Implementation of the Maynard-Based Risk Assessment Model for Venous Thromboembolism Inpatient Prophylaxis: A Before-and-After Study
Highlights
- The implementation of the Maynard risk assessment model impaired the application of prophylactic measures in orthopedic patients.
- The Maynard risk assessment model showed limited discriminative performance.
- There is a need to enhance the discriminatory performance of the Maynard risk assessment model.
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| VTE | Venous Thromboembolism |
| DVT | Deep Vein Thrombosis |
| PE | Pulmonary Embolism |
| BMI | Body Mass Index |
| INR | International Normalized Ratio |
| SPSS | Statistical Package for the Social Sciences |
| CAAE | Brazilian Ethical Review Registration System |
References
- Konstantinides, S.V.; Meyer, G.; Becattini, C.; Bueno, H.; Geersing, G.J.; Harjola, V.P.; Huisman, M.V.; Humbert, M.; Jennings, C.S.; Jiménez, D.; et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur. Heart J. 2020, 41, 543–603. [Google Scholar] [CrossRef]
- Lutsey, P.L.; Zakai, N.A. Epidemiology and prevention of venous thromboembolism. Nat. Rev. Cardiol. 2023, 20, 248–262. [Google Scholar] [CrossRef]
- Neeman, E.; Liu, V.; Mishra, P.; Thai, K.K.; Xu, J.; Clancy, H.A.; Schlessinger, D.; Liu, R. Trends and risk factors for venous thromboembolism among hospitalized medical patients. JAMA Netw. Open 2022, 5, e2240373. [Google Scholar] [CrossRef]
- Brasil. Ministério da Saúde. DATASUS: Sistema de Informações Sobre Mortalidade; Ministério da Saúde: Brasília, Brazil, 2023. Available online: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sim/cnv/obt10uf.def (accessed on 2 December 2023).
- Albricker, A.C.L.; Freire, C.M.V.; Santos, S.N.D.; Alcantara, M.L.; Saleh, M.H.; Cantisano, A.L.; Teodoro, J.A.R.; Porto, C.L.L.; Amaral, S.I.D.; Veloso, O.C.G.; et al. Joint guideline on venous thromboembolism—2022. Arq. Bras. Cardiol. 2022, 118, 797–857. [Google Scholar] [CrossRef]
