A Systematic Review of Smartphone Applications That Address Patient Care in the Peri-Operative Period
Abstract
1. Introduction
Aims and Objectives
- To describe the current attempts in smartphone apps to aid in the peri-operative care of patients by identifying and classifying published information in the literature on their benefits and perceived outcomes.
- To identify and summarize effective smartphone app features, assess the usability and effectiveness of the apps to help guide future studies, identify the limitations of the studies included in the project, identify gaps in the literature, and identify areas of interest for further clinical studies.
2. Methodology
2.1. Research Question
2.2. Search Strategy
2.3. Inclusion Criteria
- Full text.
- English language.
- Primary research.
- Used by patients who underwent any type of surgery.
- Interventions aiming to improve post-operative care.
- Interventions using mHealth.
- Patient care-oriented.
- Focused on the design, development, evaluation, or use of a smartphone-based app.
- Discussed phone apps that had the ability to function independently without the need for medical device.
- Discussed the features and utility of the app.
2.4. Exclusion Criteria
- Did not meet the inclusion criteria listed above.
- Studies not in English.
- Unavailable full-text articles.
- Studies that were research protocols, conference presentations, reviews, editorials, case reports, and case series.
- Smartphone technology used for health intervention as opposed to patient care were excluded.
- Smartphone apps whose target audience were surgical care providers as opposed to patients.
- Did not discuss the features and utility of the app.
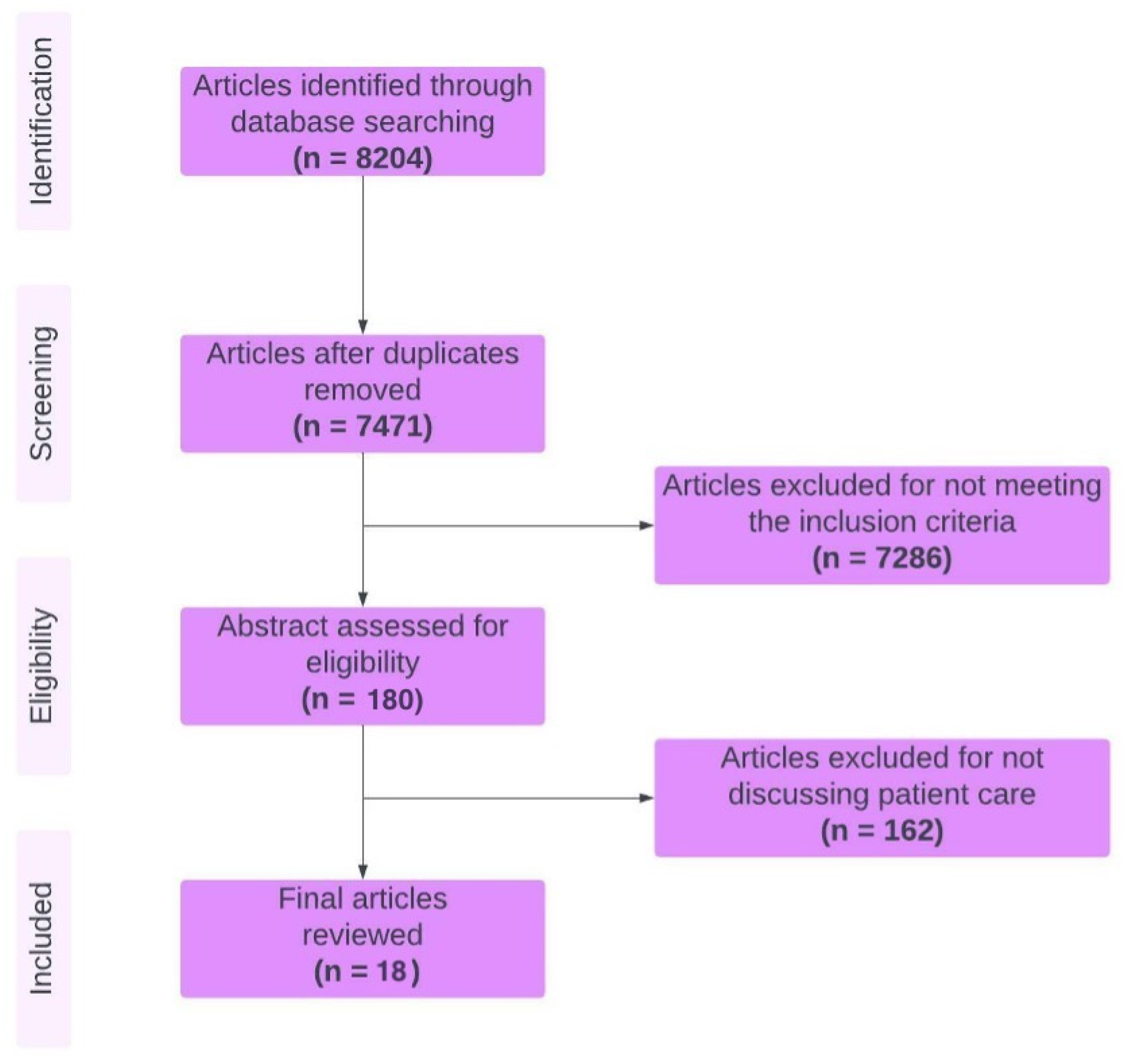
2.5. Study Screening, Selection, Analysis, and Quality Appraisal
2.6. Ethics Approval
3. Main Report—Results
3.1. Search Results
3.2. General Description of the Included Studies
3.3. Thematic Synthesis
4. Discussion
4.1. Patient Education and Instruction
4.2. Clear Communication
4.3. Decreasing Complications and Use of Healthcare Resources
4.4. Post-Operative Monitoring and Pain Control
4.5. Improved Patient Support, Satisfaction, and Safety
4.6. Requirements of an Effective Smartphone Application
4.7. What to Include in Smartphone Application Assessments
4.8. Limitations of Smartphone Application Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Morte, K.; Marenco, C.; Lammers, D.; Bingham, J.; Sohn, V.; Eckert, M. Utilization of mobile application improves perioperative education and patient satisfaction in general surgery patients. Am. J. Surg. 2021, 221, 788–792. [Google Scholar] [CrossRef] [PubMed]
- Mezei, G.; Chung, F. Return hospital visits and hospital readmissions after ambulatory surgery. Ann. Surg. 1999, 230, 721–727. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bruce, J.; Russell, E.M.; Mollison, J.; Krukowski, Z.H. The measurement and monitoring of surgical adverse events. Heal. Technol. Assess. 2001, 5, 1–194. [Google Scholar] [CrossRef] [PubMed]
