The Spanish Version of the Short Warwick–Edinburgh Mental Well-Being Scale (SWEMWBS): Evidence on Validity, Reliability, and Test of a Processual Model of Physicians’ Well-Being
Abstract
1. Introduction
1.1. Physicians’ Well-Being
1.2. Well-Being Measurement
1.3. Aims of the Study
2. Materials and Methods
2.1. Adaptation Procedure and Study of Content Validity
2.2. Study Design and Setting
2.3. Participants
2.4. Measures
- Short Warwick–Edinburgh Mental Well-being Scale (SWEMWBS) [4]. This scale was derived from the original Spanish translation proposed by López et al. [48]. To obtain a shorter version, the same items selected by the original authors (as described by Stewart-Brown et al. [4]) were used. Accordingly, seven items were selected from the long-form Spanish validated version to create the Spanish Short-Warwick Edinburgh Mental Well-being Scale (SWEMWBS). The SWEMWBS uses a 5-point Likert scale, with response options ranging from ‘Never’ (1) to ‘Always’ (5). For the total score, the mean score of the seven items needs to be calculated. Reliability estimates for this scale are reported in the Results section.
- Depression, Anxiety and Stress Scale (DASS-21) [64]. This scale was originally developed by Lovibond and Lovibond [64] as a shortened version of the 42-item DASS. The first Spanish translation was carried out by Daza et al. [65]. The DASS-21 is structured as a three-factor measure that assesses symptoms of depression, anxiety, and stress experienced during the past week using a 4-point Likert scale with response options ranging from ‘Did not apply to me at all’ (0) to ‘Applied to me very much or most of the time’ (3). Reliability estimates in this sample were 0.82 for depression, 0.78 for anxiety, and 0.87 for stress.
- Short Professional Quality of Life (Short ProQOL) [66]. Translated into Spanish by Galiana et al. [66], the short ProQOL was designed by selecting items from the original ProQOL versions 4 and 5 developed by Stamm [67,68]. This scale consists of three dimensions (compassion satisfaction, compassion fatigue, and burnout), each measured with three Likert-type items rated from (1) ‘never’ to (5) ‘very commonly’. In this sample, reliability estimates were 0.83 for burnout, 0.82 for compassion fatigue, and 0.84 for compassion satisfaction.
- Sussex-Oxford Compassion for others Scale (SOCS-O) [64]. The SOCS–O assesses five dimensions of compassion for others by using 20 items, with four items per dimension: (a) recognizing suffering, (b) understanding the universality of suffering, (c) feeling compassion for the person who is suffering, (d) tolerating uncomfortable feelings, and (e) motivation to act or acting to alleviate suffering [69]. Items are rated on a 5-point Likert-type scale ranging from (1) ‘not at all true’ to (5) ‘always true’. For this study, the Spanish version of the SOCS-O translated by Sansó et al. [70] was used. In this sample, reliability estimates were 0.87 for recognizing suffering, 0.87 for understanding the universality of suffering, 0.80 for feeling compassion for the person who is suffering, 0.72 for tolerating uncomfortable feelings, and 0.76 for motivation to act or acting to alleviate suffering.
2.5. Data Analyses
2.5.1. Participants’ Description
2.5.2. Descriptive Statistics of the Spanish Version of the SWEMWBS
