Incidental Findings on Abdominopelvic CT in Young Korean Soldiers: Prevalence, Clinical Relevance, and Healthcare System Implications
Abstract
1. Introduction
2. Materials and Methods
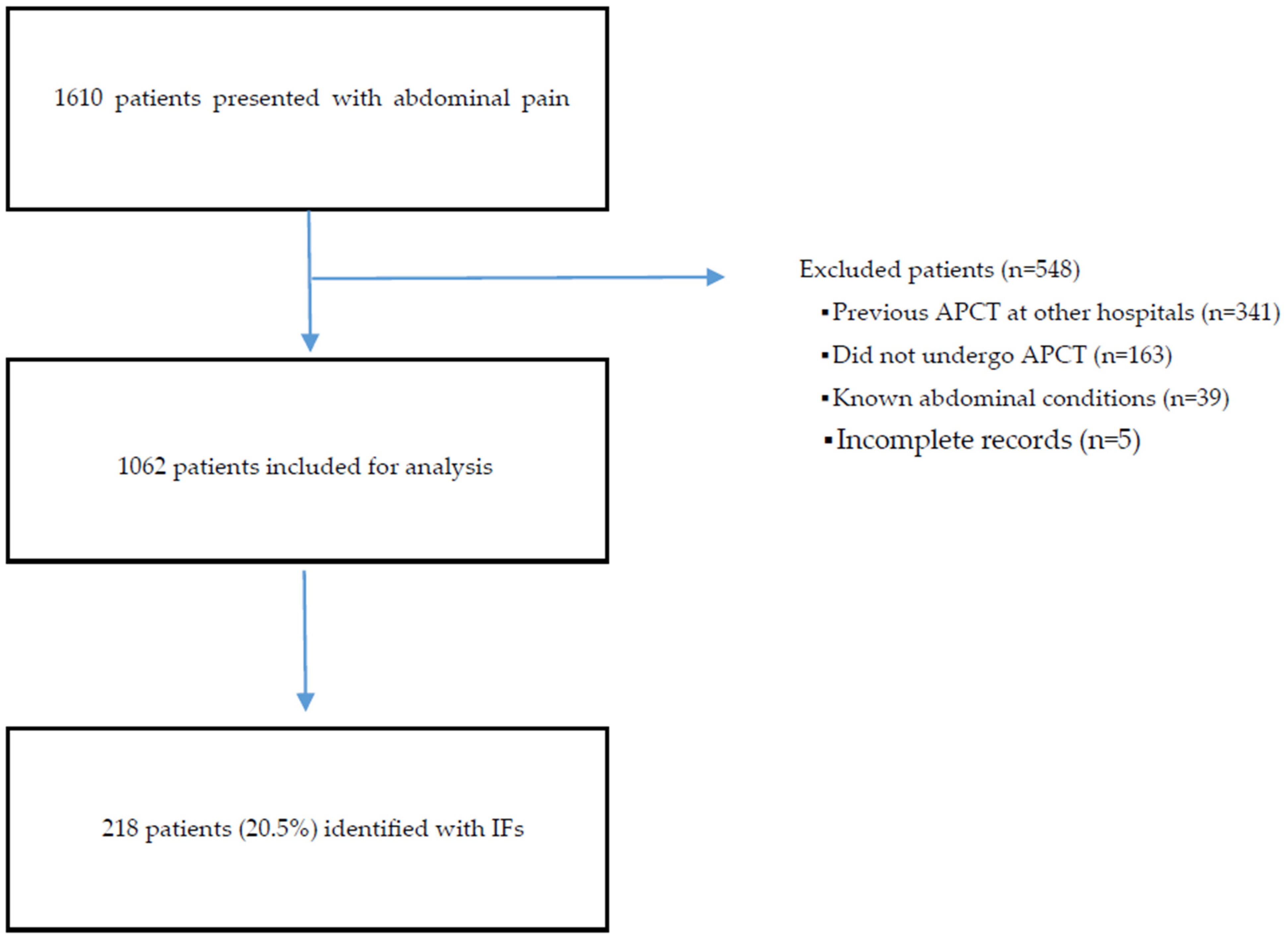
2.1. Study Design and Population
2.2. Definitions and Classification of Incidental Findings
