Influencing Factors of Health Status of Clinical Doctors in Tertiary Medical Institutions Based on Structural Equation Modeling
Highlights
- Clinicians exhibited significant differences in physical health, mental health, social health, and overall health scores, with mental health scores being the lowest, particularly among younger physicians.
- Age, years of practice, professional title, health status, sleep duration, and exercise duration are significantly associated with the health of clinical physicians.
- Physical health serves as the foundation, influencing both physiological and social well-being, which together are related to a physician’s overall health status.
- The health status of clinical physicians, particularly their mental health, warrants special attention.
- Improving physicians’ health requires equal attention to physical, mental, and social well-being—all three are essential.
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. General Information
3.2. Health Status of Clinical Doctors in Tertiary Medical Institutions
3.3. Reliability Analysis of the Questionnaire and Results of CFA
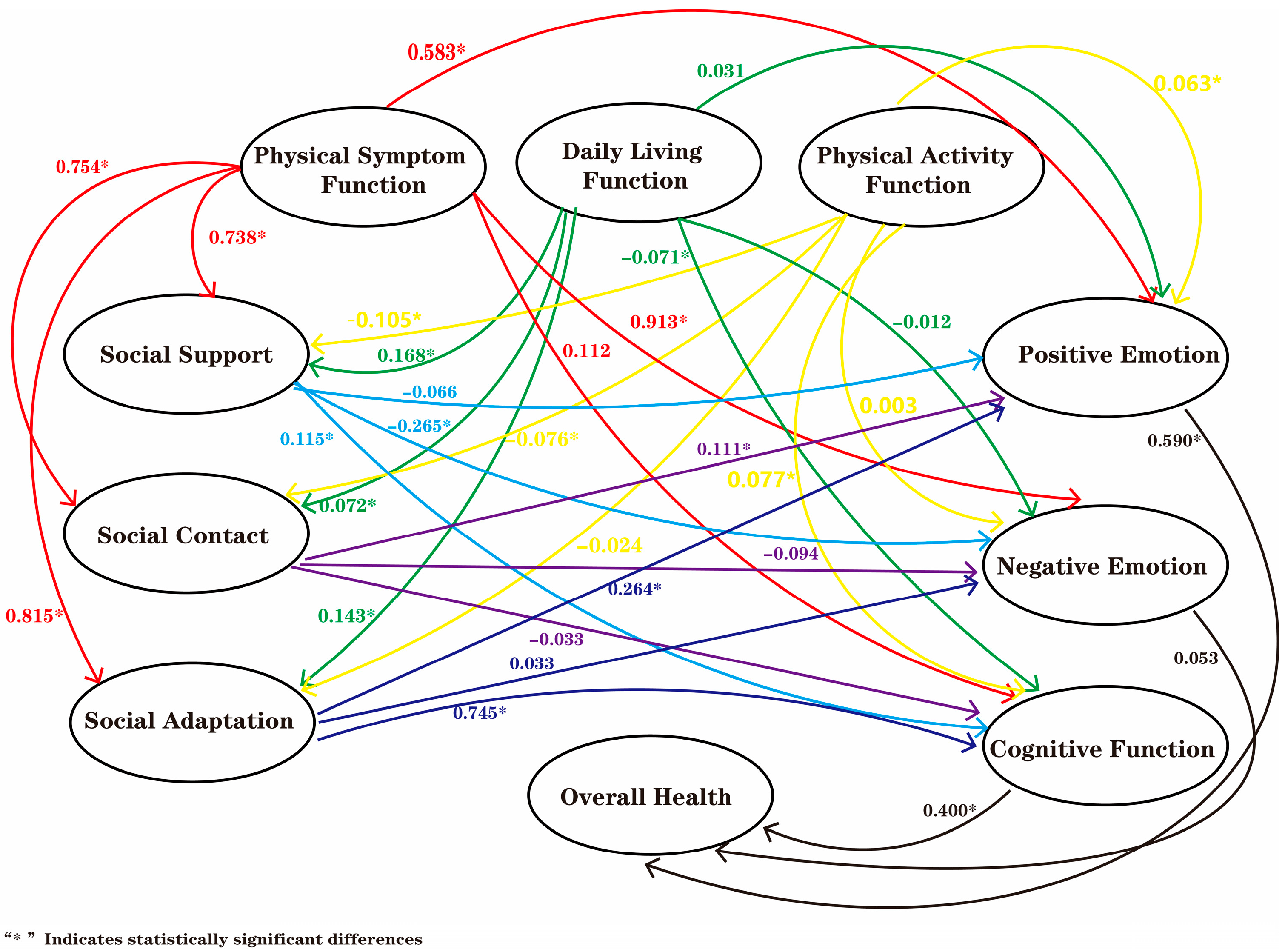
3.4. Structural Equation Model (SEM) Analysis
4. Discussion
4.1. Factors Associated with the Health of Clinical Doctors
4.2. The Relationship Between Physical Health and Social and Mental Health
4.3. The Relationship Between Social Health and Mental Health
4.4. The Relationship Between Mental Health and Overall Health
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chen, X.; Ma, J.; Wu, Y.; Wang, H.; Cao, M.; Liu, Y. Current status and trend of workload of health professionals in Chinese public hospitals. J. Chin. Res. Hospitals 2020, 7, 31–35+141–147. [Google Scholar]
- Thatrimontrichai, A.; Weber, D.J.; Apisarnthanarak, A. Mental health among healthcare personnel during COVID-19 in Asia: A systematic review. J. Formos. Med. Assoc. 2021, 120, 1296–1304. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Wang, Y.; Shi, K.; Chen, G.; Tang, S.; Li, Y.; Su, J.; Wu, S.; Zeng, Q. Analysis of psychological status and influencing factors of medical workers amid COVID-19 pandemic; analysis of influencing factors. Chin. J. Health Manag. 2021, 15, 167–172. [Google Scholar]
- Galanakis, M.D.; Tsitouri, E. Positive psychology in the working environment. Job demands-resources theory, work engagement and burnout: A systematic literature review. Front. Psychol. 2022, 13, 1022102. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E. The Job Demands-Resources model: State of the art. J. Manag. Psychol. 2007, 22, 309–328. [Google Scholar] [CrossRef]
- Gillman, J.C.; Turner, M.J.; Slater, M.J. The role of social support and social identification on challenge and threat cognitive appraisals, perceived stress, and life satisfaction in workplace employees. PLoS ONE 2023, 18, e0288563. [Google Scholar] [CrossRef] [PubMed]
