An Innovative Assessment Framework for Remote Care in Orthopedics
Abstract
1. Introduction
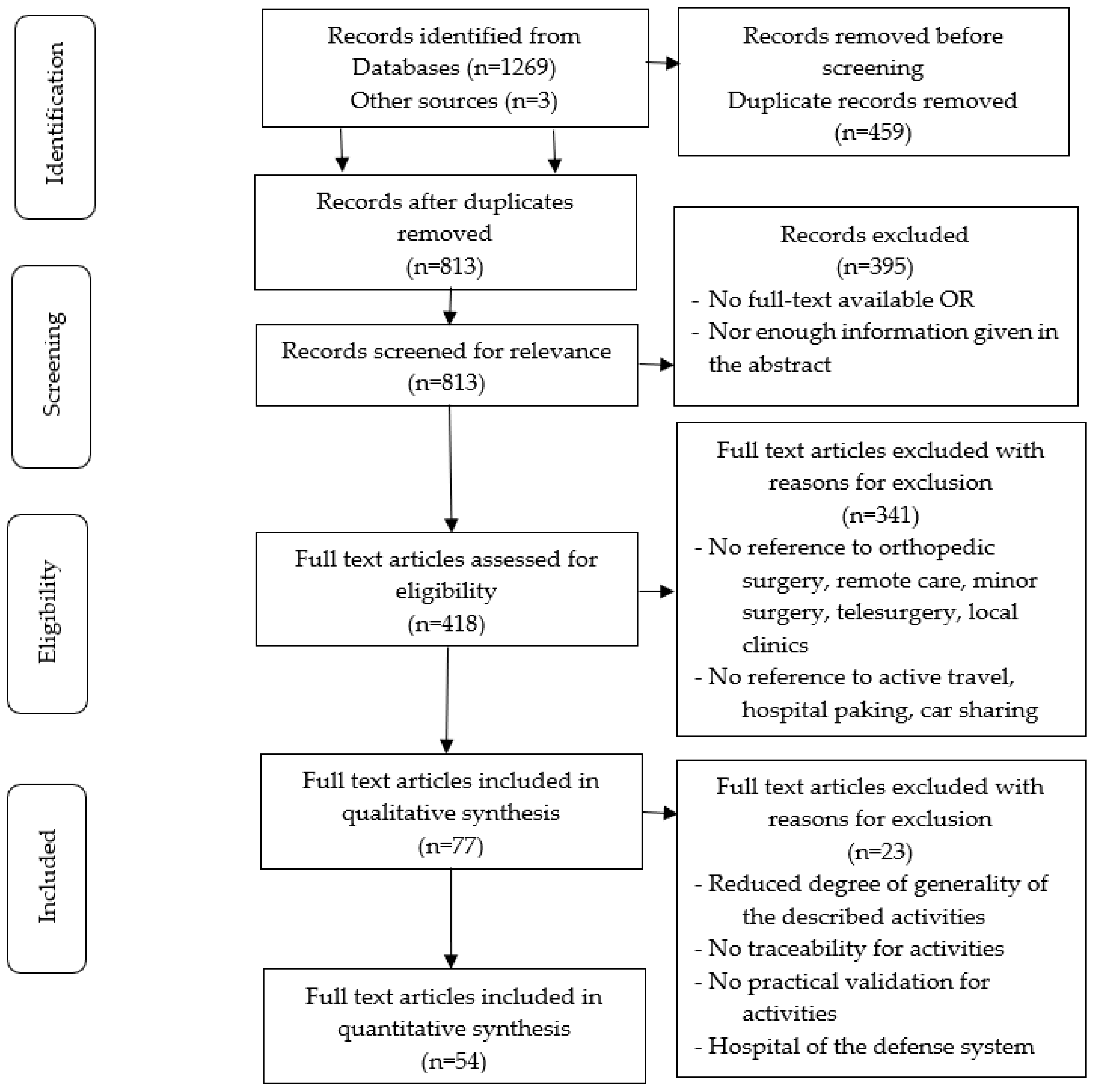
2. Materials and Methods
- Research design;
- Design of the key domains for remote care in orthopedics;
- Data collection and analysis from the scientific literature in the medical field and extracting the most relevant and recent aspects related to remote care in orthopedics that have been implemented by international hospitals;
- Elaboration of the contents and evaluation grids of the indicators for the remote care in orthopedics, where it is used as inputs for the information collected from the analysis of the scientific literature;
- Validation in practice of the developed theoretical model at an orthopedic emergency hospital.
