Comparative Effectiveness of Origami-Box-Folding and Outside-the-Box Knot-Tying Exercises in Laparoscopic Surgical Training: A Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
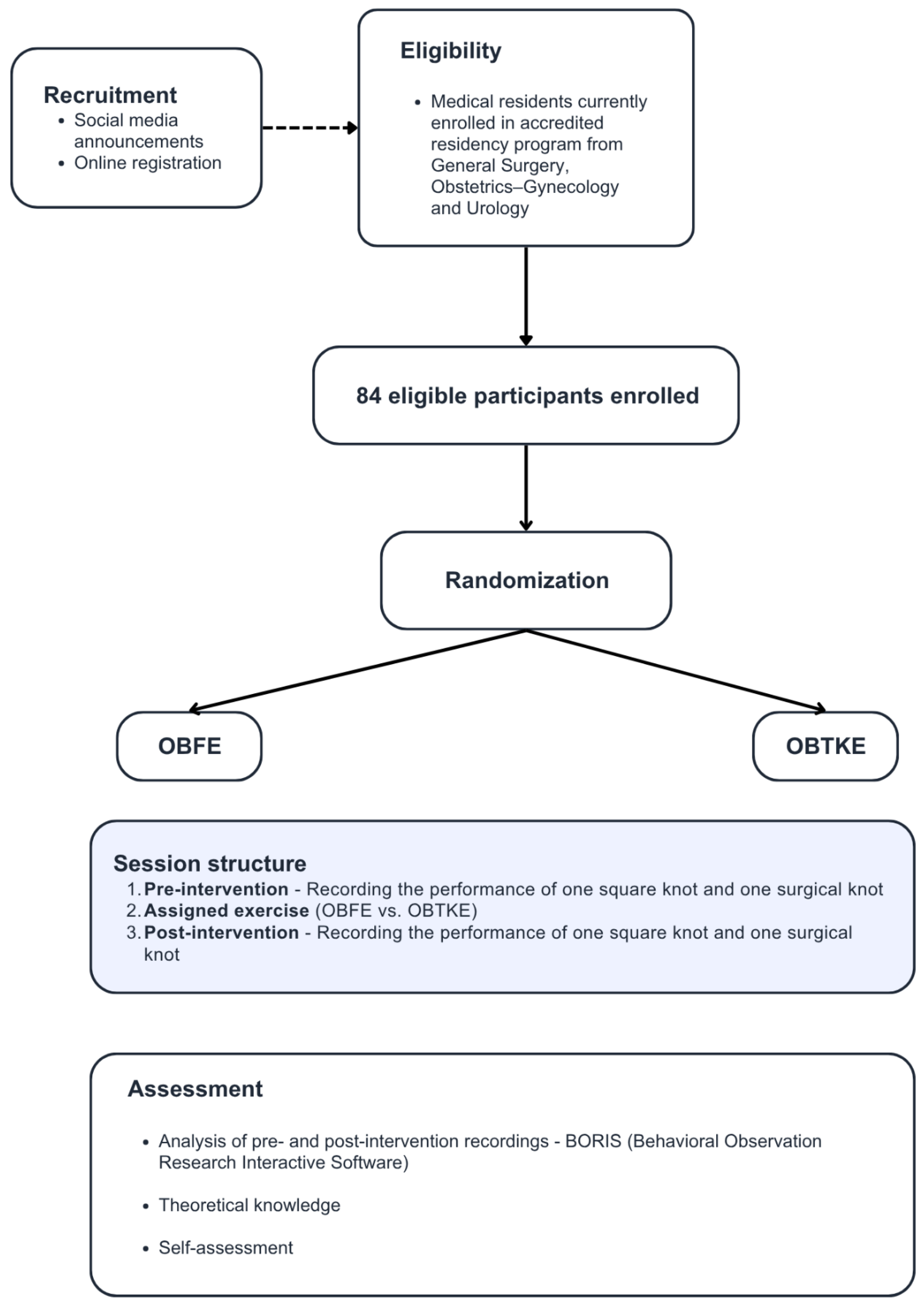
2.1. Study Design and Participants
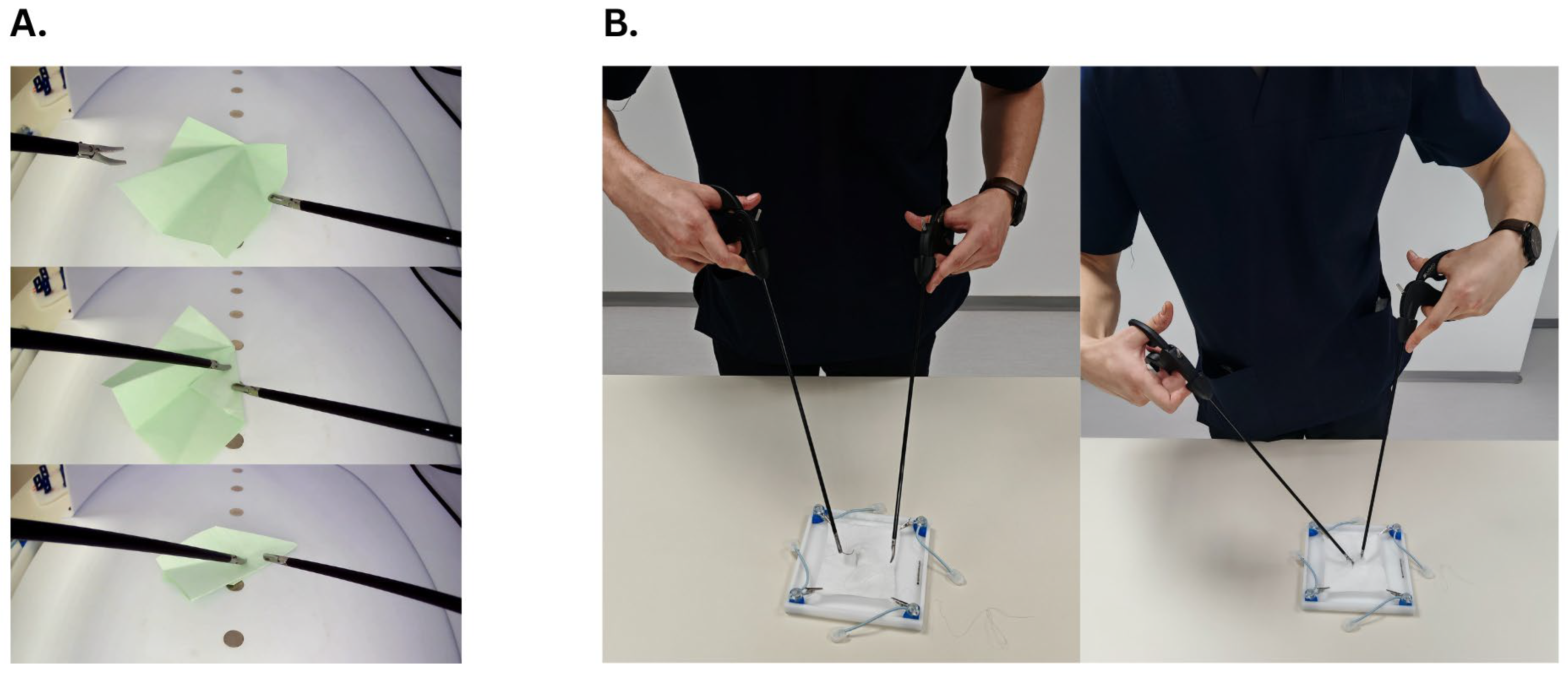
2.2. Training Methodologies
2.3. Assessment Methods
2.4. Statistical Analysis
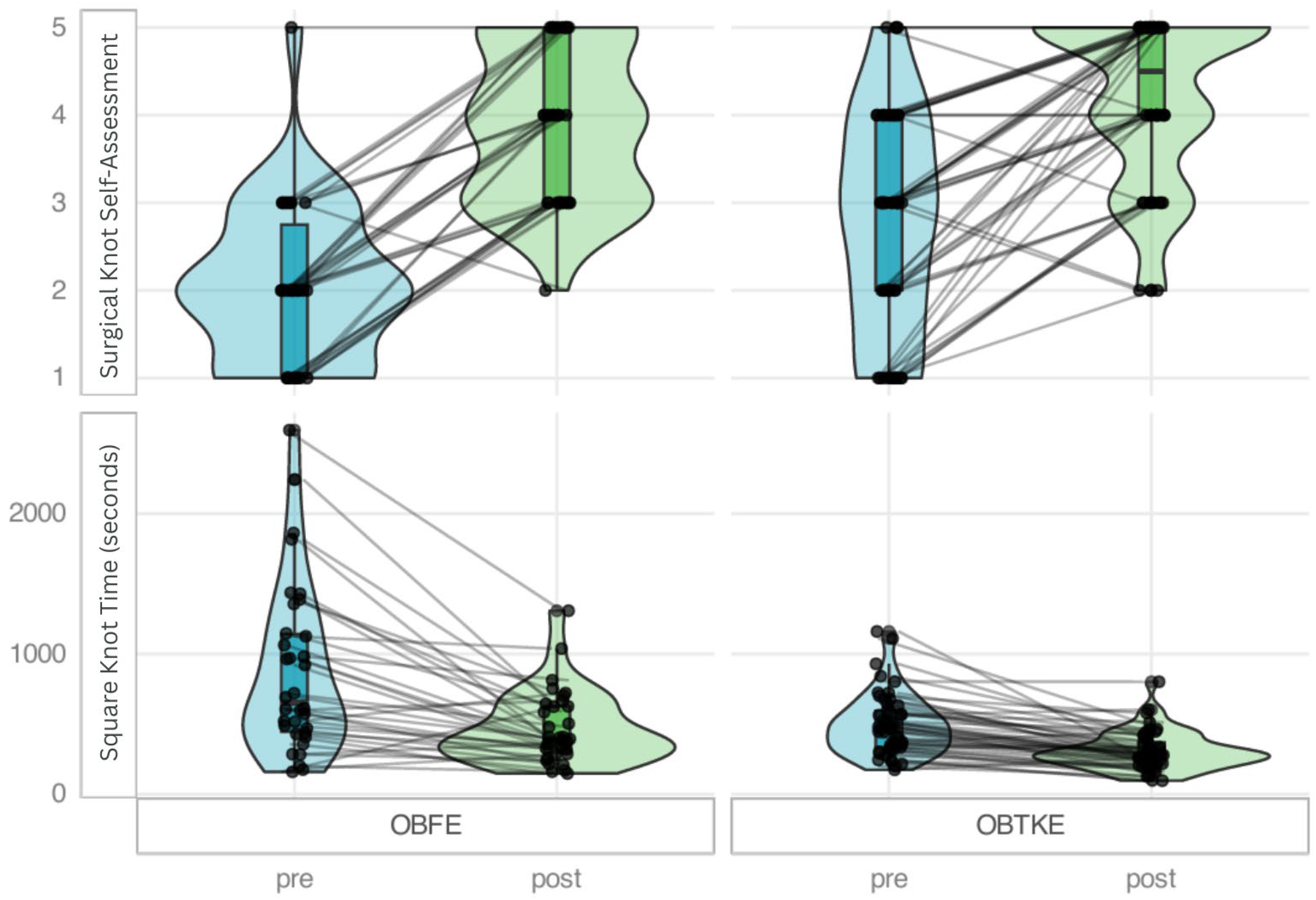
3. Results
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Balafoutas, D.; Joukhadar, R.; Kiesel, M.; Häusler, S.; Loeb, S.; Woeckel, A.; Herr, D. The Role of Deconstructive Teaching in the Training of Laparoscopy. J. Soc. Laparoendosc. Surg. 2019, 23, e2019.00020. [Google Scholar] [CrossRef] [PubMed]
- Armbrust, L.; Lenz, M.; Elrod, J.; Kiwit, A.; Reinshagen, K.; Boettcher, J.; Boettcher, M. Factors Influencing Performance in Laparoscopic Suturing and Knot Tying: A Cohort Study. Eur. J. Pediatr. Surg. Off. J. Austrian Assoc. Pediatr. Surg. Al Z. Kinderchir. 2023, 33, 144–151. [Google Scholar] [CrossRef]
- Noda, Y.; Hamamoto, S.; Shiraki, T.; Sakata, T.; Tomiyama, N.; Naiki, T.; Matsumoto, D.; Okada, T.; Kubota, H.; Yasui, T. Original Training for Laparoscopic Surgery by Making an Origami Paper Crane. Cureus 2024, 16, e62098. [Google Scholar] [CrossRef] [PubMed]
- Gazis, A.; Karaiskos, P.; Loukas, C. Surgical Gesture Recognition in Laparoscopic Tasks Based on the Transformer Network and Self-Supervised Learning. Bioengineering 2022, 9, 737. [Google Scholar] [CrossRef]
- Laski, D.; Stefaniak, T.J.; Makarewicz, W.; Proczko, M.; Gruca, Z.; Sledziński, Z. Structuralized Box-Trainer Laparoscopic Training Significantly Improves Performance in Complex Virtual Reality Laparoscopic Tasks. Wideochirurgia Inne Tech. Maloinwazyjne Videosurgery Miniinvasive Tech. 2012, 7, 27–32. [Google Scholar] [CrossRef]