- Dellafiore, F.; Arrigoni, C.; Nania, T.; Caruso, R.; Baroni, I.; Vangone, I.; Russo, S.; Barello, S. The impact of COVID-19 pandemic on family caregivers’ mental health: A rapid systematic review of the current evidence. Acta Biomed. 2022, 93, e2022154. [Google Scholar]
- Barello, S.; Falcó-Pegueroles, A.; Rosa, D.; Tolotti, A.; Graffigna, G.; Bonetti, L. The psychosocial impact of flu influenza pandemics on healthcare workers and lessons learnt for the COVID-19 emergency: A rapid review. Int. J. Public Health 2020, 65, 1205–1216. [Google Scholar] [CrossRef]
- Belita, E.; Neil-Sztramko, S.E.; Seale, C.; Zhou, F.; Zogo, C.O.; Boamah, S.; Cabaj, J.; Jack, S.M.; Banfield, L.; Neudorf, C.; et al. Organizational interventions to support and promote the mental health of healthcare workers during pandemics and epidemics: A systematic review. BMC Health Serv. Res. 2025, 25, 731. [Google Scholar] [CrossRef]
- Duan, T.; Huang, X.; Liu, S.; Hu, W.; Liu, T.; Li, Y.; Cun, B. Prevalence of job burnout among healthcare workers during the COVID-19 pandemic:a meta-analysis. J. Prev. Med. 2023, 35, 526–532. [Google Scholar]
- Liu, R.; Zhao, Q.; Dong, W.; Guo, D.; Shen, Z.; Li, Y.; Zhang, W.; Zhu, D.; Zhang, J.; Bai, J.; et al. Assessing public health service capability of primary healthcare personnel: A large-scale survey in Henan Province, China. BMC Health Serv. Res. 2024, 24, 627. [Google Scholar] [CrossRef]
- Cheng, Y.; Cao, X.; Zhang, J.; Xu, L.; Qin, L. Comprehensive assessment of emergency departments in county-level public hospitals: A multicenter descriptive cross-sectional study in Henan province, China. Front. Public Health 2023, 11, 1301030. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Zhang, J.; Feng, L.; Qiu, J. Self-rated health of population in Southern China: Association with socio-demographic characteristics measured with multiple-item self-rated health measurement scale. BMC Public Health 2010, 10, 393. [Google Scholar] [CrossRef]
- Tarka, P. An overview of structural equation modeling: Its beginnings, historical development, usefulness and controversies in the social sciences. Qual. Quant. 2018, 52, 313–354. [Google Scholar] [CrossRef]
- Hair, J.F.; Risher, J.J.; Sarstedt, M.; Ringle, C.M. When to use and how to report the results of PLS-SEM. Eur. Bus. Rev. 2019, 31, 2–24. [Google Scholar] [CrossRef]
- Li, S.; Liu, L.; Wang, Y.; Deng, X. Determinants of rural middle school students’ adoption of AI chatbots for mental health. Front. Public Health 2025, 13, 1619535. [Google Scholar] [CrossRef]
