The Impact of Smartphone Addiction on PTSD Symptoms Among South African University Students: Resilience as a Protective Factor
Highlights
- Problematic smartphone use was significantly associated with higher levels of post-traumatic stress symptoms among South African university students.
- Resilience moderated this relationship, buffering the impact of smartphone addiction on PTSD symptoms and reducing psychological distress among individuals with higher resilience.
- Resilience did not significantly moderate the relationship between smartphone addiction and the re-experiencing or hyperarousal clusters, suggesting that these physiologically driven aspects of post-traumatic distress are less amenable to cog-nitive or emotional coping resources.
- Strengthening resilience may serve as an effective strategy to mitigate the negative mental health effects of excessive smartphone use in trauma-exposed populations.
- University-based mental health initiatives should integrate digital wellbeing and resilience-building interventions to promote healthier coping and reduce vulnerability to distress.
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.3. Ethics
2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| SABAS | Smartphone Application-Based Addiction Scale |
| CDRISC-10 | Connor-Davidson Resilience Scale-10 |
| PCL-5 | Posttraumatic Stress Disorder Checklist for DSM-5 |
| PTSD | Posttraumatic Stress Disorder |
Appendix A

References
- Horwood, S.; Anglim, J. Problematic smartphone usage and subjective and psychological well-being. Comput. Hum. Behav. 2019, 97, 44–50. [Google Scholar] [CrossRef]
- Folkman, S. Stress: Appraisal and coping. In Encyclopedia of Behavioral Medicine; Springer: New York, NY, USA, 2020; pp. 2177–2179. [Google Scholar]
- Wegmann, E.; Schiebener, J.; Brand, M. Social-networks use as adaptive or maladaptive strategy for coping with stress. Sci. Rep. 2023, 13, 11895. [Google Scholar] [CrossRef] [PubMed]
- Chen, I.H.; Pramukti, I.; Gan, W.Y.; Ruckwongpatr, K.; Pham, L.A.; Huang, P.C.; Mamun, M.A.; Ullah, I.; Jahrami, H.A.; Lin, C.Y.; et al. Smartphone Application—Based Addiction Scale: Psychometric Evidence Across Nine Asian Regions Using Advanced Analytic Methods. Brain Behav. 2024, 14, e70133. [Google Scholar] [CrossRef] [PubMed]
- Ratan, Z.; Parrish, A.-M.; Zaman, S.; Alotaibi, M.; Hosseinzadeh, H. Smartphone Addiction and Associated Health Outcomes in Adult Populations: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 12257. [Google Scholar] [CrossRef]
- Crowhurst, S.; Hosseinzadeh, H. Risk Factors of Smartphone Addiction: A Systematic Review of Longitudinal Studies. Public Health Chall. 2024, 3, e202. [Google Scholar] [CrossRef]
- Stanković, M.; Nešić, M.; Čičević, S.; Shi, Z. Association of smartphone use with depression, anxiety, stress, sleep quality, and internet addiction. Empirical evidence from a smartphone application. Pers. Individ. Differ. 2021, 168, 110342. [Google Scholar] [CrossRef]
- Kardefelt-Winther, D. A conceptual and methodological critique of internet addiction research: Towards a model of compensatory internet use. Comput. Hum. Behav. 2014, 31, 351–354. [Google Scholar] [CrossRef]
- Billieux, J.; Maurage, P.; Lopez-Fernandez, O.; Kuss, D.J.; Griffiths, M.D. Can Disordered Mobile Phone Use Be Considered a Behavioral Addiction? An Update on Current Evidence and a Comprehensive Model for Future Research. Curr. Addict. Rep. 2015, 2, 156–162. [Google Scholar] [CrossRef]
- Sohn, S.Y.; Rees, P.; Wildridge, B.; Kalk, N.J.; Carter, B. Prevalence of problematic smartphone usage and associated mental health outcomes amongst children and young people: A systematic review, meta-analysis and GRADE of the evidence. BMC Psychiatry 2019, 19, 356. [Google Scholar] [CrossRef]