- Thiyagarajan, M.; Ravindrakumar, C. A Comparative Study in Learning Curves of Two Different Intracorporeal Knot Tying Techniques. Minim. Invasive Surg. 2016, 2016, 3059434. [Google Scholar] [CrossRef]
- Furukawa, S.; Hiraki, M.; Hashimoto, Y.; Noda, Y.; Kanai, H.; Ichikawa, M. Evaluating Laparoscopic Skills: Report on the Origami Crane Folding Competition Using Laparoscopic Instruments with Objective Criteria. Cureus 2024, 16, e72014. [Google Scholar] [CrossRef]
- Hiraki, M.; Kimura, N.; Kitagawa, H.; Kohya, N.; Samejima, R. Laparoscopic Training for Gastrointestinal Surgery Using Japanese Traditional Papercraft Origami. Surg. Laparosc. Endosc. Percutan. Tech. 2022, 32, 401–403. [Google Scholar] [CrossRef]
- Kuo, H.-H.; Yen, C.-F.; Chou, H.-H.; Lin, W.-L.; Huang, K.-G.; Lee, C.-L.; Wang, K.-L.; Hsieh, M.-J. Origami Box Folding Exercise: A Laparoscopic Box Simulation Training and Assessment Method in Facilitating Laparoscopic Psychomotor Skills with Minimal Preparation. Taiwan. J. Obstet. Gynecol. 2023, 62, 31–39. [Google Scholar] [CrossRef]
- Rodrigues, S.P.; Horeman, T.; Blomjous, M.S.H.; Hiemstra, E.; van den Dobbelsteen, J.J.; Jansen, F.W. Laparoscopic Suturing Learning Curve in an Open versus Closed Box Trainer. Surg. Endosc. 2016, 30, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Schwab, B.; Hungness, E.; Barsness, K.A.; McGaghie, W.C. The Role of Simulation in Surgical Education. J. Laparoendosc. Adv. Surg. Tech. A 2017, 27, 450–454. [Google Scholar] [CrossRef]
- Choy, I.; Okrainec, A. Fundamentals of Laparoscopic Surgery-FLS. In The SAGES Manual of Quality, Outcomes and Patient Safety; Tichansky, D.S., Morton, M., Jones, D.B., Eds.; Springer: Boston, MA, USA, 2012; pp. 461–471. ISBN 978-1-4419-7901-8. [Google Scholar]
