From Crisis Response to Lasting Transformation: Five-Year Insights from the Implementation of Telemedicine in Neurosurgical Care During COVID-19
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Epidemiological Context: National and Regional Infection Data
3.2. Patient Demographics and Consultation Distribution
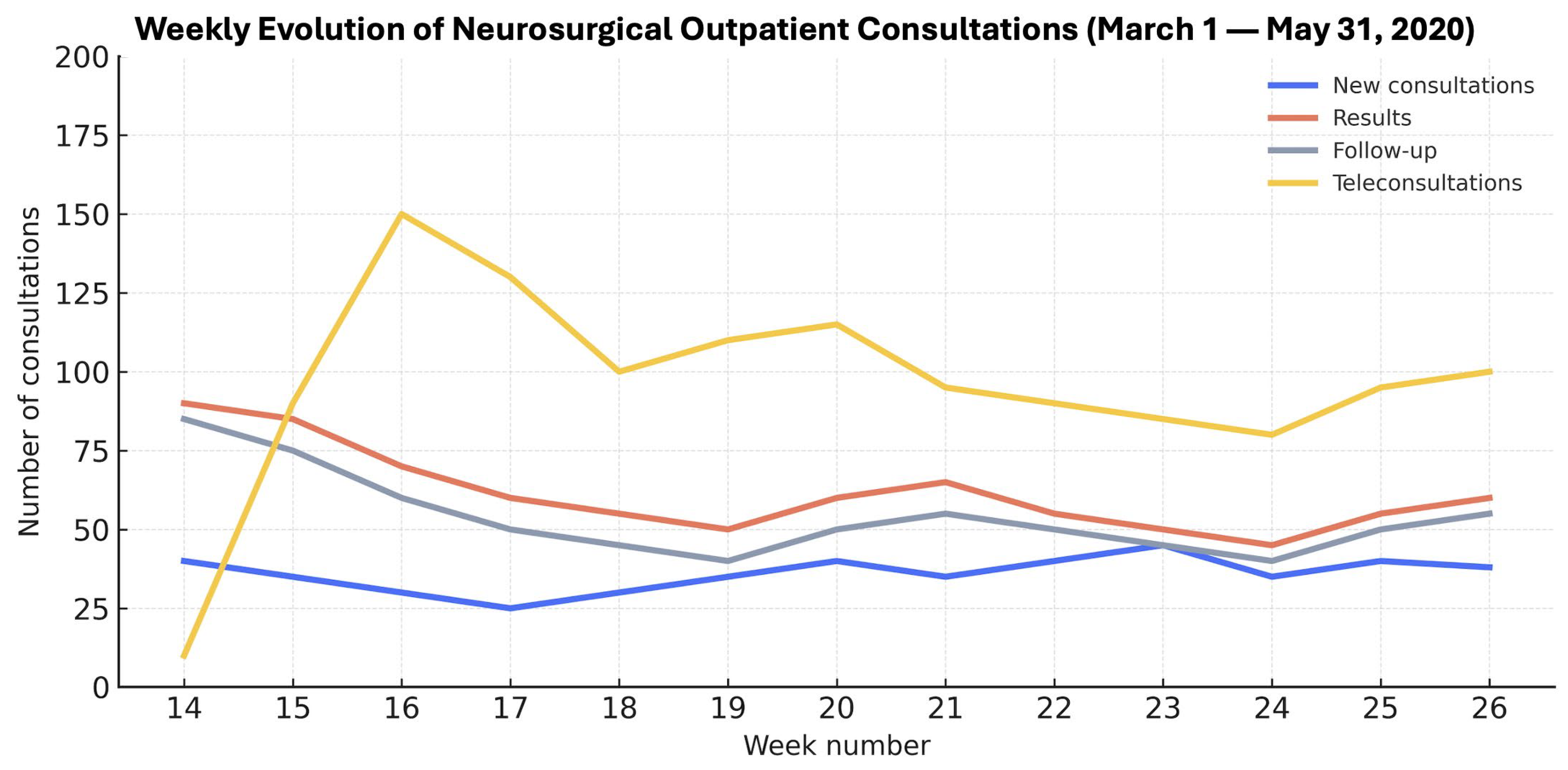
3.3. Consultation Types and Attendance
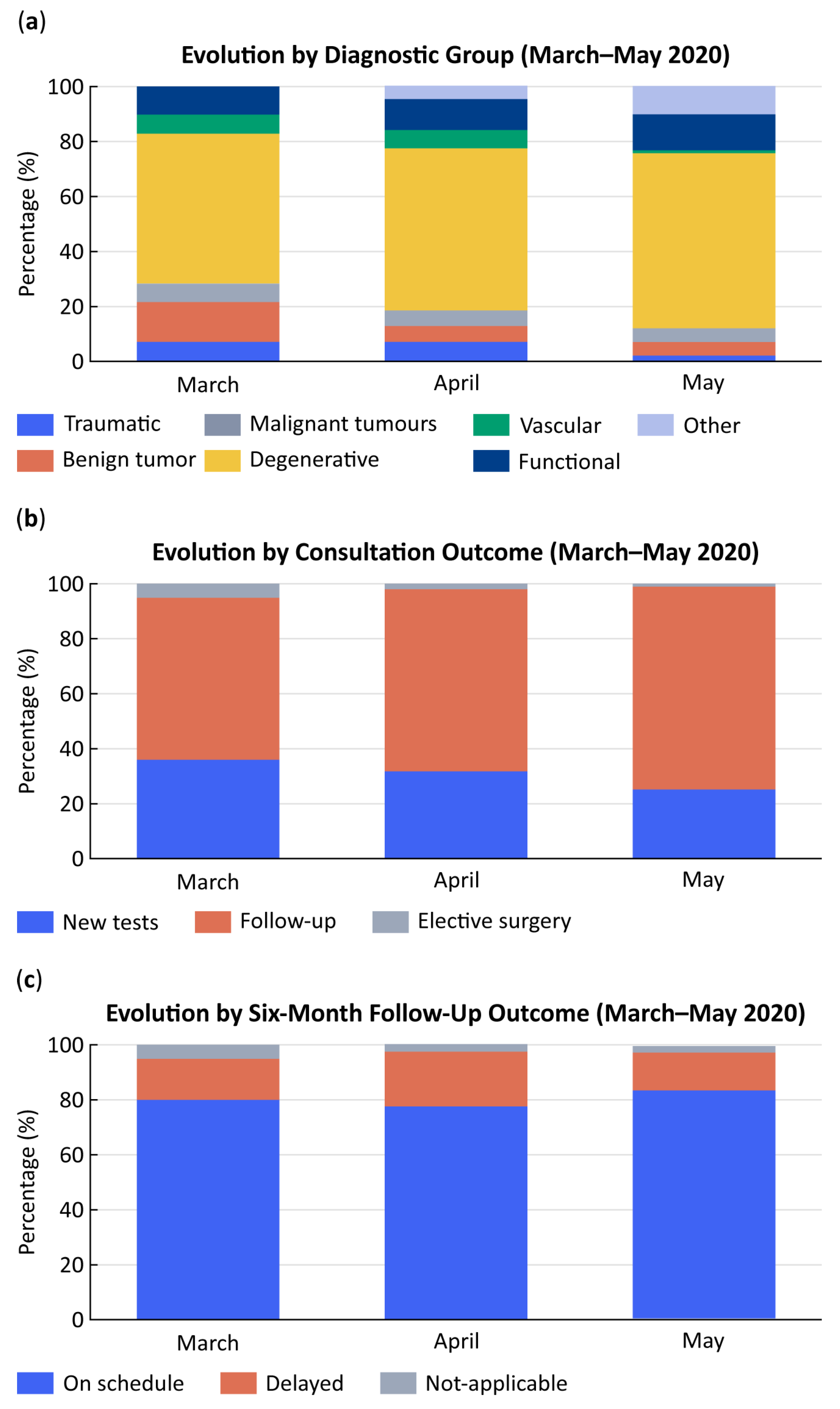
3.4. Distribution by Pathology Type and Disease Category
3.5. Consultation Outcomes
3.6. Six-Month Follow-Up
3.7. Univariate and Multivariate Analysis
4. Discussion
5. Highlights
6. Strengths and Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| aOR | Adjusted odds ratio |
| CI | Confidence interval |
| COVID-19 | Coronavirus disease 2019 |
| COVIDSurg | COVIDSurg Collaborative |
| EU | European Union |
| GDPR | General Data Protection Regulation |
| HGUGM | Hospital General Universitario Gregorio Marañón |
| IQR | Interquartile range |
| N/A | Not Analyzed |
| OR | Odds ratio |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus 2 |
| SD | Standard deviation |
| SERMAS | Servicio Madrileño de Salud (Madrid Regional Health Service) |
| WHO | World Health Organization |
References
- Shereen, M.A.; Khan, S.; Kazmi, A.; Bashir, N.; Siddique, R. COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. J. Adv. Res. 2020, 24, 91–98. [Google Scholar] [CrossRef]
- WHO. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. 2020. Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 21 January 2021).
