Effects of Motor Skills and Physical Activity Interventions on Motor Development in Children with Autism Spectrum Disorder: A Systematic Review
Abstract
1. Introduction
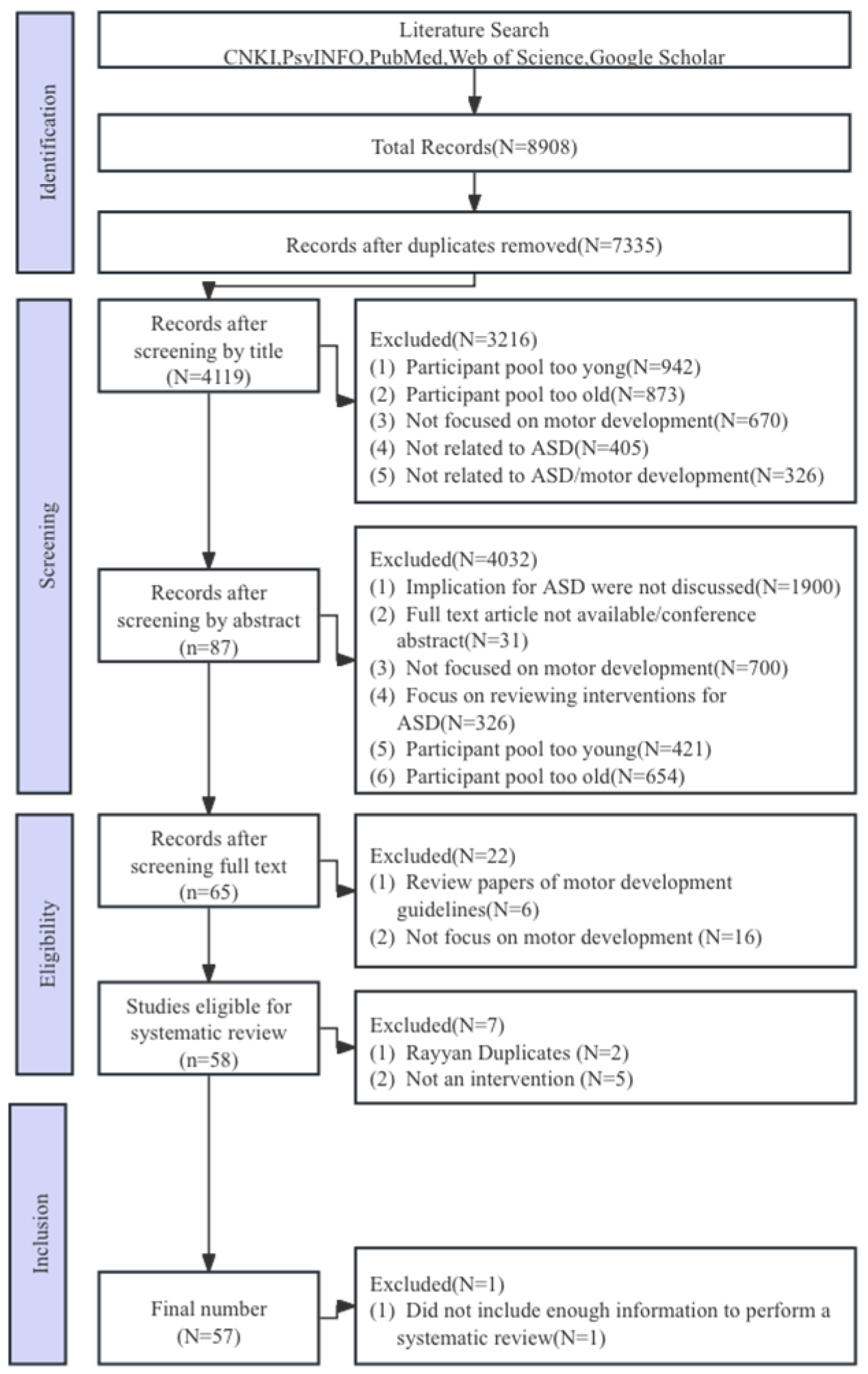
2. Materials and Methods
2.1. Literature Search Process
2.2. Inclusion Criteria
2.3. Data Extraction and Qualitative Assessment
3. Results
3.1. Characteristics of Participates
3.2. Design of Research
3.3. Methods of Evolution
3.4. Characteristics of Intervention: Typology of Exercises/Sports
3.5. Characteristics of Intervention: Place of Implementation
3.6. Effects of Intervention: Acquisition Retention and Migration
4. Discussion
4.1. Development of Sensitivity Tool and Local Research
4.2. Emphasis on Individual Factors in Children and Formulation of Systematic Intervention Plan
4.3. Emphasis of the Joint Drive of Home, School and Community, and Construction of Inclusive Intervention Environment
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Eligibility Criteria Specified | Random Allocation | Concealed Allocation | Baseline Comparability | Blind Subjects | Blind Therapists | Blind Assessors | Adequate Follow-Up | Intention-to-Treat Analysis | Between Group Comparison | Point Estimates and Variability | PEDro Score | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ferguson et al. (2010) [17] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 4 |
| Arzoglou et al. (2013) [18] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Hayward et al. (2016) [19] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Cei et al. (2017) [20] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Guest et al. (2017) [21] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Pan et al. (2017) [22] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 |
| Kokaridas et al. (2018) [23] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Sarabzadeh et al. (2019) [24] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Howell et al. (2021) [25] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Ketcheson et al. (2021) [26] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4 |
| Sansi et al. (2021) [27] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Erisin et al. (2022) [28] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Fahimeh et al. (2022) [29] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Shanker et al. (2022) [30] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 |
| Morales et al. (2022) [31] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Cheldavi et al. (2014) [32] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4 |
| Bremer et al. (2015) [33] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4 |
| Samsudin et al. (2017) [34] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4 |
| EI Shemy et al. (2018) [35] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Navaee et al. (2018) [36] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 5 |
| Bo et al. (2019) [37] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4 |
| Tse et al. (2019) [38] | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Tse et al. (2019) [39] | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 7 |
| Xing et al. (2020) [40] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 5 |
| Bremer et al. (2021) [41] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Columna et al. (2021) [42] | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Dong et al. (2021) [43] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 4 |
| Ketcheson et al. (2021) [44] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 5 |
| Liu et al. (2021) [45] | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 5 |
| Bo et al. (2023) [46] | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 |
| Wuang et al. (2010) [47] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Gabriel et al. (2012) [48] | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 6 |
| Ajzenman et al. (2013) [49] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 5 |
| Gabriel et al. (2015) [50] | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 5 |
| Srinivasan et al. (2015) [51] | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Borgi et al. (2016) [52] | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 5 |
| Taheri-Torbati et al. (2018) [53] | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Wang et al. (2022) [54] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Pan et al. (2010) [55] | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Fragala et al. (2011) [56] | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Pan et al. (2011) [57] | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Chu et al. (2012) [58] | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Alaniz et al. (2017) [59] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4 |
| Caputo et al. (2018) [60] | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Marzouki et al. (2022) [61] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Vodakova et al. (2022) [62] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 4 |
| Hitlon et al. (2014) [63] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 4 |
| Hitlon et al. (2015) [64] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 4 |
| Edward et al. (2017) [65] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Travers et al. (2017) [66] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 4 |
| Caro et al. (2017) [67] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Rafiei et al. (2021) [12] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 5 |
| Sarol et al. (2015) [68] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 4 |
| Henderson et al. (2016) [69] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 4 |
| Toscano et al. (2018) [70] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 4 |
| Chiva-Bartoll et al. (2021) [71] | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 4 |