- Smith, H.K.; Manjaly, J.G.; Yousri, T.; Upadhyay, N.; Taylor, H.; Nicol, S.G.; Livingstone, J.A. InforMed. consent in trauma: Does written information improve patient recall of risks? A prospective randomised study. Injury 2012, 43, 1534–1538. [Google Scholar] [CrossRef] [PubMed]
- Uzzaman, M.M.; Sinha, S.; Shaygi, B.; Vitish-Sharma, P.; Loizides, S.; Myint, F. Evaluation of patient’s understanding and recall of the consent process after open inguinal hernia repairs. Int. J. Surg. 2012, 10, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Semple, J.L.; Armstrong, K.A. Mobile applications for postoperative monitoring after discharge. Can. Med. Assoc. J. 2017, 189, E22–E24. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pan, S.; Rong, L.Q. Mobile Applications in Clinical and Perioperative Care for Anesthesia: Narrative Review. J. Med. Internet Res. 2021, 23, e25115. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mosa, A.S.M.; Yoo, I.; Sheets, L. A Systematic Review of Healthcare Applications for Smartphones. BMC Med. Inform. Decis. Mak. 2012, 12, 67. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Willems, S.J.; Coppieters, M.W.; Pronk, Y.; Diks, M.J.F.; van der Heijden, K.W.A.P.; Rooker, S.; Scholten-Peeters, G.G.M. A Clinical Journey Mobile Health App for Perioperative Patients: Cross-sectional Study. JMIR Hum. Factors 2021, 8, e20694. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Elbert, N.J.; van Os-Med.endorp, H.; van Renselaar, W.; Ekeland, A.G.; Hakkaart-van Roijen, L.; Raat, H.; Nijsten, T.E.; Pasmans, S.G. Effectiveness and cost-effectiveness of ehealth interventions in somatic diseases: A systematic review of systematic reviews and meta-analyses. J. Med. Internet Res. 2014, 16, e110. [Google Scholar] [CrossRef]
- Wantland, D.J.; Portillo, C.J.; Holzemer, W.L.; Slaughter, R.; McGhee, E.M. The effectiveness of web-based vs. non-web-based interventions: A meta-analysis of behavioral change outcomes. J. Med. Internet Res. 2004, 6, e40. [Google Scholar] [CrossRef]
- Walker, C.; Swerissen, H.; Belfrage, J. Self-management: Its place in the management of chronic illnesses. Aust. Health Rev. 2003, 26, 34–42. [Google Scholar] [CrossRef]
- Brooke, J.; Jordan, P.W.; Thomas, B.; Weerdmeester, B.A.; McClelland, I.L. Usability Evaluation in Industry; CRC Press: Boca Raton, FL, USA, 1996. [Google Scholar]
- Stauber, A.; Schüßler, N.; Palmdorf, S.; Schürholz, N.; Bruns, D.; Osterbrink, J.; Nestler, N. RECOVER-E—a mobile app for patients undergoing total knee or hip replacement: Study protocol. BMC Musculoskelet. Disord. 2020, 21, 71. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Martínez-Ramos, C.; Cerdán, M.T.; López, R.S. Mobile phone–based teleMed.icine system for the home follow-up of patients undergoing ambulatory surgery. TeleMed. J. e-Health 2009, 15, 531–537. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Available online: http://www.epidem.com/ (accessed on 6 July 2022).
