Abstract
Background: Non-communicable diseases (NCDs) represent a leading cause of global mortality, demanding innovative approaches to management. Voice assistants (VAs) have emerged as promising tools in healthcare, offering support for self-management, behavioral engagement, and patient care. This systematic review evaluates the role of VAs in NCD management, analyzing their impact on clinical and behavioral outcomes, quality of life, usability, and user experiences while identifying barriers to their adoption. Methods: A systematic search was conducted in PubMed, Scopus, and Web of Science from January 2014 to October 2024. Studies were selected based on predefined inclusion and exclusion criteria using the PRISMA guidelines. Data extraction focused on outcomes such as usability, acceptability, adherence, clinical metrics, and quality of life. The risk of bias was assessed using the Cochrane Risk of Bias (RoB) 2 and ROBINS-I tools. Results: Eight studies involving 541 participants were included, examining VAs across various NCD contexts such as diabetes, cardiovascular diseases, and mental health. While VAs demonstrated good usability and moderate adherence, their clinical and quality-of-life outcomes were modest. Behavioral improvements, such as increased physical activity and problem-solving skills, were noted in some interventions. Key challenges included privacy concerns, speech recognition errors, and accessibility issues. Conclusions: VAs show potential as supportive tools in NCD management, especially for enhancing patient engagement and self-management, and their impact on clinical outcomes and long-term usability requires further investigation. Future research should focus on diverse populations, standardized metrics, and comparative studies with alternative technologies.
1. Introduction
Noncommunicable diseases (NCDs) are responsible for 41 million deaths annually, representing 74% of global mortality [1]. Each year, the deaths related to NCDs account for 17 million before the age of 70, and 86% occur in low- and middle-income countries [1,2]. Cardiovascular diseases are associated with the highest number of deaths among NCDs, amounting to 17.9 million deaths annually, followed by cancers (9.3 million), chronic respiratory diseases (4.1 million), and diabetes (2 million, including kidney disease linked to diabetes) [1,2]. Together, these four diseases account for over 80% of premature deaths caused by NCDs. Risk factors such as tobacco use, physical inactivity, harmful alcohol consumption, unhealthy diets, and air pollution significantly increase the risk of NCD-related deaths [3,4]. Addressing NCDs requires a comprehensive approach that includes early detection, screening, treatment, and palliative care. In light of these considerations, both the healthcare system and patients have begun to benefit from emerging technologies, including voice assistants, particularly in telemedicine and telerehabilitation [5,6] Voice assistant (VAs) gained popularity in commerce due to their usability; in fact, digital voice assistants have become an essential part of everyday life [7]. By 2018, 15.4% of the United States population and 5.9% of the German population owned an Amazon Echo, reflecting the rapid adoption of voice assistants in private households, with smart home purchases increasing by 116% in the third quarter of 2018 compared to the previous year [8].
Beyond commercial applications, VAs have emerged as valuable tools in healthcare providing real-time medication reminders, virtual care, and e-monitoring, enhancing patient engagement and self-management [9]. Studies have demonstrated the reliability of commercial VAs, such as Amazon Alexa, Apple Siri, and Google Assistant, in responding to health-related queries pertinent to NCD management. These VAs can provide accurate information, supporting patients in making informed health decisions, and can be utilized to augment health service delivery, particularly during times when traditional healthcare access may be limited [10,11].
VAs are part of a broader category of conversational agents (CAs), which include artificial intelligence-driven chatbots capable of engaging in dynamic and interactive conversations. Unlike VAs, which primarily rely on voice commands and responses, CAs can incorporate text-based interactions and more advanced dialogue management to provide tailored healthcare support [5,12]. These technologies have gained significant attention in healthcare, supporting telemedicine, self-management of chronic diseases, and mental health interventions [13,14]. Integrating VAs and CAs into healthcare systems has the potential to enhance patient engagement, improve access to health information, and support behavioral change strategies, especially for individuals with NCDs [15].
Elderly individuals frequently face isolation, anxiety, and a feeling of helplessness, both in their homes and in care facilities, which can have a substantial effect on their physical and mental well-being [16]. Speech-based assistants can serve as a valuable tool for individuals who struggle to use other technology-driven services requiring manual dexterity, mobility, or good vision [17]. These systems have the potential to improve the independence of individuals with chronic conditions and enhance their quality of life (QoL), even in the presence of physical or cognitive impairments [18,19]. The aim of this systematic review is to explore the integration of VAs in healthcare, particularly their use in managing NCDs. By analyzing evidence from the included studies, this review aims to assess the impact of VAs on clinical and behavioral outcomes, quality of life, and user experiences, identifying the benefits and challenges associated with their adoption, including usability, acceptability, and readiness to use these technologies. Furthermore, this review provides insights into how VAs contribute to enhancing patient engagement, supporting self-management practices, and addressing broader healthcare needs across different populations.
