Towards the Identification of Patients’ Needs for Promoting Robotics and Allied Digital Technologies in Rehabilitation: A Systematic Review
Abstract
1. Introduction
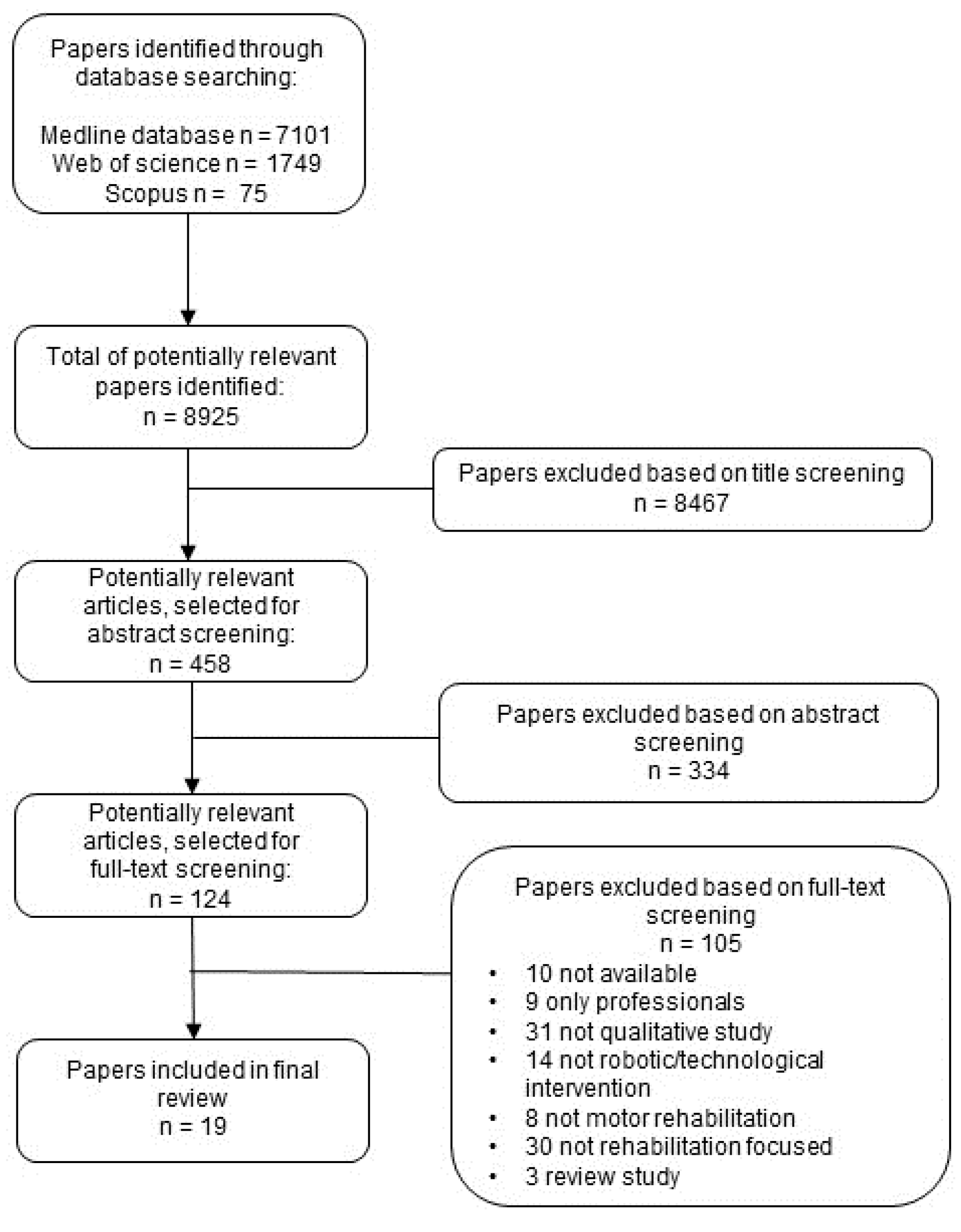
2. Materials and Methods
2.1. Study Design
2.2. Selection Criteria
2.3. Screening Process
2.4. Data Extraction and Synthesis
- source of data—title, authors, year of publication, DOI;
- sample characteristics—number of participants, diagnosis, target area of rehabilitation;
- type of robotic device/technology used;
- method of data collection and analysis employed;
- use of the ICF framework.