- Jocelyn, C. How to peer review a qualitative manuscript. In Peer Review in Health Sciences, 2nd ed.; BMJ: London, UK, 2003; pp. 219–235. Available online: https://bmjopen.bmj.com/content/suppl/2012/01/12/bmjopen-2011-000138.DC1/BMJ_Open_IMG_Physician_Migration_RATS_Checklist.pdf (accessed on 6 July 2022).
- Ke, J.X.C.; George, R.B.; Wozney, L.; Munro, A. Perioperative mobile application for mothers undergoing Cesarean delivery: A prospective cohort study on patient engagement. Can. J. Anaesth. 2021, 68, 505–513. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- A Anthony, C.; Rojas, E.O.; Keffala, V.; Glass, N.A.; Shah, A.S.; Miller, B.J.; Hogue, M.; Willey, M.C.; Karam, M.; Marsh, J.L. Acceptance and Commitment Therapy Delivered via a Mobile Phone Messaging Robot to Decrease Postoperative Opioid Use in Patients With Orthopedic Trauma: Randomized Controlled Trial. J. Med. Internet Res. 2020, 22, e17750. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Premkumar, A.; Lovecchio, F.C.; Stepan, J.G.; Kahlenberg, C.A.; Blevins, J.L.; Albert, T.J.; Cross, M.B. A Novel Mobile Phone Text Messaging Platform Improves Collection of Patient-Reported Post-operative Pain and Opioid Use Following Orthopedic Surgery. HSS J. 2019, 15, 37–41. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rojas, E.O.; Anthony, C.A.; Kain, J.; Glass, N.; Shah, A.S.; Smith, T.; Miller, B.J. Automated Mobile Phone Messaging Utilizing a Cognitive Behavioral Intervention: A Pilot Investigation. Iowa Orthop. J. 2019, 39, 85–91. [Google Scholar] [PubMed] [PubMed Central]
- Goz, V.; Anthony, C.; Pugely, A.; Lawrence, B.; Spina, N.; Brodke, D.; Spiker, W.R. Software-Based Postoperative Communication With Patients Undergoing Spine Surgery. Glob. Spine J. 2019, 9, 14–17. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wittig-Wells, D.; Higgins, M.; Carter, J.; Davis, E.; Holmes, E.; Jacob, A.; Samms-McPherson, J.; Simms, S. Impact of a Preset Daily Cell Phone Alarm on Med.ication Adherence for Aspirin as Antithrombotic Therapy. Orthop. Nurs. 2019, 38, 311–316. [Google Scholar] [CrossRef] [PubMed]
- van Dijk-Huisman, H.C.; Weemaes, A.T.; Boymans, T.A.; Lenssen, A.F.; de Bie, R.A. Smartphone App with an Accelerometer Enhances Patients’ Physical Activity Following Elective Orthopedic Surgery: A Pilot Study. Sensors 2020, 20, 4317. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Belarmino, A.; Walsh, R.; Alshak, M.; Patel, N.; Wu, R.; Hu, J.C. Feasibility of a Mobile Health Application To Monitor Recovery and Patient-reported Outcomes after Robot-assisted Radical Prostatectomy. Eur. Urol. Oncol. 2019, 2, 425–428. [Google Scholar] [CrossRef] [PubMed]
- Felbaum, D.R.; Stewart, J.J.; Anaizi, A.N.; A Sandhu, F.; Nair, M.N.; Voyadzis, J.-M. Implementation and Evaluation of a Smartphone Application for the Perioperative Care of Neurosurgery Patients at an Academic Med.ical Center: Implications for Patient Satisfaction, Surgery Cancelations, and Readmissions. Neurosurgery 2018, 14, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Heuser, J.; Maeda, A.; Yang, L.; Masino, C.; Duggal, S.; Jackson, T.; Okrainec, A. Impact of a Mobile App to Support Home Recovery of Patients Undergoing Bariatric Surgery. J. Surg. Res. 2021, 261, 179–184. [Google Scholar] [CrossRef] [PubMed]
- van Hout, L.; Bökkerink, W.J.V.; Vriens, P.W.H.E. Clinical feasibility of the Q1.6 Inguinal Hernia application: A prospective cohort study. Hernia 2023, 27, 449–458. [Google Scholar] [CrossRef]
- Sousa, C.S.; Turrini, R.N.T. Development of an educational mobile application for patients submitted to orthognathic surgery. Rev. Lat. Am. Enferm. 2019, 27, e3143. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ashraf, H.; Anderson, R.G.; Anderson, D.J.; Moug, S.J. Feasibility of a perioperative smartphone application in colorectal surgery. Br. J. Surg. 2021, 108, e282–e283. [Google Scholar] [CrossRef] [PubMed]