- Brodersen, K.; Hammami, N.; Katapally, T.R. Smartphone use and mental health among youth: It is time to develop smartphone-specific screen time guidelines. Youth 2022, 2, 23–38. [Google Scholar] [CrossRef]
- Guo, N.; Luk, T.T.; Ho, S.Y.; Lee, J.J.; Shen, C.; Oliffe, J.; Chan, S.S.-C.; Lam, T.H.; Wang, M.P. Problematic Smartphone Use and Mental Health in Chinese Adults: A Population-Based Study. Int. J. Environ. Res. Public Health 2020, 17, 844. [Google Scholar] [CrossRef]
- Subramaniam, M.; Koh, Y.S.; Sambasivam, R.; Samari, E.; Abdin, E.; Jeyagurunathan, A.; Tan, B.C.W.; Zhang, Y.; Ma, S.; Chow, W.L.; et al. Problematic smartphone use and mental health outcomes among Singapore residents: The health and lifestyle survey. Asian J. Psychiatry 2024, 98, 104124. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.; Xiong, S.; Peng, Y.; Zeng, Y.; Zeng, C.; Yang, Y.; Zhang, B. Perceived stress and mobile phone addiction among college students: The roles of self-control and security. Front. Psychiatry 2022, 13, 1005062. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wang, M.; Feng, X.; He, L.; Du, J. The influence of stress perception on mobile phone addiction tendency in nursing undergraduates: The mediating role of self-control and the moderating role of psychological capital. BMC Nurs. 2025, 24, 1116. [Google Scholar] [CrossRef] [PubMed]
- Dou, X.; Lu, J.; Yu, Y.; Yi, Y.; Zhou, L. The impact of depression and anxiety on mobile phone addiction and the mediating effect of self-esteem. Sci. Rep. 2024, 14, 23004. [Google Scholar] [CrossRef]
- Zhang, K.; Guo, H.; Wang, T.; Zhang, J.; Yuan, G.; Ren, J.; Zhang, X.; Yang, H.; Lu, X.; Zhu, Z.; et al. A bidirectional association between smartphone addiction and depression among college students: A cross-lagged panel model. Front. Public Health 2023, 11, 1083856. [Google Scholar] [CrossRef]
- Zhou, H.; Dang, L.; Lam, L.W.; Zhang, M.X.; Wu, A.M.S. A cross-lagged panel model for testing the bidirectional relationship between depression and smartphone addiction and the influences of maladaptive metacognition on them in Chinese adolescents. Addict. Behav. 2021, 120, 106978. [Google Scholar] [CrossRef]
- Milam, L.C.; Dick, O.G.; McGettrick, C.R.; Brown, J.B.; Woodward, M.J. PTSD Symptoms and Problematic Smartphone Use in Young Adults Are Indirectly Associated Via Avoidance-Focused Coping. Int. J. Ment. Health Addict. 2024. [Google Scholar] [CrossRef]
- Binford, J.; Dolan, M.; Elhai, J.D.; Contractor, A.A. Examining relationships between posttraumatic stress disorder severity and types of media/technology usage. Psychol. Trauma Theory Res. Pract. Policy 2024, 16, 92–97. [Google Scholar] [CrossRef]
- Ha, J.; Kim, J.N.; Hidalgo, J.E.; Noble, N.C.; Price, M. Understanding the Relationship Between Mobile Phone Usage Behavior and Psychopathology Among Trauma-Exposed Individuals. J. Technol. Behav. Sci. 2025. [Google Scholar] [CrossRef]
- Shen, L.; Wu, X.; Zhen, R.; Zhou, X. Post-Traumatic Stress Disorder, Mobile Phone Dependence, and Academic Boredom in Adolescents During the COVID-19 Pandemic. Front. Psychol. 2021, 12, 724732. [Google Scholar] [CrossRef]
- Somerfield, M.R.; McCrae, R.R. Stress and Coping Research: Methodological Challenges, Theoretical Advances, and Clinical Applications. Am. Psychol. 2000, 55, 620–625. [Google Scholar] [CrossRef]
- Lazarus, R.S. Stress and Emotion: A New Synthesis; Springer Publishing Company: New York, NY, USA, 2006. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5-TR, 5th ed.; Text Revision; American Psychiatric Association Publishing: Washington, DC, USA, 2022. [Google Scholar]
