by Mckay et al. shows that 49.7% and 29.2% of the pregnant women included in the study knew that multiple births were a risk factor for UI and POP [23]. Parlas and Bilgic also show that in their study population, only 56.1% of participants considered multiple births to be a risk factor for UI [29].
3.2.3. State of Knowledge on the Prevention of Pelvic Floor Dysfunction or on Measures to Restore Pelvic Floor Health in the Presence of Pregnancy-Associated Pelvic Floor Dysfunction
In the context of preventive or therapeutic PFMT during pregnancy, there is also a low level of knowledge among pregnant women [26,27,28,29,30]. Geynisman-Tan et al. showed that 83% of the study participants (n = 402) knew that UI can be counteracted by PFMT, but only 55% of the study population saw a relationship with POP [26]. Hill et al. described that 40% of the study participants (n = 633) considered UI during pregnancy to be ‘normal’ [27]. Many pregnant women do not realize that PFMT can be helpful in preventing or reducing UI during pregnancy. According to Hill et al., this was the case in one-third of all respondents [27] and in 40% of the study participants for Liu et al. [28]. Parlas and Bilgic reported that in their overall study population (n = 255), 44% did not know to what extent they could prevent UI themselves or how they could treat it. Only 53.3% of participants knew that UI can be prevented or reduced by PMFT. Only 6.7% of participants were already aware of PFMT, 37.2% had heard of PMFE, and 16.5% had performed PFMT for the prevention or management of UI [29]. Hill et al. reported that only 11% of the study cohort performed PFMT during pregnancy, and a further 30% were unsure if they had ever contracted their PFM [27]. This finding is also confirmed by Tennfjord et al. Within their study population (n = 502), there was also a low level of knowledge about preventive or therapeutic PFMT and a low level of implementation of preventive or therapeutic PMFT. Only 26.6% of participants had even heard of PMFT. Compared to multiparous women, first-time mothers had slightly better knowledge and attitudes towards PFMT, while multiparous women had slightly better PFMT practice [30].
3.2.4. Factors That Support an Improvement in Pregnant Women’s Knowledge of the Pelvic Floor and Possible Pregnancy-Associated Pelvic Floor Dysfunction
A number of factors have a favourable effect on the context-related knowledge of pregnant women. Increasing maternal age [28,30,32] and higher levels of education and training [23,24,25,28,30,32] are associated with significantly improved knowledge and understanding of the PF and PFD. A linguistic understanding of the local language can be seen as an important prerequisite for acquiring knowledge [27]. High socio-economic status [28,32], employment [28] and nulliparity [28,30] are also discussed as promoting the acquisition of knowledge. Two studies show that pregnant women who work as healthcare professionals have a higher level of knowledge about UI and POP [23], or significantly higher than pregnant women who do not [32]. Similarly, attending antenatal education (ANE) courses improves [31] or significantly improves [27] knowledge of PFF and PFD. However, ANE does not necessarily appear to be a positive resource for improving knowledge of PFD [24]. Specialist care during pregnancy is associated with better knowledge of PFD [25]. Access to the specialities of urology/urogynaecology is associated with higher knowledge of POP [23] and significantly higher knowledge of UI [32].
The main sources used by pregnant women to acquire knowledge about PFD are the internet [24,27,31] and the media as a superordinate, unspecified domain [30]. Books are an important source of information on pregnancy and childbirth [24] and other information on PFM [27] and PFD [24,31]. Family and friends [24,30,31] as well as medical staff [24,30,31] and midwives [24,27,31] are listed as groups of persons who are consulted by pregnant women to acquire knowledge about PFM and PFD.
3.2.5. Seeking Medical Help for Pregnant Women in the Event of Pelvic Floor Dysfunction
A large number of studies report a high prevalence of PFD in the context of pregnancy and childbirth [23,25,28,29,31]. During pregnancy, UI occurs most frequently, followed by POP and FI [25,28,29,31]. Four studies graded the prevalence of UI, POP, and FI [25,28,29,31]. UI is the most common form of PFD during pregnancy. Farihan et al. reported that 46.1% of n = 424 primiparous and multiparous women developed PFD, with 62.7% developing UI, 41.1% developing symptoms of POP, and 37.8% developing symptoms of FI [25]. Liu et al. also recorded a UI-prevalence of 31.7%, a POP-prevalence of 2.9%, and an FI prevalence of 0.96% in a study population of n = 104 primiparous women [28]. Parlas and Bilgic showed a high UI prevalence of 51% in n = 255 primiparous and multiparous women [29]. Toprak Celenay et al. showed a UI-prevalence of 18.9% and symptoms of POP-prevalence of 3.6% within their study population of n = 241 primiparous women [31]. Despite this relatively high prevalence of PFD in pregnant women, three studies reported that affected pregnant women rarely seek medical help. This applies to pregnant women who have newly developed symptoms of UI, POP, and also FI, or who already had them [28,29,31].
4. Discussion
4.1. Summary of the Results
The literature synthesis of 11 studies [23,24,25,26,27,28,29,30,31,32,33] shows a lack of knowledge among pregnant women about PF anatomy and PFF [27,31,33] and in the area of possible pregnancy-associated PFDs [23,24,25,26,27,28,29,30,31,32]. In addition, there is little knowledge with regard to the prevention of PFD [26,27,28,29,30] and medical assistance is relatively rarely utilized [28,29,31]. The main sources used by pregnant women to acquire knowledge about PFDs are the internet [24,27,31] and the media [30].
