Electrocardiogram Interpretation Competency of Primary Health Care Physicians: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Sampling Technique and Data Collection Process
2.3. Data Collection Tool and Competency Assessment
- -
- Q1: Absent P-wave
- -
- Q2: ECG waves and intervals (order and identification)
- -
- ECG1: Atrial flutter
- -
- ECG2: Ventricular fibrillation
- -
- ECG3: Atrial fibrillation
- -
- ECG4: Pathological Q wave
- -
- ECG5: Atrioventricular third-degree block
- -
- ECG6: Bundle branch block
- -
- ECG7: Ventricular tachycardia
- -
- ECG8: Acute myocardial infarction
- -
- ECG9: Normal ECG
- -
- ECG10: Ventricular extrasystole
- -
- ECG11: Atrial tachycardia
2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ECG | Electrocardiogram |
| ACLS | Advanced Cardiac Life Support |
| CVD | Cardiovascular disease |
| STROBE | Strengthening the Reporting of Observational Studies in Epidemiology |
References
- Amini, K.; Mirzaei, A.; Hosseini, M.; Zandian, H.; Azizpour, I.; Haghi, Y. Assessment of electrocardiogram interpretation competency among healthcare professionals and students of Ardabil University of Medical Sciences: A multidisciplinary study. BMC Med. Educ. 2022, 22, 448. [Google Scholar] [CrossRef]
- Isiguzo, G.; Iroezindu, M.; Muoneme, A.; Okeahialam, B. Knowledge and utilization of electrocardiogram among resident doctors in family medicine in Nigeria. Niger. J. Clin. Pract. 2017, 20, 1133–1138. [Google Scholar] [CrossRef]
- World Health Organization. Cardiovascular Diseases (CVDs) [Internet]; World Health Organization: Geneva, Switzerland, 31 July 2025; Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 15 November 2025).
- De Jager, J.; Wallis, L.; Marid, D. ECG interpretation skills of South African Emergency Medicine residents. Int. J. Emerg. Med. 2010, 3, 309–314. [Google Scholar] [CrossRef]
- Vishnevsky, G.; Cohen, T.; Elitzur, Y.; Reis, S. Competency and confidence in ECG interpretation among medical students. Int. J. Med. Educ. 2022, 13, 315–321. [Google Scholar] [CrossRef]
- Sterling, M.R.; Ferranti, E.P.; Green, B.B.; Moise, N.; Foraker, R.; Nam, S.; Juraschek, S.P.; Anderson, C.A.; Laurent, P.S.; Sussman, J. The Role of Primary Care in Achieving Life’s Essential 8: A Scientific Statement from the American Heart Association. In Circulation: Cardiovascular Quality and Outcomes; Lippincott Williams and Wilkins: Philadelphia, PA, USA, 2024; Volume 17, p. e000134. [Google Scholar]
- Quinn, T.; Johnsen, S.; Gale, C.P.; Snooks, H.; McLean, S.; Woollard, M.; Myocardial Ischaemia National Audit Project (MINAP) Steering Group. Effects of prehospital 12-lead ECG on processes of care and mortality in acute coronary syndrome: A linked cohort study from the Myocardial Ischaemia National Audit Project. Heart 2014, 100, 944–950. [Google Scholar] [CrossRef]
- Sur, D.K.; Kaye, L.; Mikus, M.; Goad, J.; Morena, A. Accuracy of electrocardiogram reading by family practice residents. Fam. Med. 2000, 32, 315–319. [Google Scholar] [PubMed]
- Alsubaie, A.M.; Yahia, O. Assessment of knowledge and utilization of electrocardiogram by primary health care physicians and nurses in Qassim Region, Saudi Arabia. Int. J. Med. Dev. Ctries. 2024, 8, 2045–2049. [Google Scholar] [CrossRef]
- Aljohani, M.S. Competency in ECG Interpretation and Arrhythmias Management among Critical Care Nurses in Saudi Arabia: A Cross Sectional Study. Healthcare 2022, 10, 2576. [Google Scholar] [CrossRef] [PubMed]
- Al Mousa, A.M.; Alhubail, F.M.; Almulhim, M.; AlBeladi, B.A.; Almulhim, N.A.; Almulhim, A.A.; Algouf, I. Electrocardiogram Interpretation Competency of Medical Interns in Saudi Arabia: A Cross-Sectional Study. Cureus 2023, 15, e37557. [Google Scholar] [CrossRef]
- Elsheikh, E.; Alkhteeb, N.; Alamer, A.; Alarfaj, M.O.; AlQarni, G.; Alsultan, J. Medical Students’ Competency and Confidence in Interpreting Electrocardiograms at King Faisal University, Al-Ahsa. Cureus 2023, 15, e46393. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gødsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- Coll-Badell, M.; Jiménez-Herrera, M.F.; Llaurado-Serra, M. Emergency Nurse Competence in Electrocardiographic Interpretation in Spain: A Cross-Sectional Study. J. Emerg. Nurs. 2017, 43, 560–570. [Google Scholar] [CrossRef] [PubMed]
- Kadish, A.H.; Buxton, A.E.; Kennedy, H.L.; Knight, B.P.; Mason, J.W.; Schuger, C.D.; Tracy, C.M.; Winters, W.L.; Boone, A.W.; Elnicki, M.; et al. ACC/AHA Clinical Competence Statement on Electrocardiography and Ambulatory Electrocardiography A Report of the ACC/AHA/ACP-ASIM Task Force on Clinical Competence (ACC/AHA Committee to Develop a Clinical Competence Statement on Electrocardiography and Ambulatory Electrocardiography) Endorsed by the International Society for Holter and Noninvasive Electrocardiology Committee Members. 2001. Available online: www.acc.org (accessed on 15 June 2025).