2. Materials and Methods
2.1. Study Protocol
This systematic review was performed according to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) statement [20]; before starting the literature search and data analysis, the related study protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database of systematic review (identification number: CRD42024604358).
The search strategy, research question, and study selection criteria were designed using the PICO model, with the research question framed as follows [21]:
- Population (P): Subjects with NCDs;
- Intervention (I): Voice Assistants for healthcare support;
- Comparison (C): Digital Twins/Avatars or Textual Chatbots for healthcare support;
- Outcome (O): Outcomes related to QoL, Cost–benefit, Rehospitalizations, Adherence, Accessibility, and any healthcare outcome measures.
2.2. Search Strategy and Study Selection
A literature search was conducted by three reviewers (AB, Massimo Giordano, Marina Garofano) independently, across PubMed/MEDLINE, Scopus, and Web of Science (WOS), systematically searched from January 2014 to October 2024 using the following keywords combined by Boolean operators: voice assistant, virtual assistant, speech assistant, healthcare, health services. The selected keywords were chosen to ensure a comprehensive search strategy, capturing relevant studies regardless of indexing with standardized MeSH terms. This approach maximizes search sensitivity by including various terminologies used to describe voice assistants and digital health technologies, thereby reducing the risk of missing pertinent literature. Complete search strategies are provided in Table 1.

Table 1.
Search Strategy.
Citations obtained through the literature search were recorded, duplicates were eliminated using EndNote, and titles and abstracts were independently screened by three reviewers (Massimo Giordano, Marina Garofano, AB). Available full texts, compliant with inclusion and exclusion criteria, detailed below, were also independently reviewed for potentially eligible studies (see Figure 1 for the study selection process). Any disagreement between the reviewers was solved by discussion and consensus.
The inclusion criteria were as follows:
- Source: studies published in the English language from January 2014 to 28 October 2024;
- Study design: randomized controlled trial (RCT), observational studies, feasibility studies;
- Study population: subjects with NCDs (no age or gender restrictions);
- Study intervention: use of a voice assistant;
- Study outcomes: behavioral and clinical outcomes, quality of life, user experiences (usability, readiness, acceptability), cost-effectiveness, rehospitalizations rate, adherence, accessibility.
The exclusion criteria were as follows:
- Source: studies published before 2014 and after 28 October 2024;
- Study intervention: studies that do not involve the use of a voice assistant as the primary intervention;
- Study outcomes: studies that do not report on at least one of the following outcomes, behavioral and clinical outcomes, quality of life, user experiences (usability, readiness, acceptability), cost-effectiveness, rehospitalization rate, adherence, accessibility, or studies that lack any form of quantitative or qualitative measurement of these outcomes.
2.3. Data Extraction
Two authors (Massimo Giordano, AB) independently reviewed the titles and abstracts extracted from the database searches to assess their alignment with the inclusion criteria. In cases where they agreed, studies were either included or excluded based on mutual assessment. When discrepancies arose regarding the inclusion or exclusion of a manuscript based on abstract evaluation, these were resolved through discussion and consensus. If consensus could not be reached, a third reviewer (MPDP) was consulted to make the final decision. The data extraction process was structured based on established methodologies and tailored to the research questions of this review. Extracted information included (a) author, year, country; (b) study design; (c) participants; d sample size, mean age; (e) intervention and control group; (f) outcomes; (g) key results.
This systematic approach ensured a comprehensive and consistent collection of critical data, enabling a thorough synthesis of evidence to address the research questions.
2.4. Quality Assessment
The risk of bias in the studies included in this systematic review was assessed by two independent reviewers (Marina Garofano, AB), with assistance from another reviewer (FDS) if necessary in case of disagreement to resolve the issue by discussion and achieve consensus. The Cochrane risk-of-bias tool (RoB 2) [22] was used for the RCTs, evaluating the following domains: bias arising from the randomization process, bias due to deviations from intended interventions, bias due to missing outcome data, bias in the measurement of the outcome, and bias in the selection of the reported result. The risk of bias was classified as “low”, “high”, or ”unclear” (Table 2).

Table 2.
Cochrane risk of bias tool for the risk of bias in individual studies.
The ROBINS-I Tool [25] was used for the non-RCTs to evaluate the following domains: bias due to confounding, bias in the selection of participants, bias in the classification of interventions, bias due to deviations from intended interventions, bias due to missing data, bias in the measurement of outcomes, and bias in the selection of reported results. The risk of bias for these studies was classified as “low”, “moderate”, or ”high” (Table 3).

Table 3.