4.1.1. Knowledge and Ideas About Pelvic Floor Anatomy and Pelvic Floor Functions
The lack of knowledge about PF anatomy and PFF among pregnant women [27,31,33] is obviously due to a lack of knowledge among women of reproductive age as a whole. In the Irish study by Falvey et al. [37], 895 female students were surveyed on their knowledge of the PF. This demonstrated a low level of knowledge about PF anatomy and PFF. For example, only 48% of participants knew that the PF consists of muscles. Only 50% of the participants were able to correctly categorize the body orifices urethra, vagina and anus as part of the PF [37]. In a Belgian study of 212 women who had not yet given birth and were not pregnant, it was shown that there was a lack of knowledge about the PF. Only 13% of respondents were able to correctly identify the number of female orifices. Only 73% were able to name at least one function of the PF, and only 20% were aware of the role of the PF in sexual function [38]. In another Brazilian study, only 20.3% of 133 women of childbearing age were able to name various functions of the PF [39].
Kammers et al. discussed, that even in the modern age, a shameful, conservative, lack of sex education or the historically evolved view of a female ‘sinful’ body underpins a low or rudimentary knowledge of female PF and PFF. They emphasize the importance of an enlightened sexu-al and educational policy, starting in schools and continuing during pregnancy, in order to preventively promote sexual and pelvic floor health [33]. Furthermore, suitable prenatal education programmes for pregnant women are considered necessary. These should in-clude explicit anatomy and function of the PF, but also possible pregnancy-associated PF changes, in order to promote the PF health of pregnant women and preventively counter-act PFD [27,31].
4.1.2. Basic Knowledge of Pelvic Floor Dysfunctions (UI, POP, FI) in the Context of Pregnancy and Birth
The lack of basic knowledge about PFD among pregnant women [23,24,25,26,27,28,29,30,31,32] is also reflected in a general lack of knowledge among women of reproductive age. The results of a Spanish study showed in their survey of 768 female students that overall knowledge of PFDs was moderate. The overall PIKQ score was 14 out of 24 points to be achieved (14 ± 6.919). The participants showed significantly better UI skills compared to POP (8.89 ± 2.861 vs. 5.19 ± 4.543) (p < 0.001) [40]. Freitas et al. were also able to show in their study that UI and POP were only known to 25.6% of the participants. With regard to their possible treatment options, only 23.3% were able to name them correctly [39]. The influence of pregnancy and childbirth on developing PFDs appears to be underestimated overall. Neels et al. showed that the risk factor for a possible developing UI, POP, or FI was correctly assigned by only 9% of the participants in their study population of 212 women.
Most participants were aware of the risk of pregnancy and childbirth, and only associated these with the risk of UI [38].
4.1.3. State of Knowledge on the Prevention of Pelvic Floor Dysfunction or on Measures to Restore Pelvic Floor Health in the Presence of Pregnancy-Associated Pelvic Floor Dysfunction
The lack of basic knowledge on the prevention of PFD or restoration of pelvic floor health in pregnant women [26,27,29,30] is also reflected by a general lack of knowledge among women of reproductive age. Falvey et al. showed that 83.9% of their study population rated preventive PFMT as important, but 57.6% of women had never performed PFMT before, and only 6% of participants practiced PFMT regularly [37]. Neels et al. showed that 92.7% of their study population did not feel sufficiently informed about the overall context of the PF and PFD. Furthermore, 92.8% of the participants did not know what PFMT was, and 97.1% had never performed PFMT [38].
4.1.4. Factors That Support an Improvement in Pregnant Women’s Knowledge of the Pelvic Floor and Possible Pregnancy-Associated Pelvic Floor Dysfunction
Pregnant women cite the internet as the main source of knowledge about PFD [24,27,31]. All authors also reported that the internet as a source of knowledge does not significantly improve knowledge about the PF and PFD [24,27,31]. Hill et al. pointed out that non-English-speaking study participants used the internet significantly less than those who spoke English at home [27]. Tennfjord et al. showed overarching and unspecified media as the main source used for contextualized knowledge acquisition by pregnant women, although there was also a low overall knowledge of UI and POP in this study [30]. Overall, the authors listed criticized the fact that on the one hand, the internet is a preferred medium for acquiring knowledge, which appears to have a higher status than healthcare professionals, but at the same time the content presented does not appear to be sufficient to generate adequate knowledge of PFM or PFD for pregnant women [24,27,30,31].
Books are used as an important source of information about pregnancy and birth [24] and also for information about PFM [27] and PFD [24,27,31]. O’Neill et al. reported that pregnant women with a high level of education, in particular, generate context-related information from books. At the same time, they had significantly better knowledge of UI and POP [24]. Hill et al. showed something similar and also found that books are mainly used by English-speaking pregnant women to acquire knowledge about PFM. In comparison, pregnant women who were not usually English-speaking used them significantly less [27].
In their study, Hill et al. explicitly pointed out that speaking and understanding the respective national language significantly increases knowledge about PFM compared to women who do not speak it [27]. A study from Denmark shows a general trend that pregnant migrant women in various validated surveys have both lower e-health literacy and health literacy compared to women of Danish origin. The researchers do not see the reason for this in the lack of motivation of pregnant migrant women to engage with the internet or e-books. Rather, ethnic minorities as a whole appear to face greater challenges in terms of language barriers combined with a lack of ability to use digital technology, which affects their e-health literacy [41].
Family members and friends are further sources of information for pregnant women [24,30,31], but do not necessarily lead to an increase in knowledge about UI and POP in the context of pregnancy and birth [24].
