Exploring the Potential Causal Relationship Between Health Insurance Coverage and Child Nutritional Status in Pakistan: Evidence from PDHS-2018
Abstract
1. Introduction
2. Method and Materials
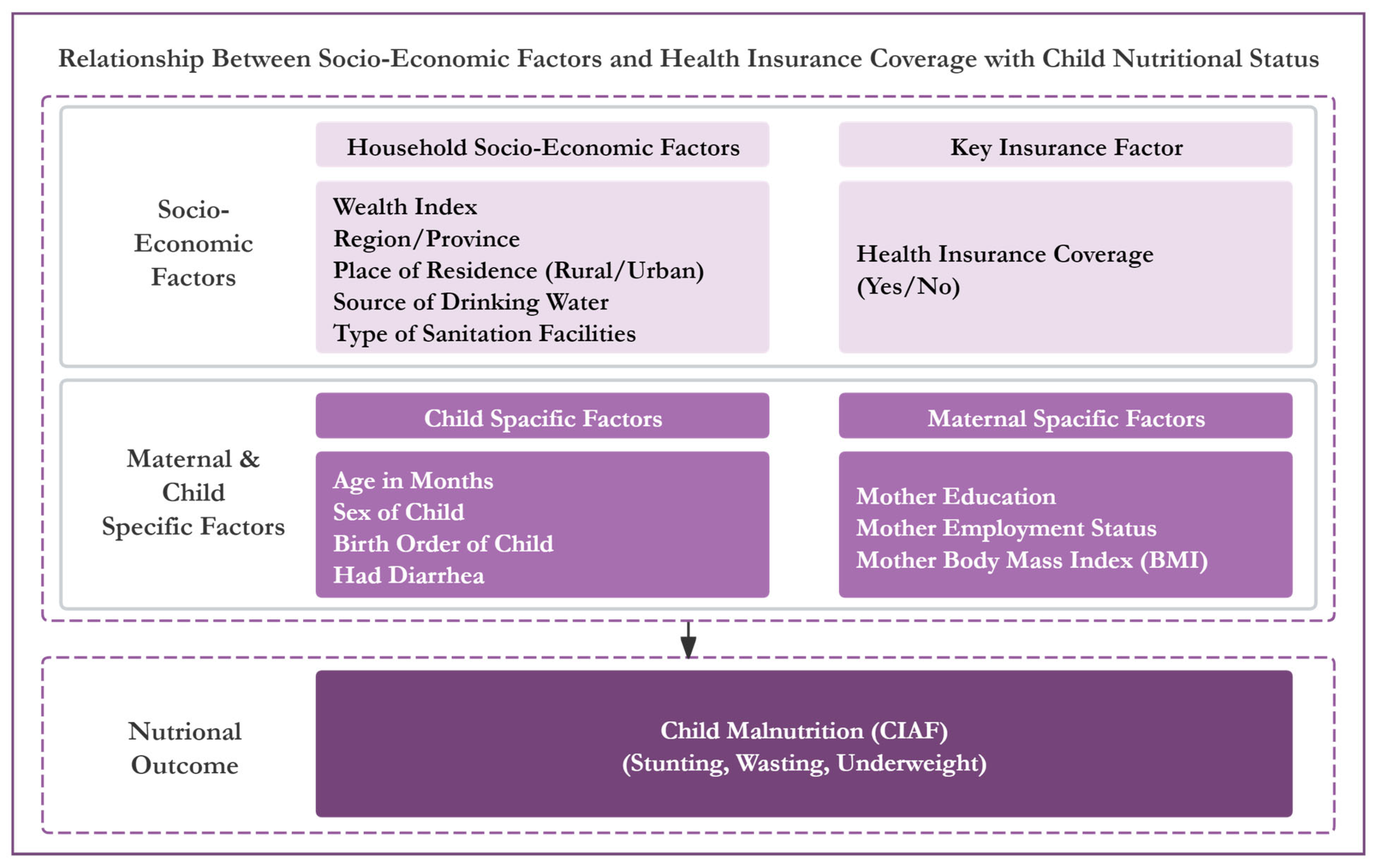
2.1. Theoretical Framework of This Study
2.2. Conceptual Framework
2.3. Main Explanatory Variables
2.4. Dependent Variables
2.5. Description of the Dataset
2.6. Public and Patient Involvement
2.7. Statistical Analysis
3. Results
3.1. The Impact of Covariates on Nutritional Status of Child
3.2. Influence of Covariates on Child Health Insurance Coverage Through Logistic Regression
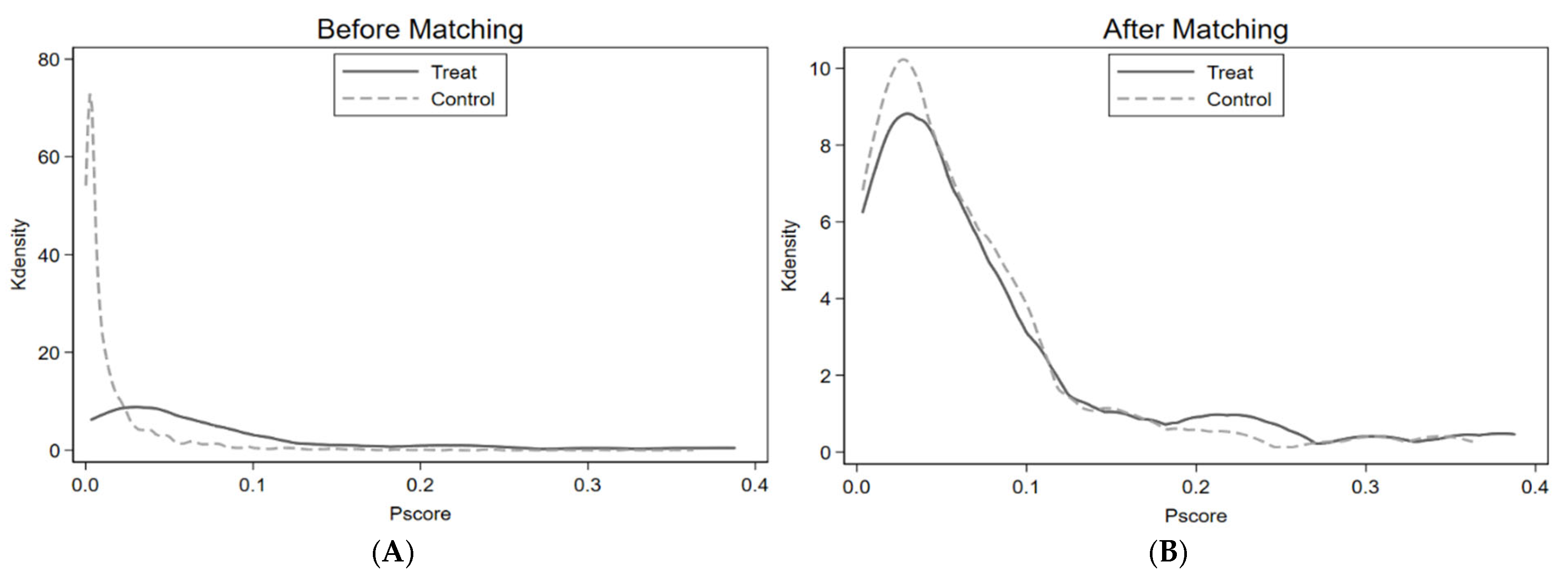
3.3. Common Support Domain
3.4. Balance Test: Nearest Neighborhood Matching
3.5. Before and After Matching Covariate Balance Findings Between Treated and Untreated Groups
3.6. Treatment Effect Estimation/Average Treatment Effect (ATT)
4. Discussion
Strengths and Limitations of the Current Investigation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lucas, R.E. On the mechanics of economic development. J. Monet. Econ. 1988, 22, 3–42. [Google Scholar] [CrossRef]
- Aggarwal, A. Impact evaluation of India’s ‘Yeshasvini’ community-based health insurance program. Health Econ. 2010, 19, 5–35. [Google Scholar] [CrossRef] [PubMed]
- Pfutze, T. The effects of Mexico’s seguro popular health insurance on infant mortality: An estimation with selection on the outcome variable. World Dev. 2014, 59, 475–486. [Google Scholar] [CrossRef]
- Lei, X.; Lin, W. The new cooperative medical scheme in rural China: Does more coverage mean more service and better health? Health Econ. 2009, 18, S25–S46. [Google Scholar] [CrossRef]
- Chen, Y.; Jin, G.Z. Does health insurance coverage lead to better health and educational outcomes? Evidence from rural China. J. Health Econ. 2012, 31, 1–14. [Google Scholar] [CrossRef]
