Integrating Sustainability in Radiology: Challenges and Opportunities from the Perspective of Radiology Professionals in Saudi Arabia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sampling
2.2. Ethical Approval
2.3. Data Collection and Instruments
2.4. Statistical Analysis
3. Results
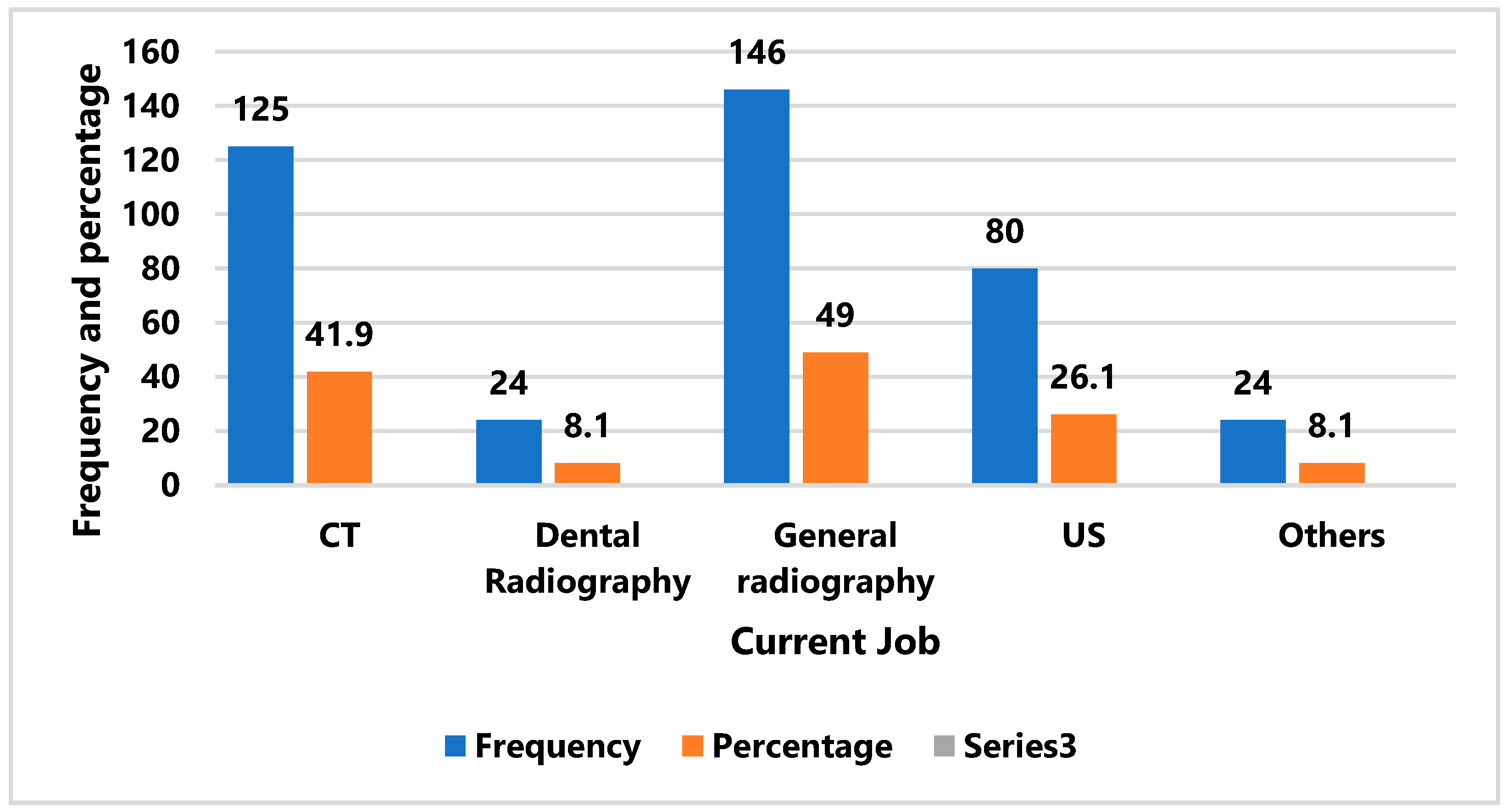
3.1. Demographic Characteristics
3.2. Sustainability Focus
4. Discussion
4.1. Knowledge and Perception
4.2. Attitude
4.3. Practice
4.4. Barriers
5. Conclusions
5.1. Practical Implications
5.2. Theoretical Implications
5.3. Recommendations
5.4. Directions for Future Research
- Use larger, more stratified data sets to improve representation across Saudi healthcare professions.
- Tracking changes in behavior and the environment around us by periodic assessments of training or technological improvements.
- Examining different countries’ strategies to identify the sustainability models that perform effectively. Investigating AI, Internet of Things (IoT), and automation technologies can further optimize radiology’s energy use and waste handling.
- Exploring behavioral interventions such as feedback systems or gamification to motivate sustainable actions among radiographers.