| Fahimeh et al. (2022) [72] | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 4 |
| Author(s) (Year) | Study Design, Level of Evidence | Atmosphere | Strength of the Evidence | Participant (Age Range and Diagnosis) | n (M) | Intervention Characteristics (Methods/Time/Frequency/Week) | Ratio (Instructor: Child) |
|---|---|---|---|---|---|---|---|
| |||||||
| Ferguson et al. (2010) [17] | Retrospective cohort, IV | School | Weak | 3–8 years, ASD | Total n = 3 | APA (gross and fine motor skills, endurance, and strength training, bat, ball and sport skill, swinging) 50 min, 3 times/week, 20 weeks | NR |
| Arzoglou et al. (2013) [18] | Non-randomized trial, III | School | Weak | 16 years (mean), ASD | Total n = 10, EG:5, CG:5 | Traditional Greek dance. 35–45 min, 3 times/week, 8 weeks | 1:1–2 |
| Hayward et al. (2016) [19] | Retrospective cohort, IV | Community | Weak | 5–19 years, ASD | EG:15 | Adaptive soccer program. 90 min, 1 times/week, 6 weeks | 1:1 |
| Cei et al. (2017) [20] | Retrospective cohort, IV | School | Weak | 6–13 years, ASD | EG:30 | Soccer together program. 60 min, 2 times/week, 24 weeks | NR |
| Guest et al. (2017) [21] | Prospective cohort, IV | School | Weak | 6–11 years, ASD | EG:13 | Multi-sport camp: locomotor skills and object control skills, translational sports | 1:3 |
| Pan et al. (2017) [22] | RCT, II | School | Adequate | 6–12 years, ASD | Total n = 22 (22), EG:11, CG:11 | Table tennis, 40 min, 2 times/week, 12 weeks | 1:1–2 |
| Kokaridas et al. (2018) [23] | Prospective cohort, IV | NR | Weak | 9 years, ASD and TD | Total n = 6 (6), EG:3, CG:3 | Indoor climbing, 40 min, 2 times/week, 12 weeks | 1:3 |
| Sarabzadeh et al. (2019) [24] | RCT, II | School | Weak | 6–12 years, ASD | Total n = 18 (14), EG:9, CG:9 | Tai Chi Chuan training, 60 min, 3 times/week, 6 weeks | NR |
| Howell et al. (2021) [25] | Non-randomized trial, II | Community | Weak | 5–12 years, ASD and TD | Total n = 35, EG:16, CG:19 | Football Program(catching, kicking and bouncing), 60–90 min, 1 times/week,13 weeks | NR |
| Ketcheson et al. (2021) [26] | Non-randomized trial, II | School | Weak | 4.67 years (mean), ASD | Total n = 25 (18) | Physical Activity Intervention, 60 min, 12 weeks | 1:1 |
| Sansi et al. (2021) [27] | RCT, II | School | Adequate | 6–11 years, ASD(21) | Total n = 45 (34), EG:27, CG:18 | Inclusive Physical Activity Program, 60 min, 2 times/week, 12 weeks | 1:5 |
| Erisin et al. (2022) [28] | RCT, II | School | Adequate | 10.07 years (mean), ASD(14) | Total n = 28 (28), EG:14, CG:14 | Circuit Exercise Program, 60 min, 3 times/week, 12 weeks | 1:1 |
| Fahimeh et al. (2022) [29] | RCT, II | School | Weak | 8–11 years, ASD | Total n = 28 (28), EG:14, CG:14 | ICPL and SPARK, 60 min, 2 times/week, 8 weeks | NR |
| Shanker et al. (2022) [30] | RCT, II | School | Weak | NR | Total n = 43, EG:23, CG:20 | Yoga, 45 min, 12 weeks | NR |
| Morales et al. (2022) [31] | Prospective cohort, III | School | Weak | 11.07 years (mean), ASD | Total n = 40, EG:21, CG:19 | Juda program, 90 min, 1 times/week, 24 weeks | 1:5–6 |
| |||||||
| Cheldavi et al. (2014) [32] | Non-randomized trial, III | School | Weak | 7–10 years, ASD | Total n = 20, EG:10, CG:10 | Balance training program, 45 min, 3 times/week, 6 weeks | NR |
| Bremer et al. (2015) [33] | Non-randomized trial, III | Rehabilitation center | Weak | 4 years, ASD | Total n = 9 (7), EG:5, CG:4 | Fundamental motor skill intervention, 60 min, 1 times/week, 12 weeks; 120 min, 1 times/week, 6 weeks | 1:1–2 |
| Samsudin et al. (2017) [34] | Non-randomized trial, III | School | Weak | 6–10 years, ASD | Total n = 10, EG:5, CG:5 | Throwing movements(lobbing) boules program. 10 throws in one set of interventions and a total finished 60 throws in about 2 weeks. | NR |
| EI Shemy et al. (2018) [35] | RCT, II | School | Weak | 8–10 years, ASD | Total n = 30, EG:10, CG:10 | Gain training with auditory rhythmic cueing, PT program: 60 min, 3 times/week,12 weeks, RAS training: 30 min, 3 times/week, 12 weeks | NR |
| Navaee et al. (2018) [36] | Non-randomized trial, III | School | Weak | 7–10 years, ASD | Total n = 20, EG:10, CG:10 | A throwing task, 1 x, and retention the next day. | 1:1 |
| Bo et al. (2019) [37] | Non-randomized trial, III | School | Weak | 8–13 years, ASD | Total n = 9 | Fundamental movement skills. 60 min, 7 times/week, 2 weeks | 1:1 |
| Tse et al. (2019) [38] | RCT, II | School | Adequate | 9–12 years, ASD | Total n = 65 EG1:22, EG2:22, CG:21 | A throwing task, 1 x, and retention/switch the next day. | NR |
| Tse et al. (2019) [39] | RCI, II | School | Adequate | 9–12 years, ASD | Total n = 48 EG1:12, EG2:12, EG3:12, EG:12 | Basketball shooting task, 6 training blocks, 15 trials, 1 day | 1:1 |
| Xing et al. (2020) [40] | RCT, III | Rehabilitation center | Weak | 6–10 years, ASD | Total n = 24 (18), E:10 (7), C:14 (11). | Fundamental movement skills (run, jump, throwing, catching, and beating), 60 min/times, 3 times/week, 12 weeks | 1:2–3 |
| Bremer et al. (2021) [41] | Non-randomized trial, II | NR | Weak | 3–5 years, ASD | Total n = 20 (15) EG:11, CG:9 | Movement skill intervention (running, hopping, catching, jumping, etc.), 60 min, 2 times/week, 12 weeks | NR |
| Columna et al. (2021) [42] | RCT, III | School, Family | Weak | 4–11 years, ASD | Total n = 15 EG:8, CG:7 | Motor skill intervention (throwing, catching, one-hand strike, etc.), NR | NR |
| Dong et al. (2021) [43] | Non-randomized trial, III | Rehabilitation center | Weak | 6–10 years, ASD | Total n = 24 (18) EG:8, CG:7 | Fundamental movement skills (run, jump, objective control skills), 60 min, 3 times/week, 12 weeks | 1:2–3 |
| Ketcheson et al. (2021) [44] | Non-randomized trial, II | School | Weak | 4–6 years, ASD | Total n = 20 (15) EG:11, CG:9 | Motor Skills Intervenion. 20 min/weeks, 8 weeks | 1:1 |