2.1. The Research Design
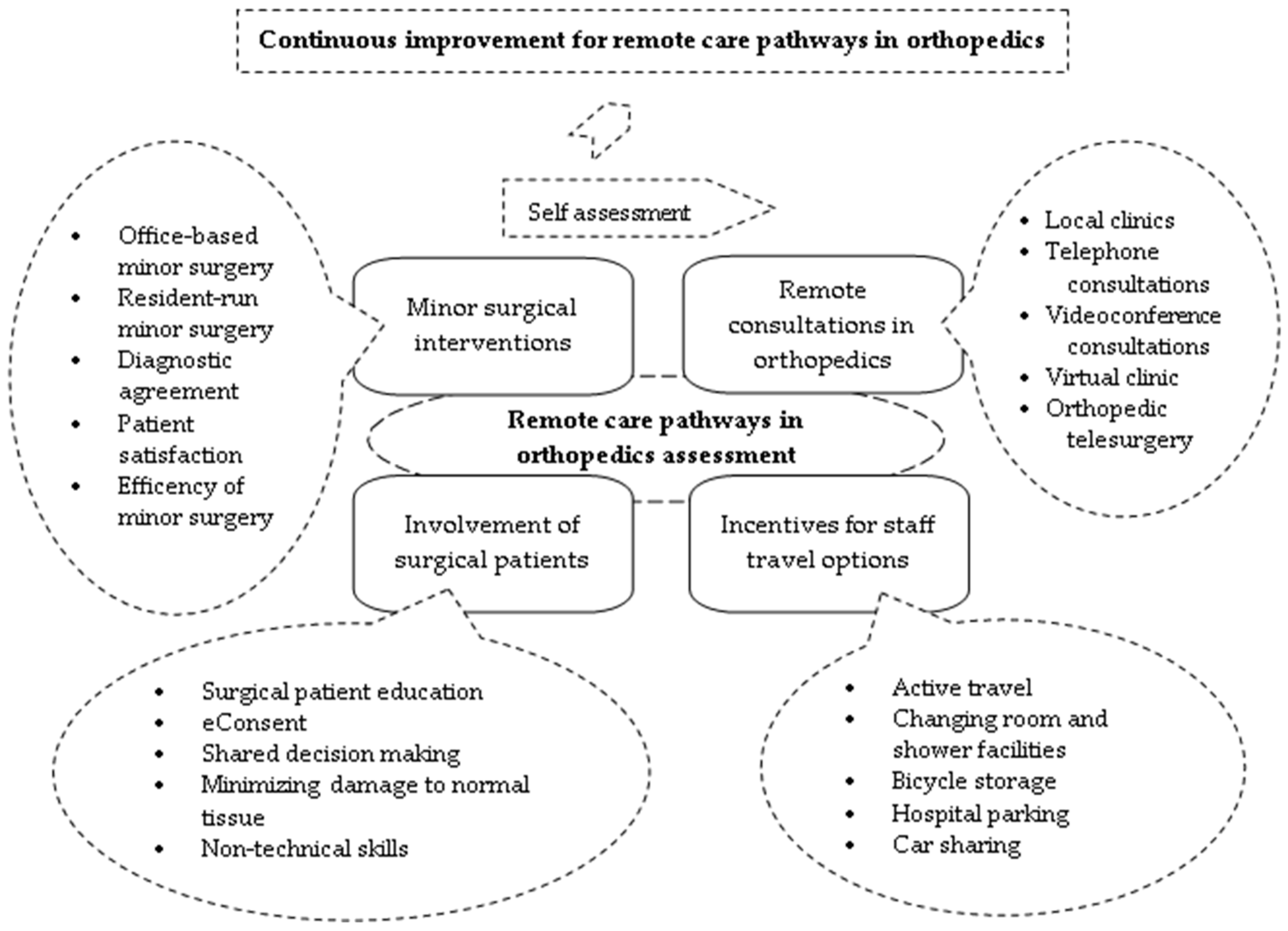
2.2. The Key Domains for Remote Care Pathways in Orthopedic Surgery
2.3. Data Collection and Analysis
2.4. Validation in Practice of the Developed Theoretical Model
3. Results
3.1. Indicators Contents and Evaluation Grids for the Key Areas
3.1.1. The Key Area Remote Consultations in Orthopedics
3.1.2. The Key Area Incentives for Staff Travel Options
3.1.3. The Key Area Involvement of Surgical Patients
3.1.4. The Key Area Minor Surgical Interventions
3.1.5. Levels of Importance for Indicators
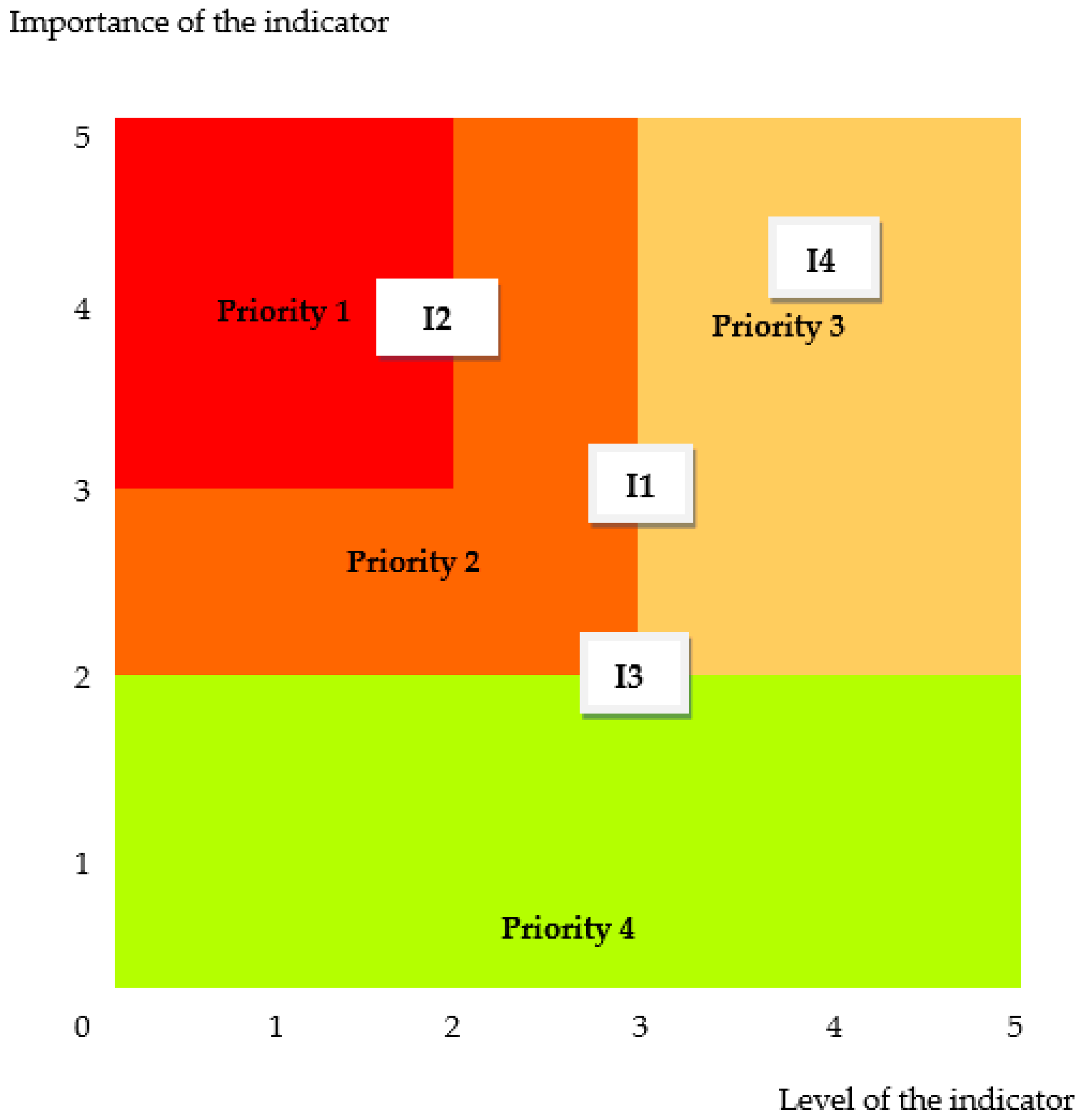
3.2. Indicator Matrix and Continuous Improvement Cycle
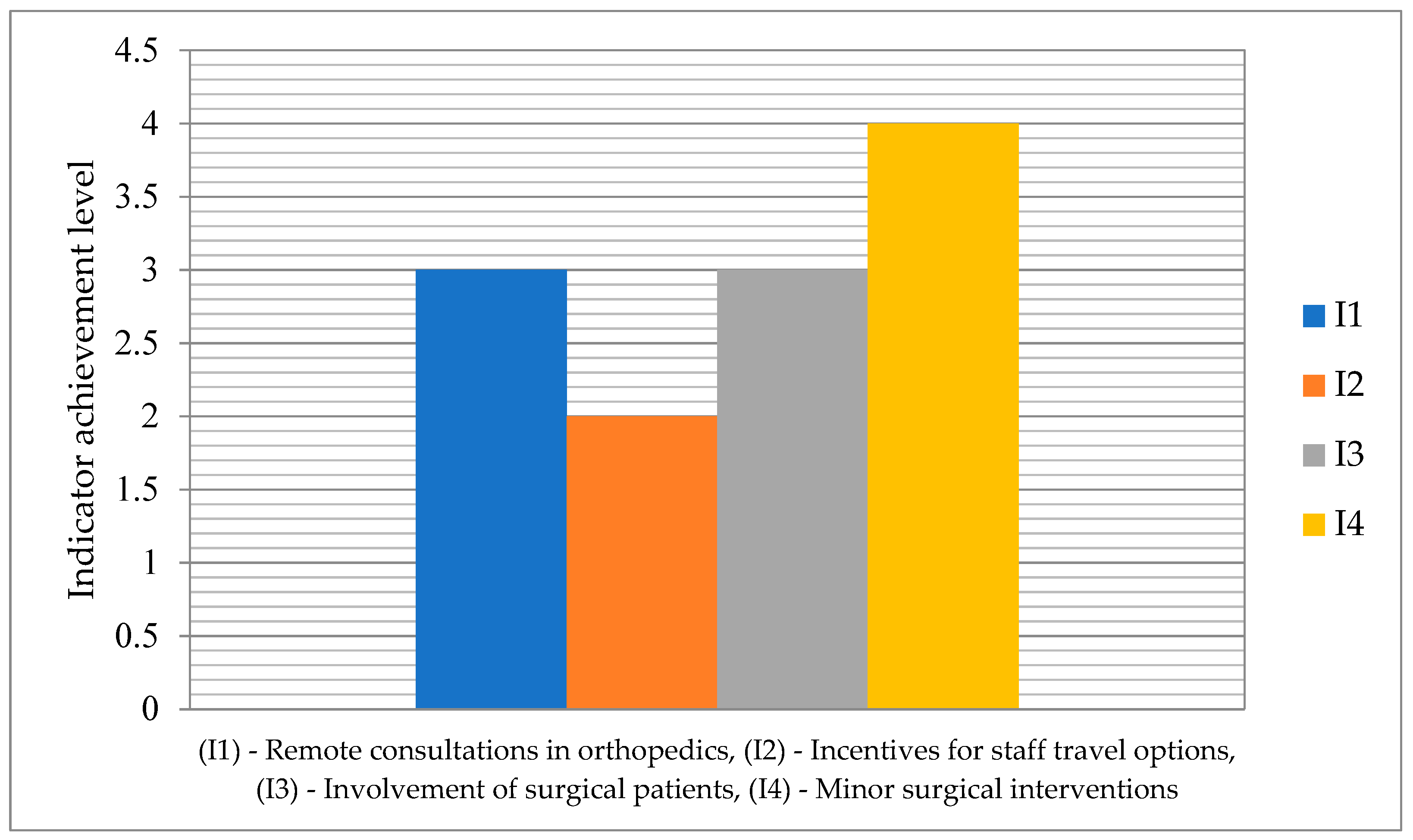
3.3. Practical Validation of the Theoretical Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yates, E.F.; Bowder, A.N.; Roa, L.; Velin, L.; Goodman, A.S.; Nguyen, L.L.; McClain, C.D.; Meara, J.G.; Cooper, Z. Empowering Surgeons, Anesthesiologists, and Obstetricians to Incorporate Environmental Sustainability in the Operating Room. Ann. Surg. 2021, 273, 1108–1114. [Google Scholar] [PubMed]
- Smith, J.T.; Boakye, L.A.T.; Ferrone, M.L.; Furie, G.L. Environmental Sustainability in the Orthopaedic Operating Room. J. Am. Acad. Orthop. Surg. 2022, 30, 1039–1045. [Google Scholar] [PubMed]
- Holmner, A.; Ebi, K.L.; Lazuardi, L.; Nilsson, M. Carbon footprint of telemedicine solutions--unexplored opportunity for reducing carbon emissions in the health sector. PLoS ONE 2014, 9, e105040. [Google Scholar]
- Mikolajczyk, T.; Moldovan, L.; Chalupczak, A.; Moldovan, F. Computer Aided Learning Process. Procedia Eng. 2017, 181, 1028–1035. [Google Scholar]
- Mikolajczyk, T.; Moldovan, F.; Ciobanu, I.; Chalupczak, A.; Georgiana Marin, A. Brain Research Using Computer Test. Procedia Technol. 2016, 22, 1113–1120. [Google Scholar]