- Li, W.; Zhao, Z.; Chen, D.; Peng, Y.; Lu, Z. Prevalence and associated factors of depression and anxiety symptoms among college students: A systematic review and meta-analysis. J. Child Psychol. Psychiatry 2022, 63, 1222–1230. [Google Scholar] [CrossRef] [PubMed]
- Rockwell, D.M.; Kimel, S.Y. A systematic review of first-generation college students’ mental health. J. Am. Coll. Health 2025, 73, 519–531. [Google Scholar] [CrossRef] [PubMed]
- Bantjes, J.; Kessler, M.J.; Hunt, X.; Stein, D.J.; Kessler, R.C. Treatment rates and barriers to mental health service utilisation among university students in South Africa. Int. J. Ment. Health Syst. 2023, 17, 38. [Google Scholar] [CrossRef] [PubMed]
- Coetzee, B.; Booysen, D.D.; Padmanabhanunni, A.; Kagee, A. Demographic correlates of indices of psychological well-being and COVID-19 related distress among South African university students. Int. J. Ment. Health 2024, 53, 192–211. [Google Scholar] [CrossRef]
- Padmanabhanunni, A.; Wiid, C. From fear to fortitude: Differential vulnerability to PTSD among South African university students. Traumatology 2022, 28, 167–174. [Google Scholar] [CrossRef]
- Bantjes, J.; Kessler, M.; Lochner, C.; Breet, E.; Bawa, A.; Roos, J.; Davids, C.; Muturiki, M.; Kessler, R.C.; Stein, D.J. The mental health of university students in South Africa: Results of the national student survey. J. Affect. Disord. 2023, 321, 217–226. [Google Scholar] [CrossRef]
- Padmanabhanunni, A. Trauma nation: Exposure to traumatic events among South African university students. J. Community Psychol. 2020, 48, 1853–1862. [Google Scholar] [CrossRef]
- Machisa, M.T.; Chirwa, E.D.; Mahlangu, P.; Sikweyiya, Y.; Nunze, N.; Dartnall, E.; Pillay, M.; Jewkes, R. Factors associated with female students’ past year experience of sexual violence in South African public higher education settings: A cross-sectional study. PLoS ONE 2021, 16, e0260886. [Google Scholar] [CrossRef]
- Pengpid, S.; Peltzer, K. Associations of serious physical injuries with posttraumatic stress and depressive symptoms: A cross-sectional survey among university students in 26 countries. BMC Psychol. 2020, 8, 129. [Google Scholar] [CrossRef]
- Mbunge, E.; Sibiya, M.N. Mobile health interventions for improving maternal and child health outcomes in South Africa: A systematic review. Glob. Health J. 2024, 8, 103–112. [Google Scholar] [CrossRef]
- Leon, N.; Surender, R.; Bobrow, K.; Muller, J.; Farmer, A. Improving treatment adherence for blood pressure lowering via mobile phone SMS-messages in South Africa: A qualitative evaluation of the SMS-text Adherence SuppoRt (StAR) trial. BMC Fam. Pract. 2015, 16, 80. [Google Scholar] [CrossRef] [PubMed]
- Mall, S.; Sibeko, G.; Temmingh, H.; Stein, D.J.; Milligan, P.; Lund, C. Using a treatment partner and text messaging to improve adherence to psychotropic medication: A qualitative formative study of service users and caregivers in Cape Town, South Africa. Afr. J. Psychiatry 2013, 16, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Hacking, D.; Haricharan, H.J.; Brittain, K.; Lau, Y.K.; Cassidy, T.; Heap, M. Hypertension Health Promotion via Text Messaging at a Community Health Center in South Africa: A Mixed Methods Study. JMIR mHealth uHealth 2016, 4, e22. [Google Scholar] [CrossRef]
- Anstey Watkins, J.O.T.; Goudge, J.; Gómez-Olivé, F.X.; Griffiths, F. Mobile phone use among patients and health workers to enhance primary healthcare: A qualitative study in rural South Africa. Soc. Sci. Med. 2018, 198, 139–147. [Google Scholar] [CrossRef]
- Musakuro, R.N.; Gie, L. University staff intentions to adopt e-health tools for digital mental health services in post-pandemic South Africa. S. Afr. J. Inf. Manag. 2024, 26, 1897. [Google Scholar] [CrossRef]