3. Results
- need for professional supervision [50];
| Study | Aim(s) | Sample | Condition and Target Area of Rehabilitation | Robotic Device | Method of Data Collection and Analysis | Use of the ICF Framework |
|---|---|---|---|---|---|---|
| Eicher et al., 2019 [19]; Germany | To identify differences regarding usability, acceptability, and barriers of usage of a robot- supported gait rehabilitation system between a younger and older group of patients with gait impairments | 13 patients | Stroke/brain hemorrhage, hemiplegia, other (e.g., accidents, falls, not specified); gait rehabilitation | Hybrid Assistive Limb exoskeleton | Structured interviews; qualitative content analysis by Mayring (2010) [58] | no |
| Sivan et al., 2016 [20]; UK | To evaluate the ICF as a framework to ensure that key aspects of user feedback are identified in the design and testing stages of development of a home-based upper limb rehabilitation system | 17 patients and 7 physiotherapists and occupational therapists | Stroke; upper limb rehabilitation | Not defined | Face-to-face semi-structured interviews; analysis based on the updated International Classification of Functioning, Disability and Health (ICF) linking rules and core set categories | only for the analysis |
| Ates et al., 2014 [21]; Three EU countries (unspecified) | To report on the technical challenges presented by the use of SPO and the feedback from therapists and patients | 24 patients; no information about the therapists | Stroke; hand impairment | SCRIPT Passive Orthosis | Clinical observation and descriptive summary into themes | no |
| Beveridge et al., 2015 [22]; Canada | To explore the experiences and perspectives of parents whose young, ambulatory children with CP were undergoing Lokomat gait training, and consider how parents’ values about walking influenced therapy decisions for their children | 5 mothers and 1 father of 5 children | Cerebral palsy; walking rehabilitation | Lokomat | Individual, semi-structured, face-to-face interviews; followed the Dierckx de Casterle approach to analysis of qualitative data: the Qualitative Analysis Guide of Leuven (QUAGOL) | no |
| Bezmez and Yardimci, 2016 [23]; Turkey | To explore the role of a robotic gait training device and its role in rehabilitation in Turkey | 42 participants (7 doctors, 2 nurses, 2 physiotherapists, 2 non-medical personnel, 20 in-patients, and 9 former patients) | Traumatic injury or illnesses; bodily disability and inability to walk | Lokomat | Individual, semi-structured interviews; no information provided on the method of analysis | no |
| Cahill et al., 2018 [24]; Ireland | To gain an understanding of the experience of using a RWD within a gym-based setting from the perspective of non-ambulatory individuals with SCI | 5 patients | Spinal cord injury; walking rehabilitation | Ekso™ | In-depth semi-structured interviews; thematic analysis | no |
| Danzl et al., 2013 [25]; USA | To investigate the feasibility of combining tDCS into the LE motor cortex with novel locomotor training to facilitate gait in subjects with chronic stroke and low ambulatory status; to obtain insight from participants and their caregivers to inform future trial design | 8 patients | Stroke; lower limb (gait) rehabilitation | Robotic gait orthosis | Semi-structured interviews; inductive thematic analysis | no |
| Elnady et al., 2018 [26]; Canada | To describe users’ perceptions about existing wearable robotic devices for the upper extremity; identify if there is a need to develop new devices for the upper extremity and the desired features; and to explore obstacles that would influence the utilization of these new devices | 8 people with stroke; 8 therapists: 4 physiotherapists, 2 occupational therapists; 2 rehabilitation assistants | Stroke; upper limb rehabilitation | Wearable Robotic Devices for the upper extremity | Focus groups; thematic analysis | no |
| Gilbert et al., 2018 [27]; UK | To determine whether or not the MUJO System was acceptable to patients with shoulder dysfunction and their rehabilitation professionals | 10 patients and 7 physiotherapists | Shoulder instability (n = 6) and rotator cuff-related pain (n = 4); rehabilitation of the rotator cuff muscles (bi-articular muscles or multiple axial joints) | MUJO System | Semi-structured interviews; Directed Content Analysis was undertaken to organize the qualitative data according to the four constructs of Normalisation Process Theory (NPT) | no |
| Heinemann et al., 2020 [28]; USA | To describe appraisals of robotic exoskeletons for locomotion by potential users with spinal cord injuries, their perceptions of device benefits and limitations, and recommendations for manufacturers and therapists regarding device use | 35 patients | Spinal cord injuries; gait rehabilitation | Robotic exoskeletons (Ekso Indego, ReWalk) | Focus groups; thematic analysis | no |