ROBINS-I Tool for non-RCTs; abbreviations: PY (Probably Yes), P (Possibly), NY (Probably No), N (No).
3. Results
3.1. Study Selection and Characteristics
The study selection process followed the PRISMA 2020 guidelines [20]. A total of 1410 records were identified through database searches, including PubMed (66 records), Scopus (427 records), and Web of Science (929 records). After removing 46 duplicate records with EndNote, 1376 records remained for screening. Following the screening, 1348 records were excluded based on relevance, leaving 28 reports for retrieval. All reports were successfully retrieved and assessed for eligibility. Of these, 17 were excluded for various reasons, including the absence of non-communicable diseases [14], being review articles [2], and lacking clinical trials [8]. Ultimately, eight studies met the inclusion criteria and were included in the systematic review. These studies were critically appraised to ensure they aligned with the research objectives and provided relevant data for analysis. This selection process is summarized in the PRISMA flow diagram (Figure 1), and in Table 4, there are the descriptive characteristics of the eight included studies, with a focus on (a) author, year, country; (b) study design; (c) participants; (d) sample size, mean age; (e) intervention and control group; (f) outcomes; (g) key results.

Table 4.
Descriptive characteristics of the included studies.
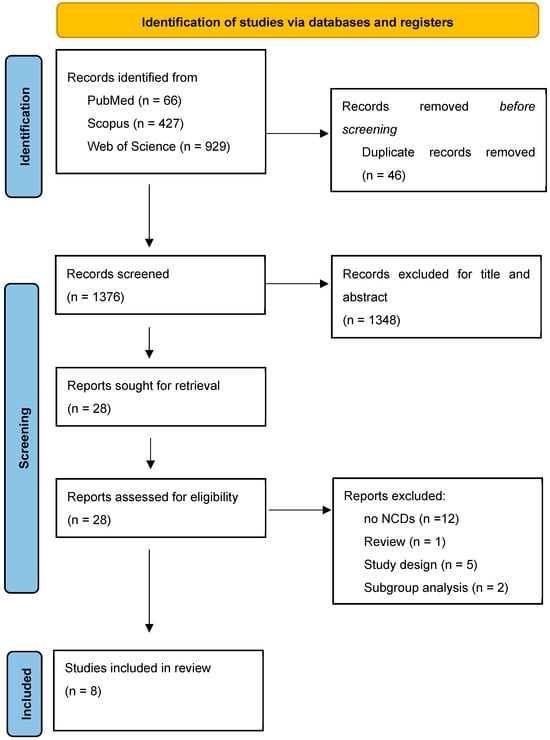
Figure 1.
Flow diagram of study selection.
3.2. Participant Demographics
The total sample consisted of 541 participants, including diverse populations:
Diabetes management: 178 participants across four studies [23,26,27,30];
Cardiovascular diseases and heart failure (HF): 257 participants across two studies [28,29];
Depression and anxiety: 63 participants across one study [24,28];
Intellectual disabilities: 44 participants across one study [31].
Participants varied in age, gender, and baseline health status, but all the studies included NCDs management with VAs.
3.3. Outcome Measures
Studies specifically investigating cost–benefit analyses, rehospitalizations, and accessibility concerning the use of VAs in the management of individuals with NCDs were not identified in the literature. The studies included in this review assessed a variety of outcomes, grouped into behavioral measures, clinical and medical outcomes, quality of life, usability, acceptability, readiness, and adherence (Table 4).
3.3.1. Behavioral Measures
Two studies analyzed behavioral changes, including physical activity and problem-solving skills. For example, in an RCT by Glavas et al. [23], participants in the intervention group showed a significant reduction in sedentary time (−67 min/day, p = 0.006) and an increase in moderate activity (+24.7 min/day, p = 0.04) compared to the control group. Kannampallil et al. [24] reported minor improvements in problem-solving behaviors, measured through problem-solving indices, with small effect sizes and limited clinical significance (Table 5).

Table 5.
Behavioral measures.
3.3.2. Clinical and Medical Outcomes
Four studies evaluated clinical outcomes such as Hemoglobin A1c (HbA1c) levels, depressive symptoms, and neural activity changes. Baptista et al. [27] observed a slight reduction, not statistically significant, in HbA1c levels from 7.3% ± 1.5 at baseline to 7.1% ± 1.4 at 6-month follow-up (n = 66), also Glavas et al. [23] observed potential benefits of the VA on glycemic management with a moderate effect size. Roca et al. [30] reported significant improvements in both HbA1c (p = 0.02) and depressive symptoms (p = 0.002), with high medication adherence (MPR ≥ 100% for several participants). Kannampallil [24] et al. examined neural activity changes but found only minor, statistically insignificant differences (Table 6).