2.5.3. Internal Structure of the Spanish Version of the SWEMWBS
2.5.4. Internal Structure of the Spanish Version of the SWEMWBS
2.5.5. Process-Based Model of Physicians’ Well-Being Using the SWEMWBS
3. Results
3.1. Participants’ Description
3.2. Descriptive Statistics of the Spanish Version of the SWEMWBS
3.3. Internal Structure of the Spanish Version of the SWEMWBS
3.4. Reliability Evidence of the Spanish Version of the SWEMWBS
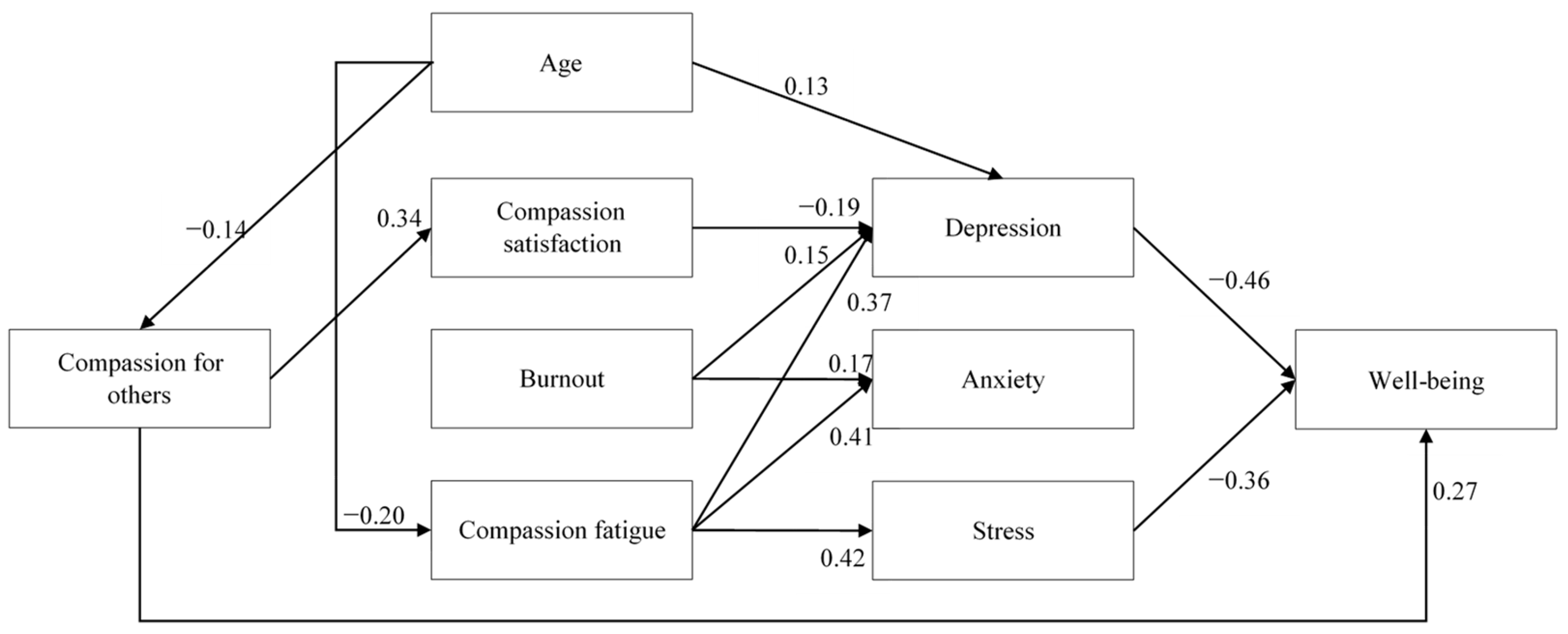
3.5. Process-Based Model of Physicians’ Well-Being Using the SWEMWBS
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| SWEMWBS | Short Warwick–Edinburgh Mental Well-Being Scale |
| WHO | World Health Organization |
| OECD | Organization for Economic Co-operation and Development |
| SWLS | Satisfaction With Life Scale |
| PANAS | Positive Affect and Negative Affect Scale |
| SPANE | Scale of Positive and Negative Experiences |
| RPWB | Ryff’s scales of Psychological Well-Being |
| WHO-5 | WHO Well-being Index |
| WEMWBS | Warwick Edinburgh Mental Well-Being Scale |
| CVR | Content Validity Ratio |
| CVI | Content Validity Index |
| CCTW | Compassion Cultivation Training Workshop |
| MBI | Mindfulness-Based Intervention |
| NI | No-Intervention Group |
| MANOVA | Multivariate Analysis of Variance |
| DASS-21 | Depression, Anxiety, and Stress Scale |
| ProQOL | Professional Quality of Life |
| SOCS-O | Sussex–Oxford Compassion for Others Scale |
| CFI | Comparative Fit Index |
| SRMR | Standardized Root Mean Square Residual |
| RMSEA | Root Mean Square Error of Approximation |
| WLSMV | Weighted Least Squares Mean and Variance-Corrected |
| MLR | Maximum Likelihood with Robust Standard Errors |
| CGCOM | Consejo General de Colegios Oficiales de Médicos |
| CESM | Confederación Estatal de Sindicatos Médicos |
Appendix A. Participants’ Medical Specialization
| Medical Specialization | n | % |
|---|---|---|
| Family and Community Medicine | 75 | 33.6 |
| Pathological Anatomy | 1 | 0.4 |
| Anesthesiology and Resuscitation | 10 | 4.5 |
| Digestive System | 2 | 0.9 |
| Cardiology | 3 | 1.3 |
| General and Digestive Surgery | 1 | 0.4 |
| Orthopedic Surgery and Traumatology | 1 | 0.4 |
| Medical-Surgical Dermatology and Venereology | 7 | 3.1 |
| Endocrinology and Nutrition | 2 | 0.9 |
| Geriatrics | 6 | 2.7 |
| Hematology and Hemotherapy | 4 | 1.8 |
| Medicine, Physical Education, and Sport | 1 | 0.4 |
| Intensive Care Medicine | 7 | 3.1 |
| Internal Medicine | 9 | 4.0 |
| Preventive Medicine and Public Health | 1 | 0.4 |
| Occupational Medicine | 3 | 1.3 |
| Microbiology Parasitology | 1 | 0.4 |
| Nephrology | 4 | 1.8 |
| Pneumology | 1 | 0.4 |
| Clinical Neurophysiology | 1 | 0.4 |
| Neurology | 9 | 4.0 |
| Obstetrics and Gynecology | 15 | 6.7 |
| Medical Oncology | 7 | 3.1 |
| Radiation Oncology | 1 | 0.4 |
| Otorhinolaryngology | 6 | 2.7 |
| Pediatrics | 14 | 6.3 |
| Psychiatry | 13 | 5.8 |
| Radiodiagnostics | 1 | 0.4 |
| Rehabilitation | 2 | 0.9 |
| Rheumatology | 2 | 0.9 |
| No specialty | 5 | 2.2 |
| Other specialty | 4 | 1.8 |
| Missing | 4 | 1.8 |
References
- OECD. Health at a Glance 2023: OECD Indicators; OECD Publishing: Paris, France, 2023. [Google Scholar] [CrossRef]
- WHO. Mental Health; WHO: Geneva, Switzerland, 2022; Available online: https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response (accessed on 13 June 2024).