| Liu et al. (2021) [45] | RCT, II | School | Weak | 6–10 years, ASD | Total n = 24 (24), EG:12, CG:12 | Motor intervention (Standing long jump and throwing beanbag), 80 min, 3 times/week, 8 weeks | NR |
| Bo et al. (2023) [46] | Non-randomized trial, III | Rehabilitation center | Weak | 6–10 years, ASD | Total n = 24 (18) EG:8, CG:7 | Fundamental movement skills (run, jump, objective control skills), 60 min, 3 times/week, 12 weeks | 1:2–3 |
| |||||||
| Wuang et al. (2010) [47] | Non-randomized trial, II | Riding therapy | Weak | 6–8 years, ASD | Total n = 60 (47), EG:30, CG:30 | Horse riding intervention, 60 min, 2 times/week, 20 weeks | NR |
| Gabriel et al. (2012) [48] | Non-randomized trial, II | Riding center | Weak | 6–16 years, ASD | Total n = 46(36), EG:26, CG:16 | Horse riding intervention, 60 min, 1 times/week, 10 weeks | 1:3–4 |
| Ajzenman et al. (2013) [49] | Prospective cohort, IV | School-based therapy | Weak | 5–12 years, ASD | Total n = 6 (4) | Horse riding intervention, 45 min, 1 times/week, 12 weeks | NR |
| Gabriel et al. (2015) [50] | RCT, II | Riding center | Adequate | 6–16 years, ASD | Total n = 116, EG:58, CG:58 | Horse riding intervention, 60 min, 1 times/week, 10 weeks | 1:2–4 |
| Srinivasan et al. (2015) [51] | RCT, II | School | Weak | 5–12 years, ASD | Total n = 36, EG1:12, EG2:12, CG:12. | Robotic, rhythm, standard-of-care, 45 min, 4 times/week, 8 weeks | 1:1 |
| Borgi et al. (2016) [52] | RCT, II | Riding center | Weak | 6–12 years, ASD | Total n = 28, EG:15, CG:13 | Equine-assisted intervention, 60–70 min, 1 times/week, 24 weeks | 1:3–4 |
| Taheri-Torbati et al. (2018) [53] | RCT, II | School | Weak | 9–13 years, ASD and TD | Total n = 48, EG1:12, TD1:1, EG2:12, TD2:12. | Video and live modeling program, 17 training blocks in 2 days, and retention after 1 week | 1:1 |
| Wang et al. (2022) [54] | RCT, II | Riding center | Adequate | 5–15 years, ASD | Total n = 30 (19), EG:15, CG:15 | Horse riding intervention, 45–60 min, 2–3 times/week, 24 weeks | 1:1 |
| Pan et al. (2010) [55] | Non-randomized trial, III | Swimming pool | Weak | 5–9 years, ASD | Total n = 16 (16), EG1:8, EG2:8 | Aquatic skills, warm-up activities, group games/activities, cool-down activities. 90 min, 2 times/week, 10 weeks | 1:2 |
| Fragala et al. (2011) [56] | Non-randomized trial, III | Swimming pool | Weak | 6–12 years, ASD | Total n = 12, EG:7, CG:5 | Aquatic skills, warm-up, aerobic activities, strengthening activities, cool down, and stretching, 40 min, 2 times/week, 14 weeks | NR |
| Pan et al. (2011) [57] | Non-randomized trial, III | Hydrotherapy and swimming pool | Weak | 7–12 years, ASD and TD | Total n = 30, ASD:15, TD:15 | Aquatic skills, structured social and floor warm-up activities, group games/activities, cool down activities 60 min, 2 times/week, 14 weeks | 1:2 |
| Chu et al. (2012) [58] | Non-randomized trial, III | School | Weak | 7–12 years, ASD and TD | Total n = 42, EG1:14, ASD:7, TD:7, EG2:14, ASD:7, TG:7 EG3:14, ASD:7, TD:7 | Aquatic skills with peer-assisted, 60 min, 2 times/week, 12 weeks | 1:2 |
| Alaniz et al. (2017) [59] | Prospective cohort IV | Swimming pool | Weak | 3–7 years, ASD | Total n = 6 (6) | An aquatic therapy program on water safety, 60 min, 1 times/week, 8.16 or 24 weeks | 1:2 |
| Caputo et al. (2018) [60] | Non-randomized trial, III | Swimming pool | Weak | 6–12 years, ASD | Total n = 26, EG:13, CG:13 | Aquatic skills, swimming, 45 min, 1–2 times/week, 10 weeks | 1:1 1:3 |
| Marzouki et al. (2022) [61] | RCT, II | Swimming pool | Adequate | 6–7 years, ASD | Total n = 28 (21), EG1:8, EG2:8, CG:6 | Aquatic training, technical vs. game-based, 50 min, 2 times/week, 8 weeks | 1:2 |
| Vodakova et al. (2022) [62] | Prospective cohort IV | Swimming pool | Weak | 9.4 years (mean), ASD | Total n = 7 (6) | Aquatic training, swimming, 60 min, 1 times/week, 9 weeks | 1:1 |
| |||||||
| Hitlon et al. (2014) [63] | Prospective cohort IV | School | Weak | 6–13 years, ASD | Total n = 7 | Speed-based game (Makotoarena), 2 min, 3 times/week, 10 weeks | NR |
| Hitlon et al. (2015) [64] | Non-randomized trial, II | School | Weak | 8–18 years, ASD | Total n = 17 | Speed-based game (Makotoarena), 2 min, 3 times/week, 6–10 weeks | NR |
| Edward et al. (2017) [65] | Non-randomized trial, II | School | Adequate | 6–12 years, ASD | Total n= 30 (18), ASD:11 (8), TD:19 (10) | AVG, 45–60 min, 3 times/week, 2 weeks | NR |
| Travers et al. (2017) [66] | Prospective cohort, IV | School | Weak | 7–17 years, ASD | Total n = 29 (27) | visual-based biofeedback training (Xbox Kinect, Wii), 60 min, 3 times/week, 6 weeks | NR |
| Caro et al. (2017) [67] | Prospective cohort, IV | School | Weak | 7–10 years, ASD | Total n = 7 | FroggyBobby exergame (Pasitos), 30 min, 2 times/week, 7 weeks | 1:2 |
| Rafiei et al. (2021) [12] | RCT, II | School | Adequate | 6–10 years, ASD | Total n = 60 (16), EG1:20, EG2:20, CG:20 | visual-based biofeedback training (Xbox Kinect), 35 min, 3 times/week, 8 weeks | 1:2 |
| |||||||
| Sarol et al. (2015) [68] | Prospective cohort, IV | School | Weak | 4–18 years, ASD | Total n = 59 | Movement program similar to locomotor, object control and balance, 120 min, 2 times/week, 8 weeks | NR |
| Henderson et al. (2016) [69] | Prospective cohort, IV | School | Weak | 5–12 years, ASD | Total n = 37 | Locomotor and object control, 40 min, 2 times/week, 20 weeks | 1:3 |
| Toscano et al. (2018) [70] | RCT, II | School | Weak | 4–18 years, ASD | Total n = 64, EG:46, CG:16 | Strength, coordination and balance, 40 min, 2 times/week, 48 weeks | 1:3 |
| Chiva-Bartoll et al. (2021) [71] | Non-randomized trial, III | School | Weak | 10.13 years (mean), ASD | Total n = 25 (19), EG:15, CG:10 | Physical education program, 60 min, 2 times/week, 28 weeks | 1:3–5 |
| Fahimeh et al. (2022) [72] | Non-randomized trial, III | School | Weak | 8–12 years, ASD | Total n = 30 (17), EG:15, CG:15 | Physical literacy program, 80 min, 2 times/week, 8 weeks | NR |