- Abdeen, A.; Monárrez, R.; Drew, J.M.; Kennedy, K.F. Use of a Smart-Phone Mobile Application is Associated With Improved Compliance and Reduced Length of Stay in Patients Undergoing Primary Total Joint Arthroplasty of the Hip and Knee. J. Arthroplast. 2022, 37, 1534–1540. [Google Scholar] [CrossRef] [PubMed]
- van der Meij, E.; Anema, J.R.; Leclercq, W.K.G.; Bongers, M.Y.; Consten, E.C.J.; Schraffordt, K.S.E.; van de Ven, P.M.; Terwee, C.B.; van Dongen, J.M.; Schaafsma, F.G.; et al. Personalised perioperative care by e-health after interMed.iate-grade abdominal surgery: A multicentre, single-blind, randomised, placebo-controlled trial. Lancet 2018, 392, 51–59. [Google Scholar] [CrossRef]
- Pickens, R.; Cochran, A.; Tezber, K.; Berry, R.; Bhattacharya, E.; Koo, D.; King, L.; Iannitti, D.A.; Martinie, J.B.; Baker, E.H.; et al. Using a Mobile Application for Real-Time Collection of Patient-Reported Outcomes in Hepatopancreatobiliary Surgery within an ERAS® Pathway. Am. Surg. 2019, 85, 909–917. [Google Scholar] [CrossRef] [PubMed]
- Fredericks, S.; Yau, T. Educational intervention reduces complications and rehospitalizations after heart surgery. West. J. Nurs. Res. 2013, 35, 1251–1265. [Google Scholar] [CrossRef] [PubMed]
- Aiello, F.A.; Gross, E.R.; Krajewski, A.; Fuller, R.; Morgan, A.; Duffy, A.; Longo, W.; Kozol, R.; Chandawarkar, R. Post-appendectomy visits to the emergency department within the global period: A target for cost containment. Am. J. Surg. 2010, 200, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Clark, N.M.; Feldman, C.H.; Evans, D.; Levison, M.J.; Wasilewski, Y.; Mellins, R.B. The impact of health education on frequency and cost of health care use by low income children with asthma. J. Allergy Clin. Immunol. 1986, 78, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Karam, J.A.; Sundre, S.M.; Smith, G.L. Cost/benefit analysis of patient education. J. Health Educ. Teach. 1986, 1, 15–19. [Google Scholar] [PubMed]
- McDonald, D.; Siegmeth, R.; Deakin, A.; Kinninmonth, A.; Scott, N. An enhanced recovery programme for primary total knee arthroplasty in the United Kingdom—follow up at one year. Knee 2012, 19, 525–529. [Google Scholar] [CrossRef]
- Vo, V.; Auroy, L.; Sarradon-Eck, A. Patients’ perceptions of mhealth apps: Meta-ethnographic review of qualitative studies. JMIR mHealth uHealth 2019, 7, e13817. [Google Scholar] [CrossRef]
- Bauer, A.M.; Iles-Shih, M.; Ghomi, R.H.; Rue, T.; Grover, T.; Kincler, N.; Miller, M.; Katon, W.J. Acceptability of mHealth augmentation of collaborative care: A mixed methods pilot study. Gen. Hosp. Psychiatry 2018, 51, 22–29. [Google Scholar] [CrossRef]
- Siggeirsdottir, K.; Olafsson, O.; Jonsson, H.; Iwarsson, S.; Gudnason, V.; Jonsson, B.Y. Short hospital stay augmented with education and home-based rehabilitation improves function and quality of life after hip replacement: Randomized study of 50 patients with 6 months of follow-up. Acta Orthop. 2005, 76, 555–562. [Google Scholar] [CrossRef]
- Sandberg, E.H.; Sharma, R.; Sandberg, W.S. Deficits in retention for verbally presented Med.ical information. Anesthesiology 2012, 117, 772–779. [Google Scholar] [CrossRef]
- Timmers, T.; Janssen, L.; Pronk, Y.; van der Zwaard, B.C.; Koëter, S.; van Oostveen, D.; de Boer, S.; Kremers, K.; Rutten, S.; Das, D.; et al. Assessing the efficacy of an educational smartphone or tablet app with subdivided and interactive content to increase patients’ Med.ical knowledge: Randomized controlled trial. JMIR Mhealth Uhealth 2018, 6, e10742. [Google Scholar] [CrossRef]