- Wiercioch, W.; Nieuwlaat, R.; Akl, E.A.; Kunkle, R.; Alexander, K.E.; Cuker, A.; Rajasekhar, A.; Alonso-Coello, P.; Anderson, D.R.; Bates, S.M.; et al. Methodology for the American Society of Hematology VTE guidelines: Current best practice, innovations, and experiences. Blood Adv. 2020, 4, 2351–2365. [Google Scholar] [CrossRef]
- Joint Commission International; National Quality Forum. National Consensus Standards for the Prevention and Care of Deep Vein Thrombosis Project; Joint Commission International: Oakbrook Terrace, IL, USA, 2023; Available online: https://www.jointcommission.org/measurement/measures/venous-thromboembolism/ (accessed on 20 December 2023).
- Eck, R.J.; Elling, T.; Sutton, A.J.; Wetterslev, J.; Gluud, C.; van der Horst, I.C.C.; Gans, R.O.B.; Meijer, K.; Keus, F. Anticoagulants for Thrombosis Prophylaxis in Acutely Ill Patients Admitted to Hospital: Systematic Review and Network Meta-Analysis. BMJ 2022, 378, e070022. [Google Scholar] [CrossRef] [PubMed]
- Lam, B.D.; Dodge, L.E.; Datta, S.; Rosovsky, R.P.; Robertson, W.; Lake, L.; Reyes, N.; Adamski, A.; Abe, K.; Panoff, S.; et al. Venous Thromboembolism Prophylaxis for Hospitalized Adult Patients: A Survey of U.S. Health Care Providers on Attitudes and Practices. Res. Pract. Thromb. Haemost. 2023, 7, 102168. [Google Scholar] [CrossRef]
- Al-Mugheed, K.; Bayraktar, N. Knowledge, Risk Assessment, Practices, Self-Efficacy, Attitudes, and Behaviours Towards Venous Thromboembolism Among Nurses: A Systematic Review. Nurs. Open 2023, 10, 6033–6044. [Google Scholar] [CrossRef] [PubMed]
- Kahn, S.R.; Morrison, D.R.; Diendéré, G.; Piché, A.; Filion, K.B.; Klil-Drori, A.J.; Douketis, J.D.; Emed, J.; Roussin, A.; Tagalakis, V.; et al. Interventions for Implementation of Thromboprophylaxis in Hospitalized Patients at Risk for Venous Thromboembolism. Cochrane Database Syst. Rev. 2018, 4, CD008201. [Google Scholar] [CrossRef] [PubMed]
