The Global Burden of Atopic Dermatitis in Elderly Populations: Trends, Disparities, and Future Projections
Abstract
1. Introduction
2. Materials and Methods
2.1. Overview and Data Collection
2.2. Predict Analysis
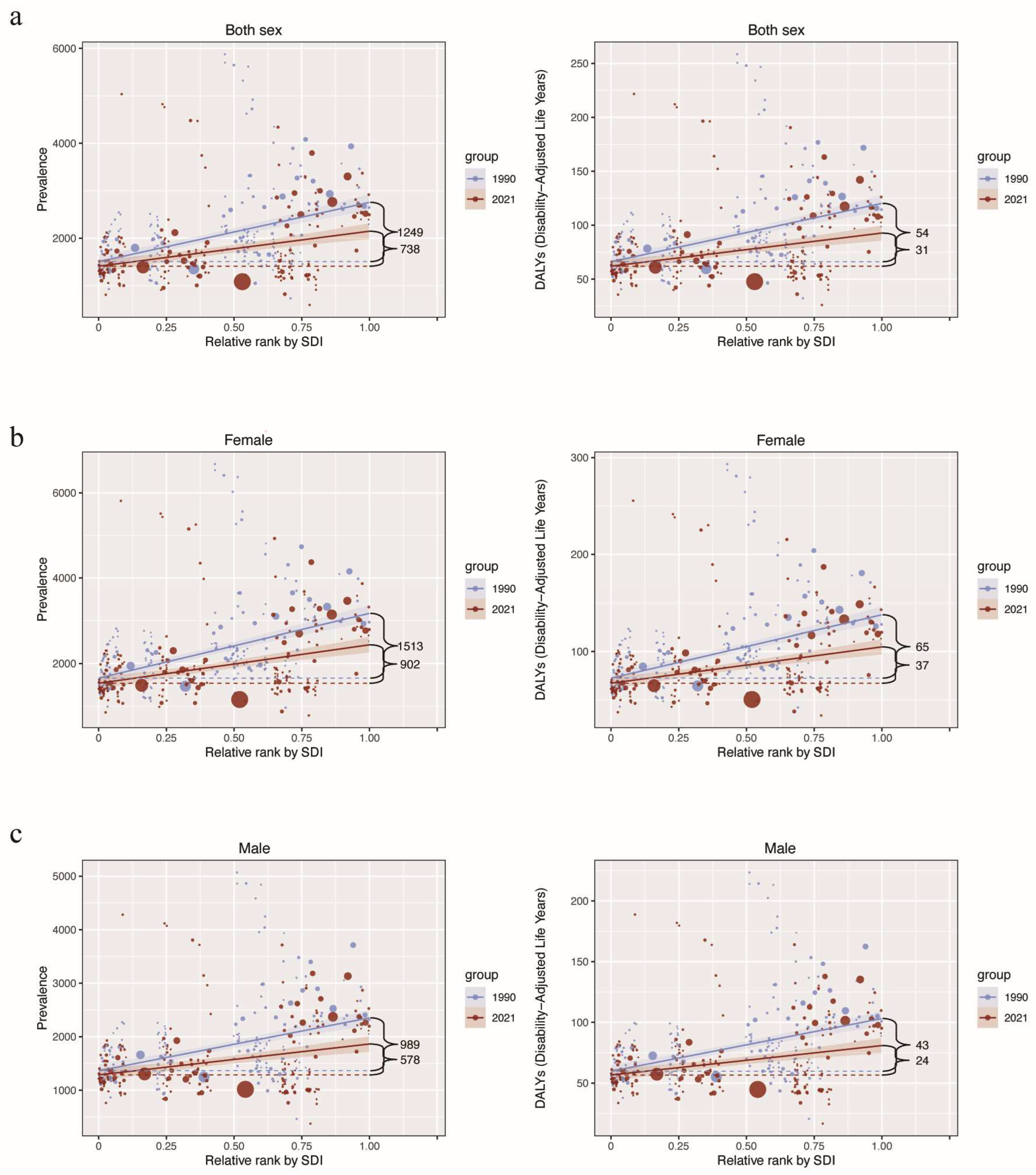
2.3. Health Inequality Analysis
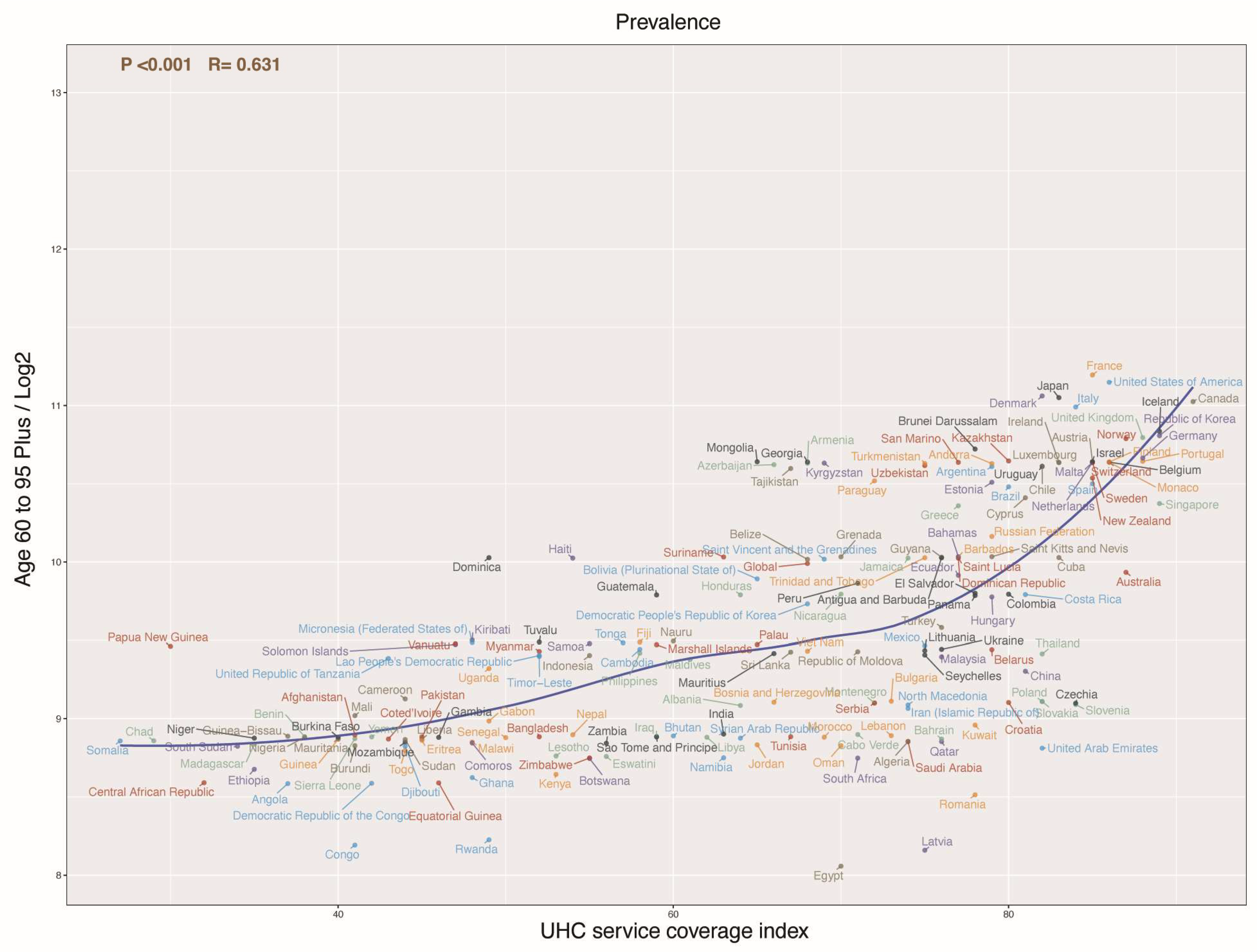
2.4. Correlation Analysis
2.5. Statistical Analysis
3. Results
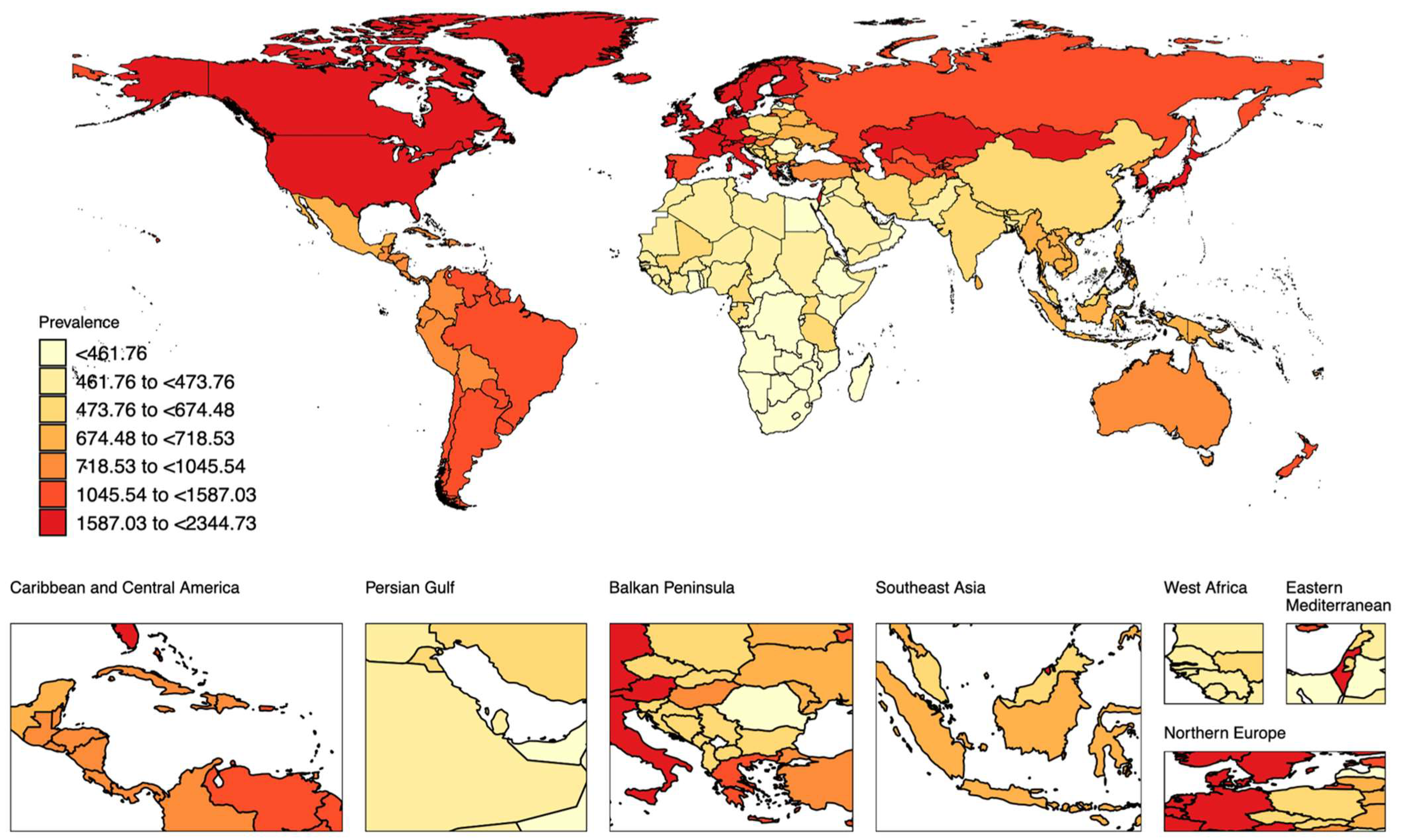
3.1. The Global and Regional Burden of Elderly AD in 2021
3.2. Trends in the Disease Burden in Elderly AD from 1990 to 2021
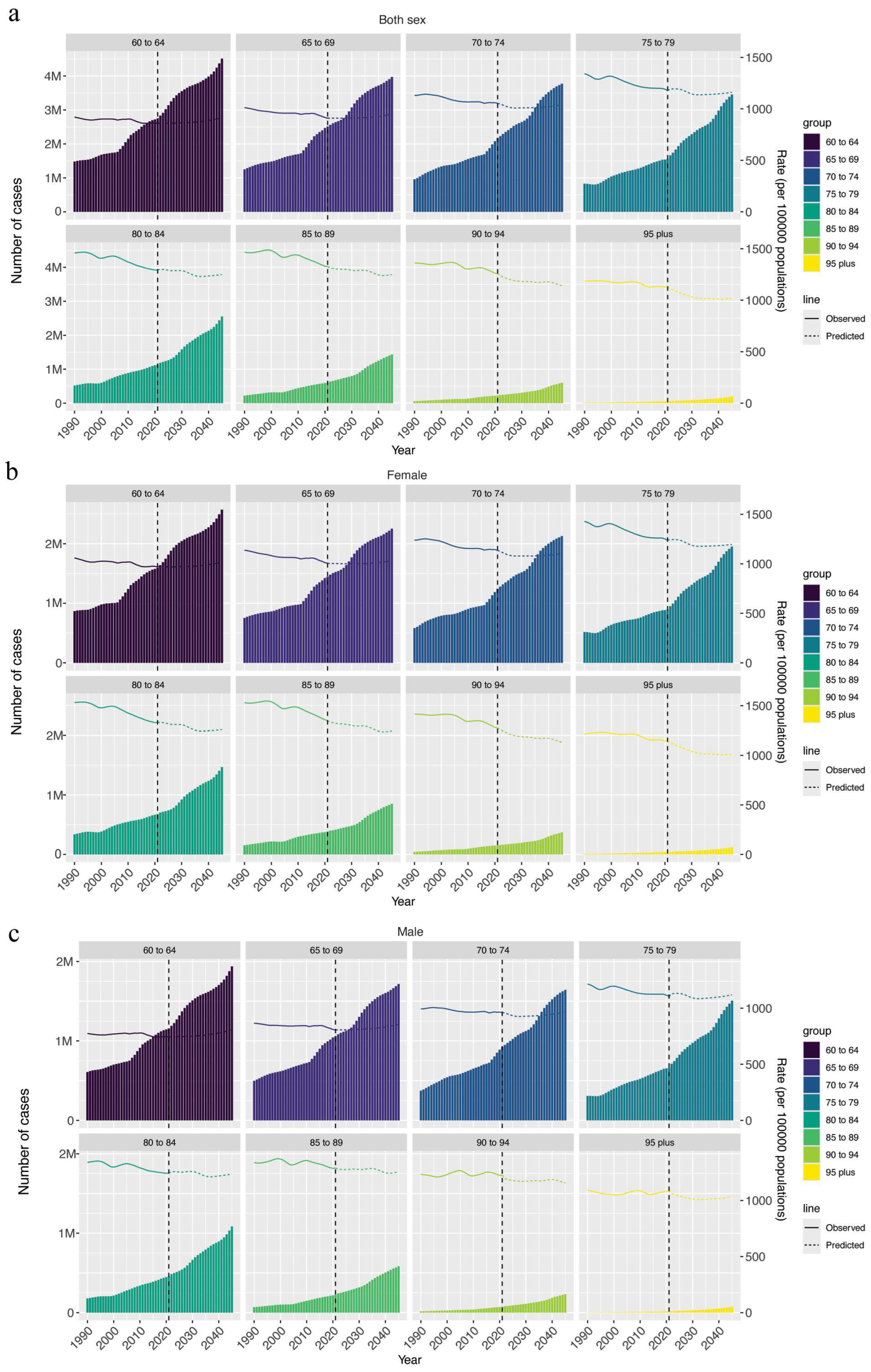
3.3. Prediction of the Disease Burden in Elderly AD from 2022 to 2045
3.4. Health Inequality and Gender Gap in Elderly AD Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AD | Atopic dermatitis |
| DALYs | Disability-adjusted life years |
| GBD | Global burden of disease |
| AAPC | Annual average percentage changes |
| UHC | Universal health coverage |
References
- Ständer, S. Atopic Dermatitis. N. Engl. J. Med. 2021, 384, 1136–1143. [Google Scholar] [CrossRef]
- Patel, K.R.; Immaneni, S.; Singam, V.; Rastogi, S.; Silverberg, J.I. Association between Atopic Dermatitis, Depression, and Suicidal Ideation: A Systematic Review and Meta-Analysis. J. Am. Acad. Dermatol. 2019, 80, 402–410. [Google Scholar] [CrossRef]
- Silverberg, J.I.; Gelfand, J.M.; Margolis, D.J.; Boguniewicz, M.; Fonacier, L.; Grayson, M.H.; Ong, P.Y.; Chiesa Fuxench, Z.C.; Simpson, E.L. Symptoms and Diagnosis of Anxiety and Depression in Atopic Dermatitis in U.S. Adults. Br. J. Dermatol. 2019, 181, 554–565. [Google Scholar] [CrossRef]