- Tennant, R.; Hiller, L.; Fishwick, R.; Platt, S.; Joseph, S.; Weich, S.; Parkinson, J.; Secker, J.; Stewart-Brown, S. The Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS): Development and UK validation. Health Qual. Life Outcomes 2007, 5, 63. [Google Scholar] [CrossRef]
- Stewart-Brown, S.; Tennant, A.; Tennant, R.; Platt, S.; Parkinson, J.; Weich, S. Internal construct validity of the Warwick-Edinburgh mental well-being scale (WEMWBS): A Rasch analysis using data from the Scottish health education population survey. Health Qual. Life Outcomes 2009, 7, 15. [Google Scholar] [CrossRef]
- Keyes, C.L. The mental health continuum: From languishing to flourishing in life. J. Health Soc. Behav. 2002, 43, 207–222. [Google Scholar] [CrossRef]
- Keyes, C.L.; Dhingra, S.S.; Simoes, E.J. Change in level of positive mental health as a predictor of future risk of mental illness. Am. J. Public Health 2010, 100, 2366–2371. [Google Scholar] [CrossRef]
- Santini, Z.I.; Ekholm, O.; Koyanagi, A.; Stewart-Brown, S.; Meilstrup, C.; Nielsen, L.; Fusar-Poli, P.; Koushede, V.; Thygesen, L.C. Higher levels of mental wellbeing predict lower risk of common mental disorders in the Danish general population. Ment. Health Prev. 2022, 26, 200233. [Google Scholar] [CrossRef]
- Vaingankar, J.A.; Abdin, E.; Chong, S.A.; Sambasivam, R.; Seow, E.; Jeyagurunathan, A.; Picco, L.; Stewart-Brown, S.; Subramaniam, M. Psychometric properties of the short Warwick Edinburgh mental well-being scale (SWEMWBS) in service users with schizophrenia, depression and anxiety spectrum disorders. Health Qual. Alife Outcomes 2017, 15, 153. [Google Scholar] [CrossRef] [PubMed]
- Campos i Arnal, A.; Galiana, L.; Sánchez-Ruiz, J.; Sansó, N. Cross-Sectional Study of the Professional Quality of Life of Palliative Care Professionals during the COVID-19 Pandemic. Healthcare 2024, 12, 4. [Google Scholar] [CrossRef] [PubMed]
- Galiana, L.; Sansó, N.; Muñoz-Martínez, I.; Vidal-Blanco, G.; Oliver, A.; Larkin, P.J. Palliative care professionals’ inner life: Exploring the mediating role of self-compassion in the prediction of compassion satisfaction, compassion fatigue, burnout and wellbeing. J. Pain Symptom Manag. 2022, 63, 112–123. [Google Scholar] [CrossRef]
- Kratzke, I.M.; Barnhill, J.L.; Putnam, K.T.; Rao, S.; Meyers, M.O.; Meltzer-Brody, S.; Farrell, T.M.; Bluth, K. Self-compassion training to improve well-being for surgical residents. Explore 2023, 19, 78–83. [Google Scholar] [CrossRef]
- Pérez-Belmonte, S.; Galiana, L.; Fernández, I.; Vidal-Blanco, G.; Sansó, N. The Personal Wellbeing Index in Spanish palliative care professionals: A cross-sectional study of wellbeing. Front. Psychol. 2021, 12, 672792. [Google Scholar] [CrossRef]
- Sahebi, A.; Nejati-Zarnaqi, B.; Moayedi, S.; Yousefi, K.; Torres, M.; Golitaleb, M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: An umbrella review of meta-analyses. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 107, 110247. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Gu, M.; Zhang, S.; Gu, J.; Shi, Y.; Yang, Y.; Zhang, L.; Li, M.; Xia, L.; Jiang, F.; et al. Unraveling the interconnectedness between physician burnout and symptoms of depression, anxiety, and stress: A network analysis among Chinese psychiatrists. Front. Public Health 2025, 12, 1493424. [Google Scholar] [CrossRef] [PubMed]
- Malik, H.; Annabi, C.A. The impact of mindfulness practice on physician burnout: A scoping review. Front. Psychol. 2022, 13, 956651. [Google Scholar] [CrossRef] [PubMed]
- Trockel, M.T.; Dyrbye, L.N.; West, C.P.; Sinsky, C.A.; Wang, H.; Carlasare, L.E.; Tutty, M.; Shanafelt, T.D. Impact of Work on Personal Relationships and Physician Well-being. Mayo Clin. Proc. 2024, 99, 1567–1576. [Google Scholar] [CrossRef]
- Patel, R.S.; Bachu, R.; Adikey, A.; Malik, M.; Shah, M. Factors related to physician burnout and its consequences: A review. Behav. Sci. 2018, 8, 98. [Google Scholar] [CrossRef]
- Teoh, K.R.H.; Hassard, J.; Cox, T. Doctors’ working conditions, wellbeing and hospital quality of care: A multilevel analysis. Saf. Sci. 2021, 135, 105115. [Google Scholar] [CrossRef]
- Gogo, A.; Osta, A.; McClafferty, H.; Rana, D.T. Cultivating a way of being and doing: Individual strategies for physician well-being and resilience. Curr. Probl. Pediatr. Adolesc. Health Care 2019, 49, 0663. [Google Scholar] [CrossRef]