| Hughes et al., 2011 [29]; UK | To understand the stroke participants’ experiences of using the novel combination of a robotic arm and iterative learning control system, and to gain greater insight into how systems might be improved in the future | 5 patients | Stroke; upper limb rehabilitation | Robotic workstation | Structured and semi-structured interview. Two types of data were collected: comments were recorded during the time when participants were receiving the intervention and immediately following the clinical study, an interview-based question set was used; content analysis | no |
| Kumar and Phillips, 2013 [30]; UK | To explore the views, experiences, benefits, and difficulties that users of one specific type of PMAS perceive, and to determine which areas of daily life they are used in | 13 patients | Neuromuscular conditions; upper limb rehabilitation | Powered mobile arm supports | Semi-structured interviews; thematic analysis | no |
| Lajeunesse et al., 2018 [31]; Canada | To present the perspectives of individuals with ASIA C or D incomplete SCI concerning the usability of lower limb exoskeletons to R&D engineers and clinicians working in motor rehabilitation | 13 patients | Incomplete spinal cord injury; lower limb rehabilitation | ReWalk exoskeleton | Individual, semi-structured interviews; inductive thematic analysis | no |
| Manns et al., 2019 [32]; Canada | To explore the expectations and experiences of persons with spinal cord injury through training with the ReWalk exoskeleton | 11 patients | Traumatic spinal cord injury; standing and walking training | ReWalk exoskeleton | Semi-structured interviews; thematic analysis | no |
| Nasr et al., 2015 [33]; UK, Italy and Netherlands | To examine stroke survivors’ experiences of living with stroke and with technology in order to provide technology developers with insight into values, thoughts, and feelings of the potential users of a to-be-designed robotic technology for home-based rehabilitation of the hand and wrist | 10 patients and 8 caregivers | Stroke; upper limb rehabilitation | Not defined | Application of qualitative methods such as in-depth interviews as well as using diaries and photography activities; thematic analysis | no |
| O’ Brien Cherry et al., 2017 [34]; USA | To determine participants’ general impressions about the benefits and barriers of using RT devices for in-home rehabilitation | 10 veterans | Stroke; upper or lower limb impairments | Hand Mentor™ and Foot Mentor™ devices | Direct observations and semi-structured interviews; inductive thematic analysis | no |
| Phelan et al., 2015 [35]; Canada | To investigate the expectations and experiences of children with CP in relation to robotic gait training using the Lokomat Pro | 5 children and their parents (3 mothers and 2 fathers) | Cerebral palsy; gait rehabilitation | Lokomat Pro | Observations during sessions, semi-structured interviews with parents and use of a customizable “toolbox” of age-appropriate child-friendly techniques; thematic analysis | no |
| Sweeney et al., 2020 [36]; UK | To understand user perceptions in order to explain low uptake of upper limb rehabilitation interventions after stroke in clinical practice within the National Health Service (NHS Scotland) | 8 patients | Stroke; upper limb rehabilitation | Not defined | Semi-structured interviews; thematic analysis | no |
| Tedesco Triccas et al., 2018 [37]; UK | To explore views and experiences of people with subacute and chronic stroke that had previously taken part in a randomized controlled trial involving tDCS and RT for their impaired upper limb | 21 patients | Stroke; upper limb rehabilitation | Armeo Spring | Structured and semi-structured interviews involving open questions; thematic analysis | no |
| Thomassen et al., 2019 [38]; USA | To generate new knowledge regarding user experiences of standing and walking with Ekso | 3 patients | Spinal cord injury (due to traumatic and non-traumatic reasons); standing and walking training | Ekso™ | In-depth interviews in a phenomenological tradition; systematic inductive content analyses | no |
| Shore et al., 2022 [39]; Ireland | To explore insights expressed by a cohort of older adults related to their life experience, their experiences using or assisting someone with assistive devices, and their perceptions of robots and robotic assistive devices | 24 patients; no information about the therapists | Stroke; lower limb rehabilitation | Assistive devices | Structured interviews | no |
| McDonald et al., 2022 [40]; Ireland | To explore the usability and acceptance of RAGT in an acute hospital setting, and to examine users’ perceptions of two different modes of robotic assistance provided during rehabilitation | 10 patients; no information about the therapists | Stroke; gait training | Ekso™ | Semi-structured interviews of end-user perspectives and two 10-point Likert scales rating | no |
| Lebrasseur B.Erg et al., 2021 [41]; Canada | To evaluate the usability of actuated arm support | 9 patients; no information about the therapists | Multiple sclerosis, spinal muscular atrophy, muscular dystrophy; upper limb rehabilitation | Gowing power-assisted arm support | Quebec User Evaluation of Satisfaction with assistive Technology (QUEST) and semi-structured interviews | no |