- Cummins, M.R.; Shishupal, S.; Wong, B.; Wan, N.; Han, J.; Johnny, J.D.; Mhatre-Owens, A.; Gouripeddi, R.; Ivanova, J.; Ong, T.; et al. Travel Distance Between Participants in US Telemedicine Sessions with Estimates of Emissions Savings: Observational Study. J. Med. Internet Res. 2024, 26, e53437. [Google Scholar]
- Ciobanu, I.; Stanculescu Badea, D.I.; Iliescu, A.; Magdalena Popescu, A.; Seiciu, P.S.; Mikolajczyk, T.; Moldovan, F.; Berteanu, M. The Usability Pilot Study of a Mechatronic System for Gait Rehabilitation. Procedia Manuf. 2018, 22, 864–871. [Google Scholar] [CrossRef]
- Sillcox, R.; Blaustein, M.; Khandelwal, S.; Bryant, M.K.; Zhu, J.; Chen, J.Y. Telemedicine Use Decreases the Carbon Footprint of the Bariatric Surgery Preoperative Evaluation. Obes. Surg. 2023, 33, 2527–2532. [Google Scholar]
- Sillcox, R.; Gitonga, B.; Meiklejohn, D.A.; Wright, A.S.; Oelschlager, B.K.; Bryant, M.K.; Tarefder, R.; Khan, Z.; Zhu, J. The environmental impact of surgical telemedicine: Life cycle assessment of virtual vs. in-person preoperative evaluations for benign foregut disease. Surg. Endosc. 2023, 37, 5696–5702. [Google Scholar] [CrossRef]
- Audrey, S.; Fisher, H.; Cooper, A.; Gaunt, D.; Garfield, K.; Metcalfe, C.; Hollingworth, W.; Gillison, F.; Gabe-Walters, M.; Rodgers, S.; et al. Evaluation of an intervention to promote walking during the commute to work: A cluster randomised controlled trial. BMC Public. Health. 2019, 19, 427. [Google Scholar] [CrossRef]
- Moldovan, F. Bone Cement Implantation Syndrome: A Rare Disaster Following Cemented Hip Arthroplasties-Clinical Considerations Supported by Case Studies. J. Pers. Med. 2023, 13, 1381. [Google Scholar] [CrossRef] [PubMed]
- Wen, L.M.; Kite, J.; Rissel, C. Is there a role for workplaces in reducing employees’ driving to work? Findings from a cross-sectional survey from inner-west Sydney, Australia. BMC Public Health 2010, 10, 50. [Google Scholar] [CrossRef] [PubMed]