- Margolis, S.; Reed, R.L. EKG Analysis Skills of Family Practice Residents in the United Arab Emirates: A Comparison with US Data. Fam. Med. 2001, 33, 447–452. Available online: https://www.researchgate.net/publication/11928036 (accessed on 7 February 2025). [PubMed]
- Mabuza, L.H.; Mntla, P.S. Generalist practitioners’ self-rating and competence in electrocardiogram interpretation in South Africa. Afr. J. Prim. Health Care Fam. Med. 2020, 12, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Abdalla, A.A.; Khanra, D. Electrocardiography Interpretation Proficiency Among Medical Doctors of Different Grades in the United Kingdom. Cureus 2022, 14, e29755. [Google Scholar] [CrossRef] [PubMed]
- Kopeć, G.; Magoń, W.; Hołda, M.; Podolec, P. Competency in ECG Interpretation Among Medical Students. Med. Sci. Monit. 2015, 21, 3386–3394. [Google Scholar] [CrossRef]
- Rahimpour, M.; Shahbazi, S.; Ghafourifard, M.; Gilani, N.; Breen, C. Electrocardiogram interpretation competency among emergency nurses and emergency medical service (EMS) personnel: A cross-sectional and comparative descriptive study. Nurs. Open 2021, 8, 1712–1719. [Google Scholar] [CrossRef]
- Mandourah, A.; Basamih, K.; Alghamdi, G.; Almatrafi, R.; Hazra, S.; Alghamdi, F.; Alraffah, Y. Evaluation of ECG Interpretation Among Undergraduate Medical Students at Universities in Makkah Region, Saudi Arabia: A Cross-Sectional Study. Niger. J. Clin. Pract. 2025, 28, 695–707. [Google Scholar] [CrossRef]
- Santos, P.; Pessanha, P.; Viana, M.; Campelo, M.; Nunes, J.; Hespanhol, A.; Macedo, F.; Couto, L. Accuracy of general practitioners’ readings of ECG in primary care. Open Med. 2014, 9, 431–436. [Google Scholar] [CrossRef]
- Salerno, S.M.; Alguire, P.C.; Waxman, H.S. Competency in Interpretation of 12-Lead Electrocardiograms: A Summary and Appraisal of Published Evidence Background: There Have Been Many Proposals for Objective. Ann. Intern. Med. 2003, 138, 751–760. Available online: www.annals.org (accessed on 5 February 2025). [CrossRef]
- Elkammash, A.; Ahmed, M.W.; Alsinan, M.; Madi, K. The Effectiveness of Online Learning in Improving the Electrocardiogram Interpretation Skills of Junior Medical Trainees: A Mixed Methods Observational Study. Cureus 2023, 15, e42320. [Google Scholar] [CrossRef]
- Mobrad, A. Electrocardiogram Interpretation Competency Among Paramedic Students. J. Multidiscip. Healthc. 2020, 13, 823–828. [Google Scholar] [CrossRef]