- Lan, F.Y.; Filler, R.; Mathew, S.; Buley, J.; Iliaki, E.; Bruno-Murtha, L.A.; Osgood, R.; Christophi, C.A.; Fernandez-Montero, A.; Kales, S.N.; et al. COVID-19 symptoms predictive of healthcare workers’ SARS-CoV-2 PCR results. PLoS ONE 2022, 17, e0262341. [Google Scholar] [CrossRef]
- Equipo COVID-19. Informe Sobre la Situación de COVID-19 en España. Red Nacional de Vigilancia Epidemiológica Instituto de Salud Carlos III 2020. Available online: https://cne.isciii.es/documents/d/cne/informe-n-24-situacion-de-covid-19-en-espana-a-21-de-abril-de-2020-pdf (accessed on 5 October 2025).
- Pollán, M.; Pérez-Gómez, B.; Pastor-Barriuso, R.; Oteo, J.; Hernán, M.A.; Pérez-Olmeda, M.; Sanmartín, J.L.; Fernández-García, A.; Cruz, I.; de Larrea, N.F.; et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): A nationwide, population-based seroepidemiological study. Lancet 2020, 396, 535–544. [Google Scholar] [CrossRef]
- Wong, J.; Goh, Q.Y.; Tan, Z.; Lie, S.A.; Tay, Y.C.; Ng, S.Y.; Soh, C.R. Preparing for a COVID-19 pandemic: A review of operating room outbreak response measures. Anesth. Analg. 2020, 130, 1409–1420. [Google Scholar] [CrossRef]
- Kandel, N.; Chungong, S.; Omaar, A.; Xing, J. Health security capacities in the context of COVID-19 outbreak: An analysis of International Health Regulations annual report data from 182 countries. Lancet 2020, 395, 1047–1053. [Google Scholar] [CrossRef] [PubMed]
- Kahn, E.N.; La Marca, F.; Mazzola, C.A. Neurosurgery and Telemedicine in the United States: Assessment of the Risks and Opportunities. World Neurosurg. 2016, 89, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Mandal, S.; Wiesenfeld, B.; Mann, D.M.; Nov, O. Telemedicine: A new normal after COVID-19 pandemic. Am. J. Manag. Care 2025, 31, e74–e78. [Google Scholar] [CrossRef]
- Vogt, H.; Tomic, O.; Haneef, R. Qunatifying the impact of COVID-19 on telemedicine utilization. Interact. J. Med. Res. 2022, 11, e29880. [Google Scholar] [CrossRef]
- Kruse, C.S.; Krowski, N.; Rodriguez, B.; Tran, L.; Vela, J.; Brooks, M. Telehealth and patient satisfaction: A systematic review and narrative analysis. BMJ Open 2017, 7, e016242. [Google Scholar] [CrossRef]
- Scott Kruse, C.; Karem, P.; Shifflett, K.; Vegi, L.; Ravi, K.; Brooks, M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J. Telemed. Telecare 2018, 24, 4–12. [Google Scholar] [CrossRef]
- Vidal-Alaball, J.; Acosta-Roja, R.; Pastor Hernández, N.; Sanchez Luque, U.; Morrison, D.; Narejos Pérez, S.; Perez-Llano, J.; Salvador Vèrges, A.; López Seguí, F. Telemedicine in the face of the COVID-19 pandemic. Aten. Primaria 2020, 52, 418–422. [Google Scholar] [CrossRef]
- Eze, N.D.; Mateus, C.; Cravo Oliveira Hashiguchi, T. Telemedicine in the OECD: An umbrella review of clinical and cost-effectiveness, patient experience and implementation. PLoS ONE 2020, 15, e0237585. [Google Scholar] [CrossRef]
- Car, J.; Koh, G.C.-H.; Foong, P.S.; Wang, C.J. Video consultations in primary and specialist care during the covid-19 pandemic and beyond. BMJ 2020, 371, m3945. [Google Scholar] [CrossRef]
- Ozoner, B.; Gungor, A.; Hasanov, T.; Toktas, Z.; Killic, T. Neurosurgical practice during coronavirus disease 2019 (COVID-19) pandemic. World Neurosurg. 2020, 140, 198–207. [Google Scholar] [CrossRef] [PubMed]