| Author(s) (Year) | Assessment Methods | Between-Group Differences Post-Intervention | Within-Group Differences Pre-Post Intervention | Clinical Implications |
|---|---|---|---|---|
| Motor activity intervention | ||||
| Ferguson et al. (2010) [17] | MABC | NR | NR | The APA program had a positive effect on improving motor abilities, including improvements in ball skills, manual dexterity, and balance. |
| Arzoglou et al. (2013) [18] | KTK | NR | ↑EG, NS CG | Traditional Greek dance programs improved the agility of children. |
| Hayward et al. (2016) [19] | Kicking accuracy | NA | ↑ | The soccer program improved the kicking accuracy and agility of children. |
| Cei et al. (2017) [20] | Motor skills (walking, running, catching, etc.) | NA | ↑ | Football training improved motor skills (walking, running, catching, etc.). |
| Guest et al. (2017) [21] | TGMD-2 | NA | ↑EG | Multi-sport camp activity improved the locomotor skills and object control skills of girls with ASD. |
| Pan et al. (2017) [22] | BOT-2 | NS | ↑EG | Table tennis improved the motor skills of children, compared with a control group, which was maintained for 3 months. |
| Kokaridas et al. (2018) [23] | Traverse speed Hand grip strength | ↑EG(TD) NS | NS NS | Indoor climbing had no difference in ASD between TD. |
| Sarabzadeh et al. (2019) [24] | MABC-2 | ↑EG | ↑EG, NS CG | Tai Chi Chuan training improved the balance and object control skills of children with ASD, compared with the control group. |
| Howell et al. (2021) [25] | MABC-2 | NS | ↑EG, NS, CG | The football program improved in total MABC-2, aiming, catching, and balance, but there is no change in manual dexterity. |
| Ketcheson et al. (2021) [26] | TGMD-3 | ↑EG | NR | Physical Activity Intervention improved object control skills. |
| Sansi et al. (2021) [27] | TGMD-3 | ↑EG | ↑EG, NS, CG | The inclusive physical activity program increased the motor skills of the ASD students and, improved the motor skills of the TD students and positively affected their attitudes towards the ASD students. |
| Erisin et al. (2022) [28] | BOT-2 | ↑EG | 30%↑EG, CG | Significant improvements in running speed and agility, balance, and standing long jump in EG; only the standing long jump scores failed to improve in CG significantly. |
| Fahimeh et al. (2022) [29] | BOT | ↑EG | ↑EG, NS, CG | There were significant differences between EG and CG groups and between the ICPL and Spark programs, which increased MS with children. |
| Shanker et al. (2022) [30] | BOT-2 | ↑EG | NR | Yoga programs improve the gross motor rather than fine motor proficiency of children. |
| Morales et al. (2022) [31] | TGMD-3 | ↑EG | ↑EG, NS, CG | The judo program improves the locomotor skills and gross motor compared with the control group. |
| Motor skill interventions | ||||
| Cheldavi et al. (2014) [32] | Postural ability (7 parameters and conditions) | ↑EG, CG | NR | Balance training programs improved the postural control of children. |
| Bremer et al. (2015) [33] | PDSM-2 MABC-2 VABS-II | ↑EG, CG NS NS | NR | The fundamental motor skills program improved motor skills with children, compared with the control group. |
| Samsudin et al. (2017) [34] | Throwing accuracy | ↑EG | NR | The throwing movements (lobbing) boules program improved throwing accuracy. |
| EI Shemy et al. (2018) [35] | BOT-2 | ↑EG | ↑EG, CG | Gaiting training with a rhythmic auditory program improved motor skills in children compared with the control group. |
| Navaee et al. (2018) [36] | Throwing accuracy | NS | NR | A throwing task did not improve throwing accuracy, and there was no retention compared with the control group. |
| Bo et al. (2019) [37] | TGMD-3 | NA | ↑EG | Gross motor skills improve, and the greater the degree of social impairment, the greater the improvement in children’s motor skills. |
| Tse et al. (2019) [38] | Throwing accuracy | NS | ↑EG | A throwing task had no difference between EG1, EG2, and CG; however, there was a retention significance between other groups. |
| Tse et al. (2019) [39] | Shooting scores | ↑EG1, EG2, EG3 | ↑EG1, EG2, EG3, NS, CG | A basketball task with 4 types improved retention and transfer with children. |
| Xing et al. (2020) [40] | TGMD-3 MABC-2 | ↑EG, CG NS | ↑EG, NS, CG NS | Fundamental movement skill intervention significantly improved gross motor ability and object control ability. |
| Bremer et al. (2021) [41] | TGMD-2 | ↑EG | ↑EG, NS, CG | Fundamental movement skill intervention significantly improved their movement skills. |
| Columna et al. (2021) [42] | TGMD-3 | ↑EG, CG | EG, NS, CG | Fundamental movement skill intervention significantly improved their movement skills and parents may facilitate the acquisition of skills of their children. |
| Dong et al. (2021) [43] | TGMD-3 | ↑EG, CG | ↑EG, CG | Fundamental movement skill intervention improved, and the average locomotor skill and object control skills also improved. |
| Ketcheson et al. (2021) [44] | TGMD-3 | NA | ↑EG | Fundamental movement skill intervention improved object control skill |
| Liu et al. (2021) [45] | TGMD-3 | NA | ↑EG | Fundamental movement skill intervention improved gross motor ability improved the most, followed by displacement motor ability and object control ability improved the least. |
| Bo et al. (2023) [46] | TGMD-3 MABC-2 | ↑EG, CG NS | ↑EG, NS, CG NS | Fundamental movement skill intervention significantly improved gross motor ability and object control ability. |
| Hippotherapy, equine-assisted, or simulated horse-riding interventions | ||||
| Wuang et al. (2010) [47] | BOT-2 | ↑EG, CG | ↑EG, NS, CG | The horse-riding program improved motor proficiency and sensory functions, and the effect was sustained for at least 24 weeks. |
| Gabriel et al. (2012) [48] | BOT-2 | NS | ↑ | The horse-riding program improved motor skills but did not significance compare with the control group. |