- Khaleel, I.; Wimmer, B.C.; Peterson, G.M.; Zaidi, S.T.R.; Roehrer, E.; Cummings, E.; Lee, K. Health information overload among health consumers: A scoping review. Patient Educ. Couns. 2020, 103, 15–32. [Google Scholar] [CrossRef]
- Houts, P.S.; Doak, C.C.; Doak, L.G.; Loscalzo, M.J. The role of pictures in improving health communication: A review of research on attention, comprehension, recall, and adherence. Patient Educ. Couns. 2006, 61, 173–190. [Google Scholar] [CrossRef]
- Bol, N.; Smets, E.M.; Rutgers, M.M.; Burgers, J.A.; de Haes, H.C.; Loos, E.F.; van Weert, J.C. Do videos improve website satisfaction and recall of online cancer-related information in older lung cancer patients? Patient Educ. Couns. 2013, 92, 404–412. [Google Scholar] [CrossRef]
- De La Cruz Monroy, M.F.I.; Mosahebi, A. The use of smartphone applications (apps) for enhancing communication with surgical patients: A systematic review of the literature. Surg. Innov. 2019, 26, 244–259. [Google Scholar] [CrossRef]
- Simpao, A.F.; Lingappan, A.M.; Ahumada, L.M.; Rehman, M.A.; Gálvez, J.A. Perioperative smartphone apps and devices for patient-centered care. J. Med. Syst. 2015, 39, 102. [Google Scholar] [CrossRef]
- Nguyen, N.; Leveille, E.; Guadagno, E.; Kalisya, L.M.; Poenaru, D. Use of mobile health technologies for postoperative care in paediatric surgery: A systematic review. J. TeleMed. Telecare 2022, 28, 331–341. [Google Scholar] [CrossRef]
- Castillo, E.; McIsaac, C.; MacDougall, B.; Wilson, D.; Kohr, R. Post-caesarean section surgical site infection surveillance using an online database and mobile phone technology. J. Obstet. Gynaecol. Can. 2017, 39, 645–651.e1. [Google Scholar] [CrossRef]
- Fawsitt, C.G.; Meaney, S.; Greene, R.A.; Corcoran, P. Surgical site infection after caesarean section? There is an app for that: Results from a feasibility study on costs and benefits. Ir. Med. J. 2017, 110, 635. [Google Scholar]
- DeNicola, N.M.; Grossman, D.; Marko, K.; Sonalkar, S.; Tobah, Y.S.B.; Ganju, N.; Witkop, C.T.; Henderson, J.T.; Butler, J.L.; Lowery, C. Telehealth interventions to improve obstetric and gynecologic health outcomes: A systematic review. Obstet. Gynecol. 2020, 135, 371–382. [Google Scholar] [CrossRef]
- Bush, J.; Barlow, D.E.; Echols, J.; Wilkerson, J.; Bellevin, K. Impact of a mobile health application on user engagement and pregnancy outcomes among wyoming Med.icaid members. TeleMed. J. e-Health 2017, 23, 891–898. [Google Scholar] [CrossRef]
- Mackillop, L.; Hirst, J.E.; Bartlett, K.J.; Birks, J.S.; Clifton, L.; Farmer, A.J.; Gibson, O.; Kenworthy, Y.; Levy, J.C.; Loerup, L.; et al. Comparing the efficacy of a mobile phone-based blood glucose management system with standard clinic care in women with gestational diabetes: Randomized controlled trial. JMIR mHealth uHealth 2018, 6, e71. [Google Scholar] [CrossRef]
- Miremberg, H.; Ben-Ari, T.; Betzer, T.; Raphaeli, H.; Gasnier, R.; Barda, G.; Bar, J.; Weiner, E. The impact of a daily smartphone-based feedback system among women with gestational diabetes on compliance, glycemic control, satisfaction, and pregnancy outcome: A randomized controlled trial. Am. J. Obstet. Gynecol. 2018, 218, 453.e1–453.e7. [Google Scholar] [CrossRef]
- Sung, J.-H.; Lee, D.Y.; Min, K.P.; Park, C.-Y. Peripartum management of gestational diabetes using a digital health care service: A pilot, randomized controlled study. Clin. Ther. 2019, 41, 2426–2434. [Google Scholar] [CrossRef]
- Dahlberg, K.; Jaensson, M.; Nilsson, U. “Let the patient decide”—Person-centered postoperative follow-up contacts, initiated via a phone app after day surgery: Secondary analysis of a randomized controlled trial. Int. J. Surg. 2019, 61, 33–37. [Google Scholar] [CrossRef]