5.5. Interdisciplinary Collaboration
5.6. Role of Technology
5.7. Education Reform
5.8. Limitation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| MRI | Magnetic Resonance Imaging |
| CT | Computed Tomography |
| US | Ultrasound |
| PNU | Princess Nourah bint Abdulrahman University |
| IRB | Institutional Review Board |
| SD | Standard Deviation |
| GBCA | Good Gadolinium-Based Contrast Media |
| GHG | Greenhouse Gas |
| ACR | American College of Radiology |
| SDGs | Sustainable Development Goals |
| WHO | World Health Organization |
| UHC | Universal Healthcare |
| SDA | Strongly Disagree |
| DA | Disagree |
| AG | Agree |
| SAG | Strongly Agree |
References
- Alnutaifi, M.M.; Majrashi, M.A.; Alshaye, F.A.; Alkahuriji, A.A.; Abueisha, M.A.; Alrashidi, R.H.; Alharbi, F.F. Sustainable Practices in Diagnostic Imaging: A Systematic Review of Environmental Initiatives and Resource Management in Saudi Radiology Departments. Front. Health Inform. 2025, 14, 2255–2281. [Google Scholar]
- Hasan, N.; Rizk, C.; AlKhaja, M.; Babikir, E. Optimisation toward Sustainable Computed Tomography Imaging Practices. Sustain. Futures 2024, 7, 100176. [Google Scholar] [CrossRef]
- Climate Change and Health (CCH); Environment, Climate Change and Health (ECH). Operational Framework for Building Climate Resilient and Low Carbon Health Systems; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Rawashdeh, M.; Ali, M.A.; McEntee, M.; El-Sayed, M.; Saade, C.; Kashabash, D.; England, A. Green Radiography: Exploring Perceptions, Practices, and Barriers to Sustainability. Radiography 2024, 30, 62–73. [Google Scholar] [CrossRef] [PubMed]
- Roletto, A.; Catania, D.; Rainford, L.; Savio, A.; Zanardo, M.; Bonfitto, G.R.; Zanoni, S. Sustainable Radiology Departments: A European Survey to Explore Radiographers’ Perceptions of Environmental and Energy Sustainability Issues. Radiography 2024, 30, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Abuzaid, M.; Almuqbil, N.; Emery, C.V.; Elshami, W.; Ibham, M.; Alsubaie, N.; Hamd, Z.; Aljamal, M. Bridging the Gap in Sustainable Radiography: Insights from Five Countries in Asia and Africa. BMC Health Serv. Res. 2025, 25, 392. [Google Scholar] [CrossRef] [PubMed]
- Chinene, B.; Mudadi, L.; Bwanga, O.; Nyawani, P.; Mutandiro, L.; Kafwimbi, S.; Matika, W.; Ohene-Botwe, B. Sustainability in Radiography: Knowledge, Practices, and Barriers among Radiographers in Zimbabwe and Zambia. J. Med. Imaging Radiat. Sci. 2024, 55, 101438. [Google Scholar] [CrossRef] [PubMed]