| Ajzenman et al. (2013) [49] | VABS-II Postural stability (12 COM and COP) | NA | ↑EG | The hippotherapy program improved postural stability but did not improve motor skills. |
| Gabriel et al. (2015) [50] | BOT-2 | NS | NR | The hippotherapy program improved motor skills but did not significance compare with the control group. |
| Srinivasan et al. (2015) [51] | BOT-2 | ↑CG> EG1, EG2 | NS, EG1, EG2, ↑CG | Robotic and rhythmic programs did not improve the manual coordination, body coordination, or praxis of children. |
| Borgi et al. (2016) [52] | VABS-II | NS | NR | The equine-assisted program did not improve motor skills with children, compared with the control group. |
| Taheri-Torbati et al. (2018) [53] | NoRMD NoRMS | NS NS | ↑EG1, TD1, EG2, TD2 ↑EG1, TD1, EG2, TD2 | Video and live modeling programs in similar in children with ASD and TD. There is a similarity in retention between ASD and TD. |
| Wang et al. (2022) [54] | CP-GMFQ | ↑EG | NS | Equine-assisted programs improved motor skills in children but did not have a significant effect compared with the control group. |
| Aquatic interventions | ||||
| Pan et al. (2010) [55] | HAAR | ↑ | ↑EG1 ↑EG2 | The aquatic skills program improved the swim skills of children, compared with the experiment group, and the effect was sustained for at least 10 weeks. |
| Fragala et al. (2011) [56] | YMCA Water Skills | NS | ↑EG | The aquatic skills program improved the swim skills of children compared with the control group. |
| Pan et al. (2011) [57] | HAAR | NS | ↑EG1, ↑EG2 | The aquatic skills program improved the swim skills of children compared with the control group. |
| Chu et al. (2012) [58] | HAAR | NS | ↑EG1, EG2, EG3 | Three types of aquatic skills programs did not improve swim skills with children. |
| Alaniz et al. (2017) [59] | ASC | NA | ↑EG | The aquatic skills program improved the swim skills of children. |
| Caputo et al. (2018) [60] | VABS-II | NS | ↑EG, CG | The aquatic skills program improved the swim and motor skills of children. |
| Marzouki et al. (2022) [61] | TGMD-2 | ↑EG1, EG2 | ↑EG1, ↑EG2 | The aquatic skills program improved gross motor skills was observed in both experimental groups compared with the control group. No significant between the experimental groups. |
| Vodakova et al. (2022) [62] | GMFM | NA | ↑EG | The aquatic skills program improved the gross motor skills of children. |
| Exergaming interventions | ||||
| Hitlon et al. (2014) [63] | BOT-2 | NA | NS | Exergaming programs improved the agility of children. |
| Hitlon et al. (2015) [64] | BOT-2 | NA | ↑EG | Exergaming programs improved motor performance. |
| Edward et al. (2017) [65] | TGMD-3 | NS | NS | Actual skill scores were not improved in either group. The ASD group improved in perceived skill. |
| Travers et al. (2017) [66] | BOT-2 | NA | ↑EG | Biofeedback-based video training programs improved the balance of children. |
| Caro et al. (2017) [67] | MABC-2 | ↑EG1, ↑EG2, CG | ↑EG1, ↑EG2 | Kinect program training improves the motor skills of children compared with the control group. No significant between the experimental groups. |
| Rafiei et al. (2021) [12] | Limb movements (accurate and simple-aimed) | NA | ↑EG | Froggy Bobby program training improves the motor performance of children. |
| Physical education interventions | ||||
| Sarol et al. (2015) [68] | PedsQL | NA | ↑EG | Movement programs improve the physical functionality of children. |
| Henderson et al. (2016) [69] | TGMD-2 | NA | NS | Locomotor and object control skills improve the motor skills of children. |
| Toscano et al. (2018) [70] | PH-CHQ | ↑EG | NR | Exercise programs improve the physical functionality of children compared with the control group. |
| Chiva-Bartoll et al. (2021) [71] | MABC-2 | NR | ↑EG, ↓CG | Physical education program improves manual dexterity manual and balance. However, the results in the control group decreased or remained stable. |
| Fahimeh et al. (2022) [72] | CAMSA | ↑EG | NR | Physical literacy program improves the motor competence of children. |
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2015. [Google Scholar]
- Narayan, B.A. Is motor impairment in autism spectrum disorder distinct from developmental coordination disorder? A report from the SPARK study. Phys. Ther. 2020, 100, 633–644. [Google Scholar]
- Christensen, D.L. Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sities, United States, 2012. MMWR Surveill. Summ. 2016, 70, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Gu, S.; Su, Y. A network meta-analysis of the effects of exercise intervention on social disorder in children and adolescents with autism spectrum disorder. Chin. J. Integr. Med. 2019, 38, 1719–1727. [Google Scholar]
- Zhang, Y.B. Movement Learning and Control; Beijing Sports University Press: Beijing, China, 2003. [Google Scholar]
- Narayan, B.A. Motor impairment increases in children with autism spectrum disorder as a function of social communication, cognitive and functional impairment, repetitive behavior severity, and comorbid diagnoses: A SPARK study report. Autism Res. 2020, 14, 202–219. [Google Scholar]
- Wang, L.; Wang, Z.; Wang, H. Neural mechanisms of motor developmental deficits in children with autism. Adv. Psychol. Sci. 2021, 29, 1239–1250. [Google Scholar] [CrossRef]
- Pang, Y.; Bo, J.; Dong, L. A review of research on motor development disorder in children with autism spectrum disorders. China Spec. Edu. 2018, 4, 46–52. [Google Scholar]
- Dong, L.; Bo, J.; Shen, B.; Pang, Y.; Song, Y.; Xing, Y. Effects of a 10-week motor intervention on basic motor skills and social interaction skills in children with autism. Chin. J. Integr. Med. 2021, 40, 171–180. [Google Scholar]
- Floris, D.L.; Barber, A.D.; Nebel, M.B.; Martinelli, M.; Lai, M.-C.; Crocetti, D.; Baron-Cohen, S.; Suckling, J.; Pekar, J.J.; Mostofsky, S.H. Atypical lateralization of motor circuit functional connectivity in children with au-tism is associated with motor deficits. Mol. Autism 2016, 7, 35. [Google Scholar] [CrossRef] [PubMed]