- Gbollie, E.F.; Bantjes, J.; Jarvis, L.; Swandevelder, S.; du Plessis, J.; Shadwell, R.; Davids, C.; Gerber, R.; Holland, N.; Hunt, X. Intention to use digital mental health solutions: A cross-sectional survey of university students attitudes and perceptions toward online therapy, mental health apps, and chatbots. Digit. Health 2023, 9, 20552076231216559. [Google Scholar] [CrossRef]
- Mostert, N. Measuring problematic smartphone use among students using the Smartphone Addiction Scale. S. Afr. Fam. Pract. 2025, 67, 6120. [Google Scholar] [CrossRef]
- Dietrich, J.J.; Otwombe, K.; Pakhomova, T.E.; Horvath, K.J.; Hornschuh, S.; Hlongwane, K.; Closson, K.; Mulaudzi, M.; Smith, P.; Beksinska, M.; et al. High cellphone use associated with greater risk of depression among young women aged 15–24 years in Soweto and Durban, South Africa. Glob. Health Action 2021, 14, 1936792. [Google Scholar] [CrossRef]
- De Doncker, K.; McLean, N. Social media, sleep difficulties and depressive symptoms: A case study of South African youth in Cape Town. Technol. Soc. 2022, 70, 102038. [Google Scholar] [CrossRef]
- Chetty-Mhlanga, S.; Fuhrimann, S.; Eeftens, M.; Basera, W.; Hartinger, S.; Dalvie, M.A.; Röösli, M. Different aspects of electronic media use, symptoms and neurocognitive outcomes of children and adolescents in the rural Western Cape region of South Africa. Environ. Res. 2020, 184, 109315. [Google Scholar] [CrossRef] [PubMed]
- Moroesi, G.P.-C.; Bongazana, D. Examining the association between self-control and mobile game addiction. Soc. Sci. Educ. Res. Rev. 2023, 10, 240–249. [Google Scholar] [CrossRef]
- Shae-Leigh Cynthia, V.; Nagesh, B.P. A theoretical review of psychological resilience: Defining resilience and resilience research over the decades. Arch. Med. Health Sci. 2019, 7, 233–239. [Google Scholar] [CrossRef]
- Stainton, A.; Chisholm, K.; Kaiser, N.; Rosen, M.; Upthegrove, R.; Ruhrmann, S.; Wood, S.J. Resilience as a multimodal dynamic process. Early Interv. Psychiatry 2019, 13, 725–732. [Google Scholar] [CrossRef]
- MacDonald, H.Z. Risk and resilience factors associated with college students’ psychological distress and PTSD symptoms during the COVID-19 pandemic. J. Am. Coll. Health 2023, 72, 3152–3166. [Google Scholar] [CrossRef]
- Csibi, S.; Griffiths, M.D.; Cook, B.; Demetrovics, Z.; Szabo, A. The Psychometric Properties of the Smartphone Application-Based Addiction Scale (SABAS). Int. J. Ment. Health Addict. 2018, 16, 393–403. [Google Scholar] [CrossRef]
- Campbell-Sills, L.; Stein, M.B. Psychometric analysis and refinement of the connor-davidson resilience scale (CD-RISC): Validation of a 10-item measure of resilience. J. Trauma. Stress 2007, 20, 1019–1028. [Google Scholar] [CrossRef]
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- Connor, K.M.; Davidson, J.R.T. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef]
- Pretorius, T.B.; Padmanabhanunni, A. Validation of the Connor-Davidson Resilience Scale-10 in South Africa: Item Response Theory and Classical Test Theory. Psychol. Res. Behav. Manag. 2022, 15, 1235–1245. [Google Scholar] [CrossRef] [PubMed]
- Padmanabhanunni, A.; Pretorius, T.B. An exploratory study of the mental health of first responders: Depression, anxiety, and post-traumatic stress disorder. S. Afr. J. Psychol. 2025, 55, 257–269. [Google Scholar] [CrossRef]
- Padmanabhanunni, A.; Pretorius, T. Demographic Factors, COVID-19-related Factors, and PTSD Symptom Clusters: Exploring Associations and Implications for Mental Health. OBM Neurobiol. 2023, 7, 184. [Google Scholar] [CrossRef]
- SmartPLS. How to Interpret Excess Kurtosis and Skewness. Available online: https://www.smartpls.com/documentation/functionalities/excess-kurtosis-and-skewness (accessed on 12 December 2024).