- Kingdom of Saudi Arabia. Vision 2030 Achievements: 2016–2020. Riyadh. Vision 2030. Available online: https://www.vision2030.gov.sa/media/2pkmoa05/vision-2030-achievements-booklet-2016-2020-1.pdf (accessed on 10 September 2025).
- The Ministry of Human Resources and Social Development Signs a Memorandum of Understanding with the National Center for Vegetative Cover Development and Desertification Control. Available online: https://www.hrsd.gov.sa/en/media-center/news/061120239 (accessed on 20 August 2025).
- Abuzaid, M.M.; Almuqbil, N. Charting a Sustainable Future in Radiology: Evaluating Radiologists’ Knowledge, Attitudes, and Practices toward Environmental Responsibility. Insights Imaging 2025, 16, 39. [Google Scholar] [CrossRef] [PubMed]
- Bwanga, O.; Chinene, B.; Mudadi, L.; Kafwimbi, S.; Nyawani, P.; Matika, W.; Mushosho, E.Y.; Mutandiro, L.; Ohene-Botwe, B. Environmental Sustainability in Radiography in Low-Resource Settings: A Qualitative Study of Awareness, Practices, and Challenges among Zimbabwean and Zambian Radiographers. Radiography 2024, 30, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Abdul Razak, W.; Takyi, C.; Ofori-Manteaw, B.B. Exploring Sustainability in Radiography: A Study of Ghanaian Radiographers. Radiography 2025, 31, 102952. [Google Scholar] [CrossRef] [PubMed]
- Ohene-Botwe, B.; Amedu, C.; Antwi, W.K.; Abdul-Razak, W.; Kyei, K.A.; Arkoh, S.; Mudadi, L.-S.; Mushosho, E.Y.; Bwanga, O.; Chinene, B.; et al. Promoting Sustainability Activities in Clinical Radiography Practice and Education in Resource-Limited Countries: A Discussion Paper. Radiography 2024, 30, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Debnath, M.; Ojha, S.; Sharma, D.A.; Shah, S.; Boora, N. Role of Green and Sustainable Practices in Shaping the Future of Medical Imaging Technology: A Cross-Sectional Multi-Stakeholder Analysis among Students, Radiographers, and Academic Experts. Radiography 2024, 30, 1332–1341. [Google Scholar] [CrossRef]
- Halkos, G.; Gkampoura, E.-C. Where Do We Stand on the 17 Sustainable Development Goals? An Overview on Progress. Econ. Anal. Policy 2021, 70, 94–122. [Google Scholar] [CrossRef]

| Demographic Characteristics | Frequency | Percent | |
|---|---|---|---|
| Gender | Male | 145 | 48.7 |
| Female | 153 | 51.3 | |
| Age group | 20–29 | 168 | 56.4 |
| 30–39 | 84 | 28.2 | |
| 40–50 | 42 | 14.1 | |
| More than 50 | 4 | 1.3 | |
| Healthcare facility | Hospital | 268 | 89.9 |
| Clinic | 30 | 10.1 | |
| Experiences | 1–10 | 239 | 80.2 |
| 11–20 | 56 | 18.8 | |