- Dow, W.H.; Schmeer, K.K. Health insurance and child mortality in Costa Rica. Soc. Sci. Med. 2003, 57, 975–986. [Google Scholar] [CrossRef]
- Miller, S.; Wherry, L.R. Health and access to care during the first 2 years of the ACA medicaid expansions. N. Engl. J. Med. 2017, 376, 947–956. [Google Scholar] [CrossRef]
- Courtemanche, C.; Marton, J.; Ukert, B.; Yelowitz, A.; Zapata, D. Early effects of the Affordable Care Act on health care access, risky health behaviors, and self-assessed health. South. Econ. J. 2018, 84, 660–691. [Google Scholar] [CrossRef]
- The Frontier Post. 2018. Available online: https://www.finance.gov.pk/survey/chapters_19/11-Health%20and%20Nutrition.pdf (accessed on 14 June 2022).
- Onah, S.; Osuorah, D.I.C.; Ebenebe, J.; Ezechukwu, C.; Ekwochi, U.; Ndukwu, I. Infant feeding practices and maternal socio-demographic factors that influence practice of exclusive breastfeeding among mothers in Nnewi southeast Nigeria: A cross-sectional and analytical study. Int. Breastfeed. J. 2014, 9, 6. [Google Scholar] [CrossRef]
- Tappis, H.; Kazi, A.; Hameed, W.; Dahar, Z.; Ali, A.; Agha, S. The role of quality health services and discussion about birth spacing in postpartum contraceptive use in Sindh, Pakistan: A multilevel analysis. PLoS ONE 2015, 10, e0139628. [Google Scholar] [CrossRef]
- Turner, J. Healthy, wealthy, and wise. Science 1958, 128, 443. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Roseboom, T.; de Rooij, S.; Painter, R. The Dutch famine and its long-term consequences for adult health. Early Hum. Dev. 2006, 82, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Elder, L.K.; Kataoka, N.; Naudeau, S.; Neuman, M.J.; Valerio, A. Investing in Young Children: An Early Childhood Development Guide for Policy Dialogue and Project Preparation. 2011. Available online: http://documents.worldbank.org/curated/en/2011/01/16283743/investing-young-children-early-childhood-developmentguide-policy-dialogue-project-preparation (accessed on 12 June 2022).