The finding that pregnant women who work as healthcare professionals have a higher level of knowledge about UI and POP [23,32] is consistent with that of Pizzoferrato et al. [42]. Here, medical professionals (MF) were asked about their knowledge of PFM and PFD compared to women in the general population (n = 856). The authors found that around half of the women surveyed without a medical specialism had a significant lack of knowledge about PFM and PFD. Thus, the medical professional (MF) background appears to be an effective protective factor against a lack of knowledge in this context [42].
Specialist care during pregnancy is associated with better knowledge of pelvic floor dysfunction in three studies. Farihan et al. reported that pregnant women who received antenatal specialist care had better knowledge of UI and POP (p = 0.000) than pregnant women who received care from medical officers or health care trainees [25]. Mckay et al. showed that pregnant women who have already been treated by a urologist or urogynaecologist tend to have a higher level of knowledge about POP [23]. Yohay et al. reported significantly higher knowledge of UI and POP when pregnant women had already seen a urologist/urogynaecologist (p = 0.004). Furthermore, pregnant women who had previously shown UI symptoms and had already received treatment were significantly more knowledgeable about UI [32]. DeLancey et al. and Hübner et al. [43,44] also emphasized the importance of sufficient specialist knowledge with regard to possible pregnancy-associated changes in PF. They recommend that pregnant and postnatal women receive adequate knowledge transfer from professional groups. Only in this way can they be empowered to make informed decisions regarding their pelvic floor health in the overall context of pregnancy and birth, and at the same time be provided with the necessary therapeutic measures. The specific transfer of knowledge on the PF and PFD by gynaecological and urogynaecological specialists is an important basis for strengthening women’s health literacy [43,44].
Kammers et al. suggest that knowledge regarding the anatomical structure of the PF could only be improved through open sexual education and sex education in schools and in families. Even in the modern age, a shameful, conservative outlook and lack of sex education, or even the historically grown view of a female ‘sinful’ body, underpins a low or rudimentary knowledge of the female PF and PFF [33]. Further studies show that a lack of knowledge about the female PF anatomy may be due to a sense of shame on the part of both women and healthcare professionals. As a result, pregnant women or women after the birth are often not sufficiently informed or not informed at all due to shame [8,9].
Attending antenatal education (ANE) courses can significantly improve [27] or improve [31] knowledge of PFM and PFD. Hill et al. showed that ANE participants had significantly more knowledge about PFM and UI compared to pregnant women who had not participated in ANE [27]. Toprak Celenay et al. showed similar results. Pregnant women who attended ANE had a higher, but non-significant, mean knowledge of UI and POP than pregnant women who had not attended ANE [31]. In contrast, O’Neill et al. reported that in their study population, only 35% of n = 249 study participants reported attending ANE as a resource for improving their knowledge of PFD [24]. It can be assumed that ANE will be provided by midwives within the studies conducted and discussed [45,46,47].
However, the midwifery profession as a whole seems to be insufficiently effective as a knowledge broker in the context of PFM and PFME. According to Hill et al., midwives do not significantly improve PF health education for pregnant women within the ANE. For example, the author states that only 50% of the study participants received information on PFD, although up to 50% of the study population already reported UI. In addition, it is evident that the information provided was not appropriate for the target group, especially when pregnant women do not speak the local language (English) [27]. O’Neill et al. show a similar conclusion. Although midwives are the most frequently mentioned source of information among health professionals for pregnancy and childbirth, they do not seem to be able to improve knowledge about the PF or PFD [24]. In Turkey, the concept of ANE is not yet well established, and this also applies to the professional group of midwives who manage an ANE [45,48]. Nevertheless, the midwifery profession does not appear to contribute to increased knowledge of the PF and PFD here either [31]. The authors assume that birth and infant care were more focused upon during the ANE that took place [31]. In principle, however, ANE seems to offer a good starting point for improving pregnant women’s knowledge of PFM or PFD. ANE can be seen as a targeted educational service provided by midwives that strengthens and promotes physiological processes in the transition to parenthood and thus has a strengthening effect on health literacy [49,50]. In this context, Butterfield et al. and Terry et al. stated that the midwifery profession lacks consistent guidelines, clear communication, and evidence-based knowledge in the specific area of PF, PFME, and PFD in antenatal education (ANE) [51,52]. An important content must therefore be to convey evidence-based knowledge with regard to the promotion of PF health to pregnant women in a structured and target group-orientated way [51,52].
4.1.5. Seeking Medical Help for Pregnant Women in the Event of Pelvic Floor Dysfunction
The data presented in the studies on the prevalence of PFD [25,28,29,31] corresponds to other studies that show the development of UI [3,4], FI or POP [5,53] in the context of pregnancy. The fact that pregnant women rarely seek medical help despite having PFDs [28,29,31] is explained by Liu et al. with a possible social taboo and a lack of knowledge and awareness of PFD among study participants [28]. Parlas and Bilgic reported that only 33.9% of pregnant women affected by UI symptoms (51% of study participants) sought medical help. Here too, the authors attribute this to the study participants’ lack of knowledge about PFD [29]. Toprak Celenay et al. also showed the same for UI and POP [31]. One possible reason, which has already been discussed, is that the topic of PFD is a taboo subject in the context of pregnancy and childbirth, and also fundamentally for women at all stages of life [8,9]. Further studies confirm this. UI is considered embarrassing by those affected, and therefore no medical help is sought. Overall, affected women lack contextualized knowledge [54,55].