- Alghamdi, S.A.A.; Almuntashiri, A.H.A.; Aljuaeed, M.S.A.; Mohamed, M.A. Electrocardiography misreading among sixth-year medical students and interns in Taif University. Int. J. Community Med. Public Health 2018, 5, 4225–4230. [Google Scholar] [CrossRef]

| Item | N | N% | |
|---|---|---|---|
| Gender | Male | 117 | 45.5% |
| Female | 140 | 54.5% | |
| Experience years | Less than 5 years | 152 | 59.1% |
| 5–10 years | 52 | 20.2% | |
| More than 10 years | 53 | 20.6% | |
| Level | Family medicine resident | 101 | 39.3% |
| Family medicine specialist | 36 | 14.0% | |
| Family medicine consultant | 43 | 16.7% | |
| General practitioner | 77 | 30.0% | |
| Education (program) sector | Al-Ahsa Health Cluster | 102 | 39.7% |
| Johns Hopkins Aramco Healthcare Center in Dhahran | 24 | 9.3% | |
| Eastern Health Cluster | 73 | 28.4% | |
| King Fahad University Hospital in Khobar | 28 | 10.9% | |
| Health Services Program in the Royal Commission in Jubail | 8 | 3.1% | |
| Other | 22 | 8.6% | |
| Cardiology rotation | Yes | 133 | 51.8% |
| No | 124 | 48.2% | |
| ACLS | Yes | 127 | 49.4% |
| No | 130 | 50.6% | |
| Knowledge Level | ||
|---|---|---|
| Classification | N | N% |
| Good (≥7.5) | 118 | 45.9% |
| Poor (<7.5) | 139 | 54.1% |
| Facilitators | N (N%) | |
|---|---|---|
| Yes | No | |
| Practical case-based training in the program | 177 (68.9%) | 80 (31.1%) |
| Extracurricular educational courses | 127 (49.4%) | 130 (50.6%) |
| Volunteer work in cardiology clinics | 70 (27.2%) | 187 (72.8%) |
| Cardiology block important aspects should be adopted and implanted in all blocks | 119 (46.3%) | 138 (53.7%) |
| Other | 39 (15.2%) | 218 (84.8%) |
| Barriers | N (N%) | |
| Yes | No | |
| Inadequate training in the program | 177 (68.9%) | 80 (31.1%) |
| Dependence on cardiologist expertise | 86 (33.5%) | 171 (66.5%) |
| ECG interpretation itself is difficult | 120 (46.7%) | 137 (53.3%) |
| Lack of resources | 78 (30.4%) | 179 (69.6%) |
| Other | 10 (3.9%) | 247 (96.1%) |
| Good | Poor | p-Value | ||
|---|---|---|---|---|
| N (%) | ||||
| Gender | Female | 67 (47.9%) | 73 (52.1%) | 0.494 |
| Male | 51 (43.6%) | 66 (56.4%) | ||
| Experience (years) | 5–10 years | 15 (28.8%) | 37 (71.2%) | 0.016 * |
| Less than 5 years | 74 (48.7%) | 78 (51.3%) | ||
| More than 10 years | 29 (54.7%) | 24 (45.3%) | ||
| Level | Family medicine consultant | 21 (48.8%) | 22 (51.2%) | 0.274 |
| Family medicine resident | 46 (45.5%) | 55 (54.5%) | ||
| Family medicine specialist | 21 (58.3%) | 15 (41.7%) | ||
| General practitioner | 30 (39.0%) | 47 (61.0%) | ||
| Cardiology rotation | Yes | 65 (48.9%) | 68 (51.1%) | 0.324 |
| No | 53 (42.7%) | 71 (57.3%) | ||