- Capucci, S.; Hahn-Pedersen, J.; Vilsbøll, A.; Kragh, N. Impact of Atopic Dermatitis and Chronic Hand Eczema on Quality of Life Compared With Other Chronic Diseases. Dermatitis 2020, 31, 178–184. [Google Scholar] [CrossRef]
- Birdi, G.; Larkin, M.; Chua, S.; Knibb, R.C. Quality of Life and Mental Well-being of Adults with Atopic Dermatitis Living in the UK. Clin. Exp. Allergy 2023, 53, 113–117. [Google Scholar] [CrossRef]
- Silverberg, J.I.; Gelfand, J.M.; Margolis, D.J.; Boguniewicz, M.; Fonacier, L.; Grayson, M.H.; Simpson, E.L.; Ong, P.Y.; Chiesa Fuxench, Z.C. Patient Burden and Quality of Life in Atopic Dermatitis in US Adults: A Population-Based Cross-Sectional Study. Ann. Allergy Asthma Immunol. 2018, 121, 340–347. [Google Scholar] [CrossRef]
- Mosam, A.; Todd, G. Global Epidemiology and Disparities in Atopic Dermatitis. Br. J. Dermatol. 2023, 188, 726–737. [Google Scholar] [CrossRef]
- Shin, Y.H.; Hwang, J.; Kwon, R.; Lee, S.W.; Kim, M.S.; GBD 2019 Allergic Disorders Collaborators; Shin, J.I.; Yon, D.K. Global, Regional, and National Burden of Allergic Disorders and Their Risk Factors in 204 Countries and Territories, from 1990 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Allergy 2023, 78, 2232–2254. [Google Scholar] [CrossRef]
- Peng, C.; Yu, N.; Ding, Y.; Shi, Y. Epidemiological Variations in Global Burden of Atopic Dermatitis: An Analysis of Trends from 1990 to 2019. Allergy 2022, 77, 2843–2845. [Google Scholar] [CrossRef]
- Abuabara, K.; Langan, S.M. Atopic Dermatitis across the Life Course. Br. J. Dermatol. 2023, 188, 709–717. [Google Scholar] [CrossRef] [PubMed]
- Vakharia, P.P.; Silverberg, J.I. Adult-Onset Atopic Dermatitis: Characteristics and Management. Am. J. Clin. Dermatol. 2019, 20, 771–779. [Google Scholar] [CrossRef]