- Caprini, J.A.; Arcelus, J.I.; Hasty, J.H.; Tamhane, A.C.; Fabrega, F. Clinical Assessment of Venous Thromboembolic Risk in Surgical Patients. Semin. Thromb. Hemost. 1991, 17, 304–312. [Google Scholar]
- Barbar, S.; Noventa, F.; Rossetto, V.; Ferrari, A.; Brandolin, B.; Perlati, M.; De Bon, E.; Tormene, D.; Pagnan, A.; Prandoni, P. A Risk Assessment Model for the Identification of Hospitalized Medical Patients at Risk for Venous Thromboembolism: The Padua Prediction Score. J. Thromb. Haemost. 2010, 8, 2450–2457. [Google Scholar] [CrossRef]
- Pandor, A.; Tonkins, M.; Goodacre, S.; Clowes, M.; Griffin, X.L.; Holland, M.; Hunt, B.J.; de Wit, K.; Horner, D. Risk Assessment Models for Venous Thromboembolism in Hospitalised Adult Patients: A Systematic Review. BMJ Open 2021, 11, e045672. [Google Scholar] [CrossRef] [PubMed]
- Maynard, G.A.; Morris, T.A.; Jenkins, I.H.; Stone, S.; Lee, J.; Renvall, M.; Fink, E.; Schoenhaus, R. Optimizing Prevention of Hospital-Acquired Venous Thromboembolism (VTE): Prospective Validation of a VTE Risk Assessment Model. J. Hosp. Med. 2010, 5, 10–18. [Google Scholar] [CrossRef]
- Maynard, G. Preventing Hospital-Associated Venous Thromboembolism: A Guide for Effective Quality Improvement, 2nd ed.; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2016; pp. 1–79. [Google Scholar]
- Leal, L.F.; Falavigna, M.; Gazzana, M.B.; Maccari, J.G.; Ghizzoni, F.; Alves, D.; Duncan, B.B.; Ribeiro, R.A. Protocol Implementation for Venous Thromboembolism Prophylaxis: A Before-and-After Study in Medical and Surgical Patients. J. Bras. Pneumol. 2020, 46, e20180325. [Google Scholar] [CrossRef]