- Giannotti, D.; Patrizi, G.; Di Rocco, G.; Vestri, A.R.; Semproni, C.P.; Fiengo, L.; Pontone, S.; Palazzini, G.; Redler, A. Play to Become a Surgeon: Impact of Nintendo WII Training on Laparoscopic Skills. PLoS ONE 2013, 8, e57372. [Google Scholar] [CrossRef]
- Middleton, K.K.; Hamilton, T.; Tsai, P.-C.; Middleton, D.B.; Falcone, J.L.; Hamad, G. Improved Nondominant Hand Performance on a Laparoscopic Virtual Reality Simulator after Playing the Nintendo Wii. Surg. Endosc. 2013, 27, 4224–4231. [Google Scholar] [CrossRef]
- Harrington, C.M.; Chaitanya, V.; Dicker, P.; Traynor, O.; Kavanagh, D.O. Playing to Your Skills: A Randomised Controlled Trial Evaluating a Dedicated Video Game for Minimally Invasive Surgery. Surg. Endosc. 2018, 32, 3813–3821. [Google Scholar] [CrossRef]
- Alaker, M.; Wynn, G.R.; Arulampalam, T. Virtual Reality Training in Laparoscopic Surgery: A Systematic Review & Meta-Analysis. Int. J. Surg. 2016, 29, 85–94. [Google Scholar] [CrossRef]
- Selva Raj, D.R.; Kumar, S.; Nallathamby, K.; Raj, K.; Hristova, M. A Systematic Review of the Learning Curves of Novices and Trainees to Achieve Proficiency in Laparoscopic Skills: Virtual Reality Simulator Versus Box Trainer. Cureus 2024, 16, e72923. [Google Scholar] [CrossRef]
- Tee, C.L.; Grieve, D. Development and Validation of an Inexpensive Home-Made Laparoscopic Trainer for Surgical Training. J. Surg. Simul. 2020, 7, 92–97. [Google Scholar] [CrossRef]
- Seltzer, H.; Swayze, E.; Thottathil, L.; Dewey, J.; Jabara, J.; Mehta, A.; Frederick, J.; Yousif, P.; Parikh, S.; Tsuei, A.; et al. The Impact of Homemade Laparoscopic Box Trainers on Medical Student Surgical Skills: A Randomized Control Pilot Study. Surg. Innov. 2023, 30, 84–93. [Google Scholar] [CrossRef] [PubMed]
- Gurusamy, K.S.; Nagendran, M.; Toon, C.D.; Davidson, B.R. Laparoscopic Surgical Box Model Training for Surgical Trainees with Limited Prior Laparoscopic Experience. Cochrane Database Syst. Rev. 2014, 2014, CD010478. [Google Scholar] [CrossRef] [PubMed]