4.2. Limitations
The methodology of the review was conducted without a critical appraisal of the included studies [16,18]. As shown in Table 4, various studies and study types with different data reports were included, with the presented results based almost exclusively on cross-sectional designs. The heterogeneity of the measurement instruments used in the included studies also warrants critical evaluation. For instance, tools such as the PIKQ, the PFDI-20, or self-developed, validated, and piloted questionnaires were employed to assess women’s individual knowledge of pelvic floor health. Moreover, the studies varied in sample size and setting. It is important to note that the results of this review are based on surveys conducted within globally heterogeneous healthcare systems and incorporate diverse cultural backgrounds. Although a systematic and sensitive search was carried out, it was performed on only three medically relevant databases. An increase in additional medical databases could have increased the validity of the review. Further restrictions include the exclusive search for publications in German and English in the period January 2004-July 2024. This may result in a potential language bias. Therefore, these results should be treated with appropriate caution.
4.3. Research Gaps and Future Directions
This scoping review, conducted in line with established methodological standards [16,17,18,21], highlights several important gaps in the current evidence on pregnant women’s knowledge of PF health. Despite a systematic and sensitive search, only a limited number of relevant studies were identified. None of the included studies originates from German-speaking countries, which limits the direct transferability of findings. However, Ayerle, and Mattern [56] emphasize that PF health is also a relevant and under-researched topic in German midwifery science, as pregnant women explicitly express a need for evidence-based support. Most studies lack socio-demographic differentiation. Factors such as education level, migration background, language skills, and socioeconomic status, which strongly influence health literacy, are rarely examined in depth [27,41]. Women with low digital or general health literacy remain underrepresented. Methodologically, the dominance of cross-sectional designs limits the depth of understanding regarding how knowledge evolves over time. Longitudinal and interventional studies are needed to evaluate the effectiveness of antenatal education (ANE) or specialist counselling [27,31]. While ANE shows some positive effects, the role of midwives as structured providers of PF education remains unclear and inconsistently implemented [24,27,31,51,52]. Qualitative research is also scarce, although several studies point to emotional and cultural barriers such as shame and taboo [8,9,33]. The increasing use of digital media by pregnant women as a primary source of information [24,27,30,31] raises concerns about the quality and accessibility of online content, especially for vulnerable groups. Finally, interdisciplinary perspectives are missing. Although specialist involvement is considered important [23,25,32,43,44], responsibilities among healthcare professionals are often undefined. Educational science, sociology, and psychology should be more strongly integrated into future research to enable comprehensive and culturally sensitive educational approaches.
4.4. Implications for Midwifery Science and Broader Practice
The findings of this scoping review clearly highlight the pivotal role of midwives in promoting pelvic floor health throughout pregnancy and the postpartum period. Midwives are uniquely positioned to support physiological processes and prevent pregnancy-related disfunctions through early risk detection, targeted education, and individualized interventions. However, the evidence shows that pregnant women generally have limited knowledge about PF anatomy, PF muscles (PFM), and pelvic floor dysfunctions (PFD), including urinary incontinence (UI), pelvic organ prolapse (POP), and fecal incontinence (FI) [23,24,25,26,27,28,29,30,31,32,33].
To address these knowledge deficits, midwives must make full use of their unique position as easily accessible experts for pregnant women to ensure a structured, evidence-based antenatal education. Relevant formats should be employed to provide fundamental information on PF anatomy and function, physiological changes during pregnancy, and the risk of pregnancy- and birth-related PFD. Preventive pelvic floor muscle training (PFMT) should be a standard component of this education. Antenatal education settings should systematically incorporate content on pelvic floor health, including basic anatomy, preventive behaviours, exercises to reduce the risk of incontinence, and information on treatment options. Participatory and culturally sensitive teaching methods, such as anatomical models, visual aids, and the use of plain language, have proven particularly effective, especially for women with low health literacy and women with a migrant background [57].
Combining verbal education with body-centered training, such as guided pelvic floor exercises, can enhance the effectiveness of information delivery. Web-based platforms should be evidence-based, interactive, and easily accessible. Recommended features include multilingual modules, practical videos, self-assessment checklists, and intuitive navigation to support users with low digital health literacy. Moreover, integrating expert-verified educational tools into prenatal care, such as apps, videos, or web modules developed by interdisciplinary teams, can help ensure that pelvic floor training websites are scientifically sound. Mobile health applications offering reminders and training instructions can further improve adherence and learning outcomes [58]. Overall, a combination of personalized midwife-led counselling and digitally supported education appears to be the most effective approach for sustainably improving PF knowledge during pregnancy and the postpartum period.
Where possible, midwives should also assess PFM function (e.g., via vaginal palpation and the Oxford score) to identify weakness or dysfunctions early and to initiate individualized support [59,60].
Furthermore, early life-stage interventions are warranted. Educational efforts on PF health should begin before pregnancy, ideally during adolescence. Current NICE guidelines recommend introducing girls and young women, starting around age 12, to the concept of PF health and preventive PFMT [61,62]. Midwifes could play a critical role in implementing such early education, which is urgently needed in heterogeneous global school and healthcare systems [63]. For example, by expanding existing initiatives like “midwives in schools” in Germany [64]. This may also help destigmatize PF-related topics and facilitate open discussions about sexual and reproductive health.