- González Moreno, M.; Reboso Morales, L.E.; Martín Hidalgo, A.Y.; Kesserwan, H.M.; García Bello, M.Á. Consultas virtuales en Traumatología y Cirugía Ortopédica [Virtual consultations in Traumatology and Orthopaedic Surgery]. Semergen 2021, 47, 305–314. [Google Scholar] [CrossRef]
- Rizan, C.; Reed, M.; Mortimer, F.; Jones, A.; Stancliffe, R.; Bhutta, M.F. Using surgical sustainability principles to improve planetary health and optimise surgical services following the COVID-19 pandemic. Bull. R. Coll. Surg. Engl. 2020, 102, 177–181. [Google Scholar] [CrossRef]
- Moldovan, F. New Approaches and Trends in Health Care. Procedia Manuf. 2018, 22, 947–951. [Google Scholar] [CrossRef]
- Jackson, A.M. Uncovering the “skeleton in the closet”: The issue of bone and joint disorders in the Maldives and the opportunities for primary prevention and health promotion. J. Prim. Prev. 2006, 27, 409–431. [Google Scholar] [CrossRef]
- Renaldo, N.; Egol, K. Damage-control orthopedics: Evolution and practical applications. Am. J. Orthop. 2006, 35, 285–291. [Google Scholar]
- Royal College of Surgeons of England. Recovery of Surgical Services During and After COVID-19. Tool 4: Virtual Consultations. 2020. Available online: https://www.rcseng.ac.uk/coronavirus/recovery-of-surgical-services/tool-4 (accessed on 18 November 2024).
- County Emergency Clinical Hospital of Targu Mures. Available online: https://www.spitalmures.ro/en/ (accessed on 18 November 2024).
- Royal College of Surgeons of England. Sustainability in the Operating Theatre. Available online: https://www.rcseng.ac.uk/standards-and-research/standards-and-guidance/good-practice-guides/sustainability-in-operating-theatre/ (accessed on 18 November 2024).