Table 6.
Clinical and medical outcomes.
3.3.3. Quality of Life
Three studies assessed quality of life using standardized tools such as the EQ-5D-5L, WEBWMS, and custom surveys. Glavas et al. (2024) found no significant differences in overall QoL scores but noted slight improvements in the intervention group’s visual analog scale (VAS) ratings (79.2 ± 19.1 to 79.6 ± 21.7). Smith et al. (2023) reported that 80% of participants with intellectual disabilities felt more independent after using voice assistants, even though no significant improvements were observed in well-being scores as measured by WEBWMS. Kannampallil et al. [24] evaluated changes in positive and negative affect as proxies for quality of life. The Positive Affect Score showed a slight increase in the intervention group (from 25.21 ± 6.26 to +4.83 ± 7.79), compared to the control group (+2.43 ± 7.89), but with a negligible effect size (Cohen’s d = 0.1). Negative Affect Scores decreased identically in both groups (−9.07 ± 7.58 in the intervention group and −9.07 ± 5.56 in the control group, Cohen’s d = 0.1). No significant changes were observed in worry levels as measured by the Penn State Worry Questionnaire (PSWQ), with a reduction in the intervention group (−3.95 ± 11.01) and no change in the control group (0.0 ± 10.95), yielding a Cohen’s d of 0.0 (Table 7)

Table 7.
Quality of life (QoL) outcomes.
3.3.4. Usability
Six studies evaluated the usability of digital and voice-assisted technologies, providing insights into user experiences and challenges. Usability was generally rated positively, with System Usability Scale (SUS) scores ranging from 70.4 to 92, indicating good to excellent usability.
The “Vitória” virtual assistant for diabetes management [26] received SUS scores of 76.59 from end users and 70.2 from experts, highlighting its simplicity and ease of use; similarly, the “Laura” app [27] was found helpful by 86% of users, with a moderate user engagement (participants interacted with the app 18–36 times over the study period). In contrast, the “Medly” voice app for heart failure management [28] achieved an SUS score of 92/100 with 75% of users that prefer it over traditional methods, but 25% expressed privacy concerns, highlighting the need for better data management.
Amazon Alexa paired with the “Buddy Link” software [23] scored 70.4 on the SUS, reflecting good usability overall; nonetheless, some users faced challenges with specific interface elements, underscoring the variability in user experiences. Among individuals with intellectual disabilities, voice assistants like Amazon Echo and Google Home [31] were rated as easy to use by 73% of participants; however, 41% required frequent assistance, and 25% experienced frustration due to speech recognition issues. Despite these difficulties, 79% of users enjoyed using the devices and continued to engage with them. Among these, a virtual assistant for medication and reminder management [30] demonstrated consistent engagement, with 74.4% of reminders answered and 69% of users planning continued use, despite occasional comprehension issues (2.6%). Retention was high (77%), and older adults particularly appreciated its ease of use, reinforcing the importance of accessibility in digital health solutions (Table 8).

Table 8.
Usability outcomes.
3.3.5. Acceptability and Readiness
Four studies assessed the acceptability and readiness to adopt digital and voice-assisted technologies, highlighting overall positive perceptions and areas for improvement.
Baptista et al. [27] explored user satisfaction with the “Laura” app for diabetes management. The study found that 86% of participants considered the app helpful and friendly, and 73% expressed trust in the virtual assistant. However, some users experienced frustration due to mismatched verbal and nonverbal cues, which limited the overall user experience.
Kowalska et al. [29] investigated readiness for telemedicine and voice technology in cardiovascular patients. The study reported high readiness rates, with 83.9% of participants open to telemedicine and 66.7% willing to use voice technology. This readiness was particularly pronounced among individuals who had faced barriers to healthcare access and was influenced by factors such as higher education levels, urban residence, and strong family support.
Smith et al. [31] focused on individuals with intellectual disabilities using voice assistants like Amazon Echo and Google Home. The study revealed that 79% of participants enjoyed using the devices despite occasional frustration with speech intelligibility. However, 41% required frequent assistance, underscoring the importance of adequate training and support to maximize usability and satisfaction.
Barbaric et al. [28] evaluated the acceptability of the “Medly” app for heart failure management, with 75% of users preferring it over traditional methods (Table 9).

Table 9.
Acceptability and readiness outcomes.
3.3.6. Adherence
Adherence, defined as the level of engagement with voice assistants, was reported in only one study. Smith et al. [31] provided data showing that 57 out of 63 participants actively used the devices, while 6 did not engage with any features. Music was the most frequently used feature (~90%), followed by reminders and weather updates (~40%). Perseverance in using the devices was high, with 79% of participants continuing to use the voice assistants despite challenges such as intelligibility issues or phrasing commands.