- Pastora-Bernal, J.M.; Martín-Valero, R.; Barón-López, F.J.; Estebanez-Pérez, M.J. Evidence of benefit of telerehabitation after orthopedic surgery: A systematic review. J. Med. Internet Res. 2017, 19, e142. [Google Scholar] [CrossRef]
- Birch, S.; Stilling, M.; Mechlenburg, I.; Hansen, T.B. Effectiveness of a physiotherapist delivered cognitive-behavioral patient education for patients who undergoes operation for total knee arthroplasty: A protocol of a randomized controlled trial. BMC Musculoskelet. Disord. 2017, 18, 116. [Google Scholar] [CrossRef]
- Seto, E.; Morita, P.P.; Tomkun, J.; Lee, T.M.; Ross, H.; Reid-Haughian, C.; Kaboff, A.; Mulholland, D.; A Cafazzo, J. Implementation of a heart failure telemonitoring system in home care nursing: Feasibility study. JMIR Public Health Surveill. 2019, 7, e11722. [Google Scholar] [CrossRef]
- Daemen, E.; Flinsenberg, I.; Van, L.E.; Cuppen, R.; Rajae-Joordens, R. The effect of experience on system usability scale ratings. J. Usability Stud. 2012, 7, 56–67. [Google Scholar]
- Sauro, J. A Practical Guide to the System Usability Scale: Background, Benchmarks & Best Practices; Createspace Independent Publishing Platform: Scotts Valley, CA, USA, 2011. [Google Scholar]
- Kelly, L.; Ziebland, S.; Jenkinson, C. Measuring the effects of online health information: Scale validation for the e-Health Impact Questionnaire. Patient Educ. Couns. 2015, 98, 1418–1424. [Google Scholar] [CrossRef]
- Zhao, Y.; Ni, Q.; Zhou, R. What factors influence the mobile health service adoption? A meta-analysis and the moderating role of age. Int. J. Inf. Manag. 2018, 43, 342–350. [Google Scholar] [CrossRef]
- Gill, P.; Stewart, K.; Treasure, E.; Chadwick, B. Methods of data collection in qualitative research: Interviews and focus groups. Br. Dent. J. 2008, 204, 291–295. [Google Scholar] [CrossRef]
- Keesara, S.; Jonas, A.; Schulman, K. COVID-19 and health care’s digital revolution. N. Engl. J. Med. 2020, 382, e82. [Google Scholar] [CrossRef]
- Ke, J.X.; George, R.B.; Wozney, L.; Chorney, J.L. Patient-centred perioperative mobile application in Cesarean delivery: Needs assessment and development. Can. J. Anaesth. 2019, 66, 1194–1201. [Google Scholar] [CrossRef]
- Mackert, M.; Mabry-Flynn, A.; Champlin, S.; Donovan, E.E.; Pounders, K. Health literacy and health information technology adoption: The potential for a new digital divide. J. Med. Internet Res. 2016, 18, e264. [Google Scholar] [CrossRef]
- Hughson, J.-A.P.; Daly, J.O.; Woodward-Kron, R.; Hajek, J.; Story, D. The rise of pregnancy apps and the implications for culturally and linguistically diverse women: Narrative review. JMIR mHealth uHealth 2018, 6, e189. [Google Scholar] [CrossRef]
- Kim, H.; Zhang, Y. Health information seeking of low socioeconomic status Hispanic adults using smartphones. Aslib J. Inf. Manag. 2015, 67, 542–561. [Google Scholar] [CrossRef]
- Vangeepuram, N.; Mayer, V.; Fei, K.; Hanlen-Rosado, E.; Andrade, C.; Wright, S.; Horowitz, C. Smartphone ownership and perspectives on health apps among a vulnerable population in East Harlem, New York. mHealth 2018, 4, 31. [Google Scholar] [CrossRef]
- Niksch, A.L. mHealth in pediatrics-finding healthcare solutions for the next generation. mHealth 2015, 1, 7. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ciechanowicz, S.; Setty, T.; Robson, E.; Sathasivam, C.; Chazapis, M.; Dick, J.; Carvalho, B.; Sultan, P. Development and evaluation of an obstetric quality-of-recovery score (ObsQoR-11) after elective caesarean delivery. Br. J. Anaesth. 2019, 122, 69–78. [Google Scholar] [CrossRef]