Given the increasing number of pregnant women with migration backgrounds, educational strategies must also be culturally sensitive and linguistically accessible. For migrant populations, it is crucial to consider cultural background, language barriers, and varying perceptions of the body and health. This should be supported through community-based access points, native-language facilitators, or cooperation with migrant organizations. Further initiatives could also be taken in the clinical setting, e.g., target-group-orientated protocols for shared care between primary care providers and public maternity hospitals, or even a commitment by hospitals to quality initiatives in the context of support for migrant women. The provision and use of interpreting services in clinical and non-clinical prenatal care should be a matter of course in order to address specific issues such as PF health appropriately and individually. Through supported interpersonal communication, women with a migration background can be enabled to understand important health information or develop adherence to treatment [57,65]. Although antenatal education is a reimbursable service in Germany [66] there is currently no national framework for standardized PF health content, and relevant professional guidelines lack clear assignments of responsibility [64,67]. The development of such standards, anchored in midwifery expertise, is essential.
These findings also point to broader interdisciplinary implications. The correlation between higher educational levels and greater PF health suggests a need to integrate PF topics into general health and sexuality education. From a sociological perspective, the persistence of shame and silence surrounding PFD highlights the importance of public discourse and cultural change. Psychiatrically, the psychological burden of undressed PFD, such as depression, anxiety, and social withdrawal, calls for collaboration with mental health professionals in prevention, education, and care pathways.
5. Conclusions
This scoping review synthesized existing evidence on the health literacy of pregnant women regarding pelvic floor anatomy, function, and dysfunctions. Across all included studies, a substantial knowledge gap was identified. No relevant data were found for Germany or German-speaking countries. But the findings can reasonably be applied to these contexts. These results emphasize the need for structured, targeted, and standardized education on PF health, delivered by midwives and integrated into both antenatal care and broader public health strategies. Midwives are ideally placed to lead this work, provided they are supported by national guidelines, institutional frameworks, and interprofessional cooperation. Educational content should be tailored to the literacy and cultural background of women, ensuring equal access to essential health knowledge. This review also reinforces the value of early education on PF health, particularly for girls and young women. Global inequalities in educational access, as documented by UNICEF [68], continue to limit opportunities for health promotion among adolescent females, especially in low-income countries. Addressing these disparities is critical for long-term improvements in women’s reproductive health. Pregnancy should be understood as a “teachable moment”, a time when women are particularly receptive to health information and motivated to engage in preventive behaviours [69,70]. Leveraging this period through coordinated educational strategies can have a lasting impact on women’s PF health, improve quality of life, and reduce the long-term burden of pelvic floor dysfunctions.
Author Contributions
Conceptualization, K.W. and C.F.P.; methodology, K.W. and C.F.P.; software, K.W.; formal analysis, K.W.; investigation, K.W.; writing—original draft preparation, K.W.; writing—review and editing, C.F.P.; visualization, K.W.; supervision C.F.P.; project administration, K.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
We acknowledge support from the Open Access Publishing Fund of the University of Tuebingen, as well as Diana Mader—Medical Library of the University Hospital of Tuebingen—for the support.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Blomquist, J.L.; Munoz, A.; Carroll, M.; Handa, V.L. Association of Delivery Mode With Pelvic Floor Disorders After Childbirth. JAMA 2018, 320, 2438–2447. [Google Scholar] [CrossRef] [PubMed]
- Van Geelen, H.; Ostergard, D.; Sand, P. A review of the impact of pregnancy and childbirth on pelvic floor function as assessed by objective measurement techniques. Int. Urogynecol. J. 2018, 29, 327–338. [Google Scholar] [CrossRef] [PubMed]
- Cerruto, M.A.; D’Elia, C.; Aloisi, A.; Fabrello, M.; Artibani, W. Prevalence, incidence and obstetric factors’ impact on female urinary incontinence in Europe: A systematic review. Urol. Int. 2013, 90, 1–9. [Google Scholar] [CrossRef]