| Basla et al., 2022 [42]; Switzerland | To investigate end-user perspectives and the adoption of an exosuit in domestic and community settings | 7 patients; no information about the therapists | Multiple sclerosis, spinal muscle atrophy, spastic paresis, Bethlem myopathy, cauda equina syndrome; walking rehabilitation | Myosuit | SUS and QUEST and one personalized questionnaire, semi-structured interview | no |
| Hampshire et al., 2022 [43]; UK | To gather users’ and caregivers’ perspectives on the assistive device | 6 patients and 2 caregivers | Stroke, spinal cord injury, hereditary spastic paraparesis; walking rehabilitation | Assistive devices | Semi-structured interview | no |
| Louie et al., 2022 [44]; Canada | To explore the experience and acceptability of an exoskeleton-based physiotherapy program for non-ambulatory patients from the perspective of patients and therapists | 14 patients; 6 physiotherapists | Stroke; gait training | Ekso™ | Semi-structured interviews and thematic analysis | no |
| Bauer et al., 2021 [45]; Switzerland | To assess the usability of a prototype assistive therapy chair (T-Chair) that induces exercise stimuli to improve trunk control and standing and walking early after stroke in a rehabilitation setting | 15 patients; 11 physiotherapists | Stroke | T-chair device | Focus groups; customized questionnaire | no |
| Charbonneau et al., 2021 [46]; Canada | To increase our understanding of SCI patient experience using a robotic exoskeleton in the acute post-injury period | 9 patients | Spinal cord injury | Ekso™ | Semi-structured interviews | no |
| Nieboer et al., 2021 [47]; Netherlands | To assess attitudes towards “Stappy” in people after stroke to practice walking performance independently at home | 17 patients | Stroke | Stappy (sensor-feedback device) | Semi-structured interviews | no |
| Webber et al., 2022 [48]; USA | To explore patient perspectives on the use of a Mioelectric elbow orthosis (MEO) following surgical treatment of a traumatic brachial plexus injuries (BPI) | 8 patients | Traumatic brachial plexus injuries | Mioelectric elbow orthosis | Focus groups; semi-structured interviews | no |
| Kobbelgaard et al., 2021 [49]; Denmark | Identify users’ needs and preferences for the design of an arm exoskeleton | 9 patients | Tetraplegia | EXOTIC arm exoskeleton | Semi-structured interviews | no |
| Kerr et al., 2023 [50]; UK | To assess the feasibility of a technology-enriched rehabilitation gym (TERG) approach and gather preliminary evidence of its effect on future research | 26 patients | Stroke | TERG (e.g., virtual reality treadmills, power-assisted equipment, balance trainers, and upper limb training systems) | Semi-structured interviews | no |
| Herrera-Valenzuela et al., 2023 [51]; Spain | To determine a comprehensive set of requirements, perceptions, and expectations that people with spinal cord injury (SCI) and the clinicians in charge of their rehabilitation have regarding the use of wearable robots (WR) for gait rehabilitation | 15 patients; 10 clinicians (5 physical medicine and rehabilitation physicians and 5 physiotherapists) | Spinal cord injury | Lower limb wearable exoskeletons | Semi-structured interviews | no |
| Chang et al., 2023 [52]; Taiwan | To develop a novel smart somatosensory wearable assistive device (called SSWAD), combined with sEMG and exergame software and hardware technology for rehabilitating the lower limb muscles of the older adult | 25 patients | Elderly frail | Smart Somatosensory Wearable Assistive Device (SSWAD) | Semi-structured interview and SUS questionnaire | no |
| Forbrigger et al., 2023 [53]; Canada | To investigate the needs of stroke survivors and therapists, and how they may contrast, for the design of robots for at-home post stroke rehabilitation therapy | 10 patients; 6 therapists (5 physiotherapists and 1 occupation therapist) | Stroke | Upper limb robotic devices (FitMi, MusicGlove) | Semi-structured interview | only for the analysis |
| Bhattacharjya et al., 2023 [54]; USA | To evaluate the participants’ approach and nature of engagement with the mRehab system and corresponding changes in outcome measures, and to identify the self-reported factors that influenced the use of the mRehab system at home by community-dwelling individuals with chronic stroke | 6 patients | Stroke | mobile Rehab | Semi-structured interview | no |
| Spits et al., 2022 [55]; Netherland | To investigate stroke survivors’ experiences regarding training using the hoMEcare aRm rehabiLItatioN (MERLIN) system, an assistive device and telecare platform | 11 patients | Stroke | MERLIN system | Semi-structured interview | only for the analysis |
| Lee et al., 2022 [56]; not specified | To present detailed design specifications and exploratory evaluations of an AI and robotic coach capable of monitoring and guiding post-stroke survivors in self-paced physical rehabilitation therapy | 5 patients; 4 therapists (3 occupational therapists, 1 physiotherapist) | Stroke | Robotic coaches | Semi-structured interview | no |