- Donaghy, C.; Smith, N.; O’Dea, F. Orthopaedic Outreach: An innovative programme for orthopaedic patients in remote areas of Newfoundland and Labrador. Can. J. Rural. Med. 2022, 27, 143–147. [Google Scholar] [CrossRef]
- Estel, K.; Richter, L.; Weber, G.; Fellmer, F.; Mardin, S.; Willy, C.; Back, D.A. The use of video consultations to support orthopedic patients’ treatment at the interface of a clinic and general practitioners. BMC Musculoskelet. Disord. 2022, 23, 968. [Google Scholar]
- Grewal, N.; Idhrees, M.; Velayudhan, B.; Klautz, R.J.M.; Grewal, S. Practical Considerations of Remote Care in Thoracic Aortopathy in India. J. Clin. Med. 2024, 13, 3327. [Google Scholar] [CrossRef]
- Roberts, A.; Johnston, G.H.F.; Landells, C. COVID-19: Pivoting from in-person to virtual orthopedic surgical evaluation. Can. J. Surg. 2021, 64, E101–E102. [Google Scholar]
- Haider, Z.; Aweid, B.; Subramanian, P.; Iranpour, F. Telemedicine in orthopaedics during COVID-19 and beyond: A systematic review. J. Telemed. Telecare 2022, 28, 391–403. [Google Scholar] [CrossRef]
- Woodmass, M.; Ramshaw, K.; Lakshmanan, P. Utility of telephone consultations during COVID-19 and beyond: A study of orthopedic spinal patients. Minerva Surg. 2022, 77, 360–367. [Google Scholar] [PubMed]
- Grandizio, L.C.; Foster, B.K.; Klena, J.C. Telemedicine in Hand and Upper-Extremity Surgery. J. Hand Surg. Am. 2020, 45, 239–242. [Google Scholar]
- Buvik, A.; Bergmo, T.S.; Bugge, E.; Smaabrekke, A.; Wilsgaard, T.; Olsen, J.A. Cost-Effectiveness of Telemedicine in Remote Orthopedic Consultations: Randomized Controlled Trial. J. Med. Internet Res. 2019, 21, e11330. [Google Scholar] [PubMed]
- Buvik, A.; Bugge, E.; Knutsen, G.; Småbrekke, A.; Wilsgaard, T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: A randomised controlled trial. J. Telemed. Telecare. 2019, 25, 451–459. [Google Scholar] [PubMed]
- St Clair, M.; Murtagh, D. Barriers to Telehealth Uptake in Rural, Regional, Remote Australia: What Can Be Done to Expand Telehealth Access in Remote Areas? Stud. Health Technol. Inform. 2019, 266, 174–182. [Google Scholar]
- Seto, E.; Smith, D.; Jacques, M.; Morita, P.P. Opportunities and Challenges of Telehealth in Remote Communities: Case Study of the Yukon Telehealth System. JMIR Med. Inform. 2019, 7, e11353. [Google Scholar] [CrossRef]
- Hughes, A.J.; Moloney, D.P.; Fraser, C.; Dembo, J.; O’Brien, L.; Corcoran, M.; Crowley, M.; Conlon, B.; Sheehan, E. Remote Delivery of the Satellite Virtual Fracture Clinic—A Pilot Report of the First 500 Cases. Injury 2021, 52, 782–786. [Google Scholar] [CrossRef]
- Snoswell, C.L.; North, J.B.; Caffery, L.J. Economic Advantages of Telehealth and Virtual Health Practitioners: Return on Investment Analysis. JMIR Perioper. Med. 2020, 3, e15688. [Google Scholar]
- Behmanesh, A.; Sadoughi, F.; Mazhar, F.N.; Joghataei, M.T.; Yazdani, S. Tele-orthopaedics: A systematic mapping study. J. Telemed. Telecare 2022, 28, 3–23. [Google Scholar] [CrossRef] [PubMed]
- Sahu, D.; Shah, D.; Joshi, M.; Shaikh, S.; Gaikwad, P.; Shyam, A. Validation of an on-screen application-based measurement of shoulder range of motion over telehealth medium. J. Shoulder Elbow Surg. 2022, 31, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, H.; Nadeem, S.; Mundi, R. How Satisfied Are Patients and Surgeons with Telemedicine in Orthopaedic Care During the COVID-19 Pandemic? A Systematic Review and Meta-analysis. Clin. Orthop. Relat. Res. 2021, 479, 47–56. [Google Scholar] [CrossRef]
- Panter, J.; Heinen, E.; Mackett, R.; Ogilvie, D. Impact of New Transport Infrastructure on Walking, Cycling, and Physical Activity. Am. J. Prev. Med. 2016, 50, e45–e53. [Google Scholar] [CrossRef]
- Levi, S.; Baron-Epel, O.; Tesler, R.; Harel-Fisch, Y. Patterns of Active Travel and Physical Activity among Adolescents in Israel. Int. J. Environ. Res. Public. Health 2022, 19, 14115. [Google Scholar]
- Götschi, T.; de Nazelle, A.; Brand, C.; Gerike, R.; PASTA Consortium. Towards a Comprehensive Conceptual Framework of Active Travel Behavior: A Review and Synthesis of Published Frameworks. Curr. Environ. Health Rep. 2017, 4, 286–295. [Google Scholar] [CrossRef]
- Heinen, E.; Panter, J.; Mackett, R.; Ogilvie, D. Changes in mode of travel to work: A natural experimental study of new transport infrastructure. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 81. [Google Scholar] [CrossRef] [PubMed]
- Wangzom, D.; White, M.; Paay, J. Perceived Safety Influencing Active Travel to School-A Built Environment Perspective. Int. J. Environ. Res. Public. Health 2023, 20, 1026. [Google Scholar]
- Patterson, R.; Ogilvie, D.; Panter, J. The social and physical workplace environment and commute mode: A natural experimental study. Prev. Med. Rep. 2020, 20, 101260. [Google Scholar] [CrossRef]
- Ohlms, P.B.; Kweon, Y.J. Facilitating bicycle travel using innovative intersection pavement markings. J. Safety Res. 2018, 67, 173–182. [Google Scholar] [CrossRef]
- Liu, Q.; Yamada, T.; Liu, H.; Lin, L.; Fang, Q. Healthy Behavior and Environmental Behavior Correlate with Bicycle Commuting. Int. J. Environ. Res. Public. Health 2022, 19, 3318. [Google Scholar] [PubMed]
- Liyana Arachige, M.; Tse, W.C.; Zhang, R.; Ma, H.; Singhal, S.; Phan, T. Estimating the cost of visiting hospital outpatient. BMJ Neurol. Open. 2024, 6, e000576. [Google Scholar]
- Baillie, J. Hospital parking--the big squeeze. Health Estate 2009, 63, 43–48. [Google Scholar] [PubMed]