| More than 20 | 3 | 1.0 | |
| Total | 298 | 100.0 | |
| Question | Answer | n (%) |
|---|---|---|
| Which of the following best describes sustainability in healthcare? | Reducing the environmental impact of healthcare operations | 143 (48.0) |
| Increasing the financial profits of healthcare facilities | 51 (17.1) | |
| Enhancing patient comfort regardless of environmental cost | 60 (20.1) | |
| None of the above | 44 (14.8) | |
| What are the key areas of focus in sustainable healthcare? | Water conservation | 12 (4.0) |
| Energy efficiency | 39 (13.1) | |
| Waste management | 44 (14.8) | |
| All the above | 203 (68.1) | |
| Which sustainable practices are incorporated into your daily routine? (Select all that apply) | Digital documentation to reduce paper use | 159 (53.4) |
| Energy-efficient lighting | 41 (13.8) | |
| Water-saving fixtures | 26 (8.7) | |
| Using reusable materials | 72 (24.2) | |
| How often do you engage in practices to reduce energy consumption at your workplace? | Daily | 66 (22.1) |
| Weekly | 35 (11.7) | |
| Monthly | 33 (11.1) | |
| Rarely | 84 (28.2) | |
| Never | 80 (26.8) | |
| What type of waste disposal methods are you familiar with in your healthcare setting? | Chemical treatment | 51 (17.1) |
| Incineration | 89 (29.9) | |
| Recycling | 137 (46.0) | |
| Composting | 21 (7.0) | |
| What is the biggest barrier to implementing sustainable practices in healthcare? | Insufficient managerial support | 54 (18.1) |
| Lack of awareness and training | 149 (50.0) | |
| Financial constraints | 71 (23.8) | |
| Perceived impact on patient care | 24 (8.1) | |
| How do you prioritize sustainability in your clinical decisions? | It’s a primary consideration | 69 (23.2) |
| It’s of some importance, but secondary to patient care | 152 (51.0) | |
| I consider it when it’s convenient | 33 (11.1) | |
| I do not consider it at all | 44 (14.8) |
| Knowledge Questions | Responses (Frequency and %) | Mean | Median | Std. Dev | Decision | ||||
|---|---|---|---|---|---|---|---|---|---|
| SDA | DA | Neutral | AG | SAG | |||||
| Q1, I understand the concept of sustainability | 27 (9.1%) | 38 (12.7%) | 92 (30.9%) | 96 (32.2%) | 45 (15.1%) | 3.32 | 3 | 1.15 | High |
| Q2, I am aware of the impact of sustainability practices on patient care | 21 (7.5%) | 57 (19.0%) | 113 (37.8%) | 86 (28.2%) | 21 (7.5%) | 3.1 | 3 | 1.02 | High |
| Q3, I am familiar with my workplace’s sustainability | 54 (18.1%) | 77 (25.8%) | 101 (33.9%) | 54 (18.1%) | 12 (4.0%) | 2.64 | 3 | 1.1 | Low |