- Kagee, A.; Bantjes, J.; Saal, W.; Sterley, A. Predicting posttraumatic stress disorder caseness using the PTSD checklist for DSM--5 among patients receiving care for HIV. J. Trauma. Stress 2022, 35, 13–21. [Google Scholar] [CrossRef]
- Peng, P.; Chen, Z.; Ren, S.; Liu, Y.; He, R.; Liang, Y.; Tan, Y.; Tang, J.; Chen, X.; Liao, Y. Determination of the cutoff point for Smartphone Application-Based Addiction Scale for adolescents: A latent profile analysis. BMC Psychiatry 2023, 23, 675. [Google Scholar] [CrossRef]
- Street, A.E.; Dardis, C.M. Using a social construction of gender lens to understand gender differences in posttraumatic stress disorder. Clin. Psychol. Rev. 2018, 66, 97–105. [Google Scholar] [CrossRef]
- Lonnen, E.; Paskell, R. Gender, sex and complex PTSD clinical presentation: A systematic review. Eur. J. Psychotraumatol. 2024, 15, 2320994. [Google Scholar] [CrossRef]
- McGinty, G.; Fox, R.; Ben-Ezra, M.; Cloitre, M.; Karatzias, T.; Shevlin, M.; Hyland, P. Sex and age differences in ICD-11 PTSD and complex PTSD: An analysis of four general population samples. Eur. Psychiatry 2021, 64, e66. [Google Scholar] [CrossRef]
- Sommer, J.L.; Reynolds, K.; El-Gabalawy, R.; Pietrzak, R.H.; Mackenzie, C.S.; Ceccarelli, L.; Mota, N.; Sareen, J. Associations between physical health conditions and posttraumatic stress disorder according to age. Aging Ment. Health 2021, 25, 234–242. [Google Scholar] [CrossRef]
- Fino, E.; Mema, D.; Russo, P.M. War trauma exposed refugees and posttraumatic stress disorder: The moderating role of trait resilience. J. Psychosom. Res. 2020, 129, 109905. [Google Scholar] [CrossRef]
- Garofalo, C.; Delvecchio, E.; Bogaerts, S.; Sellbom, M.; Mazzeschi, C. Childhood trauma and psychopathy: The moderating role of resilience. Psychol. Trauma Theory Res. Pract. Policy 2024, 17, 511–519. [Google Scholar] [CrossRef]
- Wang, H.; Liao, Y.; Guo, L.; Zhang, H.; Zhang, Y.; Lai, W.; Teopiz, K.M.; Song, W.; Zhu, D.; Li, L.; et al. Association between childhood trauma and medication adherence among patients with major depressive disorder: The moderating role of resilience. BMC Psychiatry 2022, 22, 644. [Google Scholar] [CrossRef]