- Ximena, J.B.; Koh, I.; Lutsey, P.L.; Walker, R.F.; Roetker, N.S.; Wilkinson, K.; Smith, N.L.; Plante, T.B.; Repp, A.B.; Holmes, C.E.; et al. Venous Thrombosis Risk During and After Medical and Surgical Hospitalizations: The Medical Inpatient Thrombosis and Hemostasis (MITH) Study. J. Thromb. Haemost. 2022, 20, 1645–1652. [Google Scholar] [CrossRef]
- Fuzinatto, F.; Waldemar, F.S.; Wajner, A.; Elias, C.A.; Fernandez, J.F.; Hopf, J.L.; Barreto, S.S. A Clinical Decision Support System for Venous Thromboembolism Prophylaxis at a General Hospital in a Middle-Income Country. J. Bras. Pneumol. 2013, 39, 138–146. [Google Scholar] [CrossRef][Green Version]
- Stuck, A.K.; Spirk, D.; Schaudt, J.; Kucher, N. Risk Assessment Models for Venous Thromboembolism in Acutely Ill Medical Patients: A Systematic Review. Thromb. Haemost. 2017, 117, 801–808. [Google Scholar] [CrossRef] [PubMed]
- Hayssen, H.; Cires-Drouet, R.; Englum, B.; Nguyen, P.; Sahoo, S.; Mayorga-Carlin, M.; Siddiqui, T.; Turner, D.; Yesha, Y.; Sorkin, J.D.; et al. Systematic Review of Venous Thromboembolism Risk Categories Derived from Caprini Score. J. Vasc. Surg. Venous Lymphat. Disord. 2022, 10, 1401–1409.e7. [Google Scholar] [CrossRef] [PubMed]
- Schünemann, H.J.; Cushman, M.; Burnett, A.E.; Kahn, S.R.; Beyer-Westendorf, J.; Spencer, F.A.; Rezende, S.M. American Society of Hematology 2018 Guidelines for Management of Venous Thromboembolism: Prophylaxis for Hospitalized and Nonhospitalized Medical Patients. Blood Adv. 2018, 2, 3198–3225. [Google Scholar] [CrossRef] [PubMed]
- Henke, P.K.; Kahn, S.R.; Pannucci, C.J.; Secemsky, E.A.; Evans, N.S.; Khorana, A.A.; Creager, M.A.; Pradhan, A.D.; American Heart Association Advocacy Coordinating Committee. Call to Action to Prevent Venous Thromboembolism in Hospitalized Patients: A Policy Statement from the American Heart Association. Circulation 2020, 141, e914–e931. [Google Scholar] [CrossRef]
- Mehta, Y.; Bhave, A. A Review of Venous Thromboembolism Risk Assessment Models for Different Patient Populations: What We Know and Don’t! Medicine 2023, 102, e32398. [Google Scholar] [CrossRef] [PubMed]