- de Wit, K.; Tran, A.; Clayton, N.; Seeburruth, D.; Lim, R.K.; Archambault, P.M.; Chan, T.M.; Rang, L.C.; Gray, S.; Ritchie, K.; et al. Longitudinal Survey on Canadian Emergency Physician Burnout. Ann. Emerg. Med. 2024, 83, 576–584. [Google Scholar] [CrossRef]
- Wetherall, K.; Cleare, S.; McClelland, H.; Melson, A.J.; Niedzwiedz, C.L.; O’Carroll, R.E.; O’COnnor, D.B.; Platt, S.; Scowcroft, E.; Watson, B.; et al. Mental health and well-being during the second wave of COVID-19: Longitudinal analyses of the UK COVID-19 Mental Health and Wellbeing study (UK COVID-MH). BJPsych Open 2022, 8, e103. [Google Scholar] [CrossRef]
- Aiken, L.H.; Sermeus, W.; McKee, M.; Lasater, K.B.; Sloane, D.; Pogue, C.A.; Kohnen, D.; Dello, S.; Maier, C.B.B.; Drennan, J.; et al. Physician and nurse well-being, patient safety and recommendations for interventions: Cross-sectional survey in hospitals in six European countries. BMJ Open 2024, 14, e079931. [Google Scholar] [CrossRef]
- Jachmann, A.; Loser, A.; Mettler, A.; Exadaktylos, A.; Müller, M.; Klingberg, K. Burnout, Depression, and Stress in Emergency Department Nurses and Physicians and the Impact on Private and Work Life: A Systematic Review. JACEP Open 2025, 6, 100046. [Google Scholar] [CrossRef]
- Adhikari, Y.; Senft, B. Distressed but highly satisfied: Professional and personal distress of Nepali doctors. J. Clin. Psychiatry 2022, 13, 41–55. [Google Scholar] [CrossRef]
- Zheng, J.; Feng, S.; Gao, R.; Gong, X.; Ji, X.; Li, Y.; Wang, X.; Xue, B. The relationship between organizational support, professional quality of life, decent work, and professional well-being among nurses: A cross-sectional study. BMC Nurs. 2024, 23, 425–435. [Google Scholar] [CrossRef] [PubMed]
- Chochinov, H.M. Dignity and the essence of medicine: The A, B, C, and D of dignity conserving care. BMJ 2007, 335, 184–187. [Google Scholar] [CrossRef] [PubMed]
- Goetz, J.L.; Keltner, D.; Simon-Thomas, E. Compassion: An evolutionary analysis and empirical review. Psychol. Bull. 2010, 136, 351–374. [Google Scholar] [CrossRef]
- Sprecher, S.; Fehr, B. Compassionate love for close others and humanity. J. Soc. Pers. Relat. 2005, 22, 629–651. [Google Scholar] [CrossRef]
- Klimecki, O.; Singer, T. Empathy from the Perspective of Social Neuroscience. In The Cambridge Handbook of Human Affective Neuroscience; Cambridge University Press: Cambridge, UK, 2013; pp. 533–550. [Google Scholar] [CrossRef]
- Singer, T.; Klimecki, O.M. Empathy and compassion. Curr. Biol. 2014, 24, R875–R878. [Google Scholar] [CrossRef]
- Cosley, B.J.; McCoy, S.K.; Saslow, L.R.; Epel, E.S. Is compassion for others stress buffering? Consequences of compassion and social support for physiological reactivity to stress. J. Exp. Soc. Psychol. 2010, 46, 816–823. [Google Scholar] [CrossRef]
- Kiser, S.B.; Sterns, J.D.; Lai, P.Y.; Horick, N.K.; Palamara, K. Physician coaching by professionally trained peers for Burnout and Well-Being: A Randomized Clinical Trial. JAMA Netw. Open 2024, 7, e245645. [Google Scholar] [CrossRef]
- Alcaraz-Córdoba, A.; Ruiz-Fernandez, M.D.; Ibanez-Masero, O.; Miranda, M.I.V.; Garcia-Navarro, E.B.; Ortega-Galán, Á.M. The efficacy of compassion training programmes for healthcare professionals: A systematic review and meta-analysis. Curr. Psychol. 2024, 43, 18534–18551. [Google Scholar] [CrossRef]
- San Román, M.; De Angelis, M.; Llorens, S.; Salanova, M. A Multilevel Model of Compassion in Healthcare Organizations. Rev. Psicol. Trab. Organ. 2024, 40, 151–163. [Google Scholar] [CrossRef]
- García-Campayo, J.; Barceló-Soler, A.; Martínez-Rubio, D.; Navarrete, J.; Pérez-Aranda, A.; Feliu-Soler, A.; Luciano, J.V.; Baer, R.; Kuyken, W.; Montero-Marin, J. Exploring the relationship between self-compassion and compassion for others: The role of psychological distress and wellbeing. Assessment 2024, 31, 1038–1051. [Google Scholar] [CrossRef] [PubMed]
- VanderWeele, T.J.; Trudel-Fitzgerald, C.; Allin, P.; Farrelly, C.; Fletcher, G.; Frederick, D.E.; Hall, J.; Helliwell, J.F.; Kim, E.S.; Lauinger, W.A.; et al. Current recommendations on the selection of measures for well-being. Prev. Med. 2020, 133, 106004. [Google Scholar] [CrossRef] [PubMed]
- OECD. OECD Guidelines on Measuring Subjective Well-Being; OECD Publishing: Paris, France, 2013. [Google Scholar] [CrossRef]
- Diener, E.; Emmons, R.A.; Larsen, R.J.; Griffin, S. The Satisfaction With Life Scale. J. Pers. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef]