- Brzozowska, A.; Grabowski, J. Hyperarousal, Dissociation, Emotion Dysregulation and Re-Experiencing—Towards Understanding Molecular Aspects of PTSD Symptoms. Int. J. Mol. Sci. 2025, 26, 5216. [Google Scholar] [CrossRef] [PubMed]
- Kearney, B.E.; Lanius, R.A. Why reliving is not remembering and the unique neurobiological representation of traumatic memory. Nat. Ment. Health 2024, 2, 1142–1151. [Google Scholar] [CrossRef]
- Joyce, S.; Shand, F.; Tighe, J.; Laurent, S.J.; Bryant, R.A.; Harvey, S.B. Road to resilience: A systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open 2018, 8, e017858. [Google Scholar] [CrossRef]
- Ramirez, M.W.; Woodworth, C.A.; Evans, W.R.; Grace, G.A.; Schobitz, R.P.; Villarreal, S.A.; Howells, C.J.; Gissendanner, R.D.; Katko, N.J.; Jones, K.N.; et al. A trauma-focused intensive outpatient program integrating elements of exposure therapy with acceptance and commitment therapy: Program development and initial outcomes. J. Context. Behav. Sci. 2021, 21, 66–72. [Google Scholar] [CrossRef]
| Variable | Categories | %/SD | |
|---|---|---|---|
| Gender | Women | 318 | 64.8% |
| Men | 163 | 33.2% | |
| Other | 10 | 2% | |
| Graduate Status | Undergraduate | 454 | 92.5% |
| Postgraduate | 37 | 7.5% | |
| Home Province | Western Cape | 161 | 32.8% |
| Eastern Cape | 135 | 27.5% | |
| Gauteng | 72 | 14.7% | |
| Kwazulu-Natal | 41 | 8.4% | |
| Mpumalanga | 32 | 6.5% | |
| Limpopo | 23 | 4.7% | |
| Free State | 14 | 2.9% | |
| North West | 7 | 1.4% | |
| Northern Cape | 6 | 1.2% | |
| Residential Area | Rural | 173 | 35.2% |
| Urban | 318 | 64.8% | |
| Age | 21.22 years | 3.52 |
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Smartphone addiction | — | ||||||
| 2. Resilience | −0.02 | — | |||||
| 3. PTSD | 0.40 ** | −0.09 | — | ||||
| 4. Re-experiencing | 0.38 ** | −0.08 | 0.87** | — | |||
| 5. Avoidance | 0.33 ** | −0.08 | 0.80 ** | 0.71 ** | — | ||