Overall, the reviewed interventions demonstrated promising outcomes in usability, behavioral engagement, adherence, and clinical metrics, but challenges such as user training, privacy concerns, and occasional frustration with interfaces were identified, emphasizing the need for iterative design improvements and tailored implementation strategies (Table 10).

Table 10.
Adherence outcomes.
4. Discussion
This systematic review highlights the potential and challenges of using voice VAs in managing NCDs, emphasizing their role in supporting behavioral engagement, clinical outcomes, and usability, while pointing out the need for improvements in accessibility, privacy, and personalization [32]. An initial aim of this review was to compare the effectiveness of VAs with other types of conversational agents (CAs) in NCD management. However, the current literature lacks studies that directly perform such comparisons and investigating this aspect in future research could provide valuable insights into user preferences and inform strategies to enhance adherence to these technologies. As noted in recent reviews [33,34], for example, incorporating anthropomorphic and context-aware features in conversational agents may strengthen relational outcomes and foster greater user adherence. Investigating these aspects further could guide the development of more tailored and effective interventions.
Furthermore, an important aspect of VA implementation in healthcare is their specific functionalities and regulatory approval status. The applications included in this review demonstrate a range of approaches to NCD management, from symptom tracking and behavior change [23,24,26] coaching to medication reminders [26,30] and clinician alerts [26,28]. For example, Amazon Alexa and Echo [23,29,35] integrates with wearable devices and mobile health apps to provide personalized lifestyle tracking and health coaching, making it a flexible tool for managing diabetes and obesity and cardiovascular disease. Similarly, Medly Voice Assistant [28] is specifically tailored for heart failure management, enabling remote symptom tracking, daily patient feedback, and clinician alerts when deterioration is detected. Other applications, such as Vitória and Laura [26,27], focus on diabetes self-management, offering medication reminders, dietary coaching, and emotional support through conversational artificial intelligence. In addition, the Signal-based virtual assistant studied by Roca et al. [30] is designed to enhance medication adherence in patients with type 2 diabetes and depressive disorder by providing structured reminders and enabling clinician monitoring through a secure messaging platform (Table 11).

Table 11.
Comparative overview of voice assistant applications.
A key aspect emerging from this systematic review is the lack of explicit mention of regulatory approvals, such as FDA or MDR CE certification, in the included studies. None of the analyzed voice assistants were reported to have undergone regulatory approval processes, raising concerns about their compliance with established medical device regulations. This omission suggests that many of these technologies may not yet meet the safety, efficacy, and data protection standards required for clinical use.
The absence of regulatory approval may be attributed to several factors. First, some of the voice assistants examined in this review are research prototypes or commercially available AI-driven tools that have been repurposed for healthcare applications rather than specifically designed as certified medical devices. Second, the regulatory classification of voice assistants in healthcare remains an evolving area, and many interventions may not yet fall under the category of Software as a Medical Device (SaMD), thus operating in a regulatory gray zone.
This is further supported by the limited number of studies available, with only eight included in this review, all involving a small patient population. Given the growing emphasis on regulatory compliance for Software as a Medical Device (SaMD), future research should investigate how voice assistants can meet FDA and MDR requirements and explore strategies to ensure their clinical safety and effectiveness.
Regarding clinical and behavioral outcomes, the reviewed studies showed modest improvements. For instance, Roca et al. [30] observed better glycemic control and reduced depressive symptoms using a VA intervention. These findings align with broader evidence, suggesting that personalized conversational agents can deliver behavior change strategies effectively, as noted by Anisha et al. [33], who highlighted their role in promoting self-management and behavioral modifications for NCDs. However, some interventions, such as Kannampallil et al. [24], reported limited clinical impact, emphasizing the importance of targeting intervention design to user needs. A promising opportunity for delivering tailored interventions lies in the integration of artificial intelligence that enhances personalization with more precise recommendations and interventions with a positive impact on clinical and behavioral outcomes [36].
User experience and usability are investigated in most of the studies included in this review, highlighting their critical importance when discussing virtual assistants. This focus underscores the central role that ease of use, interface design, and user satisfaction play in determining the effectiveness and adoption of these technologies. In the included studies, usability scores ranged from moderate to excellent [23,26,27,28], and participants frequently reported ease of use but highlighted challenges such as speech recognition errors [31] and interface complexities [26]. For elderly users, usability issues can pose significant barriers, particularly when dealing with complex systems that fail to account for age-related sensory or cognitive impairments [37]. Anisha et al. [33] also identified usability as a key determinant of success for conversational agents, particularly in populations with low health literacy, and Sawad et al. [38] highlighted that user satisfaction with CAs often stems from their ability to provide nonjudgmental, easily accessible support. However, some users found certain embodied agents annoying or difficult to engage with. Improved designs incorporating adaptive learning and anthropomorphic features may further enhance usability and user trust.