- Arnaout, O.; Patel, A.; Carter, B.; Chiocca, E.A. Adaptation under fire: Two harvard neurosurgical services during the COVID-19 pandemic. Neurosurgery 2020, 87, E173–E177. [Google Scholar] [CrossRef] [PubMed]
- De Biase, G.; Freeman, W.D.; Bydon, M.; Smith, N.; Jerreld, D.; Pascual, J.; Casler, J.; Hasse, C.; Quiñones-Hinojosa, A.; Abode-Iyamah, K. Telemedicine Utilization in Neurosurgery During the COVID-19 Pandemic: A Glimpse Into the Future? Mayo Clin. Proc. Innov. Qual. Outcomes 2020, 4, 736–744. [Google Scholar] [CrossRef] [PubMed]
- Gadjradj, P.S.; Matawlie, R.H.; Harhangi, B.S. Letter to the Editor: The Use of Telemedicine by Neurosurgeons During the Covid Era: Preliminary Results of a Cross-Sectional Research. World Neurosurg. 2020, 139, 746–748. [Google Scholar] [CrossRef]
- Abraham, A.; Jithesh, A.; Doraiswamy, S.; Al-Khawaga, N.; Mamtani, R.; Cheema, S. Telemental Health Use in the COVID-19 Pandemic: A Scoping Review and Evidence Gap Mapping. Front. Psychiatry 2021, 12, 748069. [Google Scholar] [CrossRef]
- Consejería de Sanidad de la Comunidad de Madrid. Datos COVID-19 Comunidad de MAdrid. 13 February 2021. Available online: https://www.comunidad.madrid/sites/default/files/doc/sanidad/210213_cam_covid19.pdf (accessed on 5 October 2025).
- Consejería de Digitalización de la Comunidad de Madrid. Plan Estratégico de Madrid Digital 2022-26. Portal de Transparencia de La Comunidad de Madrid 2022. Available online: https://www.comunidad.madrid/transparencia/informacion-institucional/planes-programas/plan-estrategico-madrid-digital-2022-26 (accessed on 5 October 2025).
- De Saracho Pantoja, I.O.; Jonathan, G.M.; Perjons, E. Rapid response for lasting impact: Examining the digital transformation of Spain’s healthcare system post-COVID-19. Procedia Comput. Sci. 2025, 256, 344–351. [Google Scholar] [CrossRef]
- Cabrerizo-Carreño, H.; Muñoz-Esquerre, M.; Santos Pérez, S.; Romero-Ortiz, A.M.; Fabrellas, N.; Guix-Comellas, E.M. Impact of the implementation of a telemedicine program on patients diagnosed with asthma. BMC Pulm. Med. 2024, 24, 32. [Google Scholar] [CrossRef]
- Piera-Jiménez, J.; Dedeu, T.; Pagliari, C.; Trupec, T. Strengthening primary health care in Europe with digital solutions. Aten. Primaria 2024, 56, 102904. [Google Scholar] [CrossRef]
- Belvís, R.; Santos-Lasaosa, S.; Irimia, P.; Blanco, R.L.; Torres-Ferrús, M.; Morollón, N.; López-Bravo, A.; García-Azorín, D.; Mínguez-Olaondo, A.; Guerrero, Á.; et al. Telemedicine in the management of patients with headache: Current situation and recommendations of the Spanish Society of Neurology’s Headache Study Group. Neurología 2023, 38, 635–646. [Google Scholar] [CrossRef] [PubMed]
- Barrios, V.; Cosín-Sales, J.; Bravo, M.; Escobar, C.; Gámez, J.M.; Huelmos, A.; Ortiz Cortés, C.; Egocheaga, I.; García-Pinilla, J.M.; Jiménez-Candil, J.; et al. Telemedicine consultation for the clinical cardiologists in the era of COVID-19: Present and future. Consensus document of the Spanish Society of Cardiology. Rev. Española Cardiol. 2020, 73, 910–918. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Úbeda, E.F.; Sánchez-Martín, P.; Torrego-Ellacuría, M.; Rey-Mejías, Á.D.; Morales-Contreras, M.F.; Puerta, J.-L. Flexibility and Bed Margins of the Community of Madrid’s Hospitals during the First Wave of the SARS-CoV-2 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 3510. [Google Scholar] [CrossRef] [PubMed]