- Ampaabeng, S.K.; Tan, C.M. The long-term cognitive consequences of early childhood malnutrition: The case of famine in Ghana. J. Health Econ. 2013, 32, 1013–1027. [Google Scholar] [CrossRef] [PubMed]
- Aziz, N.; Liu, T.; Yang, S.; Zukiewicz-Sobczak, W. Causal relationship between health insurance and overall health status of children: Insights from Pakistan. Front. Public Health 2022, 10, 934007. [Google Scholar] [CrossRef]
- Nichols, A. Causal inference with observational data. Stata J. 2007, 7, 507–541. [Google Scholar] [CrossRef]
- Berk, R.A. An introduction to sample selection bias in sociological data. Am. Sociol. Rev. 1983, 48, 386–398. [Google Scholar] [CrossRef]
- Trujillo, A.J.; Portillo, J.E.; Vernon, J.A. The impact of subsidized health insurance for the poor: Evaluating the Colombian experience using propensity score matching. Int. J. Health Care Financ. Econ. 2005, 5, 211–239. [Google Scholar] [CrossRef]
- Hadley, J. Sicker and poorer—The consequences of being uninsured: A review of the research on the relationship between health insurance, medical care use, health, work, and income. Med. Care Res. Rev. 2003, 60, 3S–75S. [Google Scholar] [CrossRef]
- Dhruv, K.; Chokshi, D.A. Health, income, & poverty: Where we are & what could help. Health Aff. 2018, 10, 1–6. [Google Scholar] [CrossRef]
- Brooks-Gunn, J.; Klebanov, P.; Liaw, F.R.; Duncan, G. Toward an understanding of the effects of poverty upon children. In Children of Poverty; Routledge: Oxfordshire, UK, 2021; pp. 3–41. Available online: https://www.taylorfrancis.com/chapters/edit/10.4324/9781315861623-2/toward-understanding-effects-poverty-upon-children-jeanne-brooks-gunn-pamela-klebanov-fong-ruey-liaw-greg-duncan (accessed on 1 May 2023).
- Cederholm, T.; Jensen, G.L.; Correia, M.I.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.J.; et al. GLIM criteria for the diagnosis of malnutrition–A consensus report from the global clinical nutrition community. J. Cachexia Sarc. Muscle 2019, 10, 207–217. [Google Scholar] [CrossRef]
- Ahmed, T.; Hossain, M.; Sanin, K.I. Global burden of maternal and child undernutrition and micronutrient deficiencies. Ann. Nutr. Metab. 2013, 61, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Müller, O.; Krawinkel, M. Malnutrition and health in developing countries. Can. Med. Assoc. J. 2005, 173, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.Q.; Li, H.; Wu, H.H.; Zong, X.N. Stunting, wasting, overweight and their coexistence among children under 7 years in the context of the social rapidly developing: Findings from a population-based survey in nine cities of China in 2016. PLoS ONE 2021, 16, e0245455. [Google Scholar] [CrossRef] [PubMed]
- Wali, N.; Agho, K.; Renzaho, A.M.N. Past drivers of and priorities for child undernutrition in South Asia: A mixed methods systematic review protocol. Syst. Rev. 2019, 8, 189. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, S. Malnutrition in South Asia—A critical reappraisal. Crit. Rev. Food Sci. 2016, 56, 2320–2330. [Google Scholar] [CrossRef]
- World Health Organization. Nutrition Landscape Information System (NLIS) Country Profile Indicators: Interpretation Guide; World Health Organization: Geneva, Switzerland, 2019; Available online: https://www.who.int/publications/i/item/9789241516952 (accessed on 30 November 2021).
- McDonald, C.M.; Olofin, I.; Flaxman, S.; Fawzi, W.W.; Spiegelman, D.; Caulfield, L.E.; Black, R.E.; Ezzati, M.; Danaei, G. Nutrition Impact Model Study. The effect of multiple anthropometric deficits on child mortality: Meta-analysis of individual data in 10 prospective studies from developing countries. Am. J. Clin. Nutr. 2013, 97, 896–901. [Google Scholar] [CrossRef]
- Becker, G.S. A Theory of the Allocation of Time. Econ. J. 1965, 75, 493–517. [Google Scholar] [CrossRef]
- Strauss, J.; Thomas, D. Human Resources: Empirical Modeling of Household and Family Decisions. In Handbook of Development Economics; Behrman, J.B., Srinivasan, T.N., Eds.; Elsevier: Amsterdam, The Netherlands, 1995; Volume 3. [Google Scholar] [CrossRef]
- Dehejia, R.; Wahba, S. Propensity score-matching methods for non-experimental causal studies. Rev. Econ. Stat. 2002, 84, 151–161. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Child Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children: A Joint Statement by the World Health Organization and the United Nations Children’s Fund; World Health Organization: Geneva, Switzerland, 2009; Available online: https://apps.who.int/iris/bitstream/handle/10665/44129/9789241598163_eng.pdf?sequence=1&isAllowed=y (accessed on 2 May 2020).