Finally, adherence to VA interventions was generally moderate. For instance, Smith et al. [31] reported active engagement from 90% of users, with perseverance levels high, despite challenges that underline the need for improved user-centric design, tailored support systems, and rigorous testing to enhance the effectiveness and adherence to such interventions in diverse populations.
4.1. Conclusions
This systematic review underscores the potential of VAs as an innovative tool in managing NCDs, offering diverse benefits across clinical, behavioral, and usability domains. While VAs demonstrate promise in promoting self-management, enhancing patient engagement, and improving usability scores, their impact on clinical and quality-of-life outcomes remains modest, reflecting variability in user experiences and intervention designs, also with privacy concerns, speech recognition errors, and accessibility challenges that limit widespread adoption. Future research should focus on including larger, diverse populations to improve the generalizability of findings and ensure underrepresented groups are adequately studied, such as those with low health literacy or limited technological access. Employing more rigorous study designs, such as multicenter RCTs, can provide stronger evidence for the effectiveness of VAs. The adoption of standardized and validated outcome measures across studies will enable better comparisons and synthesis of results.
4.2. Limitations and Research Gaps
This review underscores several limitations that need to be addressed to optimize the effectiveness and adoption of voice assistants in healthcare. First of all, many of the included studies involved small participant groups, which limits the generalizability of findings. Observational and pilot studies formed a significant portion of the reviewed literature, reducing the ability to draw robust causal conclusions; secondly, the studies measured diverse outcomes ranging from usability and adherence to clinical and behavioral improvements, making direct comparisons challenging, and also the lack of standardized metrics further complicates synthesizing results. Finally, the majority of studies focused on specific demographic groups, such as adults with diabetes or cardiovascular diseases. Vulnerable populations, including those with lower health literacy, limited access to technology, or residing in rural areas, were underrepresented.
Author Contributions
Conceptualization: A.B., A.C., G.C., L.G., M.G. (Marina Garofano), M.G. (Massimo Giordano), C.P., G.M., M.P.D.P., F.D.S., M.A., M.B., R.D.S., M.C., P.B. and P.R.; Methodology: A.B., M.G. (Marina Garofano) and M.G. (Massimo Giordano); Formal Analysis and Investigation: M.G. (Marina Garofano), M.G. (Massimo Giordano), F.D.S. and M.C.; Data Curation: F.D.S. and M.P.D.P.; Writing—Original Draft Preparation: A.B., M.G. (Marina Garofano) and M.G. (Massimo Giordano); Writing—Review and Editing: G.C., L.G., C.P., G.M., M.P.D.P., F.D.S., M.A., M.B., R.D.S., M.C., P.B. and P.R. All authors have read and agreed to the published version of the manuscript.
Funding
The project “TED: The intElligent Doctor at your home” (PRIN 2022), classified under the LS4 (Life Sciences) sector, is supported through funding identified by the Ministerial Code 2022F7C2TA and the CUP (Codice Unico di Progetto) D53D23014300006. This initiative is part of the PRIN (Progetti di Ricerca di Rilevante Interesse Nazionale) program, aimed at advancing innovative solutions in healthcare delivery by leveraging cutting-edge technologies and interdisciplinary research.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data are included in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Piovani, D.; Nikolopoulos, G.K.; Bonovas, S. Non-Communicable Diseases: The Invisible Epidemic. J. Clin. Med. 2022, 11, 5939. [Google Scholar] [CrossRef] [PubMed]
- Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [CrossRef] [PubMed]