| Q4, I can identify the benefits of implementing sustainable practices in healthcare settings | 30 (10.1%) | 50 (16.8%) | 89 (29.9%) | 93 (31.2%) | 36 (12.1%) | 3.18 | 3 | 1.16 | High |
| Q5, I regularly update my knowledge on sustainability | 36 (12.1%) | 80 (26.8%) | 92 (30.9%) | 54 (18.1%) | 36 (12.1%) | 2.91 | 3 | 1.19 | Low |
| Q6, I am aware of the environmental impact of waste from healthcare facilities | 33 (11.1%) | 50 (16.8%) | 90 (30.2%) | 80 (26.8%) | 45 (15.1%) | 3.18 | 3 | 1.21 | High |
| Q7, I understand energy conservation in a healthcare setting | 30 (10.1%) | 39 (13.1%) | 91 (30.5%) | 90 (30.2%) | 48 (16.1%) | 3.29 | 3 | 1.18 | High |
| Weighted average: 3.09 | |||||||||
| Attitude Questions | Responses (Frequency and %) | Mean | Median | Std. Dev | Decision | ||||
|---|---|---|---|---|---|---|---|---|---|
| SDA | DA | Neutral | AG | SAG | |||||
| Q8, Sustainability is important in healthcare | 15 (5.0%) | 33 (11.1%) | 77 (25.8%) | 110 (36.9%) | 63 (21.1%) | 3.58 | 4 | 1.09 | High |
| Q9, Sustainable practices are essential for improving patient outcomes. | 30 (10.1%) | 33 (11.1%) | 100 (33.6%) | 90 (30.2%) | 45 (15.1%) | 3.29 | 3 | 1.16 | Low |
| Q10, Sustainability is prioritized at my workplace. | 18 (6.0%) | 71 (23.8%) | 104 (34.9%) | 57 (19.1%) | 48 (16.1%) | 3.15 | 3 | 1.14 | Low |
| Q11, Sustainability should be integrated into all health professional training programs. | 12 (4.0%) | 32 (107%) | 99 (33.2%) | 95 (31.9%) | 60 (20.1%) | 3.52 | 4 | 1.1 | High |
| Q12, I am motivated to learn more about sustainable healthcare practices. | 12 (4.0%) | 48 (16.1%) | 68 (22.8%) | 113 (37.9%) | 57 (19.1%) | 3.53 | 4 | 1.05 | High |
| Q13, Every health professional can promote sustainability. | 12 (4.0%) | 27 (9.1%) | 94 (31.5%) | 99 (33.2%) | 66 (22.1%) | 3.6 | 4 | 1.05 | High |
| Q14, The Healthcare sector can reduce its environmental impact. | 24 (8.1%) | 39 (13.1%) | 77 (25.8%) | 107 (35.9%) | 51 (17.1%) | 3.41 | 4 | 1.15 | High |
| Weighted average: 3.44 | |||||||||
| Questions for Practice | Responses (Frequency and %) | Mean | Median | Std. Dev | Decision | ||||
|---|---|---|---|---|---|---|---|---|---|
| SDA | DA | Neutral | AG | SAG | |||||
| Q15, I follow sustainability guidelines at work. | 27 (10.8%) | 71 (23.8%) | 86 (28.9%) | 90 (30.2%) | 24 (8.1%) | 3.04 | 3 | 1.11 | Low |
| Q16, I try to reduce waste in my daily work activities. | 27 (10.8%) | 62 (20.8%) | 72 (24.2%) | 90 (30.2%) | 47 (15.8%) | 3.23 | 3 | 1.21 | High |