- Correa, A.; Boquet, G.; Morell, A.; Lopez Vicario, J. Autonomous Car Parking System through a Cooperative Vehicular Positioning Network. Sensors 2017, 17, 848. [Google Scholar] [CrossRef]
- Knott, C.S.; Sharp, S.J.; Mytton, O.T.; Ogilvie, D.; Panter, J. Changes in workplace car parking and commute mode: A natural experimental study. J. Epidemiol. Community Health 2019, 73, 42–49. [Google Scholar] [PubMed]
- Chen, M.; Sun, Y.; Waygood, E.O.D.; Yu, J.; Zhu, K. User characteristics and service satisfaction of car sharing systems: Evidence from Hangzhou, China. PLoS ONE 2022, 17, e0263476. [Google Scholar]
- Enzi, M.; Parragh, S.N.; Puchinger, J. The bi-objective multimodal car-sharing problem. OR Spectr. 2022, 44, 307–348. [Google Scholar] [CrossRef]
- Xu, Y.; Ji, X.; Jin, Z. What travel scenarios are the opportunities of car sharing? PLoS ONE 2021, 16, e0260605. [Google Scholar]
- Mitropoulos, L.; Kortsari, A.; Ayfantopoulou, G. A systematic literature review of ride-sharing platforms, user factors and barriers. Eur. Transp. Res. Rev. 2021, 13, 61. [Google Scholar]
- Shabur, M.A.; Ali, M.F. Perspectives and possibilities for developing ride-sharing services to promote sustainable mode of transport: Bangladesh perspective. Heliyon 2024, 10, e33115. [Google Scholar]
- Timmers, T.; Janssen, L.; van der Weegen, W.; Das, D.; Marijnissen, W.J.; Hannink, G.; van der Zwaard, B.C.; Plat, A.; Thomassen, B.; Swen, J.W.; et al. The Effect of an App for Day-to-Day Postoperative Care Education on Patients with Total Knee Replacement: Randomized Controlled Trial. JMIR Mhealth Uhealth 2019, 7, e15323. [Google Scholar]
- Stauber, A.; Schüßler, N.; Palmdorf, S.; Schürholz, N.; Bruns, D.; Osterbrink, J.; Nestler, N. RECOVER-E—A mobile app for patients undergoing total knee or hip replacement: Study protocol. BMC Musculoskelet. Disord. 2020, 21, 71. [Google Scholar]
- Pronk, Y.; Peters, M.C.W.M.; Sheombar, A.; Brinkman, J.M. Effectiveness of a Mobile eHealth App in Guiding Patients in Pain Control and Opiate Use After Total Knee Replacement: Randomized Controlled Trial. JMIR Mhealth Uhealth 2020, 8, e16415. [Google Scholar]
- Kassam, I.; Ilkina, D.; Kemp, J.; Roble, H.; Carter-Langford, A.; Shen, N. Patient Perspectives and Preferences for Consent in the Digital Health Context: State-of-the-art Literature Review. J. Med. Internet Res. 2023, 25, e42507. [Google Scholar] [PubMed]
- Cohen, E.; Byrom, B.; Becher, A.; Jörntén-Karlsson, M.; Mackenzie, A.K. Comparative Effectiveness of eConsent: Systematic Review. J. Med. Internet Res. 2023, 25, e43883. [Google Scholar] [PubMed]
- Spencer, K.; Sanders, C.; Whitley, E.A.; Lund, D.; Kaye, J.; Dixon, W.G. Patient Perspectives on Sharing Anonymized Personal Health Data Using a Digital System for Dynamic Consent and Research Feedback: A Qualitative Study. J. Med. Internet Res. 2016, 18, e66. [Google Scholar] [PubMed]
- Flynn, D.; Knoedler, M.A.; Hess, E.P.; Murad, M.H.; Erwin, P.J.; Montori, V.M.; Thomson, R.G. Engaging patients in health care decisions in the emergency department through shared decision-making: A systematic review. Acad. Emerg. Med. 2012, 19, 959–967. [Google Scholar]
- Bombard, Y.; Baker, G.R.; Orlando, E.; Fancott, C.; Bhatia, P.; Casalino, S.; Onate, K.; Denis, J.L.; Pomey, M.P. Engaging patients to improve quality of care: A systematic review. Implement. Sci. 2018, 13, 98. [Google Scholar]
- Park, H.K.; Chang, J.C. Microdecompression in spinal stenosis: A review. J. Neurosurg. Sci. 2014, 58, 57–64. [Google Scholar]
- Lawton, C.D.; Smith, Z.A.; Lam, S.K.; Habib, A.; Wong, R.H.; Fessler, R.G. Clinical outcomes of microendoscopic foraminotomy and decompression in the cervical spine. World Neurosurg. 2014, 81, 422–427. [Google Scholar]
- Pena, G.; Altree, M.; Field, J.; Thomas, M.J.; Hewett, P.; Babidge, W.; Maddern, G.J. Surgeons’ and trainees’ perceived self-efficacy in operating theatre non-technical skills. Br. J. Surg. 2015, 102, 708–715. [Google Scholar]
- van den Dool, H.; Jochemsen-van der Leeuw, R.; van Dijk, N. Office-Based Minor Surgery: An Ever-Increasing Challenge Not Only for the Dutch General Practitioner. Fam. Med. 2023, 55, 27–33. [Google Scholar] [PubMed]
- Johnson, K.A. Minimally Invasive Orthopaedic Surgery. Vet. Comp. Orthop. Traumatol. 2021, 34, v–vi. [Google Scholar] [PubMed]
- Moldovan, L.; Gligor, A.; Grif, H.-S.; Moldovan, F. Dynamic Numerical Simulation of the 6-PGK Parallel Robot Manipulator. Proc. Rom. Acad. Ser. A. 2019, 20, 67–75. [Google Scholar]
- Wojcik, B.M.; McKinley, S.K.; Fong, Z.V.; Mansur, A.; Bloom, J.P.; Amari, N.; Hamdi, I.; Chang, D.C.; Petrusa, E.; Mullen, J.T.; et al. The Resident-Run Minor Surgery Clinic: A Four-Year Analysis of Patient Outcomes, Satisfaction, and Resident Education. J. Surg. Educ. 2021, 78, 1838–1850. [Google Scholar]
- Moldovan, F.; Gligor, A.; Moldovan, L.; Bataga, T. The Impact of the COVID-19 Pandemic on the Orthopedic Residents: A Pan-Romanian Survey. Int. J. Environ. Res. Public. Health 2022, 19, 9176. [Google Scholar]
- Zhang, Y.Z. Minimally Invasive Reduction and Fixation in Orthopedic Trauma. Chin. Med. J. 2016, 129, 2521–2523. [Google Scholar]
- Pérez Hernández, F.J.; Goya Arteaga, L.; González Siverio, J.L.; Llada Marrero, R.P. Concordancia diagnóstica entre atención primaria y cirugía menor en una zona básica de salud [Diagnostic agreement of primary care and minor surgery in a basic health area]. Semergen 2021, 47, 144–150. [Google Scholar]