- Peters, R.; Ee, N.; Peters, J.; Beckett, N.; Booth, A.; Rockwood, K.; Anstey, K.J. Common risk factors for major noncommunicable disease, a systematic overview of reviews and commentary: The implied potential for targeted risk reduction. Ther. Adv. Chronic Dis. 2019, 10, 2040622319880392. [Google Scholar] [CrossRef]
- WHO. Noncommunicable Diseases Country Profiles; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Laranjo, L.; Dunn, A.G.; Tong, H.L.; Kocaballi, A.B.; Chen, J.; Bashir, R.; Surian, D.; Gallego, B.; Magrabi, F.; Lau, A.Y.S.; et al. Conversational agents in healthcare: A systematic review. J. Am. Med. Inform. Assoc. 2018, 25, 1248–1258. [Google Scholar] [CrossRef]
- Milne-Ives, M.; de Cock, C.; Lim, E.; Shehadeh, M.H.; de Pennington, N.; Mole, G.; Normando, E.; Meinert, E. The Effectiveness of Artificial Intelligence Conversational Agents in Health Care: Systematic Review. J. Med. Internet Res. 2020, 22, e20346. [Google Scholar] [CrossRef]
- Hoy, M.B. Alexa, Siri, Cortana, and More: An Introduction to Voice Assistants. Med. Ref. Serv. Q. 2018, 37, 81–88. [Google Scholar] [CrossRef]
- Minder, B.; Wolf, P.; Baldauf, M.; Verma, S. Voice assistants in private households: A conceptual framework for future research in an interdisciplinary field. Humanit. Soc. Sci. Commun. 2023, 10, 173. [Google Scholar] [CrossRef]
- Ahanin, E.; Sade, A.B.; Tat, H.H. Applications of Artificial Intelligence and Voice Assistant in Healthcare. Int. J. Acad. Res. Bus. Soc. Sci. 2022, 12, 2545–2554. [Google Scholar] [CrossRef]
- Bérubé, C.; Kovacs, Z.F.; Fleisch, E.; Kowatsch, T. Reliability of Commercial Voice Assistants’ Responses to Health-Related Questions in Noncommunicable Disease Management: Factorial Experiment Assessing Response Rate and Source of Information. J. Med. Internet Res. 2021, 23, e32161. [Google Scholar] [CrossRef]
- Sezgin, E.; Huang, Y.; Ramtekkar, U.; Lin, S. Readiness for voice assistants to support healthcare delivery during a health crisis and pandemic. NPJ Digit. Med. 2020, 3, 122. [Google Scholar] [CrossRef]
- Schachner, T.; Keller, R.; von Wangenheim, F. Artificial Intelligence-Based Conversational Agents for Chronic Conditions: Systematic Literature Review. J. Med. Internet Res. 2020, 22, e20701. [Google Scholar] [CrossRef] [PubMed]
- Vaidyam, A.N.; Wisniewski, H.; Halamka, J.D.; Kashavan, M.S.; Torous, J.B. Chatbots and Conversational Agents in Mental Health: A Review of the Psychiatric Landscape. Can. J. Psychiatry 2019, 64, 456–464. [Google Scholar] [CrossRef] [PubMed]
- Abd-Alrazaq, A.A.; Rababeh, A.; Alajlani, M.; Bewick, B.M.; Househ, M. Effectiveness and Safety of Using Chatbots to Improve Mental Health: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2020, 22, e16021. [Google Scholar] [CrossRef] [PubMed]
- Kocaballi, A.B.; Berkovsky, S.; Quiroz, J.C.; Laranjo, L.; Tong, H.L.; Rezazadegan, D.; Briatore, A.; Coiera, E. The Personalization of Conversational Agents in Health Care: Systematic Review. J. Med. Internet Res. 2019, 21, e15360. [Google Scholar] [CrossRef]
- Guarnera, J.; Yuen, E.; Macpherson, H. The Impact of Loneliness and Social Isolation on Cognitive Aging: A Narrative Review. J. Alzheimers Dis. Rep. 2023, 7, 699–714. [Google Scholar] [CrossRef]
- Vitlin-Stein, I.; Gitlow, L.; Fusco, B.; Pathammavong, S.; Rajotte, C. A survey of the assistive technology experience of older adults in Tompkins County, NY. Disabil. Rehabil. Assist. Technol. 2024, 19, 2991–2997. [Google Scholar] [CrossRef]
- Marasinghe, K.M.; Chaurasia, A.; Adil, M.; Liu, Q.Y.; Nur, T.I.; Oremus, M. The impact of assistive devices on community-dwelling older adults and their informal caregivers: A systematic review. BMC Geriatr. 2022, 22, 897. [Google Scholar] [CrossRef]
- Albarqi, M.N. Exploring the Effectiveness of Technology-Assisted Interventions for Promoting Independence in Elderly Patients: A Systematic Review. Healthcare 2024, 12, 2105. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Schardt, C.; Adams, M.B.; Owens, T.; Keitz, S.; Fontelo, P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med. Inform. Decis. Mak. 2007, 7, 16. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Glavas, C.; Scott, D.; Sood, S.; George, E.S.; Daly, R.M.; Gvozdenko, E.; de Courten, B.; Jansons, P. Exploring the Feasibility of Digital Voice Assistants for Delivery of a Home-Based Exercise Intervention in Older Adults With Obesity and Type 2 Diabetes Mellitus: Randomized Controlled Trial. JMIR Aging 2024, 7, e53064. [Google Scholar] [CrossRef]