| ACLS | Yes | 68 (53.5%) | 59 (46.5%) | 0.015 * |
| No | 50 (38.5%) | 80 (61.5%) | ||
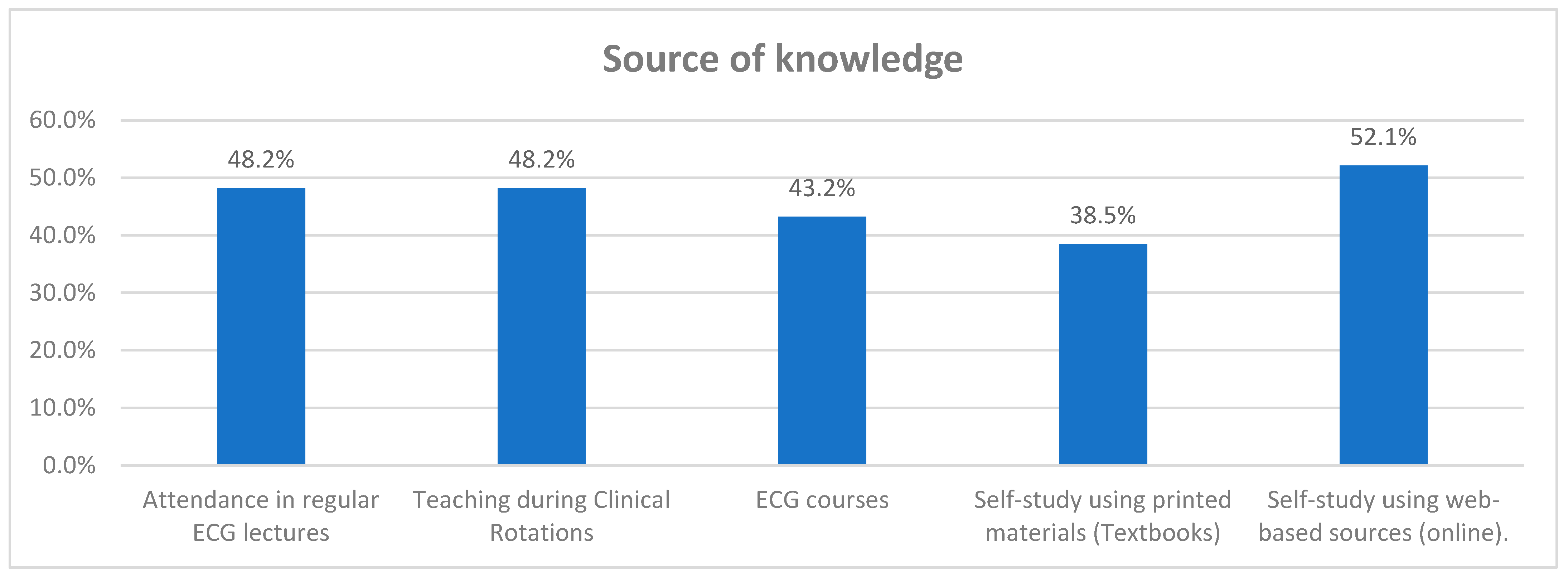
| Source of Knowledge | ||||
| Attendance in regular ECG lectures | Yes | 66 (53.2%) | 58 (46.8%) | 0.023 * |
| No | 52 (39.1%) | 81 (60.9%) | ||
| Teaching during Clinical Rotations | Yes | 65 (52.4%) | 59 (47.6%) | 0.043 * |
| No | 53 (39.8%) | 80 (60.2%) | ||
| ECG courses | Yes | 59 (53.2%) | 52 (46.8%) | 0.042 * |
| No | 59 (40.4%) | 87 (59.6%) | ||
| Self-study using printed materials (Textbooks) | Yes | 45 (45.5%) | 54 (54.5%) | 0.907 |
| No | 73 (46.2%) | 85 (53.8%) | ||
| Self-study using web-based sources (online) | Yes | 66 (49.3%) | 68 (50.7%) | 0.262 |
| No | 52 (42.3%) | 71 (57.7%) | ||
| Predictor | B | p-Value | Odds Ratio Exp(B) | 95% CI for Exp(B) | |
|---|---|---|---|---|---|
| Experience | Less than 5 years | −0.226 | 0.521 | 0.798 | 0.400–1.589 |
| 5–10 years | −1.054 | 0.014 * | 0.349 | 0.151–0.806 | |
| More than 10 years | Reference | ||||
| ACLS | 0.627 | 0.022 * | 1.872 | 1.093–3.207 | |
| Attendance in regular ECG lectures | 0.498 | 0.070 | 1.646 | 0.960–2.822 | |
| Teaching during clinical rotations | 0.436 | 0.106 | 1.547 | 0.911–2.626 | |
| ECG courses | 0.407 | 0.128 | 1.503 | 0.890–2.538 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
AlShakhs, A.A.; AlAmeer, A.A.; AlEsmaeel, Z.C.; AlMotawa, O.; AlHaddad, S.M.; AlHaddad, H.M.; Almaqhawi, A. Electrocardiogram Interpretation Competency of Primary Health Care Physicians: A Cross-Sectional Study. Healthcare 2025, 13, 3040. https://doi.org/10.3390/healthcare13233040
AlShakhs AA, AlAmeer AA, AlEsmaeel ZC, AlMotawa O, AlHaddad SM, AlHaddad HM, Almaqhawi A. Electrocardiogram Interpretation Competency of Primary Health Care Physicians: A Cross-Sectional Study. Healthcare. 2025; 13(23):3040. https://doi.org/10.3390/healthcare13233040
Chicago/Turabian StyleAlShakhs, Abdullah Afif, Abdullah A. AlAmeer, Zahra C. AlEsmaeel, Omniyah AlMotawa, Sajjad M. AlHaddad, Hasan M. AlHaddad, and Abdullah Almaqhawi. 2025. "Electrocardiogram Interpretation Competency of Primary Health Care Physicians: A Cross-Sectional Study" Healthcare 13, no. 23: 3040. https://doi.org/10.3390/healthcare13233040
APA StyleAlShakhs, A. A., AlAmeer, A. A., AlEsmaeel, Z. C., AlMotawa, O., AlHaddad, S. M., AlHaddad, H. M., & Almaqhawi, A. (2025). Electrocardiogram Interpretation Competency of Primary Health Care Physicians: A Cross-Sectional Study. Healthcare, 13(23), 3040. https://doi.org/10.3390/healthcare13233040