- Caliendo, M.; Kopeinig, S. Some practical guidance for the implementation of propensity score matching. J. Econ. Surv. 2008, 22, 3172. [Google Scholar] [CrossRef]
- Abbay, A.G.; Rutten, R. Does spatial proximity to small towns matter for rural livelihoods? A propensity score matching analysis in Ethiopia. Lett. Spat. Resour. Sci. 2016, 9, 287–307. [Google Scholar] [CrossRef]
- Stuart, E.A. Matching methods for causal inference: A review and a look forward. Stat. Sci. 2010, 25, 1–21. [Google Scholar] [CrossRef]
- Das, S.; Rahman, R.M. Application of ordinal logistic regression analysis in determining risk factors of child malnutrition in Bangladesh. Nutr. J. 2011, 10, 124. [Google Scholar] [CrossRef] [PubMed]
- Shahid, M.; Liu, Y.; Ameer, W.; Qureshi, M.G.; Ahmed, F.; Tang, K. Comparison of Different Nutritional Screening Approaches and the Determinants of Malnutrition in Under-Five Children in a Marginalized District of Punjab Province, Pakistan. Children 2022, 9, 1096. [Google Scholar] [CrossRef] [PubMed]
- Yu, T.; Chen, C.; Jin, Z.; Yang, Y.; Jiang, Y.; Hong, L.; Yu, X.; Mei, H.; Jiang, F.; Huang, H.; et al. Association of number of siblings, birth order, and thinness in 3-to 12-year-old children: A population-based cross-sectional study in Shanghai, China. BMC Pediatr. 2020, 20, 367. [Google Scholar] [CrossRef]
- Singh, A.; Arokiasamy, P.; Pradhan, J.; Jain, K.; Patel, S.K. Sibling- and family-level clustering of underweight children in northern India. J. Biosoc. Sci. 2017, 49, 348–363. [Google Scholar] [CrossRef]
- Shahid, M.; Cao, Y.; Shahzad, M.; Saheed, R.; Rauf, U.; Qureshi, M.G.; Hasnat, A.; Bibi, A.; Ahmed, F. Socio-Economic and Environmental Determinants of Malnutrition in under Three Children: Evidence from PDHS-2018. Children 2022, 9, 361. [Google Scholar] [CrossRef]
- Shahid, M.; Saheed, R.; Wang, J.; Qureshi, M.G.; Sun, X.; Bibi, A.; Zia, S.; Tang, K. Impact of Drinking Water Source and Sanitation Facility on Malnutrition Prevalence in Children under Three: A Gender-Disaggregated Analysis Using PDHS 2017–18. Children 2022, 9, 1674. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, M.; Lumbert, J. Women and nutrition: Reflection from India and Pakistan. Food Nutr. Bull. 1989, 11, 90. [Google Scholar] [CrossRef]
- Khaliq, A.; Wraith, D.; Miller, Y.; Nambiar-Mann, S. Prevalence, Trends, and Socioeconomic Determinants of Coexisting Forms of Malnutrition Amongst Children under Five Years of Age in Pakistan. Nutrients 2021, 13, 4566. [Google Scholar] [CrossRef]
- Fentaw, R.; Bogale, A.; Abebaw, D. Prevalence of child malnutrition in agro-pastoral households in Afar Regional State of Ethiopia. Nutr. Res. Pract. 2013, 7, 122–131. [Google Scholar] [CrossRef]
- Fotso, J.-C. Urban–rural differentials in child malnutrition: Trends and socioeconomic correlates in sub-Saharan Africa. Health Place. 2007, 13, 205–223. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, C.S.; Zanello, G.; Shankar, B. Rural-urban disparities in child nutrition in Bangladesh and Nepal. BMC Public Health 2013, 13, 581. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, F.; Malik, N.I.; Shahzad, M.; Ahmad, M.; Shahid, M.; Feng, X.L.; Guo, J. Determinants of Infant Young Child Feeding Among Mothers of Malnourished Children in South Punjab, Pakistan: A Qualitative Study. Front. Public Health 2022, 10, 834089. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, F.; Malik, N.I.; Malik, N.; Qureshi, M.G.; Shahzad, M.; Shahid, M.; Zia, S.; Tang, K. Key Challenges to Optimal Therapeutic Coverage and Maternal Utilization of CMAM Program in Rural Southern Pakistan: A Qualitative Exploratory Study. Nutrients 2022, 14, 2612. [Google Scholar] [CrossRef]
- Shafiq, A.; Hussain, A.; Asif, M.; Hwang, J.; Jameel, A.; Kanwel, S. The effect of “women’s empowerment” on child nutritional status in Pakistan. Int. J. Environ. Res. Public Health 2019, 16, 4499. [Google Scholar] [CrossRef]