- Simon, S.J.; Patell, R.; Zwicker, J.I.; Kazi, D.S.; Hollenbeck, B.L. Venous Thromboembolism in Total Hip and Total Knee Arthroplasty. JAMA Netw. Open 2023, 6, e2345883. [Google Scholar] [CrossRef] [PubMed]
- da Silva, L.M.; Lima, H.O.; Ferrer, R.; Ho, A.M.; Silveira, S.Q.; Abib, A.C.V.; Bellicieri, F.N.; Camire, D.; Mittermayer, O.; Botelho, K.K.; et al. Comparison of Strategies for Adherence to Venous Thromboembolism Prophylaxis in High-Risk Surgical Patients: A Before and After Intervention Study. BMJ Open Qual. 2021, 10, e001583. [Google Scholar] [CrossRef]
- Squires, J.E.; Sullivan, K.; Eccles, M.P.; Worswick, J.; Grimshaw, J.M. Are Multifaceted Interventions More Effective Than Single-Component Interventions in Changing Health-Care Professionals’ Behaviours? An Overview of Systematic Reviews. Implement. Sci. 2014, 9, 152. [Google Scholar] [CrossRef]
- Kahn, S.R.; Diendéré, G.; Morrison, D.R.; Piché, A.; Filion, K.B.; Klil-Drori, A.J.; Douketis, J.; Emed, J.; Roussin, A.; Tagalakis, V.; et al. Effectiveness of Interventions for the Implementation of Thromboprophylaxis in Hospitalised Patients at Risk of Venous Thromboembolism: An Updated Abridged Cochrane Systematic Review and Meta-Analysis of Randomised Controlled Trials. BMJ Open 2019, 9, e024444. [Google Scholar] [CrossRef]
- Huang, X.; Zhou, S.; Ma, X.; Jiang, S.; Xu, Y.; You, Y.; Qu, J.; Shang, H.; Lu, Y. Effectiveness of an Artificial Intelligence Clinical Assistant Decision Support System to Improve the Incidence of Hospital-Associated Venous Thromboembolism: A Prospective, Randomised Controlled Study. BMJ Open Qual. 2023, 12, e002267. [Google Scholar] [CrossRef] [PubMed]

| Phases | Variables | Total (n = 772) | Clinical (n = 340) | Orthopedic Surgical (n = 217) | Non-Orthopedic Surgical (n = 215) | p-Value 1 |
|---|---|---|---|---|---|---|