| Study | Year | Country | Study Design | Specialty (Procedures Included) | Sample Size (n) | Name of Application | Themes of Application Identified | Specific Features | Format | Outcome Measures | Study Outcomes | SUS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Morte et al. [1] | 2021 | United States | Single-arm study | General surgery (elective cholecystectomy, interval appendectomy, colectomy, bariatric surgery, and open hernia repairs) | 100 | MCare | Patient education and instruction | Peri-operative educational materials; text message reminders of time-sensitive events | Text messages |
|
|
|
| Williems et al. [9] | 2021 | The Netherlands | Cross-sectional study | Orthopedics (surgery for musculoskeletal disorders) | 526 | Patient Journey | Patient education and instruction | Educational materials on pre-operative exercises, surgery, and rehabilitation | iOS and Android apps |
|
|
|
| Ke et al. [19] | 2021 | Canada | Single-arm study | Obstetrics (cesarean delivery) | 36 | C-Care | Complication monitoring; pain monitoring and control; patient education and instruction | Education materials on peri-operative anesthetic topics; self-monitoring questionnaire on pain and complications | iOS app |
|
| N/A |
| Anthony et al. [20] | 2020 | United States | RCT | Orthopedics (operative fixation of a traumatic upper or lower fracture) | 82 | N/A | Pain monitoring and control | Acceptance and Commitment Therapy delivered through text messages | Text messages |
|
| N/A |
| Premkumar et al. [21] | 2018 | United States | Single-arm study | Orthopedics (total hip or knee arthroplasty) | 183 | N/A | Complication monitoring; pain monitoring and control | Daily information collection on patient-reported opioid consumption and pain | Text messages |
|
| N/A |
| Rojas et al. [22] | 2019 | United States | RCT | Orthopedics (musculoskeletal tumour patients) | 14 | N/A | Pain monitoring and control | CBT intervention text messages giving general post-operative guidance and encouragement | Text messages |
|
| N/A |
| Goz et al. [23] | 2019 | United States | Single-arm study | Orthopedics (spine surgery) | 21 | N/A | Patient education and instruction | Text messages to address common post-operative concerns of patients undergoing spine surgery | Text messages |
|
| N/A |
| Wittig-Wells et al. [24] | 2019 | United States | RCT | Orthopedics (hip or knee arthroplasty) | 29 | N/A | Patient education and instruction | Daily pre-set cellular telephone alarm as a reminder for adults to take prescribed aspirin twice daily as antithrombotic therapy | Pre-set phone alarms |
|
| N/A |
| van Dijk-Huisman et al. [25] | 2019 | The Netherlands | Non-randomized trial | Orthopedics (total hip or knee arthroplasty) | 97 | Hospital Fit | Functional recovery; patient education and instruction | Objective exercise monitoring with accelerometer and real-time feedback; provides personalized exercise programme | Smartphone app with accelerometer |
|
| N/A |
| Belarmino et al. [26] | 2019 | United States | Single-arm study | Urology (robotic-assisted radical prostatectomy) | 20 | N/A | Patient education and instruction; functional recovery; pain monitoring and control | Peri-operative reminders to perform Kegel exercises, ambulate, and hydrate | IOS app |
|
| N/A |
| Felbaum et al. [27] | 2018 | United States | Single-arm study | Neurosurgery (routine neurosurgery procedures) | 56 | TrackMyRecovery | Patient education and instruction; pain monitoring and control; complication monitoring; clear communication | Patient-specific pre- and post-operative instructions; pain scores and wound images can be reported through the app | iOS and Android app |
|
| N/A |
| Heuser et al. [28] | 2021 | Canada | Retrospective cohort study | Bariatric surgery (Roux-en-Y gastric bypass, sleeve gastrectomy) | 854 | N/A | Patient education and instruction; pain monitoring and control; complication monitoring | Notification reminders before surgery; peri-operative educational materials; post-operative symptoms and healthcare utilization monitoring | IOS and Android app |