- Nair, M.; Ohuma, E.; Ariana, P.; Webster, P.; Gray, R. Effect of the Mahatma Gandhi national rural employment guarantee act on malnutrition of children aged between 1 and 12 months in Rajasthan, India: A mixed methods study. Lancet 2012, 380, S9. [Google Scholar] [CrossRef]
- Alam, M.B.; Shahid, M.; Alzghoul, B.I.; Yang, J.; Zakar, R.; Malik, N.I.; Bibi, A.; Tang, K. The Effects of Financial Stress and Household Socio-Economic Deprivation on the Malnutrition Statuses of Children Under Five during the COVID-19 Lockdown in a Marginalized Region of South Punjab, Pakistan. Children 2023, 10, 12. [Google Scholar] [CrossRef]
- Khan, E.A.; Raza, M.A. Nutritional status of children in Bangladesh: Measuring composite index of anthropometric failure (CIAF) and its determinants. Pak. J. Commer. Soc. Sci. 2014, 8, 11–23. [Google Scholar]
- Shahid, M.; Ahmed, F.; Ameer, W.; Guo, J.; Raza, S.; Fatima, S.; Qureshi, G.M. Prevalence of child malnutrition and household socioeconomic deprivation: A case study of marginalized district in Punjab, Pakistan. PLoS ONE 2022, 17, e0263470. [Google Scholar] [CrossRef]
- Srinivasan, K.; Mohanty, S.K. Household deprivation and its linkages with reproductive health utilisation. Econ. Political Wkly. 2008, 43, 67–76. [Google Scholar] [CrossRef]
- Panda, B.K.; Mohanty, S.K.; Nayak, I.; Shastri, V.D.; Subramanian, S.V. Malnutrition and poverty in India: Does the use of public distribution system matter? BMC Nutr. 2020, 6, 41. [Google Scholar] [CrossRef] [PubMed]
- Nyman, J.A. The value of health insurance: The access motive. J. Health Econ. 1999, 18, 141–152. [Google Scholar] [CrossRef] [PubMed]
- McPake, B.; Edoka, I.; Witter, S.; Kielmann, K.; Taegtmeyer, M.; Dieleman, M.; Vaughan, K.; Gama, E.; Kok, M.; Datiko, D.; et al. Cost-effectiveness of community-based practitioner programes in Ethiopia, Indonesia and Kenya. Bull. World Health Organ. 2015, 93, 631–639. [Google Scholar] [CrossRef] [PubMed]
- Cahyadi, N.; Hanna, R.; Olken, B.A.; Prima, R.A.; Satriawan, E.; Syamsulhakim, E. Cumulative impacts of conditional cash transfer programs: Experimental evidence from Indonesia. Am. Econ. J. Econ. Policy 2020, 12, 88–110. [Google Scholar] [CrossRef]
- Joyce, T.; Racine, A. CHIP shots: Association between the state children’s health insurance programs and immunization rates. Pediatrics. 2005, 115, e526–e534. [Google Scholar] [CrossRef]
- Brooks, M.I.; Thabrany, H.; Fox, M.P.; Wirtz, V.J.; Feeley, F.G.; Sabin, L.L. Health facility and skilled birth deliveries among poor women with Jamkesmas health insurance in Indonesia: A mixed-methods study. BMC Health Serv. Res. 2017, 17, 105. [Google Scholar] [CrossRef]
- Nababan, H.Y.; Hasan, M.; Marthias, T.; Dhital, R.; Rahman, A.; Anwar, I. Trends and inequities in use of maternal health care services in Indonesia, 1986–2012. Int. J. Womens Health 2018, 10, 11–24. [Google Scholar] [CrossRef]
- Wang, W.; Temsah, G.; Mallick, L. The impact of health insurance on maternal health care utilization: Evidence from Ghana, Indonesia and Rwanda. Health Policy Plan. 2017, 32, 366–375. [Google Scholar] [CrossRef]
- Herman, B.; Pongpanich, S.; Viwattanakulvanid, P. National health insurance impact on malnutrition in under-five years old children in Indonesia. Eur. J. Public Health 2020, 30, 166–1392. [Google Scholar] [CrossRef]
- Nshakira-Rukundo, E.; Mussa, E.C.; Gerber, N.; von Braun, J. Impact of voluntary community-based health insurance on child stunting: Evidence from rural Uganda. Soc. Sci. Med. 2020, 245, 112738. [Google Scholar] [CrossRef]
- Levere, M.; Orzol, S.; Leininger, L.; Early, N. Contemporaneous and long-term effects of children’s public health insurance expansions on supplemental security income participation. J. Health Econ. 2019, 64, 80–92. [Google Scholar] [CrossRef] [PubMed]
- Hen, L.; Chu, L. Does health insurance coverage lead to better child health? Evidence from China. China Popul. Dev. Stud. 2019, 3, 1–23. [Google Scholar] [CrossRef]