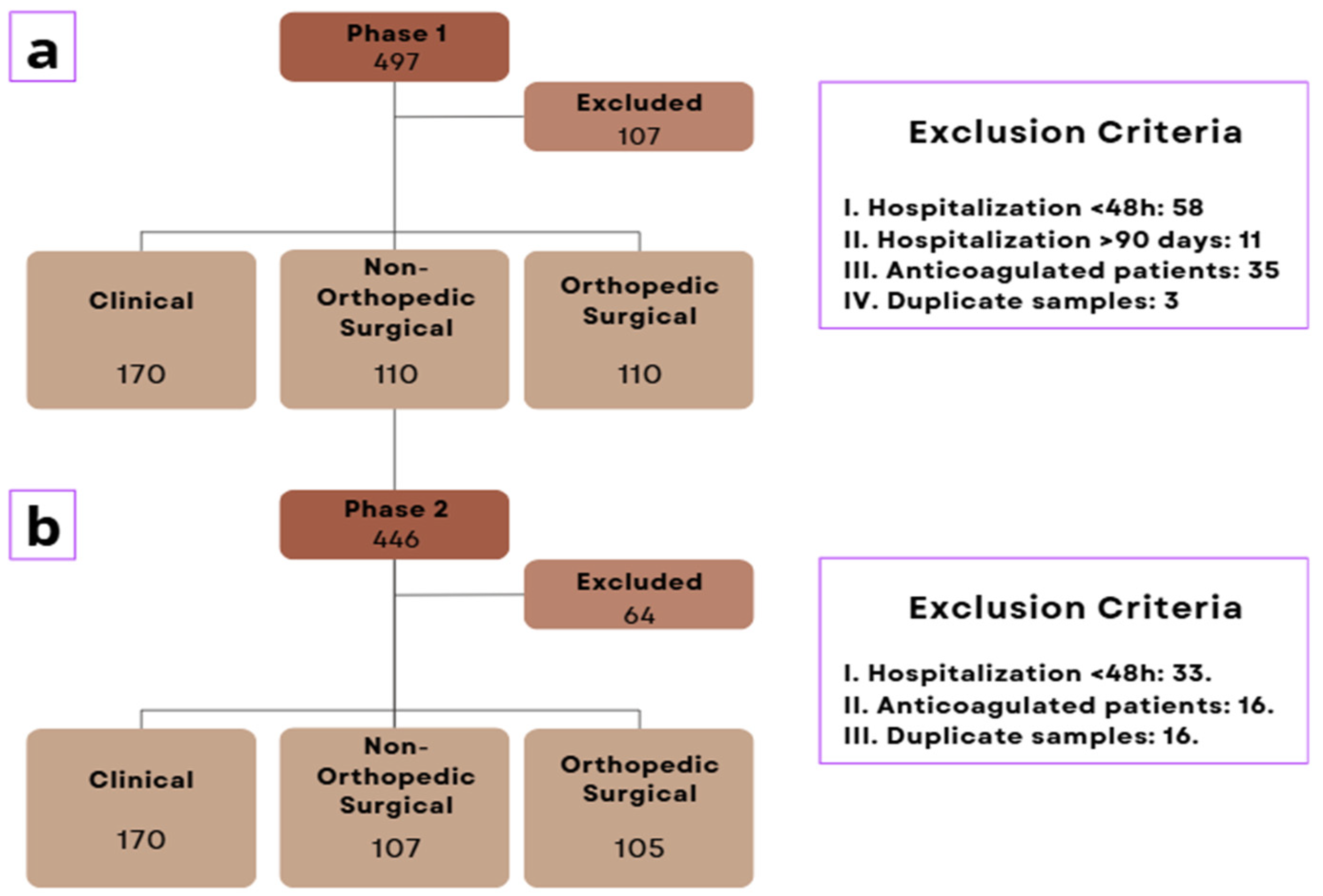
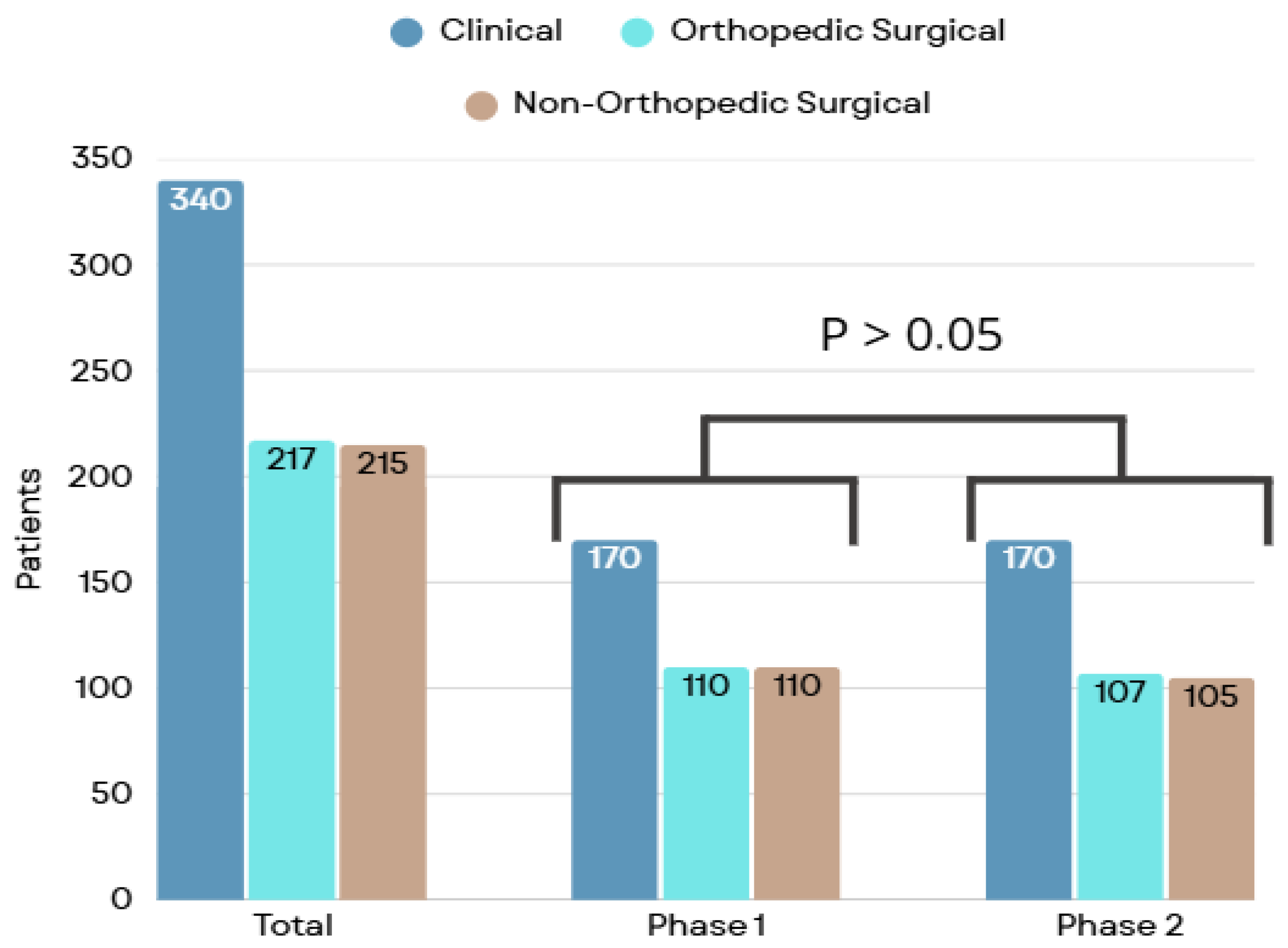
| Phase 1 | n | 390 | 170 | 110 | 110 | |
| Age (years) | 62.0 [46.0–76.0] | 64.0 [46.0–79.0] | 63.5 [47.0–76.0] | 56.0 [43.0–66.0] | <0.01 | |
| Female Sex | 237 (59.8) | 107 (62.9) | 70 (63.6) | 60 (54.5) | 0.28 | |
| White Color Ethnicity | 379 (97.1) | 167 (98.2) | 108 (98.2) | 104 (94.5) | 0.75 | |
| BMI (kg/m2) | 26.1 [23.4–29.0] | 25.1 [22.6–28.6] | 26.5 [24.3–29.3] | 26.4 [23.8–30.4] | <0.01 | |
| Phase 2 | n | 382 | 170 | 107 | 105 | |
| Age (years) | 64.0 [45.0–75.0] | 67.0 [51.0–78.0] | 61.0 [44.5–75.0] | 59.0 [41.0–70.0] | <0.01 | |
| Female Sex | 195 (51.0) | 90 (52.9) | 58 (54.2) | 47 (44.8) | 0.31 | |
| White Color Ethnicity | 382 (100.0) | 170 (100.0) | 107 (100.0) | 105 (100.0) | 0.99 | |
| BMI (kg/m2) 2 | 26.4 [23.1–30.7] | 25.7 [22.2–30.0] | 26.8 [24.3–30.7] | 26.7 [23.8–31.4] | 0.09 |
| Phases | Variables | Total (n = 772) | Clinical (n = 340) | Orthopedic Surgical (n = 217) | Non-Orthopedic Surgical (n = 215) | p-Value 1 |
|---|---|---|---|---|---|---|
| Phase 1 | n | 390 | 179 | 110 | 110 | |
| Previous PE/DVT 2 | 19 (49.0) | 11 (6.5) | 6 (5.5) | 2 (1.8) | 0.19 | |
| Active cancer | 80 (20.5) | 36 (21.2) | 6 (5.5) | 38 (34.5) | <0.01 | |
| Hormone use | 40 (10.3) | 18 (10.6) | 14 (12.7) | 8 (7.3) | 0.41 | |
| CVC 3 | 76 (19.5) | 46 (27.2) | 8 (7.3) | 22 (20.0) | <0.01 | |
| Smoking (current/or former) | 119 (32.0) | 51 (30.0) | 26 (23.7) | 44 (40.0) | 0.08 | |
| Fracture/Trauma | 23 (5.9) | 6 (3.5) | 17 (15.5) | 0 (0.0) | <0.01 | |
| Immobility | 233 (59.7) | 103 (60.6) | 73 (66.4) | 57 (51.8) | 0.08 | |
| Phase 2 | n | 382 | 170 | 107 | 105 | |
| Previous PE/DVT 2 | 39 (10.2) | 21 (12.4) | 9 (8.4) | 9 (8.6) | 0.46 | |
| Active cancer | 110 (28.8) | 48 (28.2) | 12 (11.2) | 50 (47.6) | <0.01 | |
| Hormone use | 36 (9.4) | 14 (8.2) | 11 (10.3) | 11 (10.5) | 0.77 | |