- Williamson, S.; Merritt, J.; De Benedetto, A. Atopic Dermatitis in the Elderly: A Review of Clinical and Pathophysiological Hallmarks. Br. J. Dermatol. 2020, 182, 47–54. [Google Scholar] [CrossRef]
- Boren, E.; Gershwin, M.E. Inflamm-Aging: Autoimmunity, and the Immune-Risk Phenotype. Autoimmun. Rev. 2004, 3, 401–406. [Google Scholar] [CrossRef]
- Shaw, A.C.; Goldstein, D.R.; Montgomery, R.R. Age-Dependent Dysregulation of Innate Immunity. Nat. Rev. Immunol. 2013, 13, 875–887. [Google Scholar] [CrossRef]
- Maurelli, M.; Chiricozzi, A.; Peris, K.; Gisondi, P.; Girolomoni, G. Atopic Dermatitis in the Elderly Population. Acta Derm. Venereol. 2023, 103, adv13363. [Google Scholar] [CrossRef]
- Rony, M.K.K.; Parvin, M.R.; Wahiduzzaman, M.; Akter, K.; Ullah, M. Challenges and Advancements in the Health-Related Quality of Life of Older People. Adv. Public. Health 2024, 2024, 8839631. [Google Scholar] [CrossRef]
- Kanasi, E.; Ayilavarapu, S.; Jones, J. The Aging Population: Demographics and the Biology of Aging. Periodontol. 2000 2016, 72, 13–18. [Google Scholar] [CrossRef]
- Bhattacharjee, N.V.; Schumacher, A.E.; Aali, A.; Abate, Y.H.; Abbasgholizadeh, R.; Abbasian, M.; Abbasi-Kangevari, M.; Abbastabar, H.; ElHafeez, S.A.; Abd-Elsalam, S.; et al. Global Fertility in 204 Countries and Territories, 1950–2021, with Forecasts to 2100: A Comprehensive Demographic Analysis for the Global Burden of Disease Study 2021. Lancet 2024, 403, 2057–2099. [Google Scholar] [CrossRef]
- Vollset, S.E.; Ababneh, H.S.; Abate, Y.H.; Abbafati, C.; Abbasgholizadeh, R.; Abbasian, M.; Abbastabar, H.; Magied, A.H.A.A.A.; ElHafeez, S.A.; Abdelkader, A.; et al. Burden of Disease Scenarios for 204 Countries and Territories, 2022–2050: A Forecasting Analysis for the Global Burden of Disease Study 2021. Lancet 2024, 403, 2204–2256. [Google Scholar] [CrossRef]