- Metz, M.; Junginger, B.; Henrich, W.; Baessler, K. Development and Validation of a Questionnaire for the Assessment of Pelvic Floor Disorders and Their Risk Factors During Pregnancy and Post Partum. Geburtshilfe Frauenheilkd. 2017, 77, 358–365. [Google Scholar] [CrossRef]
- Gyhagen, M.; Bullarbo, M.; Nielsen, T.F.; Milsom, I. The prevalence of urinary incontinence 20 years after childbirth: A national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG 2013, 120, 144–151. [Google Scholar] [CrossRef]
- MacArthur, C.; Wilson, D.; Herbison, P.; Lancashire, R.J.; Hagen, S.; Toozs-Hobson, P.; Dean, N.; Glazener, C.; Prolong study, g. Urinary incontinence persisting after childbirth: Extent, delivery history, and effects in a 12-year longitudinal cohort study. BJOG 2016, 123, 1022–1029. [Google Scholar] [CrossRef]
- Jundt, K.; Peschers, U.; Kentenich, H. The investigation and treatment of female pelvic floor dysfunction. Dtsch. Arztebl. Int. 2015, 112, 564–574. [Google Scholar] [CrossRef]
- Buurman, M.B.R.; Lagro-Janssen, A.L.M. Women’s perception of postpartum pelvic floor dysfunction and their help-seeking behaviour: A qualitative interview study. Scand. J. Caring Sci. 2013, 27, 406–413. [Google Scholar] [CrossRef]
- Moossdorff-Steinhauser, H.F.A.; Berghmans, B.C.M.; Spaanderman, M.E.A.; Bols, E.M.J. Prevalence, incidence and bothersomeness of urinary incontinence in pregnancy: A systematic review and meta-analysis. Int. Urogynecol. J. 2021, 32, 1633–1652. [Google Scholar] [CrossRef]
- Morkved, S.; Bo, K. Effect of pelvic floor muscle training during pregnancy and after childbirth on prevention and treatment of urinary incontinence: A systematic review. Br. J. Sports Med. 2014, 48, 299–310. [Google Scholar] [CrossRef]
- Woodley, S.J.; Lawrenson, P.; Boyle, R.; Cody, J.D.; Morkved, S.; Kernohan, A.; Hay-Smith, E.J.C. Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst. Rev. 2020, 5, CD007471. [Google Scholar] [CrossRef] [PubMed]
- Stafne, S.N.; Salvesen, K.Å.; Romundstad, P.R.; Torjusen, I.H.; Morkved, S. Does regular exercise including pelvic floor muscle training prevent urinary and anal incontinence during pregnancy? A randomised controlled trial. Bjog-Int. J. Obs. Gynaecol. 2012, 119, 1270–1280. [Google Scholar] [CrossRef] [PubMed]
- Bayat, M.; Eshraghi, N.; Naeiji, Z.; Fathi, M. Evaluation of Awareness, Adherence, and Barriers of Pelvic Floor Muscle Training in Pregnant Women: A Cross-sectional Study. Female Pelvic Med. Reconstr. Surg. 2021, 27, e122–e126. [Google Scholar] [CrossRef]
- Schäfers, R. Gesundheitsförderung Durch Hebammen. Fürsorge und Prävention Rund um Mutterschaft und Geburt; Schattauer-Verlag: Stuttgart, Germany, 2011. [Google Scholar]
- Gesetz Über das Studium und den Beruf von Hebammen (HebG). Hebammengesetz vom 22. November 2019 (BGBl. I S. 1759), das Durch Artikel 10 des Gesetzes vom 24. Februar 2021 (BGBl. I S. 274) Geändert Worden ist. Available online: https://www.gesetze-im-internet.de/hebg_2020/BJNR175910019.html (accessed on 5 January 2025).
- von Elm, E.; Schreiber, G.; Haupt, C.C. Methodische Anleitung für Scoping Reviews (JBI-Methodologie). Z. Evid. Fortbild. Qual. Gesundhwes 2019, 143, 1–7. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- PRISMA 2020 Checklist. Available online: https://www.prisma-statement.org/prisma-2020-checklist (accessed on 18 February 2025).
- PRISMA 2020 for Abstracts: Reporting Systematic Reviews in Journal and Conference Abstracts. Available online: https://www.equator-network.org/reporting-guidelines/prisma-abstracts/ (accessed on 18 February 2025).
- The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Available online: https://www.bmj.com/content/372/bmj.n71 (accessed on 18 February 2025).
- PRISMA Flow Diagram. Available online: https://www.prisma-statement.org/prisma-2020-flow-diagram (accessed on 18 February 2025).
- McKay, E.R.; Lundsberg, L.S.; Miller, D.T.; Draper, A.; Chao, J.; Yeh, J.; Rangi, S.; Torres, P.; Stoltzman, M.; Guess, M.K. Knowledge of Pelvic Floor Disorders in Obstetrics. Female Pelvic Med. Reconstr. Surg. 2019, 25, 419–425. [Google Scholar] [CrossRef]
- O’Neill, A.T.; Hockey, J.; O’Brien, P.; Williams, A.; Morris, T.P.; Khan, T.; Hardwick, E.; Yoong, W. Knowledge of pelvic floor problems: A study of third trimester, primiparous women. Int. Urogynecol. J. 2017, 28, 125–129. [Google Scholar] [CrossRef]
- Farihan, M.N.; Ng, B.K.; Phon, S.E.; Azlin, M.I.N.; Azurah, A.G.N.; Lim, P.S. Prevalence, Knowledge and Awareness of Pelvic Floor Disorder among Pregnant Women in a Tertiary Centre, Malaysia. Int. J. Environ. Res. Public Health 2022, 19, 8314. [Google Scholar] [CrossRef]
- Geynisman-Tan, J.M.; Taubel, D.; Asfaw, T.S. Is Something Missing From Antenatal Education? A Survey of Pregnant Women’s Knowledge of Pelvic Floor Disorders. Female Pelvic Med. Reconstr. Surg. 2018, 24, 440–443. [Google Scholar] [CrossRef]