- Aganzo-López, F.J.; Grima-Barbero, J.M.; Marrón-Moya, S.E.; Tomás-Aragonés, L. Correlación clínico-patológica en cirugía menor en un área de salud rural [Correlation between clinical and histological diagnosis in minor surgery in a rural health area]. Semergen 2013, 39, 12–17. [Google Scholar]
- López Santiago, A.; Lara Peñaranda, R.; de Miguel Gómez, A.; Pérez López, P.; Ribes Martínez, E. Cirugía menor en atención primaria: La satisfacción de los usuarios [Minor surgery in primary care: Consumer satisfaction]. Aten. Primaria 2000, 26, 91–95. [Google Scholar]
- Ramírez Arriola, M.G.; Hamido Mohamed, N.; Abad Vivás-Pérez, J.J.; Bretones Alcaráz, J.J.; García Torrecillas, J.M.; Huber, E. Descripción de la concordancia clinicopatológica y satisfacción del paciente en la cirugía menor en un centro de atención primaria [Description of clinical pathological concordance and patient satisfaction in minor surgery in a Primary Care centre]. Aten. Primaria 2017, 49, 86–92. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Vaquero Martínez, J.J.; García Aparicio, J.M.; Díaz Gómez, J.; Blasco Paredes, D. Eficiencia de la cirugía menor en atención primaria según el nivel de facturación [Efficiency of minor surgery in primary care according to the costs]. Aten. Primaria 2002, 30, 86–91. [Google Scholar] [CrossRef]
- Tárraga López, P.J.; Marín Nieto, E.; García Olmo, D.; Celada Rodríguez, A.; Solera Albero, J. Impacto económico de la implantación de un programa de cirugía menor en atención primaria [Economic impact of the introduction of a minor surgery program in primary care]. Aten. Primaria 2001, 27, 335–338. [Google Scholar] [CrossRef]
- Moldovan, F.; Moldovan, L. An Orthopedic Healthcare Facility Governance Assessed with a New Indicator System. Healthcare 2024, 12, 1080. [Google Scholar] [CrossRef] [PubMed]
- ANMCS. Standardele Autoritatii Nationale de Management al Calitatii in Sanatate Pentru Serviciile de Sanatate Acordate in Regim Ambulatoriu (Standards of the National Authority for Quality Management in Health for Outpatient Health Services). Available online: https://anmcs.gov.ro/web/standarde-ambulatoriu/ (accessed on 18 November 2024).
- ANMCS. Standarde de Acreditare Unitatilor Sanitare cu Paturi si Liste de Verificare (Accreditation standards for Sanitary Units with Beds and Checklists). Available online: https://anmcs.gov.ro/web/acreditarea-spitalelor/standarde-de-acreditare/ (accessed on 18 November 2024).
- Groene, O.; Kringos, D.; Sunol, R.; On Behalf of the DUQuE Project. Seven Ways to Improve Quality and Safety in Hospitals. An Evidence-Based Guide. DUQuE Collaboration. 2014. Available online: www.duque.eu (accessed on 18 July 2024).
- Moldovan, F.; Moldovan, L.; Bataga, T. Assessment of Labor Practices in Healthcare Using an Innovatory Framework for Sustainability. Medicina 2023, 59, 796. [Google Scholar] [CrossRef] [PubMed]
- Moldovan, F.; Moldovan, L.; Bataga, T. The Environmental Sustainability Assessment of an Orthopedics Emergency Hospital Supported by a New Innovative Framework. Sustainability 2023, 15, 13402. [Google Scholar] [CrossRef]
- Sodhi, N.; Hameed, D.; Barrack, R.L.; Schneider, A.M.; Bhave, A.; Mont, M.A. Use of Remote Physiologic and Therapeutic Monitoring Following Total Knee Arthroplasty. Surg. Technol. Int. 2023, 42, 321–328. [Google Scholar]
- Rizan, C.; Lillywhite, R.; Reed, M.; Bhutta, M.F. Minimising carbon and financial costs of steam sterilisation and packaging of reusable surgical instruments. Br. J. Surg. 2022, 109, 200–210. [Google Scholar] [CrossRef] [PubMed]
- Wormer, B.A.; Augenstein, V.A.; Carpenter, C.L.; Burton, P.V.; Yokeley, W.T.; Prabhu, A.S.; Harris, B.; Norton, S.; Klima, D.A.; Lincourt, A.E.; et al. The green operating room: Simple changes to reduce cost and our carbon footprint. Am. Surg. 2013, 79, 666–671. [Google Scholar]
- Eckelman, M.; Mosher, M.; Gonzalez, A.; Sherman, J. Comparative life cycle assessment of disposable and reusable laryngeal mask airways. Anesth. Analg. 2012, 114, 1067–1072. [Google Scholar]
- Scott Kruse, C.; Karem, P.; Shifflett, K.; Vegi, L.; Ravi, K.; Brooks, M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J. Telemed. Telecare 2018, 24, 4–12. [Google Scholar] [PubMed]

| Indicator Level | Name of the Indicator Level | Indicator Level Description |
|---|---|---|
| 1 | Local clinics | Setting up local clinics where orthopedic surgeons provide care for musculoskeletal problems and fracture assessments. |
| 2 | Telephone consultations | Surgeons offer consultations by phone call as part of a dedicated service. Smartphone apps are being developed to enable real-time teleconsultations. |
| 3 | Videoconference consultations | In the remote clinic, videoconferencing is used for orthopedic consultations. They are used for inpatients, emergency room patients, outpatient visits, and postoperative care. |
| 4 | Virtual clinic | Telehealth services are expanded by upgrading telehealth equipment and integrating modern technologies. A virtual orthopedic fracture clinic is implemented, and a virtual doctor is employed. |
| 5 | Orthopedic telesurgery | The two major forms of tele-orthopedics are implemented: telemonitoring through teleconsultation and telemetry and telerobotic telesurgery and telementoring. |
| Indicator Level | Name of the Indicator Level | Indicator Level Description |
|---|---|---|