- Puerta, J.-L.; Torrego-Ellacuría, M.; Del Rey-Mejías, Á.; Bienzobas López, C. Capacity and organisation of Madrid’s community hospitals during first wave of COVID-19 pandemic. J. Healthc. Qual. Res. 2022, 37, 275–282. [Google Scholar] [CrossRef]
- Rodriguez-Gonzalez, C.G.; Chamorro-de-Vega, E.; Valerio, M.; Amor-Garcia, M.A.; Tejerina, F.; Sancho-Gonzalez, M.; Narrillos-Moraza, A.; Gimenez-Manzorro, A.; Manrique-Rodriguez, S.; Machado, M.; et al. COVID-19 in hospitalised patients in Spain: A cohort study in Madrid. Int. J. Antimicrob. Agents 2021, 57, 106249. [Google Scholar] [CrossRef]
- Ramos, R.; de la Villa, S.; García-Ramos, S.; Padilla, B.; García-Olivares, P.; Piñero, P.; Garrido, A.; Hortal, J.; Muñoz, P.; Caamaño, E.; et al. COVID-19 associated infections in the ICU setting: A retrospective analysis in a tertiary-care hospital. Enferm. Infecc. Microbiol. Clin. 2023, 41, 278–283. [Google Scholar] [CrossRef]
- Tsermoulas, G.; Zisalis, A.; Flint, G.; Belli, A. Challenges to Neurosurgery during the COVID-19 pandemic. World Neurosurg. 2020, 139, 519–525. [Google Scholar] [CrossRef]
- Taha, Z.; Alghoul, M.; Anderson, R. Telemedicine and neurosurgery during COVID-19: A global survey of practice patterns. J. Clin. Neurosci. 2021, 88, 8994. [Google Scholar]
- Apostolopoulou, K.; Elmoursi, O.; deLacy, P.; Zaki, H.; McMullan, J.; Ushewokunze, S. The impact of telephone consultations due to COVID-19 on paediatric neurosurgical health services. Child’s Nerv. Syst. 2022, 38, 2133–2139. [Google Scholar] [CrossRef]
- COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans. Br. J. Surg. 2020, 107, 1440–1449. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.A.; Zimering, J.; Gilligan, J.; Rothrock, R.; McNeill, I.; Shrivastava, R.K.; Caridi, J.; Bederson, J.; Hadjipanayis, C.G. Neurosurgical management of brain and spine tumors in the COVID-19 era: An institutional experience from the epicenter of the pandemic. J. Neurooncol. 2020, 148, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Jean, W.C.; Ironside, N.T.; Sack, K.D.; Felbaum, D.R.; Syed, H.R. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: A global neurosurgery study. Acta Neurochir. 2020, 162, 1229–1240. [Google Scholar] [CrossRef]
- Eichberg, D.G.; Basil, G.W.; Di, L.; Shah, A.H.; Luther, E.M.; Lu, V.M.; Perez-Dickens, M.; Komotar, R.J.; Levi, A.D.; Ivan, M.E. Telemedicine in neurosurgery: Lessons learned from a systematic review of the literature for the COVID-19 era and beyond. Neurosurgery 2020, 88, e1–e12. [Google Scholar] [CrossRef]
- COVIDSurg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: An international cohort study. Lancet 2020, 396, 27–38. [Google Scholar] [CrossRef]
- Consejeria de Sanidad de la Comunidad de Madrid. Hospital General Universitario Gregorio Marañon. Memoria de Actividades 2023: Innovación y Transformación Digital. Madrid. 2023. Available online: https://www.comunidad.madrid/sites/default/files/doc/sanidad/memo/memoria23_hgugm_ok.pdf (accessed on 5 October 2025).