| Langerak et al., 2023 [57]; Netherlands | To define the user requirements for home-based upper extremity rehabilitation using wearable motion sensors for subacute stroke patients | 17 patients; 21 therapists | Stroke | Wearable motion sensors | Focus groups and semi-structured interview | no |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ICF | International Classification of Functioning, Disability, and Health |
| Fit4MedRob | Fit for Medical Robotics |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PICO | Population, Intervention, Comparison, and Outcome |
| MeSH | Medical Subject Headings |
| DOI | Digital Object Identifier |
| EU | European Union |
| SUS | System Usability Scale |
| QUEST | Quebec User Evaluation of Satisfaction with Assistive Technology |
| tDCS | Transcranial Direct Current Stimulation |
References
- Prange, G.B.; Jannink, M.J.A.; Groothuis-Oudshoorn, C.G.M.; Hermens, H.J.; IJzerman, M.J. Systematic Review of the Effect of Robot-Aided Therapy on Recovery of the Hemiparetic Arm after Stroke. J. Rehabil. Res. Dev. 2006, 43, 171. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Tyson, S.; Weightman, A. Professionals’ Views and Experiences of Using Rehabilitation Robotics with Stroke Survivors: A Mixed Methods Survey. Front. Med. Technol. 2021, 3, 780090. [Google Scholar] [CrossRef]
- Pavan, A.; Fasano, A.; Cortellini, L.; Lattanzi, S.; Papadopoulou, D.; Insalaco, S.; Germanotta, M.; Aprile, I. Implementation of a Robot-Mediated Upper Limb Rehabilitation Protocol for a Customized Treatment after Stroke: A Retrospective Analysis. NeuroRehabilitation 2024, 54, 411–420. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. IFC: International Classification of Functioning, Disability and Health; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Paltamaa, J.; van Lingen, E.; Haumer, C.; Kidritsch, A.; Aerts, I.; Mutanen, L. Specific ICF Training Is Needed in Clinical Practice: ICF Framework Education Is Not Enough. Front. Rehabil. Sci. 2024, 5, 1351564. [Google Scholar] [CrossRef]
- Cieza, A.; Ewert, T.; Ustün, T.B.; Chatterji, S.; Kostanjsek, N.; Stucki, G. Development of ICF Core Sets for Patients with Chronic Conditions. J. Rehabil. Med. 2004, 44, 9–11. [Google Scholar] [CrossRef]
- Ptyushkin, P.; Vidmar, G.; Burger, H.; Marinček, C.; Escorpizo, R. The International Classification of Functioning, Disability and Health (ICF) in Vocational Rehabilitation and Disability Assessment in Slovenia: State of Law and Users’ Perspective. Disabil. Rehabil. 2011, 33, 130–136. [Google Scholar] [CrossRef]
- Calabrò, R.S.; Sorrentino, G.; Cassio, A.; Mazzoli, D.; Andrenelli, E.; Bizzarini, E.; Campanini, I.; Carmignano, S.M.; Cerulli, S.; Chisari, C.; et al. Robotic-Assisted Gait Rehabilitation Following Stroke: A Systematic Review of Current Guidelines and Practical Clinical Recommendations. Eur. J. Phys. Rehabil. Med. 2021, 57, 460–471. [Google Scholar] [CrossRef]
- Rauch, A.; Cieza, A.; Stucki, G. How to Apply the International Classification of Functioning, Disability and Health (ICF) for Rehabilitation Management in Clinical Practice. Eur. J. Phys. Rehabil. Med. 2008, 44, 329–342. [Google Scholar]
- Stucki, G.; Grimby, G. Applying the ICF in Medicine. J. Rehabil. Med. 2004, 44, 5–6. [Google Scholar] [CrossRef]
- Harty, M.; Griesel, M.; van der Merwe, A. The ICF as a Common Language for Rehabilitation Goal-Setting: Comparing Client and Professional Priorities. Health Qual. Life Outcomes 2011, 9, 87. [Google Scholar] [CrossRef]
- Cieza, A.; Stucki, G. The International Classification of Functioning Disability and Health: Its Development Process and Content Validity. Eur. J. Phys. Rehabil. Med. 2008, 44, 303–313. [Google Scholar] [PubMed]
- Cieza, A.; Kostansjek, N. The International Classification of Functioning, Disability and Health: The First 20 Years. Dev. Med. Child Neurol. 2021, 63, 363. [Google Scholar] [CrossRef] [PubMed]
- Laparidou, D.; Curtis, F.; Akanuwe, J.; Goher, K.; Niroshan Siriwardena, A.; Kucukyilmaz, A. Patient, Carer, and Staff Perceptions of Robotics in Motor Rehabilitation: A Systematic Review and Qualitative Meta-Synthesis. J. Neuroeng. Rehabil. 2021, 18, 181. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Garner, P.; Hopewell, S.; Chandler, J.; MacLehose, H.; Schünemann, H.J.; Akl, E.A.; Beyene, J.; Chang, S.; Churchill, R.; Dearness, K.; et al. When and How to Update Systematic Reviews: Consensus and Checklist. BMJ 2016, 354, i3507. [Google Scholar] [CrossRef]
- Amir-Behghadami, M.; Janati, A. Population, Intervention, Comparison, Outcomes and Study (PICOS) Design as a Framework to Formulate Eligibility Criteria in Systematic Reviews. Emerg. Med. J. 2020, 37, 387. [Google Scholar] [CrossRef]
- Popay, J.; Roberts, H.M.; Sowden, A.; Petticrew, M.; Arai, L.; Rodgers, M.; Britten, N. Guidance on the Conduct of Narrative Synthesis in Sytematic Reviews; Institute for Health Research: London, UK, 2006. [Google Scholar]
- Eicher, C.; Haesner, M.; Spranger, M.; Kuzmicheva, O.; Gräser, A.; Steinhagen-Thiessen, E. Usability and Acceptability by a Younger and Older User Group Regarding a Mobile Robot-Supported Gait Rehabilitation System. Assist. Technol. 2019, 31, 25–33. [Google Scholar] [CrossRef]