- Jürgens, V.; Ess, S.; Cerny, T.; Vounatsou, P. A Bayesian Generalized Age-Period-Cohort Power Model for Cancer Projections. Stat. Med. 2014, 33, 4627–4636. [Google Scholar] [CrossRef]
- Hosseinpoor, A.R.; Bergen, N.; Kirkby, K.; Schlotheuber, A.; Antiporta, D.A.; Mac Feely, S. WHO’s Health Inequality Data Repository. Bull. World Health Organ. 2023, 101, 298–298A. [Google Scholar] [CrossRef] [PubMed]
- Cao, X.; Wang, M.; Zhou, M.; Mi, Y.; Guo, Q.; Fan, Y.; Guo, Y. Global, Regional and National Burden of Paediatric Atopic Dermatitis: A Trend and Geographic Inequalities Analysis. Clin. Exp. Allergy 2024, 54, 747–759. [Google Scholar] [CrossRef]
- Pollyn-Millot, C.; Maccari, F.; Perrot, J.L.; Reguiai, Z.; Boulard, C.; Becherel, P.A.; Poreaux, C.; Mery-Bossard, L.; Beaulieu, D.; Pourchot, D.; et al. Clinical Characteristics and Therapeutic Management of Atopic Dermatitis in Elderly Patients Compared with Young Adult Patients: A Prospective Multicentre Study. Acta Derm. Venereol. 2024, 104, adv40420. [Google Scholar] [CrossRef]
- Napolitano, M.; Potestio, L.; Nocerino, M.; Patruno, C. Considerations for Managing Elderly Patients with Atopic Dermatitis. Expert. Rev. Clin. Immunol. 2024, 20, 501–511. [Google Scholar] [CrossRef]
- Russo, F.; Milanesi, N.; Cartocci, A.; Bruzziches, F.; Tronconi, G.; Lazzeri, L.; D’erme, A.M.; Bagnoni, G.; Gola, M.; Cinotti, E.; et al. Dupilumab in Elderly Patients With Severe Atopic Dermatitis. Dermatitis 2021, 32, S24–S27. [Google Scholar] [CrossRef]