- Watson, D.; Clark, L.A.; Tellegen, A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Pers. Soc. Psychol. 1988, 54, 1063–1070. [Google Scholar] [CrossRef]
- Diener, E.; Wirtz, D.; Tov, W.; Kim-Prieto, C.; Choi, D.W.; Oishi, S.; Biswas-Diener, R. New well-being measures: Short scales to assess flourishing and positive and negative feelings. Soc. Indic. Res. 2010, 97, 143–156. [Google Scholar] [CrossRef]
- Ryff, C.D. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J. Pers. Soc. Psychol. 1989, 57, 1069–1081. [Google Scholar] [CrossRef]
- Bech, P. Clinical Psychometrics; John Wiley & Sons: Chichester, UK, 2012. [Google Scholar]
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef]
- Rose, T.; Joe, S.; Williams, A.; Harris, R.; Betz, G.; Stewart-Brown, S. Measuring mental wellbeing among adolescents: A systematic review of instruments. J. Child Fam. Stud 2017, 26, 2349–2362. [Google Scholar] [CrossRef]
- Orth, Z.; Moosajee, F.; Van Wyk, B. Measuring mental wellness of adolescents: A systematic review of instruments. Front. Psychol. 2022, 13, 835601. [Google Scholar] [CrossRef]
- Kusier, A.O.; Folker, A.P. The Well-Being Index WHO-5: Hedonistic foundation and practical limitations. Med. Humanit. 2020, 46, 333–339. [Google Scholar] [CrossRef]
- Jackson, S.J.; Sam, M.P.; Dawson, M.C.; Porter, D. The wellbeing pandemic: Outline of a contested terrain and a proposed research agenda. Front. Sociol. 2022, 7, 950557. [Google Scholar] [CrossRef]
- López, M.A.; Gabilondo, A.; Codony, M.; García-Forero, C.; Vilagut, G.; Castellví, P.; Ferrer, M.; Alonso, J. Adaptation into Spanish of the Warwick–Edinburgh Mental Well-being Scale (WEMWBS) and preliminary validation in a student sample. Qual. Life Res. 2013, 22, 1099–1104. [Google Scholar] [CrossRef]
- Su, R.; Tay, L.; Diener, E. The development and validation of the Comprehensive Inventory of Thriving (CIT) and the Brief Inventory of Thriving (BIT). Appl. Psychol. Health Well-Being 2014, 6, 251–279. [Google Scholar] [CrossRef] [PubMed]
- Lindert, J.; Bain, P.A.; Kubzansky, L.D.; Stein, C. Well-being measurement and the WHO health policy Health 2010: Systematic review of measurement scales. Eur. J. Public Health 2015, 25, 731–740. [Google Scholar] [CrossRef] [PubMed]
- Perera, B.P.R.; Caldera, A.; Godamunne, P.; Stewart-Brown, S.; Wickremasinghe, A.R.; Jayasuriya, R. Measuring mental well-being in Sri Lanka: Validation of the Warwick Edinburgh Mental Well-being Scale (WEMWBS) in a Sinhala speaking community. BMC Psychiatry 2022, 22, 569. [Google Scholar] [CrossRef] [PubMed]
- Koushede, V.; Lasgaard, M.; Hinrichsen, C.; Meilstrup, C.; Nielsen, L.; Rayce, S.B.; Torres-Sahli, M.; Gudmundsdottir, D.G.; Stewart-Brown, S.; Santini, Z.I. Measuring mental well-being in Denmark: Validation of the original and short version of the Warwick-Edinburgh mental well-being scale (WEMWBS and SWEMWBS) and cross-cultural comparison across four European settings. Psychiatry Res. 2019, 271, 502–509. [Google Scholar] [CrossRef]
- Al-Wattary, N.; Mollazehi, M.; Al-Jubouri, A.M.; Al-Qahtani, N.A.; Jolo, L.K.; Badr, A.A.; Arif, M.; Eltantawi, N.A.; Al-Kuwari, M.S. Validation and psychometric properties of the Arabic version of the Warwick–Edinburgh Mental Well-being Scale (WEMWBS) on a sample of students in Qatar. Ment. Health Sci. 2023, 1, 67–72. [Google Scholar] [CrossRef]
- Fung, S.F. Psychometric evaluation of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS) with Chinese university students. Health Qual. Life Outcomes 2019, 17, 46. [Google Scholar] [CrossRef]
- Mack, D.E.; Vo, K.T.; Wilson, P.M. The Long and Short-Form Warwick-Edinburgh Mental Well-Being Scale: A Reliability Generalization Meta-Analysis. J. Happiness Stud. 2024, 25, 12. [Google Scholar] [CrossRef]
- Crawford, M.J.; Robotham, D.; Thana, L.; Patterson, S.; Weaver, T.; Barber, R.; Wykes, T.; Rose, D. Selecting outcome measures in mental health: The views of service users. J. Ment. Health 2011, 20, 336–346. [Google Scholar] [CrossRef]
- Shah, N.; Cader, M.; Andrews, B.; McCabe, R.; Stewart-Brown, S.L. Short Warwick-Edinburgh Mental Well-being Scale (SWEMWBS): Performance in a clinical sample in relation to PHQ-9 and GAD-7. Health Qual. Life Outcomes 2021, 19, 260. [Google Scholar] [CrossRef] [PubMed]