- Jiang, G.; Tan, X.; Wang, H.; Xu, M.; Wu, X. Exploratory and confirmatory factor analyses identify three structural dimensions for measuring physical function in community-dwelling older adults. PeerJ 2023, 11, e15182. [Google Scholar] [CrossRef]
- Odonkor, S.T.; Adams, S. Predictors of stress and associated factors among healthcare workers in Western Ghana. Heliyon 2021, 7, e07223. [Google Scholar] [CrossRef]
- Izdebski, Z.; Kozakiewicz, A.; Białorudzki, M.; Dec-Pietrowska, J.; Mazur, J. Occupational Burnout in Healthcare Workers, Stress and Other Symptoms of Work Overload during the COVID-19 Pandemic in Poland. Int. J. Environ. Res. Public Health 2023, 20, 2428. [Google Scholar] [CrossRef] [PubMed]
- Adam, A.R.; Golu, F.T. Prevalence of depression among physicians: A comprehensive meta-analysis. Rom. Med. J. 2021, 68, 327–337. [Google Scholar] [CrossRef]
- Liu, T.; Chen, S.; Yang, S. Meta-analysis of mental health status of front-line medical staff in the fight against the epidemic in China based on SCL-90. Occup. Health 2023, 39, 1263–1267. [Google Scholar]
- Ng, A.P.P.; Chin, W.Y.; Wan, E.Y.F.; Chen, J.; Lau, C.S. Health-related quality of life in Hong Kong physicians up to 20 years post-graduation: A cross-sectional survey. PLoS ONE 2023, 18, e0284253. [Google Scholar] [CrossRef]
- Nassar, A.K.; Waheed, A.; Tuma, F. Academic Clinicians’ Workload Challenges and Burnout Analysis. Cureus 2019, 11, e6108. [Google Scholar] [CrossRef] [PubMed]
- Ren, J.; Gao, F.; Zheng, Y.; Wang, X.; Wan, L.; Chen, W.; Sun, Y.; Wang, Y. A single center survey and analysis on the psychological stress status and influencing factors of medical staff. Chin. J. Health Manag. 2023, 17, 544–548. [Google Scholar]
- Győrffy, Z.; Dweik, D.; Girasek, E. Workload, mental health and burnout indicators among female physicians. Hum. Resour. Health 2016, 14, 12. [Google Scholar] [CrossRef]
- Nagle, E.; Griskevica, I.; Rajevska, O.; Ivanovs, A.; Mihailova, S.; Skruzkalne, I. Factors affecting healthcare workers burnout and their conceptual models: Scoping review. BMC Psychol. 2024, 12, 637. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Zhu, S.; Shao, S. Study on Health Literacy Level and Influencing Factors of Medical Staff in the Tertiary Hospital of Hangzhou City. J. Nurs. Sci. 2024, 13, 1042–1049. [Google Scholar] [CrossRef]
- EUrbón CSalavera JMLópez-Chamorro, A.F. Diaz-Carrasco. Relationship Between Sleep Duration and Psychosocial Well-Being in Healthcare Personnel: Identification of Predictors and Vulnerability Patterns. Behav. Sci. 2025, 15, 1290. [Google Scholar]
- Saintila, J.; Soriano-Moreno, A.N.; Ramos-Vera, C.; Oblitas-Guerrero, S.M.; Calizaya-Milla, Y.E. Association between sleep duration and burnout in healthcare professionals: A cross-sectional survey. Front. Public Health 2023, 11, 1268164. [Google Scholar] [CrossRef]