- Sivan, M.; Gallagher, J.; Holt, R.; Weightman, A.; O’Connor, R.; Levesley, M. Employing the International Classification of Functioning, Disability and Health Framework to Capture User Feedback in the Design and Testing Stage of Development of Home-Based Arm Rehabilitation Technology. Assist. Technol. 2016, 28, 175–182. [Google Scholar] [CrossRef]
- Ates, S.; Leon, B.; Basteris, A.; Nijenhuis, S.; Nasr, N.; Sale, P.; Cesario, A.; Amirabdollahian, F.; Stienen, A.H.A. Technical Evaluation of and Clinical Experiences with the SCRIPT Passive Wrist and Hand Orthosis. In Proceedings of the 2014 7th International Conference on Human System Interactions (HSI), Lisbon, Portugal, 16–18 June 2014; pp. 188–193. [Google Scholar]
- Beveridge, B.; Feltracco, D.; Struyf, J.; Strauss, E.; Dang, S.; Phelan, S.; Wright, F.V.; Gibson, B.E. “You Gotta Try It All”: Parents’ Experiences with Robotic Gait Training for Their Children with Cerebral Palsy. Phys. Occup. Ther. Pediatr. 2015, 35, 327–341. [Google Scholar] [CrossRef]
- Bezmez, D.; Yardımcı, S. Rehabilitation Technology and the Reproduction of Bodily Normality: A Critical Analysis of Robotic Gait Training in Turkey. Scand. J. Disabil. Res. 2016, 18, 343–353. [Google Scholar] [CrossRef]
- Cahill, A.; Ginley, O.M.; Bertrand, C.; Lennon, O. Gym-Based Exoskeleton Walking: A Preliminary Exploration of Non-Ambulatory End-User Perspectives. Disabil. Health J. 2018, 11, 478–485. [Google Scholar] [CrossRef] [PubMed]
- Danzl, M.M.; Chelette, K.C.; Lee, K.; Lykins, D.; Sawaki, L. Brain Stimulation Paired with Novel Locomotor Training with Robotic Gait Orthosis in Chronic Stroke: A Feasibility Study. NeuroRehabilitation 2013, 33, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Elnady, A.; Mortenson, W.B.; Menon, C. Perceptions of Existing Wearable Robotic Devices for Upper Extremity and Suggestions for Their Development: Findings from Therapists and People with Stroke. JMIR Rehabil. Assist. Technol. 2018, 5, e12. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, A.W.; Hauptmannova, I.; Jaggi, A. The Use of Assistive Technology in Shoulder Exercise Rehabilitation—A Qualitative Study of Acceptability within a Pilot Project. BMC Musculoskelet. Disord. 2018, 19, 133. [Google Scholar] [CrossRef]
- Heinemann, A.W.; Kinnett-Hopkins, D.; Mummidisetty, C.K.; Bond, R.A.; Ehrlich-Jones, L.; Furbish, C.; Field-Fote, E.; Jayaraman, A. Appraisals of Robotic Locomotor Exoskeletons for Gait: Focus Group Insights from Potential Users with Spinal Cord Injuries. Disabil. Rehabil. Assist. Technol. 2020, 15, 762–772. [Google Scholar] [CrossRef]
- Hughes, A.-M.; Burridge, J.; Freeman, C.T.; Donnovan-Hall, M.; Chappell, P.H.; Lewin, P.L.; Rogers, E.; Dibb, B. Stroke Participants’ Perceptions of Robotic and Electrical Stimulation Therapy: A New Approach. Disabil. Rehabil. Assist. Technol. 2011, 6, 130–138. [Google Scholar] [CrossRef]
- Kumar, A.; Phillips, M.F. Use of Powered Mobile Arm Supports by People with Neuromuscular Conditions. J. Rehabil. Res. Dev. 2013, 50, 61–70. [Google Scholar] [CrossRef]
- Lajeunesse, V.; Routhier, F.; Vincent, C.; Lettre, J.; Michaud, F. Perspectives of Individuals with Incomplete Spinal Cord Injury Concerning the Usability of Lower Limb Exoskeletons: An Exploratory Study. Technol. Disabil. 2018, 30, 63–76. [Google Scholar] [CrossRef]
- Manns, P.J.; Hurd, C.; Yang, J.F. Perspectives of People with Spinal Cord Injury Learning to Walk Using a Powered Exoskeleton. J. Neuroeng. Rehabil. 2019, 16, 94. [Google Scholar] [CrossRef]
- Nasr, N.; Leon, B.; Mountain, G.; Nijenhuis, S.M.; Prange, G.; Sale, P.; Amirabdollahian, F. The Experience of Living with Stroke and Using Technology: Opportunities to Engage and Co-Design with End Users. Disabil. Rehabil. Assist. Technol. 2016, 11, 653–660. [Google Scholar] [CrossRef]
- Cherry, C.O.; Chumbler, N.R.; Richards, K.; Huff, A.; Wu, D.; Tilghman, L.M.; Butler, A. Expanding Stroke Telerehabilitation Services to Rural Veterans: A Qualitative Study on Patient Experiences Using the Robotic Stroke Therapy Delivery and Monitoring System Program. Disabil. Rehabil. Assist. Technol. 2017, 12, 21–27. [Google Scholar] [CrossRef]
- Phelan, S.K.; Gibson, B.E.; Wright, F.V. What Is It like to Walk with the Help of a Robot? Children’s Perspectives on Robotic Gait Training Technology. Disabil. Rehabil. 2015, 37, 2272–2281. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, G.; Barber, M.; Kerr, A. Exploration of Barriers and Enablers for Evidence-Based Interventions for Upper Limb Rehabilitation Following a Stroke: Use of Constraint Induced Movement Therapy and Robot Assisted Therapy in NHS Scotland. Br. J. Occup. Ther. 2020, 83, 690–700. [Google Scholar] [CrossRef]
- Tedesco Triccas, L.; Burridge, J.H.; Hughes, A.M.; Meadmore, K.L.; Donovan-Hall, M.; Rothwell, J.C.; Verheyden, G. A Qualitative Study Exploring Views and Experiences of People with Stroke Undergoing Transcranial Direct Current Stimulation and Upper Limb Robot Therapy. Top. Stroke Rehabil. 2018, 25, 480–488. [Google Scholar] [CrossRef]