- Dong, A.; Huang, J.; Lin, S.; Zhu, J.; Zhou, H.; Jin, Q.; Zhao, W.; Zhu, L.; Guo, W. Psychometric properties of the Chinese Warwick-Edinburgh mental well-being scale in medical staff: Cross-sectional study. J. Med. Internet Res. 2022, 24, e38108. [Google Scholar] [CrossRef] [PubMed]
- Waqas, A.; Ahmad, W.; Haddad, M.; Taggart, F.M.; Muhammad, Z.; Bukhari, M.H.; Sami, S.A.; Batool, S.M.; Najeeb, F.; Hanif, A.; et al. Measuring the well-being of health care professionals in the Punjab: A psychometric evaluation of the Warwick–Edinburgh mental well-being scale in a Pakistani population. PeerJ 2015, 3, e1264. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, J.; Boxley, E.; Simons, G. A national cross-sectional survey and interviews exploring the relationship between well-being and burnout in doctors. BJPsych Open 2021, 7, S32–S33. [Google Scholar] [CrossRef]
- Lawshe, C.H. A quantitative approach to content validity. Pers. Psychol. 1975, 28, 563–575. [Google Scholar] [CrossRef]
- Salvado, M.; Marques, D.L.; Pires, I.M.; Silva, N.M. Mindfulness-based interventions to reduce burnout in primary healthcare professionals: A systematic review and meta-analysis. Healthcare 2021, 9, 1342. [Google Scholar] [CrossRef]
- Nam, S.; Toneatto, T. The influence of attrition in evaluating the efficacy and effectiveness of mindfulness-based interventions. Int. J. Ment. Health Addict. 2016, 14, 969–981. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–342. [Google Scholar] [CrossRef]
- Daza, P.; Novy, D.M.; Stanley, M.A.; Averill, P. The Depression Anxiety Stress Scale-21: Spanish translation and validation with a Hispanic sample. J. Psychopathol. Behav. Assess. 2002, 24, 195–205. [Google Scholar] [CrossRef]
- Galiana, L.; Oliver, A.; Arena, F.; De Simone, G.; Tomás, J.M.; Vidal-Blanco, G.; Muñoz-Martínez, I.; Sansó, N. Development and validation of the Short Professional Quality of Life Scale based on versions IV and V of the Professional Quality of Life Scale. Health Qual. Life Outcomes 2020, 18, 364. [Google Scholar] [CrossRef] [PubMed]
- Stamm, B.H. Professional Quality of Life Measure: Compassion, Satisfaction, and Fatigue Version 4 (ProQOL). Available online: https://proqol.org/ (accessed on 20 July 2022).
- Stamm, B.H. Professional Quality of Life Measure: Compassion, Satisfaction, and Fatigue Version 5 (ProQOL). Available online: https://proqol.org/ (accessed on 20 July 2022).
- Gu, J.; Baer, R.; Cavanagh, K.; Kuyken, W.; Strauss, C. Development and psychometric properties of the Sussex-Oxford compassion scales (SOCS). Assessment 2020, 27, 3–20. [Google Scholar] [CrossRef] [PubMed]
- Sansó, N.; Escrivá-Martínez, T.; Flowers, S.; West, M.A.; Galiana, L. The Spanish version of the Sussex-Oxford Compassion for Others Scale (SOCS–O) in nursing students: Psychometric properties and Its relation with mindfulness. Mindfulness 2024, 15, 1778–1792. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practices of Structural Equation Modeling; Guilford Press: New York, NY, USA, 2023. [Google Scholar]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Flora, D.B.; Curran, P.J. An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychol. Methods 2004, 9, 466–491. [Google Scholar] [CrossRef]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research; Guilford Press: New York, NY, USA, 2006. [Google Scholar]
- Muthén, L.; Muthén, B. Mplus, Version 8.4; Muthén & Muthén: Los Angleles, California, USA, 2017. [Google Scholar]
- MacKinnon, D.P.; Fairchild, A.J.; Fritz, M.S. Mediation analysis. Annu. Rev. Psychol. 2007, 58, 593–614. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics for Windows, Version 26.0; IBM Corp: New York, NY, USA, 2019. [Google Scholar]
- Kenny, D.A.; Kaniskan, B.; McCoach, D.B. The performance of RMSEA in models with small degrees of freedom. Sociol. Methods Res. 2015, 44, 486–507. [Google Scholar] [CrossRef]
- Consejo General de Colegios Oficiales de Médicos (CGCOM). Only 23% of the Presidencies of FACME Scientific Societies are Held by Women [Solo el 23% de las Presidencias de las Sociedades Científicas de FACME Están Ocupadas por Mujeres]. Available online: https://www.cgcom.es/noticias/solo-el-23-de-las-presidencias-de-las-sociedades-cientificas-de-facme-estan-ocupadas-por (accessed on 20 July 2024).
- Confederación Estatal de Sindicatos Médicos (CESM). Medical Demographics Study [Estudio sobre Demografía Médica]. Available online: https://www.cgcom.es/sites/main/files/files/2025-10/OMC_Demograf%C3%ADa_M%C3%A9dica_2025.pdf (accessed on 7 June 2025).