- Hou, B.; Wu, Y.; Huang, S. Participating in health insurance and health improvements for the relatively poor population: A propensity score analysis. Front. Public Health 2022, 10, 968009. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Xing, J.; Yang, X.; Zhan, K. Heterogeneous Effects of Health Insurance on Rural Children’s Health in China: A Causal Machine Learning Approach. Int. J. Environ. Res. Public Health 2021, 18, 9616. [Google Scholar] [CrossRef]
- Sarpong, S.; Achille, D.F. Health Insurance and Child Health Outcomes in West Africa. Int. J. Sci. Res. 2018, 8, 329–332. [Google Scholar] [CrossRef]
- Ekhator-Mobayode, U.E.; Gajanan, S.; Ekhator, C. Does Health Insurance Eligibility Improve Child Health: Evidence from the National Health Insurance Scheme (NHIS) in Nigeria. Cureus 2022, 14, e28660. [Google Scholar] [CrossRef]
- Kofinti; Raymond, E.; Isaac, K.; Jones, A.P.; Edward, K.A. Reducing children’s malnutrition by increasing mothers’ health insurance coverage: A focus on stunting and underweight across 32 sub-Saharan African countries. Econ. Model. 2022, 117, 106049. [Google Scholar] [CrossRef]
| Variable | Frequency | Percentage | p-Value |
|---|---|---|---|
| Sex of Child | |||
| Female | 887 | 21.66% | 0.67 |
| Male | 921 | 22.49% | |
| Child Age in Months | |||
| 0–12 Months | 284 | 6.94% | p < 0.001 |
| 13–24 Months | 325 | 7.94% | |
| 25–36 Months | 423 | 10.33% | |
| 37–48 Months | 427 | 10.43% | |
| 48–60 Months | 349 | 8.52% | |
| Child Birth Order Number | |||
| ≤2 Years | 766 | 18.71% | p < 0.001 |
| 3–4 Years | 548 | 13.38% | |
| 5–7 Years | 378 | 9.23% | |
| Greater than 7 Years | 116 | 2.83% | |
| Child Had Diarrhea Recently | |||
| No | 1435 | 35.04% | p < 0.01 |
| Yes | 373 | 9.11% | |
| Place of Residence | |||
| Rural | 1074 | 26.23% | p < 0.001 |
| Urban | 734 | 17.92% | |
| Region | |||
| Punjab | 297 | 7.25% | p < 0.001 |
| Sindh | 416 | 10.16% | |
| KPK | 288 | 7.03% | |
| Balochistan | 305 | 7.45% | |
| FATA | 189 | 4.62% | |
| Gilgit Baltistan | 108 | 2.64% | |
| Islamabad Capital | 63 | 1.54% | |
| Azad Jammu and Kashmir | 142 | 3.47% | |
| Source of Drinking Water | |||
| Unimproved | 1430 | 34.92% | p < 0.001 |
| Improved | 378 | 9.23% | |
| Form of Sanitation Facility | |||
| Unimproved | 1284 | 31.36% | p < 0.001 |
| Improved | 524 | 12.80% | |
| Mother’s Body Mass Index | |||
| Less than 18.5 kg/m2 or Underweight | 181 | 39.62% | p < 0.001 |
| ≥18.5 kg/m2 or Normal | 1615 | 4.44% | |
| Mother’s Education | |||
| Illiterate | 1146 | 27.99% | p < 0.001 |
| Primary | 234 | 5.71% | |
| Secondary | 290 | 7.08% | |
| Higher | 138 | 3.37% | |
| Womens’ Working Status | |||
| Not working | 1579 | 38.58% | p < 0.001 |
| Working | 229 | 5.59% | |
| Household Wealth Index/Status | |||
| Poorest | 550 | 13.43% | p < 0.001 |
| Poorer | 507 | 12.38% | |
| Middle | 324 | 7.91% | |
| Richer | 254 | 6.20% | |
| Richest | 173 | 4.22% | |
| Household Health Insurance Coverage | |||
| Not Insured | 1588 | 43.64% | p < 0.001 |
| Insured | 220 | 5.0% | |
| Variables | Odds Ratios (p-Value) | 95% Confidence Intervals |
|---|---|---|
| Biological Sex of Child | ||
| Female (as a Reference Category) | 1 | - |
| Male | 1.046 (0.49) | 0.92–1.19 |
| Child Age in Months | ||
| 0–12 Months (Reference Category) | 1 | - |
| 13–24 Months | 1.58 (0.00) *** | 1.29–1.94 |
| 25–36 Months | 2.37 (0.00) *** | 1.94–2.89 |
| 37–48 Months | 2.32 (0.00) *** | 1.89–2.83 |
| 48–60 Months | 1.93 (0.00) *** | 1.56–2.36 |
| Child Birth Order Number | ||
| ≤2 Years (Reference Category) | 1 | - |
| 3–4 Years | 1.21 (0.01) *** | 1.04–1.40 |
| 5–7 Years | 1.32 (0.002) *** | 1.10–1.57 |
| Greater than 7 Years | 1.36 (0.04) ** | 1.01–1.82 |
| Residence Type | ||
| Rural (Reference Category) | 1 | - |
| Urban | 0.79 (0.001) *** | 0.69–0.91 |
| Region | ||
| Punjab (Reference Category) | 1 | - |
| Sindh | 2.05 (0.000) *** | 1.65–2.54 |
| KPK | 1.29 (0.03) ** | 1.03–1.61 |
| Balochistan | 2.52 (0.000) *** | 1.95–3.26 |
| FATA | 1.53 (0.003) *** | 1.16–2.02 |
| Gilgit Baltistan | 1.02 (0.88) | 0.76–1.38 |