- Hill, A.M.; McPhail, S.M.; Wilson, J.M.; Berlach, R.G. Pregnant women’s awareness, knowledge and beliefs about pelvic floor muscles: A cross-sectional survey. Int. Urogynecol. J. 2017, 28, 1557–1565. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Tan, S.Q.; Han, H.C. Knowledge of pelvic floor disorder in pregnancy. Int. Urogynecol. J. 2019, 30, 991–1001. [Google Scholar] [CrossRef] [PubMed]
- Parlas, M.; Bilgic, D. Awareness of urinary incontinence in pregnant women as a neglected issue: A cross-sectional study. Malawi Med. J. 2024, 36, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Tennfjord, M.K.; Kassie, B.A.; Gashaw, Z.M.; Asaye, M.M.; Muche, H.A.; Fenta, T.T.; Chala, K.N.; Maeland, K.S. Pelvic Floor Disorders and Pelvic Floor Muscle Exercise: A Survey on Knowledge, Attitude, and Practice among Pregnant Women in Northwest Ethiopia. Int. J. Environ. Res. Public Health 2023, 20, 4201. [Google Scholar] [CrossRef]
- Toprak Celenay, S.; Coban, O.; Korkut, Z.; Alkan, A. Do community-dwelling pregnant women know about pelvic floor disorder? Women Health 2021, 61, 609–616. [Google Scholar] [CrossRef]
- Yohay, N.Z.; Weiss, A.; Weintraub, A.Y.; Daya, K.; Katz, M.E.; Elharar, D.; Yohay, Z.; Madar, R.T.; Eshkoli, T. Knowledge of women during the third trimester of pregnancy regarding pelvic floor disorders. Int. Urogynecol. J. 2022, 33, 3407–3414. [Google Scholar] [CrossRef]
- Kammers, I.; Sperandio, F.; Sacomori, C.; Moreira, G.; Cardoso, F. Knowledge and perceptions of pregnant women about the reproductive system: A qualitative study. Man. Ther. Posturol. Rehabil. J. 2021, 19, 1–7. [Google Scholar] [CrossRef]
- Shah, A.D.; Massagli, M.P.; Kohli, N.; Rajan, S.S.; Braaten, K.P.; Hoyte, L. A reliable, valid instrument to assess patient knowledge about urinary incontinence and pelvic organ prolapse. Int. Urogynecol. J. Pelvic Floor. Dysfunct. 2008, 19, 1283–1289. [Google Scholar] [CrossRef]
- Barber, M.D.; Walters, M.D.; Bump, R.C. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am. J. Obs. Gynecol. 2005, 193, 103–113. [Google Scholar] [CrossRef]
- Yuan, H.; Williams, B.A. Knowledge of urinary incontinence among Chinese community nurses and community-dwelling older people. Health Soc. Care Community 2010, 18, 82–90. [Google Scholar] [CrossRef]
- Falvey, L.; Salameh, F.; O’Sullivan, O.E.; O’Reilly, B.A. What Does Your Pelvic Floor Do for You? Knowledge of the Pelvic Floor in Female University Students: A Cross-sectional Study. Female Pelvic Med. Reconstr. Surg. 2021, 27, e457–e464. [Google Scholar] [CrossRef] [PubMed]
- Neels, H.; Wyndaele, J.J.; Tjalma, W.A.; De Wachter, S.; Wyndaele, M.; Vermandel, A. Knowledge of the pelvic floor in nulliparous women. J. Phys. Ther. Sci. 2016, 28, 1524–1533. [Google Scholar] [CrossRef] [PubMed]
- de Freitas, L.M.; Bo, K.; Fernandes, A.; Uechi, N.; Duarte, T.B.; Ferreira, C.H.J. Pelvic floor muscle knowledge and relationship with muscle strength in Brazilian women: A cross-sectional study. Int. Urogynecol. J. 2019, 30, 1903–1909. [Google Scholar] [CrossRef]
- Queiruga, M.B.; Delgado-Morell, A.; Garcia, M.P.; Girona, S.C.; Saladich, I.G.; Roda, O.P. What do female university students know about pelvic floor disorders? A cross-sectional survey. Int. Urogynecol. J. 2022, 33, 659–664. [Google Scholar] [CrossRef]
- Villadsen, S.F.; Hadi, H.; Ismail, I.; Osborne, R.H.; Ekstrom, C.T.; Kayser, L. ehealth literacy and health literacy among immigrants and their descendants compared with women of Danish origin: A cross-sectional study using a multidimensional approach among pregnant women. BMJ Open 2020, 10, e037076. [Google Scholar] [CrossRef]
- Pizzoferrato, A.C.; Deparis, J.; Fritel, X.; Rousseau, M.; Blanchard, V. Impact of educational workshops to increase awareness of pelvic floor dysfunction and integrate preventive lifestyle habits. Int. J. Gynaecol. Obs. 2024, 164, 596–604. [Google Scholar] [CrossRef]
- DeLancey, J.O.L.; Masteling, M.; Pipitone, F.; LaCross, J.; Mastrovito, S.; Ashton-Miller, J.A. Pelvic floor injury during vaginal birth is life-altering and preventable: What can we do about it? Am. J. Obs. Gynecol. 2024, 230, 279–294.e2. [Google Scholar] [CrossRef]
- Hübner, M.; Meschede, J.; Reister, F.; Deniz, M. Aufklärung über Schwangerschafts- und geburtsbedingte Veränderungen des weiblichen Beckenbodens aus urogynäkologischer Sicht. Gynäkologie 2023, 56, 6–13. [Google Scholar] [CrossRef]
- Deliktas, A.; Kukulu, K. Pregnant Women in Turkey Experience Severe Fear of Childbirth: A Systematic Review and Meta-Analysis. J. Transcult. Nurs. 2019, 30, 501–511. [Google Scholar] [CrossRef]
- What Are Midwifes Do. Available online: https://www.pregnancybirthbaby.org.au/the-role-of-your-midwife (accessed on 2 January 2025).
- Antenatal Classes. Available online: https://www.nhs.uk/pregnancy/labour-and-birth/preparing-for-the-birth/antenatal-classes/ (accessed on 5 January 2025).