- Mincarone, P.; Bodini, A.; Tumolo, M.R.; Sabina, S.; Colella, R.; Mannini, L.; Sabato, E.; Leo, C.G. Association Between Physical Activity and the Risk of Burnout in Health Care Workers: Systematic Review. JMIR Public Health Surveill. 2024, 10, e49772. [Google Scholar] [CrossRef]
- McKeon, G.; Steel, Z.; Wells, R.; Fitzpatrick, A.; Vancampfort, D.; Rosenbaum, S. Exercise and PTSD Symptoms in Emergency Service and Frontline Medical Workers: A Systematic Review. Transl. J. Am. Coll. Sports Med. 2022, 7, e000189. [Google Scholar] [CrossRef]
- Zhou, F.; Sun, X.; Shen, L.; Wu, C.; Zhang, J.; Lin, J. Analysis of the health status of medical staff in tertiary hospitals of Shaoxing and countermeasures. Chin. J. Crit. Care Med. 2015, 8, 377–378. [Google Scholar]
- Schmuck, J.; Hiebel, N.; Rabe, M.; Schneider, J.; Erim, Y.; Morawa, E.; Jerg-Bretzke, L.; Beschoner, P.; Albus, C.; Hannemann, J.; et al. Sense of coherence, social support and religiosity as resources for medical personnel during the COVID-19 pandemic: A web-based survey among 4324 health care workers within the German Network University Medicine. PLoS ONE 2021, 16, e0255211. [Google Scholar] [CrossRef]
- Hinz, A.; Esser, P.; Richter, D.; Schönfelder, A.; Glaesmer, H.; Lehmann-Laue, A.; Heyne, S.; Leuteritz, K.; Sender, A.; Springer, F.; et al. Social support in a large general population sample over the course of six years. Sci. Rep. 2025, 15, 6405. [Google Scholar] [CrossRef]
- Bentulila, Y.; Shalem, L.L.; Cohen, B.; Adler, L. Physical work environment and burnout among primary care physicians in Israel: A cross-sectional study. BMC Prim. Care 2024, 25, 74. [Google Scholar] [CrossRef]
- Guo, X.D.; Zheng, H.; Ruan, D.; Hu, D.D.; Wang, Y.; Wang, Y.Y.; Raymond, C.K. Associations between empathy and negative affect: Effect of emotion regulation. Acta Psychol. Sin. 2023, 55, 892–904. [Google Scholar] [CrossRef]
- Sun, Y.; Lv, J.; Lan, F.; Zhang, L. Emotion regulation strategy of self-focused and situation-focused reappraisal and their impact on subsequent cognitive control. Acta Psychol. Sin. 2020, 52, 1393–1406. [Google Scholar] [CrossRef]
- Jefferson, L.; Heathcote, C.; Bloor, K. General practitioner well-being during the COVID-19 pandemic: A qualitative interview study. BMJ Open 2023, 13, e061531. [Google Scholar] [CrossRef]
- Santini, Z.I.; Jose, P.E.; Cornwell, E.Y.; Koyanagi, A.; Nielsen, L.; Hinrichsen, C.; Meilstrup, C.; Madsen, K.R.; Koushede, V. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Health 2020, 5, e62–e70. [Google Scholar] [CrossRef]
- Cacioppo, S.; Grippo, A.J.; London, S.; Goossens, L.; Cacioppo, J.T. Loneliness: Clinical import and interventions. Perspect. Psychol. Sci. 2015, 10, 238–249. [Google Scholar] [CrossRef]