| Islamabad Capital | 0.97 (0.87) | 0.69–1.37 |
| Azad Jammu and Kashmir | 0.90 (0.45) | 0.69–1.18 |
| Mother’s Body Mass Index | ||
| Less than 18.5 kg/m2 or Underweight (Reference Category) | 1 | - |
| ≥18.5 kg/m2 or Normal | 0.78 (0.04) ** | 0.62–0.98 |
| Child Had Diarrhea Recently | ||
| No (Reference Category) | 1 | - |
| Yes | 1.26 (0.008) *** | 1.06–1.49 |
| Drinking Water Source | ||
| Unimproved (Reference Category) | 1 | - |
| Improved | 0.79 (0.01) *** | 0.66–0.95 |
| Sanitation Facility Type | ||
| Unimproved (Reference Category) | 1 | - |
| Improved | 0.59 (0.000) *** | 0.52–0.70 |
| Mother’s Education | ||
| Illiterate (Reference Category) | 1 | - |
| Primary | 0.84 (0.11) | 0.68–1.04 |
| Secondary | 0.75 (0.006) *** | 0.61–0.91 |
| Higher | 0.51 (0.000) *** | 0.39–0.66 |
| Womens’ Working Status | ||
| Not Working (Reference Category) | 1 | - |
| Working | 1.28 (0.01) *** | 1.045–1.58 |
| Household Wealth Index | ||
| Poorest (Reference Category) | 1 | - |
| Poorer | 0.92 (0.48) | 0.52–1.65 |
| Middle | 0.53 (0.000) *** | 0.42–0.67 |
| Richer | 0.41 (0.000) *** | 0.32–0.53 |
| Richest | 0.31 (0.000) *** | 0.23–0.41 |
| Health Insurance Coverage | ||
| Not Insured (Reference Category) | 1 | - |
| Insured | 0.18 (0.002) *** | 0.06–0.55 |
| Overall Model Significance | ||
| Number of Total Observations = 4074 | Prob > Chi2 = 0.0000 | |
| LR Chi2 (29) = 576.25 | Pseudo R2 = 0.1031 | |
| Indicators | Odds Ratios (p-Value) | 95% Confidence Intervals |
|---|---|---|
| Gender of Child | 1.283 (0.34) | 0.77–2.13 |
| Age of Child | 1.127 (0.21) | 0.94–1.36 |
| Child Birth Order Number | ||
| ≤2 Years (Reference Category) | 1 | - |
| 3–4 Years | 0.58 (0.15) | 0.85–0.96 |
| 5–7 Years | 3.58 (0.001) *** | 1.74–7.38 |
| Greater than 7 Years | 5.79 (0.001) *** | 1.99–16.8 |
| Place of Residence | ||
| Urban (Reference Category) | 1 | - |
| Rural | 0.94 (0.001) *** | 0.53–0.69 |
| Region | ||
| Punjab (Reference Category) | 1 | - |
| Sindh | 0.27 (0.098) ** | 0.55–1.28 |
| Balochistan | 0.28 (0.02) ** | 0.03–2.22 |
| KPK | 4.37 (0.000) *** | 1.93–9.92 |
| Islamabad Capital | 2.58 (0.07) ** | 1.91–7.31 |
| Azad Jammu and Kashmir | 2.05 (0.15) | 0.76–5.55 |
| Gilgit Baltistan | 8.64 (0.000) *** | 3.58–20.8 |
| Mother’s Body Mass Index | ||
| ≥18.5 kg/m2 or Normal (Reference Category) | 1 | - |
| Less than 18.5 kg/m2 or Underweight | 1.02 (0.03) ** | 1.31–3.42 |
| Child Had Diarrhea Recently | ||
| No (Reference Category) | 1 | - |
| Yes | 1.87 (0.007) *** | 1.45–1.73 |
| Child Nutritional Status (CIAF) | ||
| Not Malnourished (Reference Category) | 1 | - |
| Malnourished | 1.98 (0.001) *** | 1.56–1.72 |
| Source of Drinking Water | ||
| Improved (Reference Category) | 1 | - |
| Unimproved | 2.07 (0.02) ** | 1.84–5.13 |
| Type of Sanitation Facility | ||
| Improved (Reference Category) | 1 | - |
| Unimproved | 1.96 (0.01) *** | 1.41–2.26 |
| Mother’s Education | ||
| Illiterate (Reference Category) | 1 | - |
| Primary | 0.53 (0.37) | 0.61–3.90 |
| Secondary | 1.01 (0.98) | 0.39–2.58 |
| Higher | 5.91 (0.000) *** | 2.52–13.9 |
| Womens’ Working Status | ||
| Not Working (Reference Category) | 1 | - |
| Working | 2.01 (0.03) ** | 1.07–3.81 |
| Household Wealth Index | ||
| Poorest (Reference Category) | 1 | - |
| Poorer | 0.58 (0.27) | 0.22–1.53 |
| Middle | 0.94 (0.91) | 0.34–2.64 |
| Richer | 1.06 (0.09) ** | 1.34–3.26 |
| Richest | 1.03 (0.06) ** | 1.31–3.46 |
| Overall Model Significance | ||
| Number of Observed Data = 3741 | Prob > Chi2 = 0.0000 | |
| LR Chi2 (25) = 122.95 | Pseudo R2 = 0.1809 | |
| Samples | Unmatched Sample | Matched Sample | Total |
|---|---|---|---|
| Untreated/Control | 198 | 2650 | 2848 |
| Treated | 3 | 890 | 893 |
| Total | 201 | 3540 | 3741 |
| The Samples/Trials | The Unmatched/Unequal | From Nearest Neighborhood Matching |
|---|---|---|
| Ps R2 | 0.190 | 0.015 |
| LR Chi2 | 129.15 | 21.34 |
| p > Chi2 | 0.000 | 0.724 |
| Mean bias | 21.4 | 10.7 |
| Med bias | 16.5 | 10.2 |