- Thomassen, G.-K.K.; Jørgensen, V.; Normann, B. “Back at the Same Level as Everyone Else”-User Perspectives on Walking with an Exoskeleton, a Qualitative Study. Spinal Cord Ser. Cases 2019, 5, 103. [Google Scholar] [CrossRef]
- Shore, L.; de Eyto, A.; O’Sullivan, L. Technology Acceptance and Perceptions of Robotic Assistive Devices by Older Adults—Implications for Exoskeleton Design. Disabil. Rehabil. Assist. Technol. 2022, 17, 782–790. [Google Scholar] [CrossRef]
- McDonald, C.; Fingleton, C.; Murphy, S.; Lennon, O. Stroke Survivor Perceptions of Using an Exoskeleton during Acute Gait Rehabilitation. Sci. Rep. 2022, 12, 14185. [Google Scholar]
- Lebrasseur, A.; Lettre, J.; Routhier, F.; Bouffard, J.; Archambault, P.S.; Campeau-Lecours, A. Evaluation of the Usability of an Actively Actuated Arm Support. Assist. Technol. 2021, 33, 271–277. [Google Scholar] [CrossRef]
- Basla, C.; Hungerbühler, I.; Meyer, J.T.; Wolf, P.; Riener, R.; Xiloyannis, M. Usability of an Exosuit in Domestic and Community Environments. J. NeuroEngineering Rehabil. 2022, 19, 131. [Google Scholar] [CrossRef]
- Hampshire, L.; Dehghani-Sanij, A.; O’Connor, R.J. Restorative Rehabilitation Robotics to Promote Function, Independence and Dignity: Users’ Perspectives on Clinical Applications. J. Med. Eng. Technol. 2022, 46, 527–535. [Google Scholar] [CrossRef]
- Louie, D.R.; Mortenson, W.B.; Lui, M.; Durocher, M.; Teasell, R.; Yao, J.; Eng, J.J. Patients’ and Therapists’ Experience and Perception of Exoskeleton-Based Physiotherapy during Subacute Stroke Rehabilitation: A Qualitative Analysis. Disabil. Rehabil. 2022, 44, 7390–7398. [Google Scholar] [CrossRef] [PubMed]
- Bauer, C.M.; Nast, I.; Scheermesser, M.; Kuster, R.P.; Textor, D.; Wenger, M.; Kool, J.; Baumgartner, D. A Novel Assistive Therapy Chair to Improve Trunk Control during Neurorehabilitation: Perceptions of Physical Therapists and Patients. Appl. Ergon. 2021, 94, 103390. [Google Scholar] [CrossRef] [PubMed]
- Charbonneau, R.; Loyola-Sanchez, A.; McIntosh, K.; MacKean, G.; Ho, C. Exoskeleton Use in Acute Rehabilitation Post Spinal Cord Injury: A Qualitative Study Exploring Patients’ Experiences. J. Spinal Cord Med. 2022, 45, 848–856. [Google Scholar] [CrossRef] [PubMed]
- Nieboer, M.; Jie, L.-J.; Willemse, L.; Peek, S.; Braun, S.; Wouters, E. Attitudes towards a Sensor-Feedback Technology in Gait Rehabilitation of Patients after Stroke. Disabil. Rehabil. Assist. Technol. 2023, 18, 889–895. [Google Scholar] [CrossRef]
- Webber, C.M.; Egginton, J.S.; Shin, A.Y.; Kaufman, K.R. Application of a Myoelectric Elbow Flexion Assist Orthosis in Adult Traumatic Brachial Plexus Injury: Patient Perspectives. Prosthet. Orthot. Int. 2021, 45, 526–531. [Google Scholar] [CrossRef]
- Kobbelgaard, F.V.; Kanstrup, A.M.; Struijk, L.N.S.A. Exploring User Requirements for an Exoskeleton Arm Insights from a User-Centered Study with People Living with Severe Paralysis. In Proceedings of the Human-Computer Interaction—INTERACT 2021, Bari, Italy, 30 August–3 September 2021; Ardito, C., Lanzilotti, R., Malizia, A., Petrie, H., Piccinno, A., Desolda, G., Inkpen, K., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 312–320. [Google Scholar]
- Kerr, A.; Keogh, M.; Slachetka, M.; Grealy, M.; Rowe, P. An Intensive Exercise Program Using a Technology-Enriched Rehabilitation Gym for the Recovery of Function in People with Chronic Stroke: Usability Study. JMIR Rehabil. Assist. Technol. 2023, 10, e46619. [Google Scholar] [CrossRef]
- Herrera-Valenzuela, D.; Díaz-Peña, L.; Redondo-Galán, C.; Arroyo, M.J.; Cascante-Gutiérrez, L.; Gil-Agudo, Á.; Moreno, J.C.; Del-Ama, A.J. A Qualitative Study to Elicit User Requirements for Lower Limb Wearable Exoskeletons for Gait Rehabilitation in Spinal Cord Injury. J. Neuroeng. Rehabil. 2023, 20, 138. [Google Scholar] [CrossRef]
- Chang, C.-H.; Lien, W.-C.; Chiu, T.-P.; Yang, T.-H.; Wei, C.-C.; Kuo, Y.-L.; Yeh, C.-H.; Liu, B.; Chen, P.-J.; Lin, Y.-C. A Novel Smart Somatosensory Wearable Assistive Device for Older Adults’ Home Rehabilitation during the COVID-19 Pandemic. Front. Public Health 2023, 11, 1026662. [Google Scholar] [CrossRef]
- Forbrigger, S.; DePaul, V.G.; Davies, T.C.; Morin, E.; Hashtrudi-Zaad, K. Home-Based Upper Limb Stroke Rehabilitation Mechatronics: Challenges and Opportunities. Biomed. Eng. Online 2023, 22, 67. [Google Scholar] [CrossRef]
- Bhattacharjya, S.; Linares, I.; Langan, J.; Xu, W.; Subryan, H.; Cavuoto, L.A. Engaging in a Home-Based Exercise Program: A Mixed-Methods Approach to Identify Motivators and Barriers for Individuals with Stroke. Assist. Technol. 2023, 35, 487–496. [Google Scholar] [CrossRef]
- Spits, A.H.; Rozevink, S.G.; Balk, G.A.; Hijmans, J.M.; van der Sluis, C.K. Stroke Survivors’ Experiences with Home-Based Telerehabilitation Using an Assistive Device to Improve Upper Limb Function: A Qualitative Study. Disabil. Rehabil. Assist. Technol. 2024, 19, 730–738. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.H.; Siewiorek, D.P.; Smailagic, A.; Bernardino, A.; Badia, S.B.I. Enabling AI and Robotic Coaches for Physical Rehabilitation Therapy: Iterative Design and Evaluation with Therapists and Post-Stroke Survivors. Int. J. Soc. Robot. 2024, 16, 1–22. [Google Scholar] [CrossRef]