|
| N/A |
| van Hout et al. [29] | 2022 | The Netherlands | Single-arm study | General surgery (inguinal hernia repair) | 242 | Q1.6 Inguinal Hernia | Pain monitoring and control; complication monitoring | Continuous digital patient outcome measurement using non-intrusive, short questions | IOS and Android app |
|
| N/A |
| Sousa et al. [30] | 2019 | Brazil | Single-arm study | Maxillofacial surgery (orthognathic surgery) | 30 | OrtogApp | Patient education and instruction; clear communication | Provides five learning content sessions essential for managing peri-operative care; email contact with specialist nurses | IOS and Android app |
|
| Average SUS of 79.8 |
| Ashraf et al. [31] | 2021 | United Kingdom | Single-arm study | General surgery (colorectal surgery) | 17 | N/A | Patient education and instruction; complication monitoring | Three main components of education, physical, and psychological functional measurements (questionnaires and journal), and post-operative wound monitoring | iOS app |
|
| N/A |
| Abdeen et al. [32] | 2022 | United States | Non-randomized trial | Orthopedics (total hip or knee arthroplasty) | 274 | N/A | Patient education and instruction | Customized messages including appointment reminders for pre-anesthetic appointment, links to educational videos, and real-time text message reminders to perform the requisite tasks of the peri-operative protocols | iOS and Android app |
|
| N/A |
| van der Meij et al. [33] | 2018 | The Netherlands | RCT | General surgery and gynecology (laparoscopic cholecystectomy, hernia inguinal surgery, or laparoscopic adnexal surgery) | 344 | ikHerstel | Functional recovery; patient education and instruction; clear communication | Recovery advice based on personalized convalescence plan; information about the peri-operative period; monitoring and feedback on recovery; e-consult feature | Smartphone app, website, and activity tracker |
|
| N/A |
| Pickens et al. [34] | 2019 | United States | Single-arm study | General surgery (hepatectomy, distal pancreatectomy, pancreatico-duodenectomy) | 122 | N/A | Patient education and instruction; complication monitoring | Pre-operative scheduled task reminders for both general preparation; daily post-discharge health checks with customized responses to guide out-of-hospital care | Web-based platform |
|
| N/A |
| |
| |
| |
| |
| Questionnaires Should Include Data Metrics Such As |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
El-Hadi, H.; Chan, B.L.-H.; Siu, B.W.-H.; Ko, I.C.-H.; Leung, D.K.-W.; Teoh, J.Y.-C.; Chiu, P.K.-F.; Ng, C.-F.; Liu, A.Q. A Systematic Review of Smartphone Applications That Address Patient Care in the Peri-Operative Period. Healthcare 2025, 13, 2775. https://doi.org/10.3390/healthcare13212775
El-Hadi H, Chan BL-H, Siu BW-H, Ko IC-H, Leung DK-W, Teoh JY-C, Chiu PK-F, Ng C-F, Liu AQ. A Systematic Review of Smartphone Applications That Address Patient Care in the Peri-Operative Period. Healthcare. 2025; 13(21):2775. https://doi.org/10.3390/healthcare13212775
Chicago/Turabian StyleEl-Hadi, Hadal, Brandon Lok-Hang Chan, Brian Wai-Hei Siu, Ivan Ching-Ho Ko, David Ka-Wai Leung, Jeremy Yuen-Chun Teoh, Peter Ka-Fung Chiu, Chi-Fai Ng, and Alex Qinyang Liu. 2025. "A Systematic Review of Smartphone Applications That Address Patient Care in the Peri-Operative Period" Healthcare 13, no. 21: 2775. https://doi.org/10.3390/healthcare13212775
APA StyleEl-Hadi, H., Chan, B. L.-H., Siu, B. W.-H., Ko, I. C.-H., Leung, D. K.-W., Teoh, J. Y.-C., Chiu, P. K.-F., Ng, C.-F., & Liu, A. Q. (2025). A Systematic Review of Smartphone Applications That Address Patient Care in the Peri-Operative Period. Healthcare, 13(21), 2775. https://doi.org/10.3390/healthcare13212775