- Nagendran, M.; Gurusamy, K.S.; Aggarwal, R.; Loizidou, M.; Davidson, B.R. Virtual Reality Training for Surgical Trainees in Laparoscopic Surgery. Cochrane Database Syst. Rev. 2013, 2013, CD006575. [Google Scholar] [CrossRef] [PubMed]
- Dawe, S.R.; Pena, G.N.; Windsor, J.A.; Broeders, J.A.J.L.; Cregan, P.C.; Hewett, P.J.; Maddern, G.J. Systematic Review of Skills Transfer after Surgical Simulation-Based Training. Br. J. Surg. 2014, 101, 1063–1076. [Google Scholar] [CrossRef] [PubMed]
- Papanikolaou, I.G.; Haidopoulos, D.; Paschopoulos, M.; Chatzipapas, I.; Loutradis, D.; Vlahos, N.F. Changing the Way We Train Surgeons in the 21th Century: A Narrative Comparative Review Focused on Box Trainers and Virtual Reality Simulators. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 235, 13–18. [Google Scholar] [CrossRef] [PubMed]
| Overall N = 84 | OBFE N = 34 | OBTKE N = 50 | p-Value | q-Value | Test | |
|---|---|---|---|---|---|---|
| Age | 26 (25, 27) | 27 (25, 28) | 26 (25, 27) | 0.12 | 0.20 | W |
| Residency year | 1 (1, 2) | 2 (1, 2) | 1 (1, 2) | 0.19 | 0.23 | W |
| Previous laparoscopic box simulation experience (yes) | 29/84 (35%) | 9/34 (26%) | 20/50 (40%) | 0.20 | 0.23 | chi |
| Laparoscopic surgery experience (yes) | 77/84 (92%) | 29/34 (85%) | 48/50 (96%) | 0.11 | 0.20 | F |
| Camera | 61 (73%) | 28 (82%) | 33 (66%) | |||
| Secondary role | 12 (14%) | 3 (8.8%) | 9 (18%) | |||
| Observatory | 11 (13%) | 3 (8.8%) | 8 (16%) | |||
| Knowledge acquisition (Likert scale) | 5 (4, 5) | 4 (4, 5) | 5 (4, 5) | 0.03 | 0.09 | W |
| Dexterity acquisition (Likert scale) | 5 (4, 5) | 4 (4, 5) | 5 (4, 5) | <0.01 | 0.05 | W |
| General Surgery | Obstetrics and Gynecology | Urology | Total | p-Value | |
|---|---|---|---|---|---|
| Residency year | 0.56 | ||||
| I | 21 | 11 | 12 | 44 | |
| II | 13 | 6 | 7 | 26 | |