- Asaoka, H.; Watanabe, K.; Miyamoto, Y.; Restrepo-Henao, A.; van der Ven, E.; Moro, M.F.; Alnasser, L.A.; Ayinde, O.; Balalian, A.A.; Basagoitia, A.; et al. Association of depressive symptoms with incidence and mortality rates of COVID-19 over 2 years among healthcare workers in 20 countries: Multi-country serial cross-sectional study. BMC Med. 2024, 22, 386. [Google Scholar] [CrossRef] [PubMed]
- Pressman, S.D.; Jenkins, B.N.; Moskowitz, J.T. Positive Affect and Health: What Do We Know and Where Next Should We Go? Annu. Rev. Psychol. 2019, 70, 627–650. [Google Scholar] [CrossRef] [PubMed]
- Hagger, M.S.; Koch, S.; Chatzisarantis, N.L.D.; Orbell, S. The common sense model of self-regulation: Meta-analysis and test of a process model. Psychol. Bull. 2017, 143, 1117–1154. [Google Scholar] [CrossRef]
- Smith, B.J.; Lim, M.H. How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Res. Pract. 2020, 30, e3022008. [Google Scholar] [CrossRef] [PubMed]
| Variable | n | Physical Health (170) | Mental Health (150) | Social Health (120) | Overall Health (40) | Total Score (480) |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Male | 333 | 127.64 ± 22.51 | 88.38 ± 23.05 | 80.20 ± 79.46 | 26.62 ± 6.94 | 322.92 ± 53.69 |
| Female | 410 | 127.31 ± 20.32 | 88.20 ± 25.30 | 79.46 ± 18.72 | 26.82 ± 7.30 | 321.77 ± 57.60 |
| Age | ||||||
| <25 | 25 | 124.92 ± 26.85 | 89.48 ± 22.37 * | 81.12 ± 18.13 * | 28.72 ± 5.66 * | 324.24 ± 51.18 * |
| <45 | 636 | 127.70 ± 20.96 | 86.95 ± 24.00 | 78.53 ± 18.27 | 26.30 ± 7.20 | 319.49 ± 55.65 |
| ≥45 | 82 | 126.34 ± 22.43 | 98.20 ± 25.29 | 89.50 ± 16.99 | 29.39 ± 6.34 | 343.43 ± 54.73 |
| Working Years | ||||||
| <5 | 212 | 128.20 ± 21.90 | 88.85 ± 23.94 | 80.89 ± 17.15 * | 27.54 ± 6.64 | 325.50 ± 53.31 |
| <11 | 300 | 127.74 ± 20.38 | 86.54 ± 25.44 | 77.49 ± 19.42 | 26.09 ± 7.70 | 317.86 ± 59.11 |
| ≥11 | 231 | 126.40 ± 22.01 | 90.00 ± 23.11 | 81.90 ± 17.99 | 26.80 ± 6.76 | 325.09 ± 53.57 |
| Education Level | ||||||
| Bachelor | 384 | 126.30 ± 23.11 | 88.92 ± 23.71 | 80.84 ± 18.20 | 27.09 ± 7.04 | 323.16 ± 50.26 |
| Master | 324 | 129.00 ± 18.26 | 87.40 ± 24.82 | 78.94 ± 18.21 | 26.19 ± 7.17 | 321.53 ± 54.50 |
| Doctorate | 30 | 124.27 ± 28.18 | 90.20 ± 27.06 | 78.60 ± 23.41 | 27.67 ± 7.99 | 320.73 ± 68.46 |
| Others | 5 | 135.60 ± 4.72 | 83.80 ± 25.80 | 67.60 ± 15.19 | 27.00 ± 4.90 | 314.00 ± 37.35 |
| Marital Status | ||||||
| Unmarried | 177 | 127.28 ± 22.25 | 88.20 ± 25.95 | 80.76 ± 18.90 | 27.24 ± 7.52 | 323.49 ± 60.44 |
| Married | 566 | 127.51 ± 21.04 | 88.30 ± 23.81 | 79.54 ± 18.29 | 26.56 ± 7.00 | 321.91 ± 54.38 |
| Professional Title | ||||||
| Resident physician | 280 | 128.26 ± 21.95 | 89.16 ± 25.31 * | 80.84 ± 18.82 * | 27.64 ± 7.22 * | 325.90 ± 58.69 * |
| Attending Physician | 316 | 126.34 ± 21.62 | 85.03 ± 23.27 | 77.21 ± 18.01 | 25.45 ± 7.112 | 333.33 ± 51.95 |