- Patruno, C.; Fabbrocini, G.; Longo, G.; Argenziano, G.; Ferrucci, S.M.; Stingeni, L.; Peris, K.; Ortoncelli, M.; Offidani, A.; Amoruso, G.F.; et al. Effectiveness and Safety of Long-Term Dupilumab Treatment in Elderly Patients with Atopic Dermatitis: A Multicenter Real-Life Observational Study. Am. J. Clin. Dermatol. 2021, 22, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Yew, Y.W.; Thyssen, J.P.; Silverberg, J.I. A Systematic Review and Meta-Analysis of the Regional and Age-Related Differences in Atopic Dermatitis Clinical Characteristics. J. Am. Acad. Dermatol. 2019, 80, 390–401. [Google Scholar] [CrossRef]
- Brunner, P.M.; Guttman-Yassky, E. Racial Differences in Atopic Dermatitis. Ann. Allergy Asthma Immunol. 2019, 122, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Zhao, Y.; Mu, Z.-L.; Lu, Q.-J.; Zhang, L.; Yao, X.; Zheng, M.; Tang, Y.-W.; Lu, X.-X.; Xia, X.-J.; et al. Clinical Features of Adult/Adolescent Atopic Dermatitis and Chinese Criteria for Atopic Dermatitis. Chin. Med. J. 2016, 129, 757–762. [Google Scholar] [CrossRef]
- Wang, S.; Zhu, R.; Gu, C.; Zou, Y.; Yin, H.; Xu, J.; Li, W. Distinct Clinical Features and Serum Cytokine Pattern of Elderly Atopic Dermatitis in China. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 2346–2352. [Google Scholar] [CrossRef]
- Martínez-González, M.C.; Martínez-González, R.-A.; Guerra-Tapia, A. Esthetic Dermatology and Emotional Well-Being According to Gender. J. Cosmet. Dermatol. 2018, 17, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.-P.; Stefanovic, N.; Orfali, R.L.; Aoki, V.; Brown, S.J.; Dhar, S.; Eichenfield, L.F.; Flohr, C.; Ha, A.; Mora, C.; et al. Impact of Climate Change on Atopic Dermatitis: A Review by the International Eczema Council. Allergy 2024, 79, 1455–1469. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.; Jing, D.; Xiao, Y.; Zhou, G.; Yang, S.; Liu, H.; Chen, X.; Shen, M. Association of Air Pollution and Genetic Risks with Incidence of Elderly-Onset Atopic Dermatitis: A Prospective Cohort Study. Ecotoxicol. Environ. Saf. 2023, 253, 114683. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.-C.; Liang, H.; Shi, L. The Convergence of Racial and Income Disparities in Health Insurance Coverage in the United States. Int. J. Equity Health 2021, 20, 96. [Google Scholar] [CrossRef]
- Zhou, M.; Zhao, S.; Zhao, Z. Gender Differences in Health Insurance Coverage in China. Int. J. Equity Health 2021, 20, 52. [Google Scholar] [CrossRef]
- Bollemeijer, J.F.; Zheng, K.J.; van der Meer, A.M.; Ikram, M.K.; Kavousi, M.; Brouwer, W.P.; Luik, A.I.; Chaker, L.; Xu, Y.; Gunn, D.A.; et al. Lifetime Prevalence and Associated Factors of Itch with Skin Conditions: Atopic Dermatitis, Psoriasis and Dry Skin in Individuals Aged > 50 Years. Clin. Exp. Dermatol. 2024, 49, 1036–1043. [Google Scholar] [CrossRef]
- Wu, P.-C.; Li, C.-L.; Chang, Y.-T.; Chen, C.-C.; Wu, C.-Y.; Ma, S.-H. Management of Atopic Dermatitis During the COVID-19 Pandemic: Key Questions and Review of the Current Evidence. Dermatitis 2023, 34, 77–84. [Google Scholar] [CrossRef]
- Hernández, N.; Sanclemente, G.; Tamayo, L.; López, Á.; Seidel, A. Colombian Atopic Dermatitis Research Group Members Atopic Dermatitis in the COVID-19 Era: Results from a Web-Based Survey. World Allergy Organ. J. 2021, 14, 100571. [Google Scholar] [CrossRef] [PubMed]
| Rate (per 100,000) (95% UI) | |||
|---|---|---|---|
| 1990 | 2021 | AAPC (%) | |