| III | 3 | 3 | 0 | 6 | |
| IV | 1 | 2 | 3 | 6 | |
| V | 1 | 1 | 0 | 2 | |
| Total | 39 | 23 | 22 | 84 |
| Post-Pre OBFE | Post-Pre OBTKE | Effect Size OBFE | Effect Size OBTKE | p-Value OBFE | p-Value OBTKE | p-Value Between Modules | |
|---|---|---|---|---|---|---|---|
| Square Knot | |||||||
| Completion time (s) | −278 (−763, 36) | −169 (−332, −23) | 0.74 | 0.82 | 0.01 | <0.01 | 0.02 |
| Instances outside field | 0 (−1, 0) | 0 (−2, 0) | 0.37 | 0.52 | 0.03 | <0.01 | 0.56 |
| Time outside field (s) | 0 (−7.7, 0) | 0 (−3.9, 0) | 0.53 | 0.45 | <0.01 | <0.01 | 0.53 |
| Tissue lesions | −1 (−2, 0) | −1 (−2, 0) | 0.52 | 0.63 | <0.01 | <0.01 | 0.81 |
| Needle drops | 0 (−1, 0) | −1 (−1, 0) | 0.30 | 0.60 | 0.08 | <0.01 | 0.28 |
| Surgical Knot | |||||||
| Completion time (s) | −316 (−775, −1) | −360 (−714, −42) | 0.79 | 0.85 | <0.01 | <0.01 | 0.96 |
| Instances outside field | 0 (−1, 0) | 0 (−2, 0) | 0.26 | 0.47 | 0.14 | <0.01 | 0.30 |
| Time outside field (s) | 0 (−13.68, 0) | 0 (−8.44, 0) | 0.55 | 0.55 | <0.01 | <0.01 | 0.70 |
| Tissue lesions | −1 (−2, 0) | 0 (−1, 0) | 0.62 | 0.48 | 0.01 | <0.01 | 0.32 |
| Needle drops | 0 (−2, 0) | 0 (−1, 0) | 0.54 | 0.49 | <0.01 | <0.01 | 0.66 |
| Theory test score | 1 (0, 2) | 1 (0, 2) | 0.75 | 0.77 | <0.01 | <0.01 | 0.32 |
| Post-Pre OBFE | Post-Pre OBTKE | Effect Size OBFE | Effect Size OBTKE | p-Value OBFE | p-Value OBTKE | p-Value Between Modules | |
|---|---|---|---|---|---|---|---|
| Square Knot | |||||||
| Self-confidence | 2 (1, 3) | 2 (1, 3) | 0.86 | 0.84 | <0.01 | <0.01 | 0.60 |
| Self-rated knot-tying skills | 2 (1, 3) | 2 (1, 3) | 0.87 | 0.85 | <0.01 | <0.01 | 0.25 |
| Self-rated knot-tying knowledge | 2 (1, 3) | 2 (1, 3) | 0.87 | 0.84 | <0.01 | <0.01 | 0.17 |
| Surgical Knot | |||||||
| Self-confidence | 2 (1, 3) | 2 (1, 3) | 0.84 | 0.82 | <0.01 | <0.01 | 0.90 |