- Demirci, A.D.; Kabukcuglu, K.; Haugan, G.; Aune, I. “I want a birth without interventions”: Women’s childbirth experiences from Turkey. Women Birth 2019, 32, E515–E522. [Google Scholar] [CrossRef]
- Ricchi, A.; La Corte, S.; Molinazzi, M.T.; Messina, M.P.; Banchelli, F.; Neri, I. Study of childbirth education classes and evaluation of their effectiveness. Clin. Ter. 2020, 171, E78–E86. [Google Scholar]
- Avignon, V.; Gaucher, L.; Baud, D.; Legardeur, H.; Dupont, C.; Horsch, A. What do mothers think about their antenatal classes? A mixed-method study in Switzerland. BMC Pregnancy Childb. 2023, 23, 741. [Google Scholar] [CrossRef]
- Butterfield, Y.C.; O’Connell, B.; Phillips, D. Peripartum urinary incontinence: A study of midwives’ knowledge and practices. Women Birth 2007, 20, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Terry, R.; Jarvie, R.; Hay-Smith, J.; Salmon, V.; Pearson, M.; Boddy, K.; MacArthur, C.; Dean, S. “Are you doing your pelvic floor?” An ethnographic exploration of the interaction between women and midwives about pelvic floor muscle exercises (PFME) during pregnancy. Midwifery 2020, 83, 102647. [Google Scholar] [CrossRef]
- MacArthur, C.; Wilson, D.; Herbison, P.; Lancashire, R.J.; Hagen, S.; Toozs-Hobson, P.; Dean, N.; Glazener, C.; ProLong study group. Faecal incontinence persisting after childbirth: A 12 year longitudinal study. BJOG 2013, 120, 169–179. [Google Scholar] [CrossRef]
- Day, M.R.; Patricia, L.W.; Loughran, S.; O’Sullivan, E. Community-dwelling women’s knowledge of urinary incontinence. Br. J. Community Nurs. 2014, 19, 534–538. [Google Scholar] [CrossRef]
- Cardoso, A.M.B.; Lima, C.; Ferreira, C.W.S. Prevalence of urinary incontinence in high-impact sports athletes and their association with knowledge, attitude and practice about this dysfunction. Eur. J. Sport. Sci. 2018, 18, 1405–1412. [Google Scholar] [CrossRef]
- Ayerle, G.; Mattern, E. Priority topics for research by midwives: An analysis of focus groups with pregnant women, mothers and midwives. GMS Z. Für Hebammenwissenschaft 2017, 4, 1–19. [Google Scholar]
- Nawabi, F.; Krebs, F.; Vennedey, V.; Shukri, A.; Lorenz, L.; Stock, S. Health Literacy in Pregnant Women: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 3847. [Google Scholar] [CrossRef]
- Willburger, B.; Chen, Z.; Mansfield, K.J. Investigation of the quality and health literacy demand of online information on pelvic floor exercises to reduce stress urinary incontinence. Aust. N. Z. J. Obs. Gynaecol. 2024, 64, 542–547. [Google Scholar] [CrossRef]
- Bo, K.; Sherburn, M. Evaluation of female pelvic-floor muscle function and strength. Phys. Ther. 2005, 85, 269–282. [Google Scholar] [CrossRef] [PubMed]
- Laycock, J.; Jerwood, D. Pelvic Floor Muscle Assessment: The PERFECT Scheme. Physiotherapy 2001, 87, 631–641. [Google Scholar]
- NICE Guideline [NG210]. Available online: https://www.nice.org.uk/guidance/ng210 (accessed on 2 January 2025).
- Okeahialam, N.A.; Oldfield, M.; Stewart, E.; Bonfield, C.; Carboni, C. Pelvic floor muscle training: A practical guide. Bmj 2022, 378, e070186. [Google Scholar] [CrossRef]
- Souza, J.P.; Day, L.T.; Rezende-Gomes, A.C.; Zhang, J.; Mori, R.; Baguiya, A.; Jayaratne, K.; Osoti, A.; Vogel, J.P.; Campbell, O.; et al. A global analysis of the determinants of maternal health and transitions in maternal mortality. Lancet Glob. Health 2024, 12, e306–e316. [Google Scholar] [CrossRef]
- Berufspolitik. Available online: https://hebammenverband.de/berufspolitik#positionen (accessed on 10 January 2025).
- Yelland, J.; Riggs, E.; Small, R.; Brown, S. Maternity services are not meeting the needs of immigrant women of non-English speaking background: Results of two consecutive Australian population based studies. Midwifery 2015, 31, 664–670. [Google Scholar] [CrossRef]
- Befristete Übergangsvereinbarung zur Anpassung der Vergütung für Leistungen der Hebammenhilfe nach § 134a Abs. 1 SGB V vom 7 February 2024. Available online: https://www.gkv-spitzenverband.de/media/dokumente/krankenversicherung_1/ambulante_leistungen/hebammen/aktuelle_dokumente/24-02-07_Uebergangsvereinbarung_Verguetungsanpassung_Hebammen.pdf (accessed on 2 January 2025).
- AWMF-Registernummer 015-091-Harninkontinenz der Frau. Available online: https://www.awmf.org/service/awmf-aktuell/harninkontinenz-der-frau. (accessed on 2 January 2025).
- The State of the World’s Children. Available online: https://www.unicef.org/media/165156/file/SOWC-2024-full-report-EN.pdf (accessed on 2 January 2025).
- Uzan, L.M.; Brust, M.; Molenaar, J.M.; Leistra, E.; Boor, K.; Jong, J.C.K.D. A cross-sectional analysis of factors associated with the teachable moment concept and health behaviors during pregnancy. BMC Pregnancy Childbirth 2024, 24, 147. [Google Scholar] [CrossRef]
- Rockliffe, L.; Peters, S.; Heazell, A.E.P.; Smith, D.M. Understanding pregnancy as a teachable moment for behaviour change: A comparison of the COM-B and teachable moments models. Health Psychol. Behav. Med. 2022, 10, 41–59. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).