| 6. Negative alterations | 0.34 ** | −0.09 * | 0.93 ** | 0.69 ** | 0.68 ** | — | |
| 7. Hyperarousal | 0.36 ** | 0.05 | 0.90 ** | 0.67 ** | 0.61 ** | 0.79 ** | — |
| Mean | 21.92 | 25.19 | 32.57 | 7.99 | 3.63 | 11.52 | 9.43 |
| SD | 6.64 | 8.28 | 18.62 | 5.50 | 2.49 | 7.18 | 5.81 |
| Skewness | −0.18 | −0.52 | 0.12 | 0.28 | 0.14 | 0.18 | 0.21 |
| Kurtosis | −0.57 | −0.01 | −0.61 | −0.86 | −1.03 | −0.70 | −0.63 |
| Alpha | 0.81 | 0.90 | 0.94 | 0.89 | 0.81 | 0.88 | 0.83 |
| Effects | B | SE | 95% CI | β | p | |
|---|---|---|---|---|---|---|
| LL | UL | |||||
| Direct Effects | ||||||
| Smartphone addiction → PTSD | 1.04 | 0.12 | 0.81 | 1.27 | 0.37 ** | <0.001 |
| Smartphone addiction → Re-experiencing | 0.30 | 0.04 | 0.23 | 0.37 | 0.36 ** | <0.001 |
| Smartphone addiction → Avoidance | 0.11 | 0.02 | 0.08 | 0.14 | 0.29 ** | <0.001 |
| Smartphone addiction → Negative alterations | 0.34 | 0.05 | 0.25 | 0.43 | 0.31 ** | <0.001 |
| Smartphone addiction → Hyperarousal | 0.29 | 0.04 | 0.22 | 0.37 | 0.34 ** | <0.001 |
| Resilience → PTSD | −0.21 | 0.10 | −0.40 | −0.02 | −0.09 * | 0.029 |
| Resilience → Re-experiencing | −0.06 | 0.03 | −0.11 | 0.00 | −0.08 | 0.060 |
| Resilience → Avoidance | −0.03 | 0.02 | −0.05 | −0.00 | −0.09 * | 0.041 |
| Resilience → Negative alterations | −0.09 | 0.04 | −0.16 | −0.11 | −0.10 * | 0.020 |
| Resilience → Hyperarousal | −0.04 | 0.03 | −0.10 | 0.00 | −0.06 | 0.197 |
| Moderating Effects | ||||||
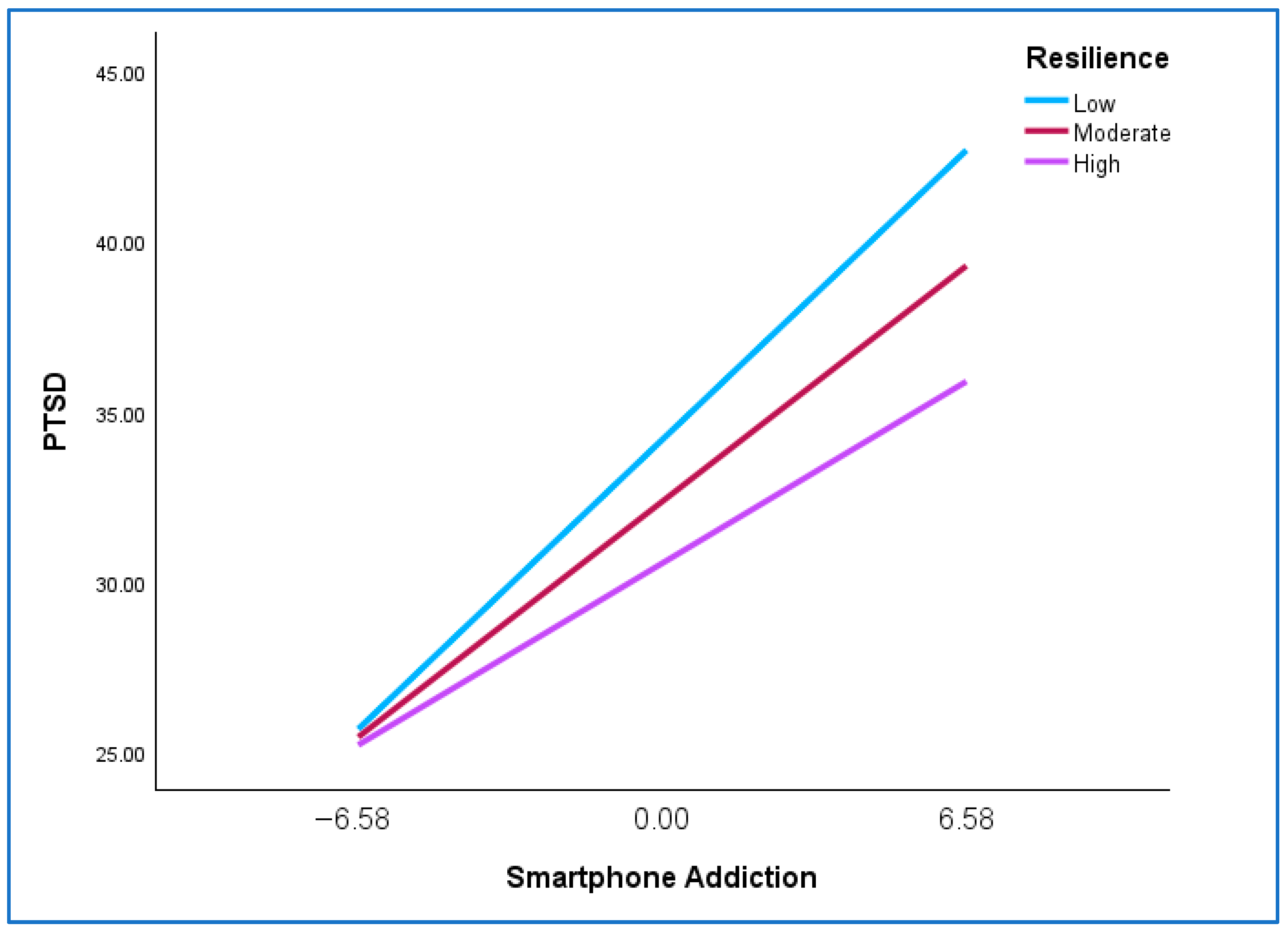
| Smartphone addiction X Resilience → PTSD | −0.03 | 0.01 | −0.05 | −0.01 | −0.09 * | 0.016 |
| Smartphone addiction X Resilience → Re-experiencing | −0.01 | 0.00 | −0.01 | 0.00 | −0.05 | 0.164 |
| Smartphone addiction X Resilience → Avoidance | −0.01 | 0.00 | −0.01 | −0.00 | −0.11 * | 0.003 |
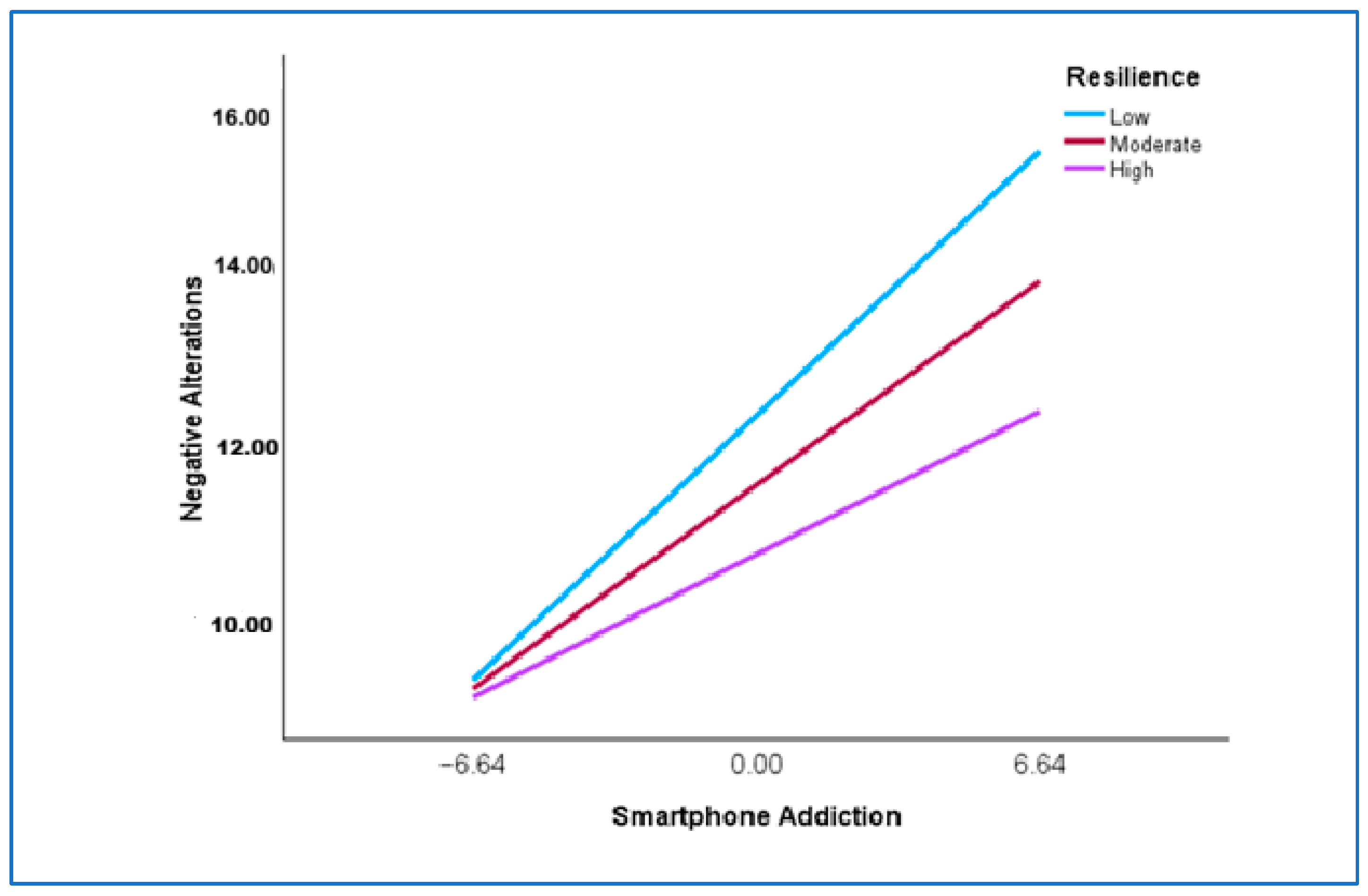
| Smartphone addiction X Resilience → Negative alterations | −0.01 | 0.01 | −0.02 | −0.00 | −0.09 ** | 0.010 |
| Smartphone addiction X Resilience → Hyperarousal | −0.01 | 0.00 | −0.01 | 0.00 | −0.06 | 0.078 |