| Self-rated knot-tying skills | 2 (1, 2) | 2 (1, 3) | 0.87 | 0.82 | <0.01 | <0.01 | 0.56 |
| Self-rated knot-tying knowledge | 2 (1, 3) | 1 (0, 3) | 0.86 | 0.77 | <0.01 | <0.01 | 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Toma, C.-V.; Georgevici, A.-I.; Barbalata, D.-C.; Popescu, G.-S.; Visan, I.G.; Petrescu, G.E.D.; Nechita, C.O.; Bădescu, D.L.; Tieranu, C.G.; Ciudin, A.; et al. Comparative Effectiveness of Origami-Box-Folding and Outside-the-Box Knot-Tying Exercises in Laparoscopic Surgical Training: A Prospective Cohort Study. Healthcare 2025, 13, 2820. https://doi.org/10.3390/healthcare13212820
Toma C-V, Georgevici A-I, Barbalata D-C, Popescu G-S, Visan IG, Petrescu GED, Nechita CO, Bădescu DL, Tieranu CG, Ciudin A, et al. Comparative Effectiveness of Origami-Box-Folding and Outside-the-Box Knot-Tying Exercises in Laparoscopic Surgical Training: A Prospective Cohort Study. Healthcare. 2025; 13(21):2820. https://doi.org/10.3390/healthcare13212820
Chicago/Turabian StyleToma, Cristian-Valentin, Adrian-Iustin Georgevici, Didina-Catalina Barbalata, George-Sabin Popescu, Ioana Gabriela Visan, George E. D. Petrescu, Cătălin Ovidiu Nechita, Daniel Liviu Bădescu, Cristian George Tieranu, Alexandru Ciudin, and et al. 2025. "Comparative Effectiveness of Origami-Box-Folding and Outside-the-Box Knot-Tying Exercises in Laparoscopic Surgical Training: A Prospective Cohort Study" Healthcare 13, no. 21: 2820. https://doi.org/10.3390/healthcare13212820
APA StyleToma, C.-V., Georgevici, A.-I., Barbalata, D.-C., Popescu, G.-S., Visan, I. G., Petrescu, G. E. D., Nechita, C. O., Bădescu, D. L., Tieranu, C. G., Ciudin, A., & Jinga, V. (2025). Comparative Effectiveness of Origami-Box-Folding and Outside-the-Box Knot-Tying Exercises in Laparoscopic Surgical Training: A Prospective Cohort Study. Healthcare, 13(21), 2820. https://doi.org/10.3390/healthcare13212820