| Variables | Unmatched and Matched | Mean (Treated) | Mean (Control) | Bias Percentage | Reduction Percentage | t-Test Value | p-Value |
|---|---|---|---|---|---|---|---|
| Socio-Economic Variables | |||||||
| Household Wealth | |||||||
| Poorer | Unmatched | 0.161 | 0.239 | −19.3 | 61.9 | −1.48 | 0.138 |
| Matched | 0.161 | 0.191 | −7.4 | −0.45 | 0.656 | ||
| Middle | Unmatched | 0.206 | 0.196 | 2.3 | −215.8 | 0.19 | 0.848 |
| Matched | 0.206 | 0.196 | 7.3 | 0.43 | 0.666 | ||
| Richer | Unmatched | 0.205 | 0.188 | 4.2 | −160.5 | 0.35 | 0.724 |
| Matched | 0.205 | 0.162 | 11.0 | 0.66 | 0.510 | ||
| Richest | Unmatched | 0.294 | 0.183 | 26.2 | 100.0 | 2.34 | 0.019 |
| Matched | 0.294 | 0.294 | 0.0 | 0.00 | 1.000 | ||
| Place of Residence | Unmatched | 0.515 | 0.477 | 7.6 | 100.0 | 0.62 | 0.534 |
| Matched | 0.515 | 0.515 | 0.0 | 0.00 | 1.000 | ||
| Region | Unmatched | 4.029 | 3.219 | 42.3 | 89.1 | 3.35 | 0.001 |
| Matched | 4.029 | 4.117 | −4.6 | −0.28 | 0.778 | ||
| Drinking Water Source | Unmatched | 0.912 | 0.826 | 25.5 | −2.9 | 1.85 | 0.064 |
| Matched | 0.912 | 0.824 | 26.3 | 1.52 | 0.131 | ||
| Type of Sanitation | Unmatched | 0.882 | 0.782 | 27.1 | 85.4 | 2.00 | 0.046 |
| Matched | 0.882 | 0.897 | −4.0 | −0.27 | 0.786 | ||
| Maternal and Child Variables | |||||||
| Gender | Unmatched | 0.573 | 0.509 | 13.0 | 77.3 | 1.06 | 0.291 |
| Matched | 0.573 | 0.589 | −2.9 | −0.17 | 0.863 | ||
| Age | Unmatched | 3.147 | 2.929 | 15.5 | −55.7 | 1.26 | 0.209 |
| Matched | 3.147 | 3.485 | −24.2 | −1.43 | 0.156 | ||
| Birth Order | Unmatched | 2.059 | 1.818 | 25.3 | 26.6 | 2.16 | 0.031 |
| Matched | 2.059 | 1.882 | 18.6 | 1.05 | 0.296 | ||
| Mother’s BMI | Unmatched | 0.956 | 0.909 | 18.5 | −58.9 | 1.32 | 0.186 |
| Matched | 0.956 | 0.882 | 29.4 | 1.58 | 0.118 | ||
| Mother’s Education | |||||||
| Primary | Unmatched | 0.103 | 0.143 | −12.3 | 27.4 | −0.95 | 0.344 |
| Matched | 0.103 | 0.132 | −8.9 | −0.53 | 0.598 | ||
| G1 Secondary | Unmatched | 0.118 | 0.224 | −28.4 | 58.4 | −2.09 | 0.037 |
| Matched | 0.118 | 0.074 | 11.8 | 0.87 | 0.385 | ||
| Higher | Unmatched | 0.455 | 0.152 | 69.8 | 100.0 | 6.87 | 0.000 |
| Matched | 0.455 | 0.456 | 0.0 | −0.00 | 1.000 | ||
| Mother’s Employment | Unmatched | 0.235 | 0.119 | 30.5 | 11.1 | 2.90 | 0.004 |
| Matched | 0.235 | 0.338 | −27.1 | −1.33 | 0.187 | ||
| Disease Related Variable | |||||||
| Child Had Diarrhea | Unmatched | 0.162 | 0.188 | −7.1 | 100.0 | −0.56 | 0.574 |
| Matched | 0.162 | 0.162 | 0.0 | −0.00 | 1.000 | ||
| The Sample/Trials | Unmatched/Unequal | ATT |
|---|---|---|
| Treatment | 0.3235 | 0.3236 |
| Controled | 0.4324 | 0.2868 |
| Differences | −0.1088 | 0.0367 *** |
| Standard (SD) error | 0.0606 | 0.0823 |
| T-test value | −1.80 | 0.45 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shahid, M.; Ali, Z.; Khan, S.; Yousaf, M.S.; Zhang, Z.; Song, J. Exploring the Potential Causal Relationship Between Health Insurance Coverage and Child Nutritional Status in Pakistan: Evidence from PDHS-2018. Healthcare 2025, 13, 532. https://doi.org/10.3390/healthcare13050532
Shahid M, Ali Z, Khan S, Yousaf MS, Zhang Z, Song J. Exploring the Potential Causal Relationship Between Health Insurance Coverage and Child Nutritional Status in Pakistan: Evidence from PDHS-2018. Healthcare. 2025; 13(5):532. https://doi.org/10.3390/healthcare13050532
Chicago/Turabian StyleShahid, Muhammad, Zaiba Ali, Subuhi Khan, Muhammad Shahzad Yousaf, Zhe Zhang, and Jiayi Song. 2025. "Exploring the Potential Causal Relationship Between Health Insurance Coverage and Child Nutritional Status in Pakistan: Evidence from PDHS-2018" Healthcare 13, no. 5: 532. https://doi.org/10.3390/healthcare13050532
APA StyleShahid, M., Ali, Z., Khan, S., Yousaf, M. S., Zhang, Z., & Song, J. (2025). Exploring the Potential Causal Relationship Between Health Insurance Coverage and Child Nutritional Status in Pakistan: Evidence from PDHS-2018. Healthcare, 13(5), 532. https://doi.org/10.3390/healthcare13050532