| Prevalence | |||
| Global | 1117.11 (1005.84–1234.26) | 1017.00 (915.91–1124.40) | −0.3 (0.28 to 0.32) |
| Sex | |||
| Female | 1229.35 (1108.02–1357.44) | 1099.24 (991.32–1216.65) | −0.36 (−0.38 to −0.33) |
| Male | 979.51 (879.88–1082.78) | 924.82 (831.96–1023.50) | −0.19 (−0.20 to −0.17) |
| SDI regions | |||
| Low SDI | 482.46 (427.16–541.41) | 483.57 (428.53–542.78) | 0.01 (0.01 to 0.02) |
| Low-middle SDI | 578.59 (518.86–643.57) | 586.51 (525.58–651.69) | 0.04 (0.03 to 0.05) |
| Middle SDI | 697.89 (627.06–772.39) | 693.08 (624.80–767.56) | −0.03 (−0.03 to −0.02) |
| High-middle SDI | 1010.72 (905.53–1124.15) | 921.59 (824.87–1024.74) | −0.30 (−0.33 to −0.26) |
| High SDI | 1865.91 (1681.75–2059.43) | 1839.83 (1657.87–2030.61) | −0.04 (−0.05 to −0.04) |
| Incidence | |||
| Global | 136.94 (115.24–160.86) | 128.22 (108.19–150.09) | −0.21 (−0.22 to 0.20) |
| Sex | |||
| Female | 145.58 (122.46–171.46) | 134.86 (113.46–158.24) | −0.25 (−0.25 to −0.24) |
| Male | 126.53 (106.73–148.27) | 120.78 (101.91–141.52) | −0.15 (−0.16 to −0.14) |
| SDI regions | |||
| Low SDI | 72.34 (60.12–86.03) | 72.70 (60.33–86.18) | 0.02 (0.017 to 0.025) |
| Low-middle SDI | 84.37 (71.35–98.80) | 85.36 (72.06–100.02) | 0.034 (0.03 to 0.04) |
| Middle SDI | 103.01 (87.62–119.84) | 102.34 (87.59–118.85) | −0.02 (−0.023 to −0.019) |
| High-middle SDI | 130.42 (109.78–153.18) | 122.67 (103.49–143.96) | −0.20 (−0.21 to −0.18) |
| High SDI | 205.49 (171.60–243.28) | 203.26 (169.80–240.63) | −0.03 (−0.04 to −0.03) |
| DALY | |||
| Global | 44.86 (23.91–75.27) | 40.83 (21.77–68.63) | −0.30 (−0.32 to −0.29) |
| Sex | |||
| Female | 49.28 (26.28–82.59) | 44.00 (23.49–73.88) | −0.36 (−0.39 to −0.33) |