| 1 | Active travel | Behavioral theories that encourage active travel are promoted. Walking and taking the bus are encouraged, and there are bus routes and bus stops in the vicinity of the hospital. |
| 2 | Changing room and shower facilities | Staff lockers are adapted to support active travel. Shower facilities are provided. |
| 3 | Bicycle storage | There are safety features for traveling by bicycle. The hospital operates a bicycle parking lot that is accessible and includes safety features. |
| 4 | Hospital parking | Hospital management engages in traffic management in the congested and increasingly congested areas in the hospital neighborhood. A new intelligent parking management architecture facilitates the relaxation of parking policy. |
| 5 | Car sharing | By increasing public awareness and education, car sharing is promoted as a new mode of transportation. Car-sharing industry, route optimization, and scheduling are developed. |
| Indicator Level | Name of the Indicator Level | Indicator Level Description |
|---|---|---|
| 1 | Surgical patient education | The education of orthopedic surgical patients takes place in the preoperative, surgical, and recovery phases, including with the support of electronic health apps. |
| 2 | eConsent | In clinical care, patient consent is obtained with the support of digital tools. The digital consent system is in a robust data infrastructure. Patient feedback is collected using surveys, which is processed with the support of the data infrastructure. |
| 3 | Shared decision making | Patients are incentivized to get involved in shared decision making. Based on patient feedback, measures to improve medical services are developed and discussed with them. |
| 4 | Minimizing damage to normal tissue | Patients are referred for procedures to minimize injury to normal tissue. Microdecompression techniques are used in procedures performed with small incisions. Minimally invasive decompression of the cervical spine uses the cervical microendoscopic foraminotomy and cervical microendoscopic diskectomy procedures. |
| 5 | Non-technical skills | The organizational system identifies physicians who, in addition to professional skills, have well-developed, non-practical skills, and patients prefer them to perform medical interventions. The degree of patient satisfaction is high. |
| Indicator Level | Name of the Indicator Level | Indicator Level Description |
|---|---|---|
| 1 | Office-based minor surgery | Minor surgical procedures are performed in the outpatient setting and are accredited. Small skin incisions, minimized muscle dissection, improved visibility with endoscopy and fluoroscopy, application of special instruments, and robotic assistance are practiced. |
| 2 | Resident-run minor surgery | Surgical residents independently perform outpatient procedures without jeopardizing patient safety or satisfaction. Biologic osteosynthesis is used in the management of orthopedic trauma. |
| 3 | Diagnostic agreement | In the initial diagnosis of lesions referred for evaluation in primary care, there is a high correlation between the clinical diagnosis and the histologic findings that are obtained with the support of minor surgery. |
| 4 | Patient satisfaction in minor surgery | Patients are satisfied with the minor surgery, the explanations of anatomopathologic concordances in primary care, and the hygiene of the doctor’s office. |
| 5 | Efficiency of minor surgery | In primary care, the minor surgery program has lower costs compared to specialty surgery. The minor surgery program reduces patients’ waiting lists. |
| Level → Indicator ↓ | Level 1 | Level 2 | Level 3 | Level 4 | Level 5 |
|---|---|---|---|---|---|
| Remote consultations in orthopedics (I1) | Local clinics | Telephone consultations | Videoconference consultations | Virtual clinic | Orthopedic telesurgery |
| Incentives for staff travel options (I2) | Active travel | Changing room and shower facilities | Bicycle storage | Hospital parking | Car sharing |
| Involvement of surgical patients (I3) | Surgical patient education | eConsent | Shared decision making | Minimizing damage to normal tissue | Non-technical skills |
| Minor surgical interventions (I4) | Office-based minor surgery | Resident-run minor surgery | Diagnostic agreement | Patient satisfaction | Efficiency of minor surgery |
| No. | Indicator Description | Level (Li) | Importance (Ii) | Sustainability Indicator (Si = Li · Ii) |
|---|---|---|---|---|
| 1 | (I1) Remote consultations in orthopedics | 3 | 3 | 9 |
| 2 | (I2) Incentives for staff travel options | 2 | 4 | 8 |
| 3 | (I3) Involvement of surgical patients | 3 | 2 | 6 |
| 4 | (I4) Minor surgical interventions | 4 | 5 | 20 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moldovan, F.; Moldovan, L. An Innovative Assessment Framework for Remote Care in Orthopedics. Healthcare 2025, 13, 736. https://doi.org/10.3390/healthcare13070736
Moldovan F, Moldovan L. An Innovative Assessment Framework for Remote Care in Orthopedics. Healthcare. 2025; 13(7):736. https://doi.org/10.3390/healthcare13070736
Chicago/Turabian StyleMoldovan, Flaviu, and Liviu Moldovan. 2025. "An Innovative Assessment Framework for Remote Care in Orthopedics" Healthcare 13, no. 7: 736. https://doi.org/10.3390/healthcare13070736
APA StyleMoldovan, F., & Moldovan, L. (2025). An Innovative Assessment Framework for Remote Care in Orthopedics. Healthcare, 13(7), 736. https://doi.org/10.3390/healthcare13070736