- Nebel, M.B.; Eloyan, A.; Nettles, C.A.; Sweeney, K.L.; Ament, K.; Ward, R.E.; Choe, A.S.; Barber, A.D.; Pekar, J.J.; Mostofsky, S.H. Intrinsic visual-motor synchrony correlates with social deficits in autism. Biol. Psychiat. 2016, 79, 633–641. [Google Scholar] [CrossRef]
- Rafiei Milajerdi, H.; Sheikh, M.; Najafabadi, M.G.; Saghaei, B.; Naghdi, N.; Dewey, D. The effects of physical activity and exergaming on motor skills and executive functions in children with autism spectrum disorder. Games Health J. 2021, 10, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Rafie, F.; Ghasemi, A.; Jalali, S. Effect of exercise intervention on the perceptual-motor skills in adolescents with autism. J. Sports Med. Fit. 2016, 57, 53–59. [Google Scholar] [CrossRef]
- Zhou, M. A Study on the Effect of Peer Intervention Method on Motor Skills of Children with Autism in Small Basketball. Chinese Society of Sports Science. In Abstracts of the 13th National Sports Science Conference—Special Report; Tianjin University of Sport: Tianjin, China, 2023. [Google Scholar]
- Ruggeri, A.; Dancel, A.; Johnson, R.; Sargent, B. The effect of motor and physical activity intervention on motor outcomes of children with autism spectrum disorder: A systematic review. Autism 2020, 24, 544–568. [Google Scholar] [CrossRef]
- Healy, S.; Nacario, A.; Braithwaite, R.E.; Hopper, C. The effect of physical activity interventions on youth with autism spectrum disorder: A meta-analysis. Autism Res. 2018, 11, 818–833. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, L. The Effects of an Adapted Physical Activity Program on Motor Performance and Behaviour of Children with Autism Spectrum Disorder; University of Stellenbosch: Stellenbosch, South Africa, 2010. [Google Scholar]
- Arzoglou, D.; Tsimaras, V.; Kotsikas, G.; Fotiadou, E.; Sidiropoulou, M.; Proios, M.; Bassa, E. The effect of traditional dance training program on neuromuscular coordination of individuals with autism. J. Phy. Edu. Sport 2013, 13, 563. [Google Scholar]
- Hayward, L.M.; Fragala-pinkham, M.; Johnson, K.; Torres, A.A. A community-based, adaptive soccer program for children with autism: Design, implementation, and evaluation. Palaestra 2016, 30, 44–50. [Google Scholar]
- Cei, A.; Franceschi, P.; Rosci, M.; Sepio, D.; Ruscello, B. Motor and psychosocial development in children with autism spectrum disorder through soccer. Int. J. Sport Psychol. 2017, 48, 485–507. [Google Scholar]
- Guest, L.; Balogh, R.; Dogra, S.; Lloyd, M. Examining the impact of a multi-sport camp for girls ages 8–11 with autism spectrum dis-order. Ther. Recreat. J. 2017, 51, 109–126. [Google Scholar]
- Pan, C.Y.; Chu, C.H.; Tsai, C.L.; Sung, M.C.; Huang, C.Y.; Ma, W.Y. The impacts of physical activity intervention on physical and cognitive outcomes in children with autism spectrum disorder. Autism 2017, 21, 190–202. [Google Scholar] [CrossRef] [PubMed]
- Kokaridas, D.; Demerouti, I.; Margariti, P.; Charalampos, K. The effect of an indoor climbing program on improving handgrip strength and traverse speed of children with and without autism spectrum disorder. Palaestra 2018, 32, 1–8. [Google Scholar]
- Sarabzadeh, M.; Azari, B.B.; Helalizadeh, M. The effect of six weeks of Tai Chi Chuan training on the motor skills of children with Autism Spectrum Disorder. J. Bodyw. Mov. Ther. 2019, 23, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Howells, K.; Sivaratnam, C.; Lindor, E.; He, J.; Hyde, C.; McGillivray, J.; Wilson, R.B.; Rinehart, N. Can a community-based football program benefit motor ability in children with autism spectrum disorder? A pilot evaluation considering the role of social impairments. J. Autism. Dev. Disord. 2021, 52, 402–413. [Google Scholar] [CrossRef] [PubMed]
- Ketcheson, L.; Staples, K.; Pitchford, E.A.; Loetzner, F. Promoting positive health outcomes in an urban community-based physical activity intervention for preschool aged children on the autism spectrum. J. Autism. Dev. Disord. 2023, 53, 633–646. [Google Scholar] [CrossRef] [PubMed]
- Sansi, A.; Nalbant, S.; Ozer, D. Effects of an inclusive physical activity program on the motor skills, social skills and attitudes of students with and without autism spectrum disorder. J. Autism. Dev. Disord. 2021, 51, 2254–2270. [Google Scholar] [CrossRef] [PubMed]
- Ersin, A.; Gonca, I.; Murat, A. Effects of a 12-week structured circuit exercise program on physical fitness levels of children with autism spectrum condition and typically developing children. Int. J. Devl. Disabil. 2022, 68, 500–510. [Google Scholar]
- Fahimeh, H.; Shahnaz, S.; Seyed, H.S.; Mahmoud, S. Playing games can improve physical performance in children with autism. Int. J. Devl. Disabil. 2022, 68, 219–226. [Google Scholar]
- Shanker, S.; Pradhan, B. Effect of yoga on the motor proficiency of children with autism spectrum disorder and the feasibility of its inclusion in special school environments. Adapt. Phys. Act. Q. 2022, 39, 247–267. [Google Scholar] [CrossRef] [PubMed]
- Morales, J.; Pierantozzi, E.; Fukuda, D.H.; Garcia, V.; Guerra-Balic, M.; Sevilla-Sánchez, M.; Carballeira, E. Improving motor skills and psychosocial behaviors in children with autism spectrum disorder through an adapted judo program. Front. Psychol. 2022, 13, 1067310. [Google Scholar] [CrossRef] [PubMed]
- Cheldavi, H.; Shakerian, S.; Boshehri, S.N.S.; Zarghami, M. The effects of balance training intervention on postural control of children with autism spectrum disorder: Role of sensory information. Res. Autism Spect. Dis. 2014, 8, 8–14. [Google Scholar] [CrossRef]
- Bremer, E.; Robert, B.; Meghann, L. Effectiveness of a fundamental motor skill intervention for 4-year-old children with au-tism spectrum disorder: A pilot study. Autism 2015, 19, 980–991. [Google Scholar] [CrossRef] [PubMed]