| Associate Chief Physician | 119 | 129.37 ± 18.72 | 93.50 ± 23.39 | 82.80 ± 18.14 | 27.66 ± 6.62 | 305.6 ± 46.68 |
| Chief Physician | 28 | 123.82 ± 21.78 | 93.75 ± 25.38 | 86.71 ± 16.66 | 28.11 ± 6.61 | 332.39 ± 57.38 |
| Disease | ||||||
| With Disease | 108 | 127.02 ± 18.23 | 82.11 ± 23.73 * | 76.97 ± 17.36 | 23.63 ± 7.19 * | 309.73 ± 52.40 * |
| Without Disease | 635 | 127.53 ± 21.81 | 89.32 ± 24.28 | 80.33 ± 18.58 | 27.25 ± 7.00 | 324.42 ± 56.17 |
| Sleep Duration | ||||||
| ≤5 h | 28 | 120.32 ± 22.58 | 75.79 ± 26.87 * | 70.71 ± 21.64 * | 20.93 ± 9.51 * | 287.75 ± 65.71 * |
| <7 h | 545 | 127.79 ± 20.53 | 86.52 ± 24.14 | 79.09 ± 18.19 | 26.35 ± 6.94 | 319.74 ± 54.83 |
| ≥7 h | 170 | 127.56 ± 23.42 | 95.95 ± 22.61 | 83.72 ± 17.91 | 28.89 ± 6.57 | 336.13 ± 54.00 |
| Exercise Duration | ||||||
| 0 h | 139 | 126.91 ± 18.51 | 79.96 ± 25.14 * | 73.33 ± 18.42 * | 24.12 ± 7.91 * | 304.32 ± 56.33 * |
| <2 h | 427 | 127.76 ± 19.67 | 86.63 ± 23.11 | 78.76 ± 17.96 | 26.27 ± 6.85 | 319.42 ± 54.08 |
| <5 h | 130 | 126.05 ± 26.70 | 97.65 ± 23.79 | 87.19 ± 17.80 | 29.51 ± 6.25 | 340.39 ± 55.09 |
| ≥5 h | 47 | 130.19 ± 26.57 | 101.89 ± 21.00 | 88.40 ± 14.84 | 30.89 ± 5.17 | 351.38 ± 48.52 |
| Disease | n | (%) | Average Age at Diagnosis |
|---|---|---|---|
| Hypertension | 29 | 3.9 | 36.4 |
| Stroke | 1 | 0.1 | 29.0 |
| Coronary Heart Disease | 4 | 0.5 | 45.0 |
| Diabetes | 6 | 0.8 | 48.8 |
| Fatty Liver | 60 | 8.1 | 33.9 |
| Chronic Kidney Disease | 3 | 0.4 | 30.3 |
| Abnormal Lipid Levels | 43 | 5.8 | 36.2 |
| Variable | Mean | SD | Min | Max | Percentage | F | p |
|---|---|---|---|---|---|---|---|
| Physical Health (170) | 127.46 | 21.32 | 29.00 | 168.00 | 74.98 | 177.89 | <0.001 |
| Mental Health (150) | 88.27 | 24.32 | 12.00 | 150.00 | 58.85 | ||
| Social Health (120) | 79.83 | 18.43 | 16.00 | 120.00 | 66.53 | ||
| Overall Health (40) | 26.73 | 7.13 | 3.00 | 40.00 | 66.83 | ||
| Total Score (480) | 322.29 | 55.85 | 144.00 | 477.00 | 67.14 |
| Variable | Cronbach’s Alpha | Number of Items |
|---|---|---|
| Physical Health | 0.863 | 17 |
| Mental Health | 0.905 | 15 |
| Social Health | 0.908 | 12 |
| Overall Health | 0.847 | 4 |
| Overall reliability | 0.944 | 48 |
| Fit Index | Ideal Standard | General Standard | Result |
|---|---|---|---|
| CMIN/DF | 1–3 | 3–5 | 3.314 |
| RMSEA | <0.05 | <0.08 | 0.056 |
| TLI | >0.9 | >0.8 | 0.903 |
| CFI | >0.9 | >0.8 | 0.893 |
| IFI | >0.9 | >0.8 | 0.903 |
| GFI | >0.9 | >0.8 | 0.842 |
| AGFI | >0.9 | >0.8 | 0.818 |
| Path Relationship | Path Coefficient | p | ||
|---|---|---|---|---|
| Social Support | ← | Physical Symptom Function | 0.738 | <0.001 |
| Social Contact | ← | Physical Symptom Function | 0.754 | <0.001 |
| Social Adaptation | ← | Physical Symptom Function | 0.815 | <0.001 |