| Q17, I encourage others to adopt sustainable practices at work. | 48 (16.1%) | 68 (22.8%) | 72 (24.2%) | 89 (29.9%) | 21 (7.0%) | 2.89 | 3 | 1.2 | Low |
| Q18, I participate in training/workshops on sustainability in healthcare when available. | 65 (21.8%) | 81 (27.2%) | 69 (23.1%) | 56 (18.8%) | 27 (9.1%) | 2.66 | 3 | 1.26 | Low |
| Q19, I use resources responsibly to minimize environmental impact | 24 (8.1%) | 59 (19.8%) | 110 (36.9%) | 72 (24.1%) | 33 (11.1%) | 3.03 | 3 | 1.15 | Low |
| Q20, I consider the environmental impact of my clinical decisions. | 36 (12.1%) | 56 (18.8%) | 95 (31.9%) | 84 (28.2%) | 27 (9.1%) | 3.1 | 3 | 1.09 | Low |
| Q21, I support initiatives aimed at reducing energy consumption. | 36 (12.1%) | 35 (11.7%) | 99 (33.2%) | 98 (32.9%) | 30 (10.1%) | 3.17 | 3 | 1.14 | Low |
| Q22, I make suggestions for improving sustainability practices at work. | 33 (11.1%) | 77 (25.8%) | 99 (33.2%) | 63 (21.1%) | 26 (8.7%) | 2.91 | 3 | 1.12 | Low |
| Q23, I follow proper disposal procedures for different types of waste. | 24 (8.1%) | 60 (20.1%) | 71 (23.8%) | 92 (30.9%) | 51 (17.1%) | 3.29 | 3 | 1.2 | High |
| Q24 I actively engage in discussions about sustainability issues at work. | 39 (13.1%) | 95 (31.9%) | 89 (29.9%) | 48 (16.1%) | 27 (9.1%) | 2.76 | 3 | 1.15 | Low |
| Q25, I seek out sustainable product alternatives for use in my clinical practice. | 45 (15.1%) | 74 (24.8%) | 93 (31.2%) | 60 (20.2%) | 26 (8.7%) | 2.83 | 3 | 1.17 | Low |
| Q26, I try to implement sustainable practices in my daily life activities. | 30 (10.1%) | 68 (22.8%) | 102 (34.2%) | 75 (25.16%) | 23 (7.7%) | 2.98 | 3 | 1.09 | Low |
| Q27, I contribute to sustainability feedback processes at work. | 42 (14.1%) | 104 (34.9%) | 95 (31.9%) | 39 (13.1%) | 18 (6.0%) | 2.62 | 3 | 1.07 | Low |
| Q 28 I evaluate the effectiveness of my sustainability practices regularly. | 15 (5.0%) | 36 (12.0%) | 66 (22.1%) | 118 (39.6%) | 63 (21.1%) | 2.76 | 3 | 1.11 | Low |
| Q29 There is a lack of training on sustainable practices. | 15 (5.0%) | 24 (8.1%) | 39 (13.1%) | 148 (49.7%) | 72 (24.2%) | 3.8 | 4 | 1.05 | High |
| Weighted average: 3.00 | |||||||||
| Barriers Questions | Responses (Frequency and %) | Mean | Median | STD | Decision | ||||
|---|---|---|---|---|---|---|---|---|---|
| SDA | DA | Neutral | AG | SAG | |||||
| Q30 There is insufficient financial support to implement sustainable practices. | 39 (13.1%) | 89 (29.9%) | 95 (31.9%) | 54 (18.1%) | 21 (7.0%) | 3.6 | 4 | 1.1 | Low |
| Q31 Current workload and staff shortages make it difficult to prioritize sustainability | 15 (5.0%) | 27 (9.1%) | 69 (23.2%) | 85 (28.5%) | 102 (34.2%) | 3.78 | 4 | 1.16 | High |