- West, C.P.; Dyrbye, L.N.; Rabatin, J.T.; Call, T.G.; Davidson, J.H.; Multari, A.; Romanski, S.A.; Hellyer, J.M.H.; Sloan, J.A.; Shanafelt, T.D. Intervention to promote physician well-being, job satisfaction, and professionalism: A randomized clinical trial. JAMA Intern. Med. 2014, 174, 527–533. [Google Scholar] [CrossRef]
- Capone, V.; Borrelli, R.; Marino, L.; Schettino, G. Mental well-being and job satisfaction of hospital physicians during COVID-19: Relationships with efficacy beliefs, organizational support, and organizational non-technical skills. Int. J. Environ. Res. Public Health 2022, 19, 734. [Google Scholar] [CrossRef]
- Fainstad, T.; Rodriguez, C.; Kreisel, C.; Caragol, J.; Thibodeau, P.S.; Kostiuk, M.; Mann, A. Impact of an Online Group-Coaching Program on Ambulatory Faculty Physician Well-Being: A Randomized Trial. J. Am. Board Fam. Med. 2024, 37, 5. [Google Scholar] [CrossRef]
- Khan, A.; Vinson, A.E. Physician well-being in practice. Anesth. Analg. 2020, 131, 1359–1369. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Sloan, J.A.; Habermann, T.M. The well-being of physicians. Am. J. Med. 2003, 114, 513–519. [Google Scholar] [CrossRef]
- Sansó, N.; Galiana, L.; Oliver, A.; Pascual, A.; Sinclair, S.; Benito, E. Palliative Care Professionals’ Inner Life: Exploring the Relationships Among Awareness, Self-Care, and Compassion Satisfaction and Fatigue, Burnout, and Coping with Death. J. Pain Symptom Manag. 2015, 50, 200–207. [Google Scholar] [CrossRef]
- Ringdal, R.; Bradley Eilersten, M.E.; Bjørnsen, H.N.; Espnes, G.A.; Moksnes, U.K. Validation of two versions of the Warwick-Edinburgh Mental Well-Being Scale among Norwegian adolescents. Scand. J. Public Health 2018, 46, 718–725. Available online: https://www.jstor.org/stable/48615077 (accessed on 12 June 2023). [CrossRef]
- Haver, A.; Akerjordet, K.; Caputi, P.; Furunes, T.; Magee, C. Measuring mental well-being: A validation of the short Warwick–Edinburgh mental well-being scale in Norwegian and Swedish. Scand. J. Public Health 2015, 43, 721–727. [Google Scholar] [CrossRef]
- McKay, M.T.; Andretta, J.R. Evidence for the psychometric validity, internal consistency and measurement invariance of Warwick Edinburgh Mental Well-being Scale scores in Scottish and Irish adolescents. Psychiatry Res. 2017, 255, 382–386. [Google Scholar] [CrossRef] [PubMed]
- Melendez-Torres, G.J.; Hewitt, G.; Hallingberg, B.; Anthony, R.; Collishaw, S.; Hall, J.; Murphy, S.; Moore, G. Measurement invariance properties and external construct validity of the short Warwick-Edinburgh mental wellbeing scale in a large national sample of secondary school students in Wales. Health Qual. Life Outcomes 2019, 17, 139. [Google Scholar] [CrossRef] [PubMed]
- Hooper, C.; Craig, J.; Janvrin, D.R.; Wetsel, M.A.; Reimels, E. Compassion satisfaction, burnout, and compassion fatigue among emergency nurses compared with nurses in other selected inpatient specialties. J. Emerg. Nurs. 2010, 36, 420–427. [Google Scholar] [CrossRef] [PubMed]
- Stamm, B.H. Helping the helpers: Compassion satisfaction and compassion fatigue in self-care, management, and policy. In Resources for Community Suicide Prevention; AKirkwood, D., Stamm, B.H., Eds.; Idaho State University Article: Pocatello, ID, USA, 2012. [Google Scholar]
- Figley, C.R. Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in Those Who Treat the Traumatized; Routledge: Oxfordshire, UK, 2013. [Google Scholar]
- Freudenberger, H.J. Staff Burn-Out. J. Soc. Issues 1974, 30, 159–165. [Google Scholar] [CrossRef]
- Maslach, C.; Leiter, M.P. Burnout. In Stress: Concepts, Cognition, Emotion, and Behavior; Fink, G., Ed.; Elsevier Academic Press: Cambridge, MA, USA, 2016. [Google Scholar]
- Kim, S.J.; Na, H. A study of the relationships between compassion fatigue, compassion satisfaction, depression, anxiety, and sleep disorders among oncology nurses. Asian Oncol. Nurs. 2017, 17, 116–123. [Google Scholar] [CrossRef]
- Hegney, D.G.; Craigie, M.; Hemsworth, D.; Osseiran-Moisson, R.; Aoun, S.; Francis, K.; Drury, V. Compassion satisfaction, compassion fatigue, anxiety, depression and stress in registered nurses in Australia: Study 1 results. J. Nurs. Manag. 2014, 22, 506–518. [Google Scholar] [CrossRef]
- Guthier, C.; Dormann, C.; Voelkle, M.C. Reciprocal effects between job stressors and burnout: A continuous time meta-analysis of longitudinal studies. Psychol. Bull. 2020, 146, 1146–1173. [Google Scholar] [CrossRef]