| Effects | B | SE | 95% CI | β | p | |
|---|---|---|---|---|---|---|
| LL | UL | |||||
| Smartphone addiction → PTSD | ||||||
| Low Resilience (1 SD below the mean) | 1.28 | 0.14 | 1.00 | 1.56 | 0.46 ** | <0.001 |
| Moderate Resilience (at the mean) | 1.04 | 0.12 | 0.81 | 1.27 | 0.37 ** | <0.001 |
| High Resilience (1 SD above the mean) | 0.80 | 0.16 | 0.48 | 1.12 | 0.29 ** | <0.001 |
| Smartphone addiction → Avoidance | ||||||
| Low Resilience (1 SD below the mean) | 0.15 | 0.02 | 0.11 | 0.19 | 0.40 ** | <0.001 |
| Moderate Resilience (at the mean) | 0.11 | 0.02 | 0.08 | 0.14 | 0.29 ** | <0.001 |
| High Resilience (1 SD above the mean) | 0.07 | 0.02 | 0.02 | 0.11 | 0.18 * | 0.002 |
| Smartphone addiction → Negative alterations | ||||||
| Low Resilience (1 SD below the mean) | 0.44 | 0.06 | 0.33 | 0.55 | 0.40 ** | <0.001 |
| Moderate Resilience (at the mean) | 0.34 | 0.05 | 0.25 | 0.43 | 0.31 ** | <0.001 |
| High Resilience (1 SD above the mean) | 0.24 | 0.07 | 0.11 | 0.36 | 0.22 ** | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Padmanabhanunni, A.; Pretorius, T.B. The Impact of Smartphone Addiction on PTSD Symptoms Among South African University Students: Resilience as a Protective Factor. Healthcare 2025, 13, 3087. https://doi.org/10.3390/healthcare13233087
Padmanabhanunni A, Pretorius TB. The Impact of Smartphone Addiction on PTSD Symptoms Among South African University Students: Resilience as a Protective Factor. Healthcare. 2025; 13(23):3087. https://doi.org/10.3390/healthcare13233087
Chicago/Turabian StylePadmanabhanunni, Anita, and Tyrone B. Pretorius. 2025. "The Impact of Smartphone Addiction on PTSD Symptoms Among South African University Students: Resilience as a Protective Factor" Healthcare 13, no. 23: 3087. https://doi.org/10.3390/healthcare13233087
APA StylePadmanabhanunni, A., & Pretorius, T. B. (2025). The Impact of Smartphone Addiction on PTSD Symptoms Among South African University Students: Resilience as a Protective Factor. Healthcare, 13(23), 3087. https://doi.org/10.3390/healthcare13233087