- Ministerio de Sanidad. Estrategia de Salud Digital del Sistema Nacional de Salud; Ministerio de Sanidad: Madrid, Spain, 2024. [Google Scholar]
- Servicio Madrileño de Salud. Memoria Anual de Actividad 2023; Servicio Madrileño de Salud: Madrid, Spain, 2024. [Google Scholar]

| Region | Cases |
|---|---|
| Andalusia | 15,819 |
| Aragon | 6766 |
| Asturias | 2690 |
| Madrid | 64,408 |
| Catalonia | 55,196 |
| Castilla-La Mancha | 20,477 |
| Castilla y León | 23,192 |
| Valencian Community | 13,777 |
| Total | 250,273 |
| Variable | Total (n = 5175) | 2019 (n = 3105) | 2020 (n = 2070) | p |
|---|---|---|---|---|
| Age (mean) | 59 | 59 | 58 | p > 0.05 |
| Sex (n, %): Female Male | 2905 (56%) 2270 (44%) | 1738 (56%) 1367 (44%) | 1167 (56%) 903 (44%) | p > 0.05 |
| Month March | 2058 | 1077 | 981 | p > 0.05 |
| Month April | 1607 | 996 | 611 | p < 0.001 |
| Month May | 1510 | 1032 | 478 | p < 0.001 |
| New consultations | 795 | 608 | 187 | p < 0.001 |
| Teleconsultations | 1203 | 0 | 1203 | p < 0.001 |
| Type | March 2019 | April 2019 | May 2019 | March 2020 | April 2020 | May 2020 |
|---|---|---|---|---|---|---|
| New | 222 (21%) | 185 (19%) | 201 (20%) | 136 (14%) | 47 (8%) | 4 (1%) |
| Results | 402 (37%) | 366 (37%) | 384 (37%) | 230 (24%) | 48 (8%) | 42 (9%) |
| Follow-up | 450 (42%) | 445 (45%) | 447 (43%) | 204 (21%) | 62 (10%) | 65 (14%) |
| Teleconsultations | 0 | 0 | 0 | 382 (40%) | 454 (74%) | 367 (77%) |
| Pathology | March | April | May | p |
|---|---|---|---|---|
| Location: | ||||
| Cranial | 58% | 31% | 11% | p < 0.001 |
| Spinal | 56% | 32% | 12% | p < 0.001 |
| Other | 74% | 11% | 14% | p < 0.001 |
| Type: | ||||
| Non-tumoral | 46% | 30% | 25% | p < 0.001 |
| Tumoral | 60% | 28% | 11% | p < 0.001 |
| Variable | By Month p and OR (95% CI) | By Consultation Type p and OR (95% CI) | ||
|---|---|---|---|---|
| Pathology: | ||||
| Tumoral | <0.001 | 0.6 (0.447–0.798) | 0.004 | 0.7 (0.508–0.884) |
| Tumoral benign | <0.001 | 0.5 (0.384–0.760) | 0.014 | 0.7 (0.486–0.923) |
| Tumoral malignant | 0.461 | 0.8 (0.493–1.378) | 0.195 | 0.7 (0.434–1.188) |
| Vascular | <0.001 | 0.3 (0.203–0.599) | 0.314 | 1.3 (0.791–2.075) |
| Degenerative | <0.001 | 0.5 (0.437–0.636) | 0.810 | 1.0 (0.811–1.177) |
| Traumatic | n/a | - | 0.398 | - |
| Request for diagnostic tests | <0.001 | 0.5 (0.414–0.681) | 0.364 | 1.0 (0.878–1.426) |
| Follow-up visits | <0.001 | 0.7 (0.567–0.832) | 0.030 | 1.2 (1.021–1.506) |
| Surgical indications | <0.001 | 0.2 (0.056–0.449) | <0.001 | 0.3 (0.123–0.540) |
| Delayed 6-month follow-up | 0.112 | 0.8 (0.586–1.390) | <0.001 | 2.0 (1.433–2.741) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mateo-Sierra, O.; Romero-Cumbreras, E.; García-Llorente, E.; Rubín-Alduán, S. From Crisis Response to Lasting Transformation: Five-Year Insights from the Implementation of Telemedicine in Neurosurgical Care During COVID-19. Healthcare 2025, 13, 2939. https://doi.org/10.3390/healthcare13222939
Mateo-Sierra O, Romero-Cumbreras E, García-Llorente E, Rubín-Alduán S. From Crisis Response to Lasting Transformation: Five-Year Insights from the Implementation of Telemedicine in Neurosurgical Care During COVID-19. Healthcare. 2025; 13(22):2939. https://doi.org/10.3390/healthcare13222939
Chicago/Turabian StyleMateo-Sierra, Olga, Elena Romero-Cumbreras, Estela García-Llorente, and Sofía Rubín-Alduán. 2025. "From Crisis Response to Lasting Transformation: Five-Year Insights from the Implementation of Telemedicine in Neurosurgical Care During COVID-19" Healthcare 13, no. 22: 2939. https://doi.org/10.3390/healthcare13222939
APA StyleMateo-Sierra, O., Romero-Cumbreras, E., García-Llorente, E., & Rubín-Alduán, S. (2025). From Crisis Response to Lasting Transformation: Five-Year Insights from the Implementation of Telemedicine in Neurosurgical Care During COVID-19. Healthcare, 13(22), 2939. https://doi.org/10.3390/healthcare13222939