| CVC 3 | 87 (22.8) | 52 (30.6) | 12 (11.3) | 23 (21.9) | <0.01 | |
| Smoking (current or former) | 146 (38.2) | 72 (42.4) | 30 (28.0) | 44 (41.9) | 0.04 | |
| Fracture/Trauma | 29 (7.6) | 8 (4.7) | 19 (17.8) | 2 (1.9) | <0.01 | |
| Immobility | 219 (57.3) | 92 (54.1) | 76 (71.0) | 51 (48.6) | <0.01 |
| Phases | Variables | Total (n = 772) | Clinical (n = 340) | Orthopedic Surgical (n = 217) | Non-Orthopedic Surgical (n = 215) | p-Value 1 |
|---|---|---|---|---|---|---|
| Phase 1 (n = 390) | Pádua | |||||
| Low Risk | 80 (47.1) | 80 (47.1) | - | - | - | |
| High Risk | 90 (52.9) | 90 (52.9) | - | - | ||
| Maynard | ||||||
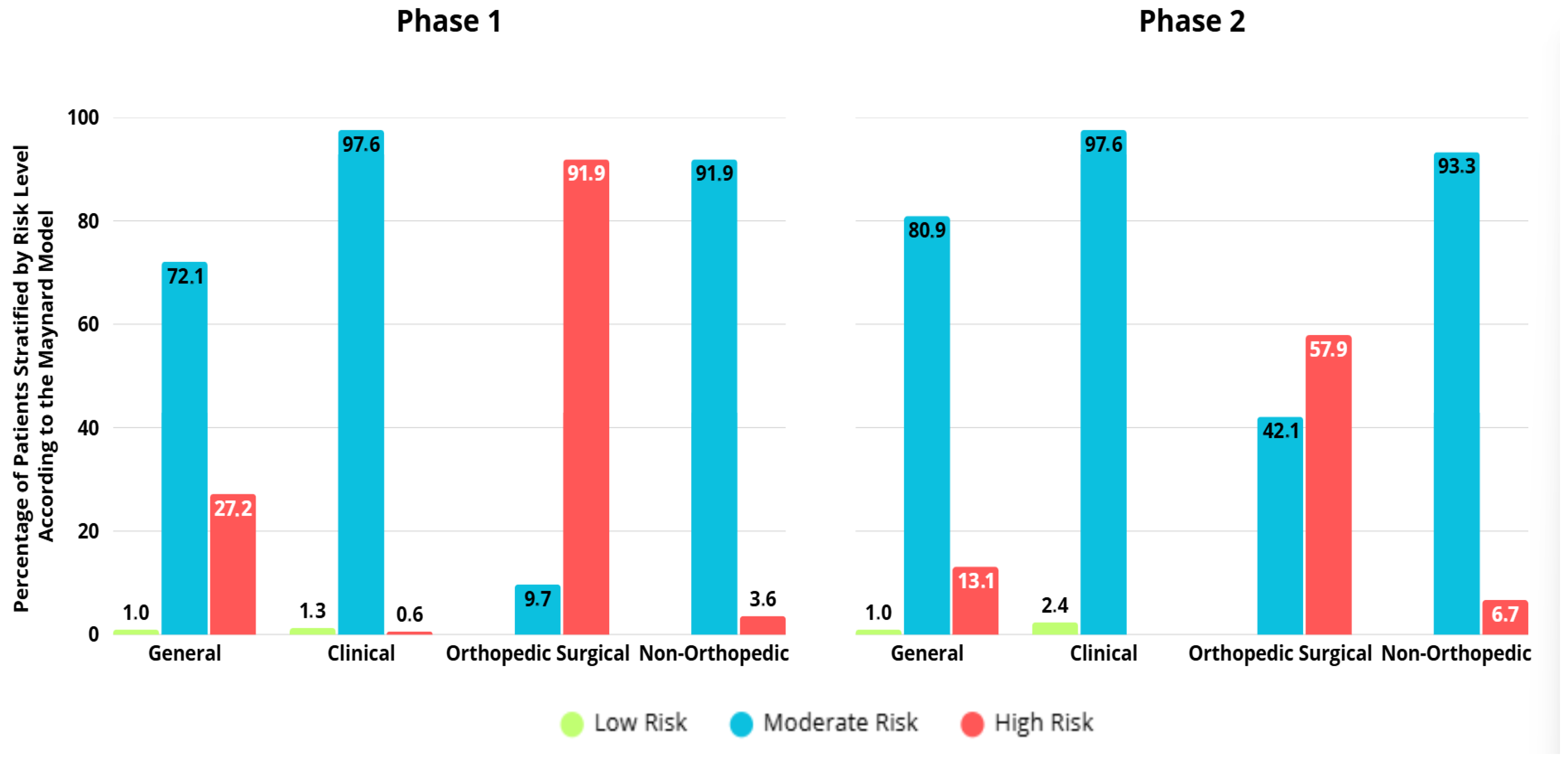
| Low Risk | 3 (0.8) | 3 (1.8) | 0 | 0 | <0.01 | |
| Intermediate Risk | 281 (72.1) | 166 (97.6) | 9 (8.2) | 106 (96.4) | ||
| High Risk | 106 (27.2) | 1 (0.6) | 101 (91.8) | 4 (3.6) | ||
| Caprini | ||||||
| Very Low Risk | 0 | - | 0 | 0 | 0.08 | |
| Low Risk | 0 | - | 0 | 0 | ||
| Intermediate Risk | 13 (5.9) | - | 3 (2.7) | 10 (9.1) | ||
| High Risk | 207 (94.1) | - | 107 (97.3) | 100 (90.9) | ||
| Phase 2 (n = 382) | Pádua | |||||
| Low Risk | 45 (26.5) | 45 (26.5) | - | - | - | |
| High Risk | 125 (73.5) | 125 (73.5) | - | - | ||
| Maynard | ||||||
| Low Risk | 4 (1.0) | 4 (2.4) | 0 | 0 | <0.01 | |
| Intermediate Risk | 309 (80.9) | 166 (97.6) | 45 (42.1) | 98 (93.3) | ||
| High Risk | 69 (18.1) | 0 | 62 (57.9) | 7 (6.7) | ||
| Caprini | ||||||
| Very Low Risk | 0 | - | 0 | 0 | 0.01 | |
| Low Risk | 4 (1.9) | - | 0 | 4 (3.8) | ||
| Intermediate Risk | 16 (7.5) | - | 4 (3.7) | 12 (11.4) | ||
| High Risk | 192 (90.6) | - | 103 (96.3) | 89 (84.8) | ||
| Group | Phase 1 (n = 390) | Phase 2 (n = 382) | p-Value |
|---|---|---|---|
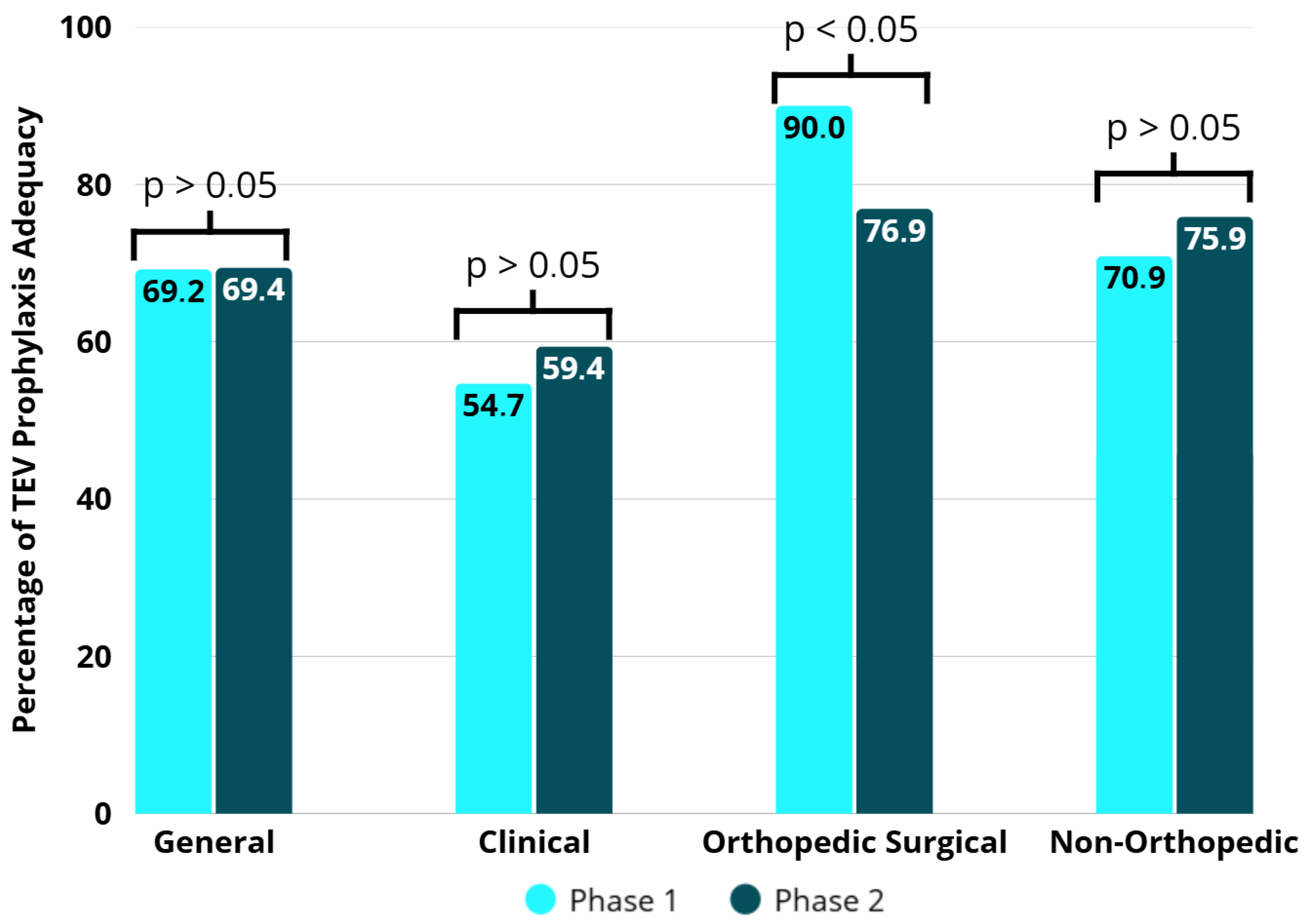
| General | |||
| Not Adequate | 120 (30.8) | 117 (30.6) | 0.99 |
| Adequate | 270 (69.2) | 265 (69.4) | |
| Clinical | |||
| Not Adequate | 77 (45.3) | 69 (40.6) | 0.44 |