- Samsudin, N.A.; Low, J.F.L. The effects of different focus of attention on throwing skills among autistic spectrum disorder chil-dren. Malays. J. Fundam. Appl. 2017, 9, 1312–1322. [Google Scholar] [CrossRef]
- El, S.; Samah, A.; Mohamed, S.E. The impact of auditory rhythmic cueing on gross motor skills in children with autism. J. Phy. Ther. Sci. 2018, 30, 1063–1068. [Google Scholar]
- Navaee, S.A.; Abedanzadeh, R.; Salar, S.; Sharif, M.R. The effects of positive normative feedback on-learning a throwing task among children with autism spectrum disorder. Nurs. Midwifery Stud. 2018, 7, 87–89. [Google Scholar]
- Bo, J.; Pang, Y.; Dong, L.; Xing, Y.; Xiang, Y.; Zhang, M.; Shen, B. Brief report: Does social functioning moderate the motor outcomes of a phys-ical activity program for children with autism spectrum disorders—A pilot study. J. Autism Dev. Disord. 2019, 49, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Tse, A.C.Y. Effects of attentional focus on motor learning in children with autism spectrum disorder. Autism 2019, 23, 405–412. [Google Scholar] [CrossRef]
- Tse, A.C.Y.; Masters, R.S.W. Improving motor skill acquisition through analogy in children with autism spectrum disorders. Psychol. Sport Exerc. 2019, 41, 63–69. [Google Scholar] [CrossRef]
- Xing, Y. The influence of gross motor skill learning on fundamental movement skill of children with autism spectrum disorder. J. Capit. Ins. Phys. Edu. 2020, 32, 13–17. [Google Scholar]
- Bremer, E.; Lloyd, M. Baseline behavior moderates movement skill intervention outcomes among young children with autism spectrum disorder. Autism 2021, 25, 2025–2033. [Google Scholar] [CrossRef]
- Columna, L.; Prieto, L.A.; Beach, P.; Russo, N.; Foley, J.T. A randomized feasibility trial of a fundamental motor skill parent-mediated intervention for children with autism spectrum disorders. Int. J. Environ. Res. Public Health 2021, 18, 12398. [Google Scholar] [CrossRef]
- Dong, L.; Shen, B.; Pang, Y.L.; Zhang, M.; Xiang, Y.; Xing, Y.; Wright, M.; Li, D.; Bo, J. FMS effects of a motor program for children with autism spectrum disorders. Percept. Motor Ski. 2021, 128, 1421–1442. [Google Scholar] [CrossRef]
- Ketcheson, L.; Felzer-Kim, I.T.; Hauck, J.L. Promoting adapted physical activity regardless of language ability in young children with autism spectrum disorder. Res. Q. Exerc. Sport 2021, 92, 813–823. [Google Scholar] [CrossRef]
- Liu, R. Study on the Effects of Large Muscle Movements on Motor and Social Communication Skills of Children with Autism; Jiangxi Normal University: Nanchang, China, 2021. [Google Scholar]
- Bo, J.; Shen, B.; Pang, Y.L.; Zhang, M.; Xiang, Y.; Dong, L.; Song, Y.; Lasutschinkow, P.; Dillahunt, A.; Li, D. Transfer and retention effects of a motor program in children with autism spectrum disorders. Adapt. Phys. Act. Q. 2023, 41, 88–106. [Google Scholar] [CrossRef]
- Wang, Y.P.; Wang, C.; Huang, M.; Su, C.Y. The effectiveness of simulated developmental horse-riding program in children with autism. Adapt. Phys. Act. Q. 2010, 27, 113. [Google Scholar] [CrossRef]
- Gabriels, R.L.; Agnew, J.A.; Holt, K.D.; Shoffner, A.; Zhaoxing, P.; Ruzzano, S.; Clayton, G.H.; Mesibov, G. Pilot study measuring the effects of therapeutic horseback riding on school-age children and adolescents with autism spectrum disorders. Res. Autism Spect. Dis. 2012, 6, 578. [Google Scholar] [CrossRef]
- Ajzenman, H.F.; Standeven, J.W.; Shurtleff, T.L. Effect of hippotherapy on motor control, adaptive behaviors, and participa-tion in children with autism spectrum disorder: A pilot study. Am. J. Occup. Ther. 2013, 67, 653–663. [Google Scholar] [CrossRef] [PubMed]
- Gabriels, R.L.; Pan, Z.; Dechant, B.; Agnew, J.A.; Brim, N.; Mesibov, G. Randomized controlled trial of therapeutic horseback riding in children and adoles-cents with autism spectrum disorder. J. Am. Child. Psy. 2015, 54, 541–549. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, S.M.; Maninderjit, K.; Park, I.K.; Gifford, T.D.; Marsh, K.L.; Bhat, A.N. The effects of rhythm and robotic interventions on the imitation/praxis, inter-personal syn-chrony, and motor performance of children with autism spectrum disorder (ASD): A pilot randomized controlled trial. Autism Res. Treat. 2015, 2015, 736516. [Google Scholar]
- Borgi, M.; Loliva, D.; Cerino, S.; Chiarotti, F.; Venerosi, A.; Bramini, M.; Nonnis, E.; Marcelli, M.; Vinti, C.; Chiara, D.S.; et al. Effectiveness of a standardized equine-assisted therapy program for children with autism spectrum disorder. J. Autism Dev. Disord. 2016, 46, 1–9. [Google Scholar] [CrossRef]
- Taheri-Torbati, H.; Sotoodeh, M.S. Using video and live modelling to teach motor skill to children with autism spectrum disor-der. Int. J. Incl. Educ. 2018, 23, 405–418. [Google Scholar] [CrossRef]
- Wang, X.; Tang, S.; Shi, X. Equestrian sport curative effect and the application of the auxiliary intervention in autism spectrum disorder children study. J Contemp. Sports Sci. Technol. 2022, 12, 23–26. [Google Scholar]
- Pan, C.Y. Effects of water exercise swimming program on aquatic skills and social behaviors in children with autism spectrum disorders. Autism 2010, 14, 9–28. [Google Scholar] [CrossRef]
- Fragala-Pinkham, M.A.; Haley, S.M.; O’Neil Margaret, E. Group swimming and aquatic exercise programme for children with autism spectrum disorders: A pilot study. Dev. Neurorehabil. 2011, 14, 230–241. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.Y. The efficacy of an aquatic program on physical fitness and aquatic skills in children with and without autism spec-trum disorders. Res. Autism Spect. Dis. 2011, 5, 657–665. [Google Scholar] [CrossRef]
- Chu, C.H.; Pan, C.Y. The effect of peer- and sibling-assisted aquatic program on interaction behaviors and aquatic skills of children with autism spectrum disorders and their peers/siblings. Res. Autism Spect. Dis. 2012, 6, 1211–1223. [Google Scholar] [CrossRef]