- Zhou, A.Y.; Panagioti, M.; Esmail, A.; Agius, R.; Van Tongeren, M.; Bower, P. Factors associated with burnout and stress in trainee physicians: A systematic review and meta-analysis. JAMA Netw. Open 2020, 3, e2013761. [Google Scholar] [CrossRef]
- Neff, K.D. The Development and Validation of a Scale to Measure Self-Compassion. Self Identity 2003, 2, 223–250. [Google Scholar] [CrossRef]
- Pommier, E.; Neff, K.D.; Tóth-Király, I. The Development and Validation of the Compassion for Others Scale. J. Pers. Assess. 2020, 102, 573–586. [Google Scholar] [CrossRef]
- MacCallum, R.C.; Austin, J.T. Applications of structural equation modeling in psychological research. Annu. Rev. Psychol 2000, 51, 201–226. [Google Scholar] [CrossRef] [PubMed]
- Khoury, B.; Sharma, M.; Rush, S.E.; Fournier, C. Mindfulness-based stress reduction for healthy individuals: A meta-analysis. J. Psychosom. Res. 2015, 78, 519–528. [Google Scholar] [CrossRef]
- Goldin, P.R.; Jazaieri, H. The Compassion Cultivation Training (CCT) Program. In The Oxford Handbook of Compassion Science; Seppala, E.M., Simon-Thomas, E., Brown, S.L., Worline, M.C., Cameron, C.D., Doty, J.R., Eds.; Oxford University Press: Oxford, UK, 2017; pp. 237–246. [Google Scholar]
- Pace, T.W.; Negi, L.T.; Adame, D.D.; Cole, S.P.; Sivilli, T.I.; Brown, T.D.; Issa, M.J.; Raison, C.L. Effect of compassion meditation on neuroendocrine, innate immune and behavioral responses to psychosocial stress. Psychoneuroendocrinology 2009, 34, 87–98. [Google Scholar] [CrossRef]
- Gilbert, P. The origins and nature of compassion focused therapy. Br. J. Clin. Psychol. 2014, 53, 6–41. [Google Scholar] [CrossRef]

| Variable | Expert 1 | Expert 2 | Expert 3 | Expert 4 | CVR | M | SD | Sk | K | Min | Max | λ | cHI | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Item 1 | 1 | 1 | 1 | 1 | 1.00 | 3.52 | 0.82 | −0.46 | 0.07 | 1.00 | 5.00 | 0.73 | 0.80 | 0.57 |
| Item 2 | 1 | 1 | 1 | 0 | 0.50 | 3.78 | 0.67 | −0.78 | 1.62 | 1.00 | 5.00 | 0.69 | 0.80 | 0.57 |
| Item 3 | 1 | 1 | 1 | 1 | 1.00 | 3.15 | 0.85 | −0.30 | −0.44 | 1.00 | 5.00 | 0.70 | 0.80 | 0.59 |
| Item 4 | 1 | 1 | 1 | 1 | 1.00 | 3.72 | 0.57 | −0.85 | 2.07 | 1.00 | 5.00 | 0.79 | 0.81 | 0.56 |
| Item 5 | 1 | 1 | 1 | 1 | 1.00 | 3.66 | 0.69 | −0.66 | 0.90 | 1.00 | 5.00 | 0.81 | 0.79 | 0.67 |
| Item 6 | 1 | 1 | 1 | 0 | 0.50 | 3.84 | 0.68 | −0.53 | 0.68 | 2.00 | 5.00 | 0.72 | 0.80 | 0.56 |
| Item 7 | 1 | 1 | 1 | 1 | 1.00 | 4.01 | 0.64 | −0.23 | 0.16 | 2.00 | 5.00 | 0.67 | 0.81 | 0.52 |
| Total score | -- | -- | -- | -- | -- | 25.67 | 3.54 | −0.48 | 0.17 | 15.00 | 35.00 | -- | -- | -- |
| Model | df | p | CFI | SRMR | RMSEA | 90%IC | |
|---|---|---|---|---|---|---|---|
| Confirmatory factor analysis | 152.37 | 14 | <0.01 | 0.92 | 0.07 | 0.22 | 0.19, 0.25 |
| Total mediation model | 68.99 | 7 | <0.01 | 0.91 | 0.07 | 0.20 | 0.16, 0.45 |
| Partial mediation model | 49.23 | 6 | <0.01 | 0.94 | 0.05 | 0.18 | 0.14, 0.23 |
| Variables | Compassion Satisfaction | Burnout | Compassion Fatigue |
|---|---|---|---|
| Compassion satisfaction | -- | ||
| Burnout | −0.48 | -- | |
| Compassion fatigue | −0.47 | 0.69 | -- |
| Variables | Depression | Anxiety | Stress |
| Depression | -- | ||
| Anxiety | 0.52 | -- | |
| Stress | 0.42 | 0.62 | -- |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andreu, M.A.; Sánchez-Ruiz, J.; Sansó, N.; Galiana, L. The Spanish Version of the Short Warwick–Edinburgh Mental Well-Being Scale (SWEMWBS): Evidence on Validity, Reliability, and Test of a Processual Model of Physicians’ Well-Being. Healthcare 2025, 13, 2855. https://doi.org/10.3390/healthcare13222855
Andreu MA, Sánchez-Ruiz J, Sansó N, Galiana L. The Spanish Version of the Short Warwick–Edinburgh Mental Well-Being Scale (SWEMWBS): Evidence on Validity, Reliability, and Test of a Processual Model of Physicians’ Well-Being. Healthcare. 2025; 13(22):2855. https://doi.org/10.3390/healthcare13222855
Chicago/Turabian StyleAndreu, Maria A., Javier Sánchez-Ruiz, Noemí Sansó, and Laura Galiana. 2025. "The Spanish Version of the Short Warwick–Edinburgh Mental Well-Being Scale (SWEMWBS): Evidence on Validity, Reliability, and Test of a Processual Model of Physicians’ Well-Being" Healthcare 13, no. 22: 2855. https://doi.org/10.3390/healthcare13222855
APA StyleAndreu, M. A., Sánchez-Ruiz, J., Sansó, N., & Galiana, L. (2025). The Spanish Version of the Short Warwick–Edinburgh Mental Well-Being Scale (SWEMWBS): Evidence on Validity, Reliability, and Test of a Processual Model of Physicians’ Well-Being. Healthcare, 13(22), 2855. https://doi.org/10.3390/healthcare13222855