| Adequate | 93 (54.7) | 101 (59.4) | |
| Orthopedic Surgical | |||
| Not Adequate | 11(10.0) | 25 (23.1) | 0.02 |
| Adequate | 110 (90.0) | 83 (76.9) | |
| Non-Orthopedic Surgical | |||
| Not Adequate | 32 (29.1) | 23 (22.1) | 0.31 |
| Adequate | 78 (70.9) | 81 (77.9) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alves, B.M.; Vieira, R.P.; Febras, L.L.T.; Soper, M.S.; Wolf, J.M.; Rohsig, V.; Carvalho, S.M.; de Lima, C.C.D.; Lazzari, C.; Machado, D.L.; et al. Implementation of the Maynard-Based Risk Assessment Model for Venous Thromboembolism Inpatient Prophylaxis: A Before-and-After Study. Healthcare 2025, 13, 3204. https://doi.org/10.3390/healthcare13243204
Alves BM, Vieira RP, Febras LLT, Soper MS, Wolf JM, Rohsig V, Carvalho SM, de Lima CCD, Lazzari C, Machado DL, et al. Implementation of the Maynard-Based Risk Assessment Model for Venous Thromboembolism Inpatient Prophylaxis: A Before-and-After Study. Healthcare. 2025; 13(24):3204. https://doi.org/10.3390/healthcare13243204
Chicago/Turabian StyleAlves, Belisa Marin, Raquel Pereira Vieira, Larissa Luma Tomasi Febras, Mauricio Santiago Soper, Jonas Michel Wolf, Vania Rohsig, Sidiclei Machado Carvalho, Cássia Cristine Damasio de Lima, Cintia Lazzari, Daniel Luft Machado, and et al. 2025. "Implementation of the Maynard-Based Risk Assessment Model for Venous Thromboembolism Inpatient Prophylaxis: A Before-and-After Study" Healthcare 13, no. 24: 3204. https://doi.org/10.3390/healthcare13243204
APA StyleAlves, B. M., Vieira, R. P., Febras, L. L. T., Soper, M. S., Wolf, J. M., Rohsig, V., Carvalho, S. M., de Lima, C. C. D., Lazzari, C., Machado, D. L., Nasi, L. A., & Gazzana, M. B. (2025). Implementation of the Maynard-Based Risk Assessment Model for Venous Thromboembolism Inpatient Prophylaxis: A Before-and-After Study. Healthcare, 13(24), 3204. https://doi.org/10.3390/healthcare13243204