| Q32 There is a lack of leadership commitment to sustainability. | 18 (6.0%) | 21 (7.0%) | 64 (21.5%) | 120 (40.3%) | 75 (25.2%) | 3.71 | 4 | 1.1 | High |
| Q33 The benefits of implementing sustainability are not well communicated. | 18 (6.0%) | 27 (9.1%) | 89 (29.9%) | 125 (41.9%) | 39 (13.1%) | 3.47 | 4 | 1.03 | Low |
| Weighted average 3.64 | |||||||||
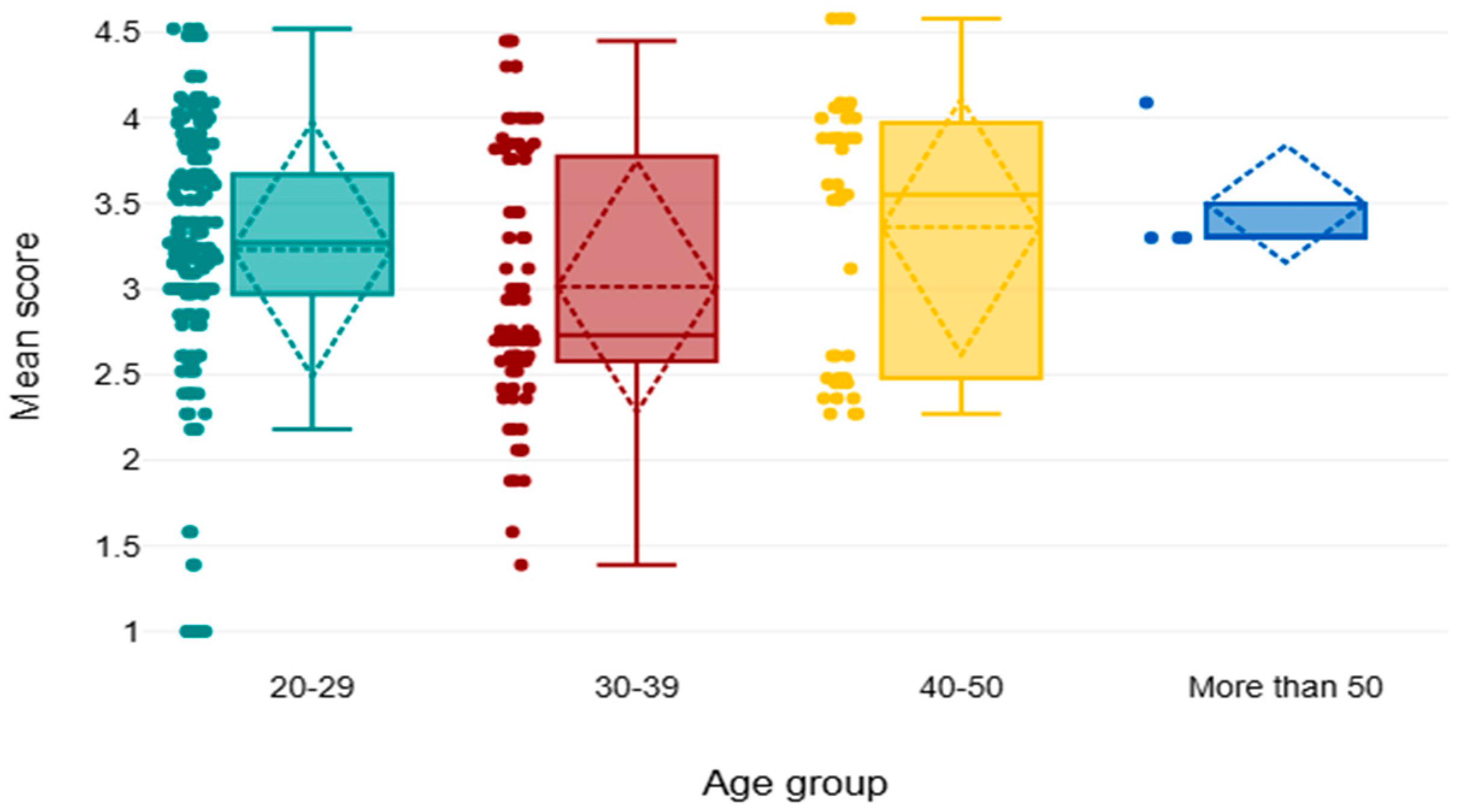
| Categories | Domains | n | Median | Mean Rank | Chi2 | p | |
|---|---|---|---|---|---|---|---|
| Age groups | Knowledge | 20–29 | 168 | 3.07 | 146.18 | 6.28 | 0.099 |
| 30–39 | 84 | 2.86 | 140.84 | ||||
| 40–50 | 42 | 3.43 | 175.19 | ||||
| More than 50 | 4 | 3.57 | 201 | ||||
| Attitude | 20–29 | 168 | 3.71 | 157.32 | 9.64 | 0.022 | |
| 30–39 | 84 | 3 | 125.37 | ||||
| 40–50 | 42 | 4 | 166.42 | ||||
| More than 50 | 4 | 3.43 | 150.38 | ||||
| Practice | 20–29 | 168 | 3.07 | 163.61 | 20.44 | <0.001 | |
| 30–39 | 84 | 2.53 | 113.96 | ||||
| 40–50 | 42 | 3.27 | 160.07 | ||||
| More than 50 | 4 | 3.07 | 192 | ||||
| Barriers | 20–29 | 168 | 3.5 | 136.56 | 10.05 | 0.018 | |
| 30–39 | 84 | 4 | 171.46 | ||||
| 40–50 | 42 | 4 | 158.96 | ||||
| More than 50 | 4 | 3.5 | 132.38 | ||||
| Overall | 20–29 | 168 | 3.27 | 156.78 | 10.53 | 0.015 * | |
| 30–39 | 84 | 2.73 | 124.71 | ||||
| 40–50 | 42 | 3.55 | 166.37 | ||||
| >50 | 4 | 3.3 | 187.13 | ||||
| Total | 298 | 3.26 |
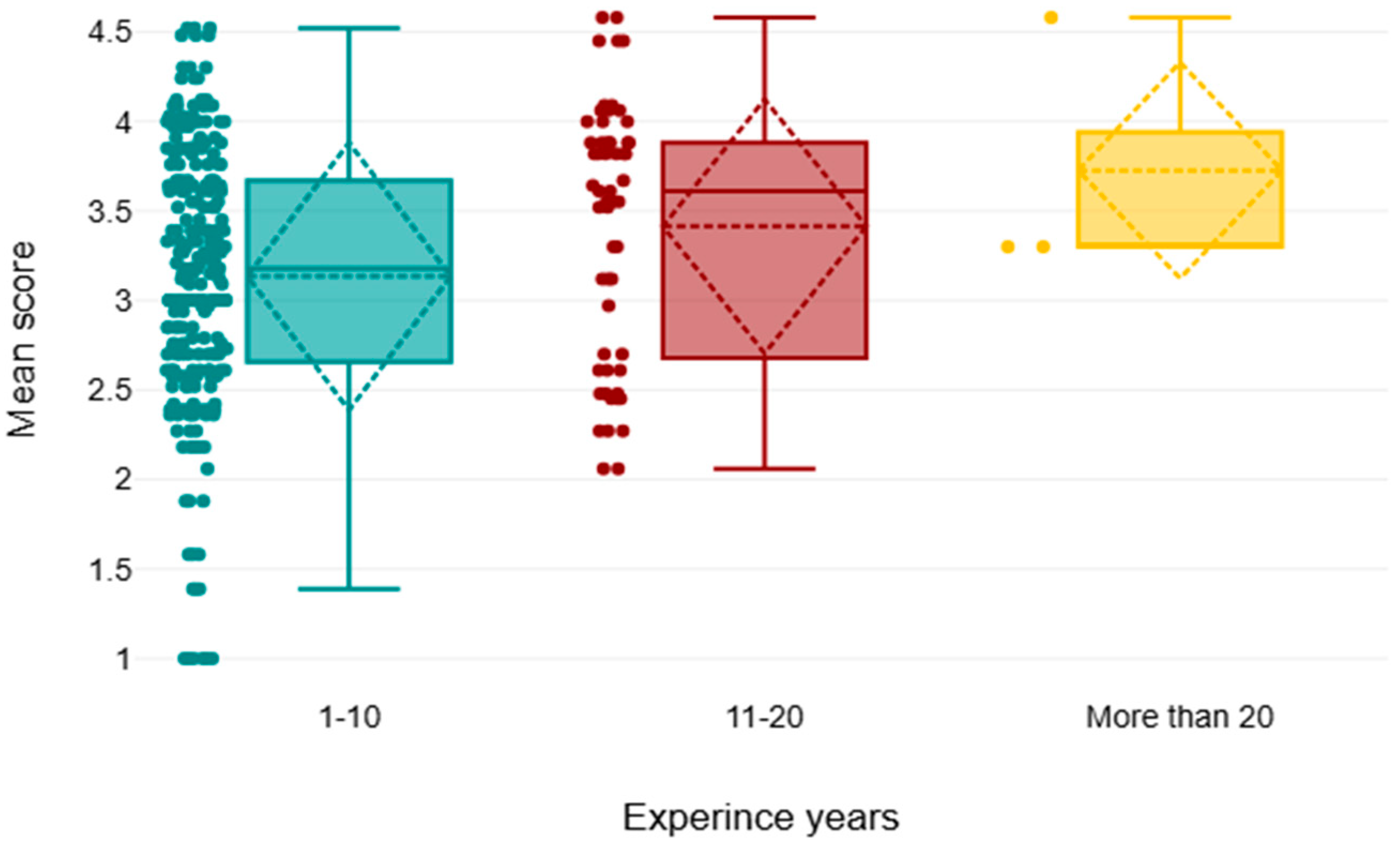
| Domains | Experience/Years | Numbers | Median | Mean Rank | Chi2 | p Value | |
|---|---|---|---|---|---|---|---|
| Knowledge | Experiences | 1–10 | 239 | 3.00 | 140.95 | 12.78 | 0.002 * |
| 11–20 | 56 | 3.57 | 181.71 | ||||
| >20 | 3 | 3.57 | 229.00 | ||||
| Awareness | 1–10 | 239 | 3.57 | 142.16 | 8.82 | 0.012 * | |
| 11–20 | 56 | 4.14 | 179.67 | ||||
| >20 | 3 | 3.43 | 170.83 | ||||
| Practice | 1–10 | 239 | 3.00 | 145.63 | 3.10 | 0.212 | |
| 11–20 | 56 | 3.27 | 163.05 | ||||
| >20 | 3 | 3.07 | 204.67 | ||||
| Barriers | 1–10 | 239 | 3.75 | 145.51 | 2.97 | 0.227 | |
| 11–20 | 56 | 4.00 | 167.16 | ||||
| >20 | 3 | 3.5 | 137.50 | ||||
| Overall | 1–10 | 239 | 3.18 | 143.28 | 6.68 | 0.035 * | |
| 11–20 | 56 | 3.61 | 173.09 | ||||
| >20 | 3 | 3.3 | 204.67 | ||||
| Total | 298 | 3.26 |
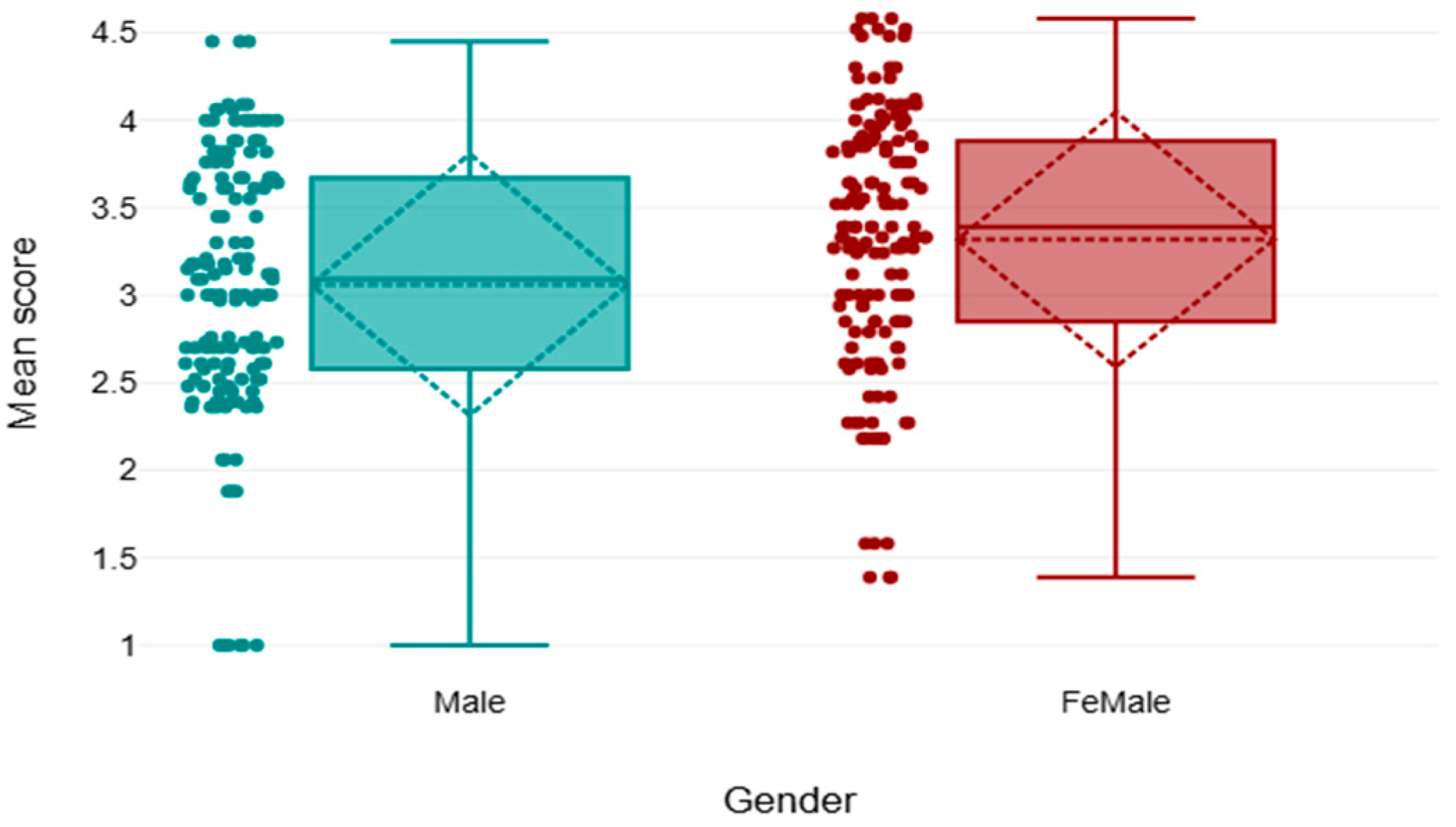
| Categories | n | Mean Rank | U | Z | p | r | ||
|---|---|---|---|---|---|---|---|---|
| Gender | Knowledge | Male | 145 | 139.80 | 9685.50 | −1.90 | 0.059 | 0.11 |
| Females | 153 | 158.70 | ||||||