- Kannampallil, T.; Ajilore, O.A.; Lv, N.; Smyth, J.M.; Wittels, N.E.; Ronneberg, C.R.; Kumar, V.; Xiao, L.; Dosala, S.; Barve, A.; et al. Correction: Effects of a virtual voice-based coach delivering problem-solving treatment on emotional distress and brain function: A pilot RCT in depression and anxiety. Transl Psychiatry 2023, 13, 242. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Balsa, J.; Félix, I.; Cláudio, A.P.; Carmo, M.B.; Silva, I.C.E.; Guerreiro, A.; Guedes, M.; Henriques, A.; Guerreiro, M.P. Usability of an Intelligent Virtual Assistant for Promoting Behavior Change and Self-Care in Older People with Type 2 Diabetes. J. Med. Syst. 2020, 44, 130. [Google Scholar] [CrossRef]
- Baptista, S.; Wadley, G.; Bird, D.; Oldenburg, B.; Speight, J. Acceptability of an Embodied Conversational Agent for Type 2 Diabetes Self-Management Education and Support via a Smartphone App: Mixed Methods Study. JMIR Mhealth Uhealth 2020, 8, e17038. [Google Scholar] [CrossRef]
- Barbaric, A.; Munteanu, C.; Ross, H.; Cafazzo, J.A. Design of a Patient Voice App Experience for Heart Failure Management: Usability Study. JMIR Form. Res. 2022, 6, e41628. [Google Scholar] [CrossRef]
- Kowalska, M.; Gładyś, A.; Kalańska-Łukasik, B.; Gruz-Kwapisz, M.; Wojakowski, W.; Jadczyk, T. Readiness for Voice Technology in Patients With Cardiovascular Diseases: Cross-Sectional Study. J. Med. Internet Res. 2020, 22, e20456. [Google Scholar] [CrossRef]
- Roca, S.; Lozano, M.L.; García, J.; Alesanco, Á. Validation of a Virtual Assistant for Improving Medication Adherence in Patients with Comorbid Type 2 Diabetes Mellitus and Depressive Disorder. Int. J. Environ. Res. Public. Health 2021, 18, 12056. [Google Scholar] [CrossRef]
- Smith, E.; Sumner, P.; Hedge, C.; Powell, G. Smart-speaker technology and intellectual disabilities: Agency and wellbeing. Disabil. Rehabil. Assist. Technol. 2023, 18, 432–442. [Google Scholar] [CrossRef]
- Angelelli, M.; Catalano, C.; Hill, D.; Koshutanski, H.; Pascarelli, C.; Rafferty, J. A reference architecture proposal for secure data management in mobile health. In Proceedings of the 2022 7th International Conference on Smart and Sustainable Technologies (SpliTech), Split, Croatia, 5–8 July 2022; pp. 1–6. [Google Scholar]
- Anisha, S.A.; Sen, A.; Bain, C. Evaluating the Potential and Pitfalls of AI-Powered Conversational Agents as Humanlike Virtual Health Carers in the Remote Management of Noncommunicable Diseases: Scoping Review. J. Med. Internet Res. 2024, 26, e56114. [Google Scholar] [CrossRef]
- Griffin, A.C.; Xing, Z.; Khairat, S.; Wang, Y.; Bailey, S.; Arguello, J.; Chung, A.E. Conversational Agents for Chronic Disease Self-Management: A Systematic Review. AMIA Annu. Symp. Proc. 2020, 2020, 504–513. [Google Scholar] [PubMed]
- Pighin, M.; Choi, Y.K. The Evaluation of Smart Speaker Skills for Chronic Disease Management of Older Adults. Innov. Aging 2021, 5, 689. [Google Scholar] [CrossRef]
- Al Kuwaiti, A.; Nazer, K.; Al-Reedy, A.; Al-Shehri, S.; Al-Muhanna, A.; Subbarayalu, A.V.; Al Muhanna, D.; Al-Muhanna, F.A. A Review of the Role of Artificial Intelligence in Healthcare. J. Pers. Med. 2023, 13, 951. [Google Scholar] [CrossRef] [PubMed]
- De Cola, M.C.; Maresca, G.; D’Aleo, G.; Carnazza, L.; Giliberto, S.; Maggio, M.G.; Bramanti, A.; Calabrò, R.S. Teleassistance for frail elderly people: A usability and customer satisfaction study. Geriatr. Nurs. 2020, 41, 463–467. [Google Scholar] [CrossRef]
- Bin Sawad, A.; Narayan, B.; Alnefaie, A.; Maqbool, A.; McKie, I.; Smith, J.; Yuksel, B.; Puthal, D.; Prasad, M.; Kocaballi, A.B. A Systematic Review on Healthcare Artificial Intelligent Conversational Agents for Chronic Conditions. Sensors 2022, 22, 2625. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).