- Alaniz, M.L.; Rosenberg, S.S.; Beard, N.R. The effectiveness of aquatic group therapy for improving water safety and social interactions in children with autism spectrum disorder: A pilot program. J. Autism Dev. Dis. 2017, 47, 4006–4017. [Google Scholar] [CrossRef]
- Caputo, G.; Ippolito, G.; Mazzotta, M.; Sentenza, L.; Muzio, M.R.; Salzano, S.; Conson, M. Effectiveness of a multisystem aquatic therapy for children with autism spectrum disorders. J. Autism Dev. Disord. 2018, 48, 1945–1956. [Google Scholar] [CrossRef] [PubMed]
- Marzouki, H.; Soussi, B.; Selmi, O.; Hajji, Y.; Marsigliante, S.; Bouhlel, E.; Muscella, A.; Weiss, K.; Knechtle, B. Effects of aquatic training in children with autism spectrum disorder. Biology 2022, 11, 657. [Google Scholar] [CrossRef]
- Vodakova, E.; Chatziioannou, D.; Jesina, O.; Kudlacek, M. The effect of halliwick method on aquatic skills of children with au-tism spectrum disorder. Int. J. Environ. Res. Public Health 2022, 19, 16250. [Google Scholar] [CrossRef] [PubMed]
- Hilton, C.; Cumpata, K.; Klohr, C.; Gaetke, S.; Artner, A.; Johnson, H.; Dobbs, S. Effects of exergaming on executive function and motor skills in children with autism spectrum disorder: A pilot study. Am. J. Occup. Ther. 2014, 68, 57. [Google Scholar] [CrossRef]
- Hilton, C.L. Exergaming to improve physical and mental fitness in children and adolescents with autism spectrum disorders: Pilot study. Int. J. Sports Exerc. Med. 2015, 1, 017. [Google Scholar] [CrossRef]
- Edwards, J.; Jeffrey, S.; May, T.; Rinehart, N.J.; Barnett, L.M. Does playing a sports active video game improve object control skills of children with autism spectrum disorder? J. Sport Health Sci. 2017, 6, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Travers, B.G.; Mason, A.H.; Mrotek, L.A.; Ellertson, A.; Dean, D.C.; Engel, C.; Gomez, A.; Dadalko, O.I.; McLaughlin, K. Biofeedback-based, videogame balance training in autism. J. Autism Dev. Disord. 2018, 48, 163–175. [Google Scholar] [CrossRef]
- Caro, K.; Tentori, M.; Martinez-Garcia, A.I.; Alvelais, M. Using the Froggy Bobby exergame to support eye-body coordination development of children with severe autism. Int. J. Hum.-Comput. St. 2017, 105, 12–27. [Google Scholar] [CrossRef]
- Sarol, H.; Imen, Z. The Effects of adapted recreational physical activity on the life quality of individuals with autism. Anthro-pologist 2015, 21, 522–527. [Google Scholar] [CrossRef]
- Henderson, H.; Fuller, A.; Noren, S.; Stout, V.M.; Williams, D. The effects of a physical education program on the motor skill performance of chil-dren with autism spectrum disorder. Palaestra 2016, 30, 1–11. [Google Scholar]
- Toscano, C.V.A.; Carvalho, H.M.; José, P.F. Exercise Effects for children with autism spectrum disorder: Metabolic health, au-tistic traits, and quality of life. Percept. Motor Ski. 2018, 125, 126–146. [Google Scholar] [CrossRef]
- Chiva-Bartoll, O.; Maravé-Vivas, M.; Salvador-García, C.; Valverde-Esteve, T. Impact of a physical education service-learning programme on ASD children: A mixed-methods approach. Child. Youth Serv. Rev. 2021, 126, 106008. [Google Scholar] [CrossRef]
- Fahimeh, H.; Mahmoud, S.; Shahnaz, S. The physical literacy and children with autism, Early Child. Dev. Care 2022, 192, 470–480. [Google Scholar]
- Wang, Z. ACSM Guidelines for Exercise Testing and Prescription, 10th ed.; Beijing Sport University: Beijing, China, 2019. [Google Scholar]
- Li, F.; Harmer, P.; Fitzgerald, K.; Eckstrom, E.; Stock, R.; Galver, J.; Maddalozzo, G.; Batya, S.S. Tai Chi and postural stability in patients with Parkinson’s disease. N. Engl. J. Med. 2012, 366, 511–519. [Google Scholar] [CrossRef]
- Sowa, M.; Meulenbroek, R. Effects of physical exercise on autism spectrum disorders: A meta-analysis. Res. Autism Spect. Dis-ord. 2012, 6, 46–57. [Google Scholar] [CrossRef]
- Schmitz, O.S.; Mcfadden, B.A.; Golem, D.L.; Pellegrino, J.K.; Walker, A.J.; Sanders, D.J.; Arent, S.M. The effects of exercise dose on stereotypical behavior in children with autism. Med. Sci. Sports Exerc. 2017, 49, 983–990. [Google Scholar] [CrossRef]
- Kern, L.; Koegel, R.L.; Dunlap, G. The influence of vigorous versus mild exercise on autistic stereotyped behaviors. J. Autism Dev. Disord. 1984, 14, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Levinson, L.J.; Reid, G. The effects of exercise intensity on the stereotypic behaviors of individuals with autism. Adapt. Phys. Activ. Q. 1993, 10, 255–268. [Google Scholar] [CrossRef]
- Huang, J.; Du, C.; Liu, J.; Tan, G. Meta-analysis on intervention effects of physical activities on children and adolescents with autism. Int. J. Environ. Res. Public Health 2020, 17, 1950. [Google Scholar] [CrossRef]
- Jachyra, P.; Renwick, R.; Gladstone, B.; Anagnostou, E.; Gibson, B.E. Physical activity participation among adolescents with autism spectrum disorder. Autism 2021, 25, 613–626. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xing, Y.; Wu, X. Effects of Motor Skills and Physical Activity Interventions on Motor Development in Children with Autism Spectrum Disorder: A Systematic Review. Healthcare 2025, 13, 489. https://doi.org/10.3390/healthcare13050489
Xing Y, Wu X. Effects of Motor Skills and Physical Activity Interventions on Motor Development in Children with Autism Spectrum Disorder: A Systematic Review. Healthcare. 2025; 13(5):489. https://doi.org/10.3390/healthcare13050489
Chicago/Turabian StyleXing, Yu, and Xueping Wu. 2025. "Effects of Motor Skills and Physical Activity Interventions on Motor Development in Children with Autism Spectrum Disorder: A Systematic Review" Healthcare 13, no. 5: 489. https://doi.org/10.3390/healthcare13050489
APA StyleXing, Y., & Wu, X. (2025). Effects of Motor Skills and Physical Activity Interventions on Motor Development in Children with Autism Spectrum Disorder: A Systematic Review. Healthcare, 13(5), 489. https://doi.org/10.3390/healthcare13050489