| Attitude | Male | 145 | 130.89 | 8394.00 | −3.64 | <0.001 | 0.21 | |
| Females | 153 | 167.14 | ||||||
| Practice | Male | 145 | 134.47 | 8913.00 | −2.93 | 0.003 | 0.17 | |
| Females | 153 | 163.75 | ||||||
| Barriers | Male | 145 | 150.48 | 10,950.00 | −0.19 | 0.849 | 0.01 | |
| Females | 153 | 148.57 | ||||||
| Overall | Male | 145 | 134.21 | 8875.5 | −2.98 | 0.003 | 0.17 | |
| Female | 153 | 163.99 | ||||||
| Area of work | Knowledge | Hospital | 268 | 154.76 | 2611.50 | −3.15 | 0.002 | 0.18 |
| Clinic | 30 | 102.55 | ||||||
| Attitude | Hospital | 268 | 154.10 | 2787.00 | −2.76 | 0.006 | 0.16 | |
| Clinic | 30 | 108.40 | ||||||
| Practice | Hospital | 268 | 154.26 | 2743.50 | −2.85 | 0.004 | 0.17 | |
| Clinic | 30 | 106.95 | ||||||
| Barriers | Hospital | 268 | 153.04 | 3070.50 | −2.14 | 0.034 | 0.12 | |
| Clinic | 30 | 117.85 | ||||||
| Overall | Hospital | 268 | 154.89 | 2575.5 | −3.23 | 0.001 | 0.19 | |
| Clinic | 30 | 101.35 | ||||||
| Total | 298 | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hamd, Z.Y.; Alkahtani, T.O.; Almudaimeegh, L.; Gareeballah, A.; Aljamal, M.; Abuzaid, M.; Alhaarbi, N.; Alqarni, B.; Alnoufal, J.; Alanazi, S.; et al. Integrating Sustainability in Radiology: Challenges and Opportunities from the Perspective of Radiology Professionals in Saudi Arabia. Healthcare 2025, 13, 3038. https://doi.org/10.3390/healthcare13233038
Hamd ZY, Alkahtani TO, Almudaimeegh L, Gareeballah A, Aljamal M, Abuzaid M, Alhaarbi N, Alqarni B, Alnoufal J, Alanazi S, et al. Integrating Sustainability in Radiology: Challenges and Opportunities from the Perspective of Radiology Professionals in Saudi Arabia. Healthcare. 2025; 13(23):3038. https://doi.org/10.3390/healthcare13233038
Chicago/Turabian StyleHamd, Zuhal Y., Tahani O. Alkahtani, Lama Almudaimeegh, Awadia Gareeballah, Mohammad Aljamal, Mohamed Abuzaid, Nada Alhaarbi, Bayan Alqarni, Jood Alnoufal, Shmouk Alanazi, and et al. 2025. "Integrating Sustainability in Radiology: Challenges and Opportunities from the Perspective of Radiology Professionals in Saudi Arabia" Healthcare 13, no. 23: 3038. https://doi.org/10.3390/healthcare13233038
APA StyleHamd, Z. Y., Alkahtani, T. O., Almudaimeegh, L., Gareeballah, A., Aljamal, M., Abuzaid, M., Alhaarbi, N., Alqarni, B., Alnoufal, J., Alanazi, S., & Aldhahi, A. (2025). Integrating Sustainability in Radiology: Challenges and Opportunities from the Perspective of Radiology Professionals in Saudi Arabia. Healthcare, 13(23), 3038. https://doi.org/10.3390/healthcare13233038