| Social Support | ← | Daily Living Function | 0.168 | <0.001 |
| Social Contact | ← | Daily Living Function | 0.072 | 0.025 |
| Social Adaptation | ← | Daily Living Function | 0.143 | <0.001 |
| Social Support | ← | Physical Activity Function | −0.105 | 0.004 |
| Social Contac | ← | Physical Activity Function | −0.076 | 0.018 |
| Social Adaptation | ← | Physical Activity Function | −0.024 | 0.43 |
| Positive Emotion | ← | Physical Symptom Function | 0.583 | <0.001 |
| Negative Emotion | ← | Physical Symptom Function | 0.913 | <0.001 |
| Cognitive Function | ← | Physical Symptom Function | 0.112 | 0.289 |
| Positive Emotion | ← | Daily Living Function | 0.031 | 0.319 |
| Negative Emotion | ← | Daily Living Function | −0.012 | 0.788 |
| Cognitive Function | ← | Daily Living Function | −0.071 | 0.028 |
| Positive Emotion | ← | Physical Activity Function | 0.063 | 0.022 |
| Negative Emotion | ← | Physical Activity Function | 0.003 | 0.936 |
| Cognitive Function | ← | Physical Activity Function | 0.077 | 0.008 |
| Cognitive Function | ← | Social Adaptation | 0.745 | <0.001 |
| Negative Emotion | ← | Social Adaptation | 0.033 | 0.713 |
| Positive Emotion | ← | Social Adaptation | 0.264 | <0.001 |
| Cognitive Function | ← | Social Contact | −0.033 | 0.513 |
| Negative Emotion | ← | Social Contact | −0.094 | 0.165 |
| Positive Emotion | ← | Social Contact | 0.111 | 0.025 |
| Cognitive Function | ← | Social Support | 0.115 | 0.044 |
| Negative Emotion | ← | Social Support | −0.265 | <0.001 |
| Positive Emotion | ← | Social Support | −0.066 | 0.235 |
| Overall Health | ← | Cognitive Function | 0.4 | <0.001 |
| Overall Health | ← | Negative Emotion | 0.053 | 0.065 |
| Overall Health | ← | Positive Emotion | 0.59 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ou, Y.; Yin, S.; Chen, S. Influencing Factors of Health Status of Clinical Doctors in Tertiary Medical Institutions Based on Structural Equation Modeling. Healthcare 2025, 13, 3019. https://doi.org/10.3390/healthcare13233019
Ou Y, Yin S, Chen S. Influencing Factors of Health Status of Clinical Doctors in Tertiary Medical Institutions Based on Structural Equation Modeling. Healthcare. 2025; 13(23):3019. https://doi.org/10.3390/healthcare13233019
Chicago/Turabian StyleOu, Yangfan, Shanshan Yin, and Shuaiyin Chen. 2025. "Influencing Factors of Health Status of Clinical Doctors in Tertiary Medical Institutions Based on Structural Equation Modeling" Healthcare 13, no. 23: 3019. https://doi.org/10.3390/healthcare13233019
APA StyleOu, Y., Yin, S., & Chen, S. (2025). Influencing Factors of Health Status of Clinical Doctors in Tertiary Medical Institutions Based on Structural Equation Modeling. Healthcare, 13(23), 3019. https://doi.org/10.3390/healthcare13233019