| Male | 39.47 (21.06–66.46) | 37.29 (19.81–62.85) | −0.18 (−0.19 to −0.17) |
| SDI regions | |||
| Low SDI | 19.69 (10.42–34.05) | 19.81 (10.45–34.56) | 0.03 (0.02–0.04) |
| Low-middle SDI | 23.42 (12.45–40.12) | 23.73 (12.63–40.71) | 0.04 (0.03–0.06) |
| Middle SDI | 28.48 (15.12–48.61) | 28.23 (15.01–48.23) | −0.03 (−0.04 to −0.02) |
| High-middle SDI | 40.67 (21.75–68.40) | 37.24 (19.94–63.03) | −0.28 (−0.32 to −0.24) |
| High SDI | 74.66 (39.95–124.69) | 73.28 (39.10–122.07) | −0.06 (−0.07 to −0.05) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Z.; Gu, J.; Tang, T.; Huang, X.; Wu, Y.; Li, Y.; Dou, X.; Yu, B.; Li, C.; Zhang, H. The Global Burden of Atopic Dermatitis in Elderly Populations: Trends, Disparities, and Future Projections. Healthcare 2025, 13, 788. https://doi.org/10.3390/healthcare13070788
Li Z, Gu J, Tang T, Huang X, Wu Y, Li Y, Dou X, Yu B, Li C, Zhang H. The Global Burden of Atopic Dermatitis in Elderly Populations: Trends, Disparities, and Future Projections. Healthcare. 2025; 13(7):788. https://doi.org/10.3390/healthcare13070788
Chicago/Turabian StyleLi, Zizhuo, Jiaxu Gu, Tian Tang, Xinyue Huang, You Wu, Yannan Li, Xia Dou, Bo Yu, Chengxin Li, and Han Zhang. 2025. "The Global Burden of Atopic Dermatitis in Elderly Populations: Trends, Disparities, and Future Projections" Healthcare 13, no. 7: 788. https://doi.org/10.3390/healthcare13070788
APA StyleLi, Z., Gu, J., Tang, T., Huang, X., Wu, Y., Li, Y., Dou, X., Yu, B., Li, C., & Zhang, H. (2025). The Global Burden of Atopic Dermatitis in Elderly Populations: Trends, Disparities, and Future Projections. Healthcare, 13(7), 788. https://doi.org/10.3390/healthcare13070788