- Langerak, A.J.; Regterschot, G.R.H.; Selles, R.W.; Meskers, C.G.M.; Evers, M.; Ribbers, G.M.; van Beijnum, B.J.F.; Bussmann, J.B.J. Requirements for Home-Based Upper Extremity Rehabilitation Using Wearable Motion Sensors for Stroke Patients: A User-Centred Approach. Disabil. Rehabil. Assist. Technol. 2024, 19, 1392–1404. [Google Scholar] [CrossRef] [PubMed]
- Mayring, P. Qualitative Inhaltsanalyse: Grundlagen Und Techniken; Beltz: Basel, Switzerland, 2010. [Google Scholar]
| S1 | robotic* OR robot* OR robotic therap* OR robot-assisted OR robot assisted OR exoskeleton* OR assistive robotic* OR walking robotic device* OR personal care robot* OR medical robot* OR assistive OR assistive automation OR wearable robot* OR orthotic* OR orthosis OR exoskeletal* OR exo OR end-effector OR haptic* OR robot regulation* | |
| S2 | rehab* OR intervention* OR treatment* OR therap* OR program* OR strateg* OR training OR physiotherap* OR physio-therap* OR “physiotherap*” OR “physical therap*” | |
| S3 | Qualitative research OR qualitative OR interview* OR focus group* OR ethno* OR phenomenolog* OR hermeneutic* OR grounded theory OR narrative analysis OR thematic analysis OR lived experience* OR life experience* | |
| S4 | (MH “Qualitative Research”) OR “Qualitative research” | |
| S5 | S3 OR S4 | |
| Searched | S1 AND S2 AND S5 | |
| Applied Filters | Published: 2021–2023 | |
| Language: English | ||
| Species: Humans | ||
| S1 | robotic* OR robot* OR robotic therap* OR robot-assisted OR robot assisted OR exoskeleton* OR assistive robotic* OR walking robotic device* OR personal care robot* OR medical robot* OR assistive OR assistive automation OR wearable robot* OR orthotic* OR orthosis OR exoskeletal* OR exo OR end-effector OR haptic* OR robot regulation* | |
| S2 | rehab* OR intervention* OR treatment* OR therap* OR program* OR strateg* OR training OR physiotherap* OR physio-therap* OR “physiotherap*” OR “physical therap*” | |
| S3 | Qualitative research OR qualitative OR interview* OR focus group* OR ethno* OR phenomenolog* OR hermeneutic* OR grounded theory OR narrative analysis OR thematic analysis OR lived experience* OR life experience* | |
| S4 | (“population group*” OR “patient* group*”) OR (men OR women OR patient* OR female OR male OR subjects) | |
| S5 | “animal models” OR animal | |
| Searched | S1 AND S2 AND S3 AND S4 AND NOT S5 | |
| Applied Filters | Published: 2021–2023 | |
| Language: English | ||
| S1 | robotic* OR robot* OR robotic therap* OR robot-assisted OR robot assisted OR exoskeleton* OR assistive robotic* OR walking robotic device* OR personal care robot* OR medical robot* OR assistive OR assistive automation OR wearable robot* OR orthotic* OR orthosis OR exoskeletal* OR exo OR end-effector OR haptic* OR robot regulation* | |
| S2 | rehab* OR intervention* OR treatment* OR therap* OR program* OR strateg* OR training OR physiotherap* OR physio-therap* OR “physiotherap*” OR “physical therap*” | |
| S3 | Qualitative research OR qualitative OR interview* OR focus group* OR ethno* OR phenomenolog* OR hermeneutic* OR grounded theory OR narrative analysis OR thematic analysis OR lived experience* OR life experience* | |
| S4 | (“population group*” OR “patient* group*”) OR (men OR women OR patient* OR female OR male OR subjects) | |
| S5 | “animal models” OR animal | |
| Searched | S1 AND S2 AND S3 AND (S4 NOT S5) | |
| Applied Filters | Published: 2021–2023 | |
| Language: English | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fasano, A.; Mauro, M.C.; Beani, E.; Nicora, G.; Germanotta, M.; Falchini, F.; Pavan, A.; Habib, V.; Quaglini, S.; Sgandurra, G.; et al. Towards the Identification of Patients’ Needs for Promoting Robotics and Allied Digital Technologies in Rehabilitation: A Systematic Review. Healthcare 2025, 13, 828. https://doi.org/10.3390/healthcare13070828
Fasano A, Mauro MC, Beani E, Nicora G, Germanotta M, Falchini F, Pavan A, Habib V, Quaglini S, Sgandurra G, et al. Towards the Identification of Patients’ Needs for Promoting Robotics and Allied Digital Technologies in Rehabilitation: A Systematic Review. Healthcare. 2025; 13(7):828. https://doi.org/10.3390/healthcare13070828
Chicago/Turabian StyleFasano, Alessio, Maria Cristina Mauro, Elena Beani, Giovanna Nicora, Marco Germanotta, Francesca Falchini, Arianna Pavan, Valeria Habib, Silvana Quaglini, Giuseppina Sgandurra, and et al. 2025. "Towards the Identification of Patients’ Needs for Promoting Robotics and Allied Digital Technologies in Rehabilitation: A Systematic Review" Healthcare 13, no. 7: 828. https://doi.org/10.3390/healthcare13070828
APA StyleFasano, A., Mauro, M. C., Beani, E., Nicora, G., Germanotta, M., Falchini, F., Pavan, A., Habib, V., Quaglini, S., Sgandurra, G., & Aprile, I. G. (2025). Towards the Identification of Patients’ Needs for Promoting Robotics and Allied Digital Technologies in Rehabilitation: A Systematic Review. Healthcare, 13(7), 828. https://doi.org/10.3390/healthcare13070828