2.3. CT Acquisition and Protocol
2.4. Radiologic Assessment
2.5. Statistical Analysis
3. Results
3.1. Patient Inclusion and Characteristics
3.1.1. Incidental Findings on APCT: Frequencies and Types
3.1.2. Clinically Significant Incidental Findings
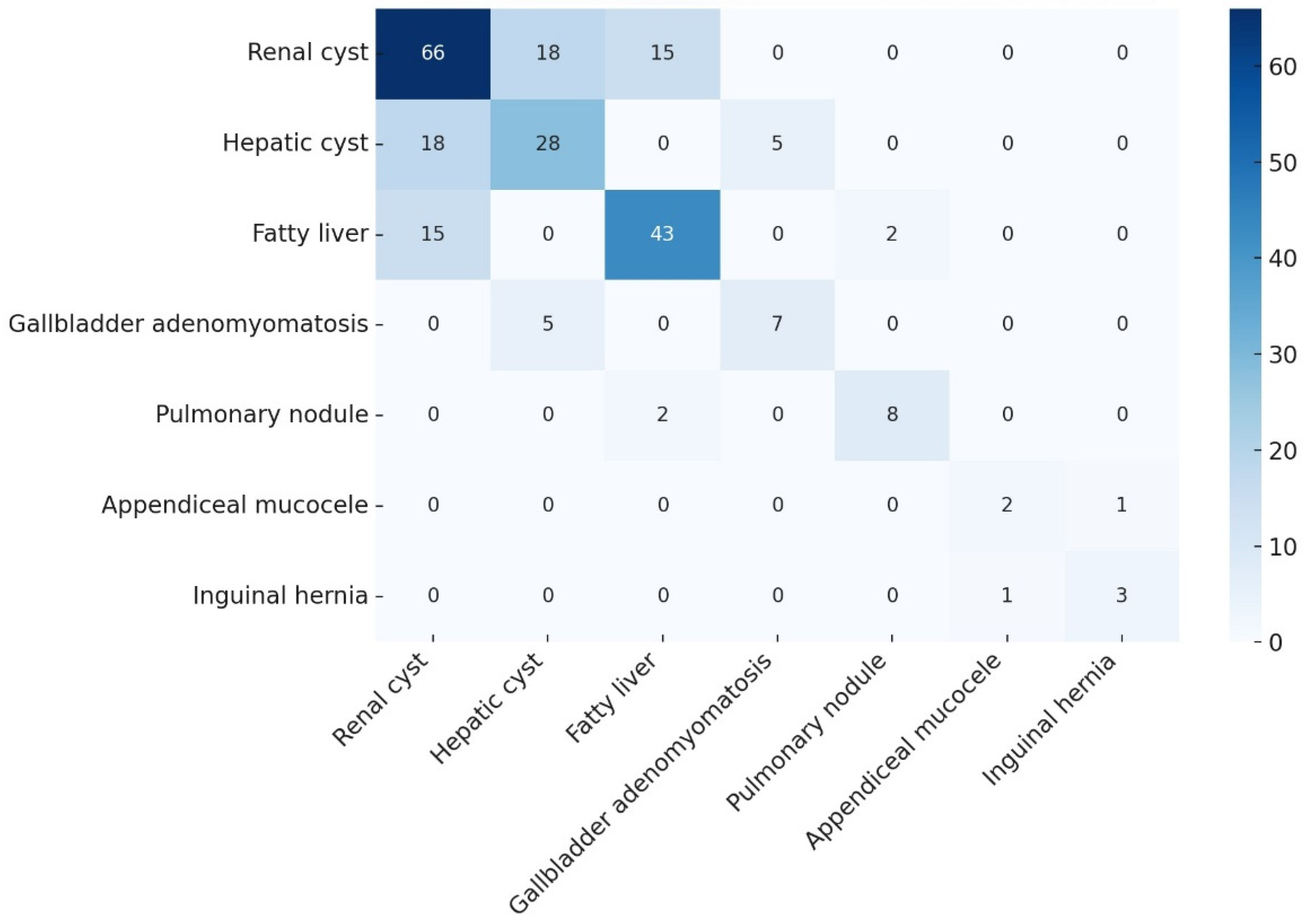
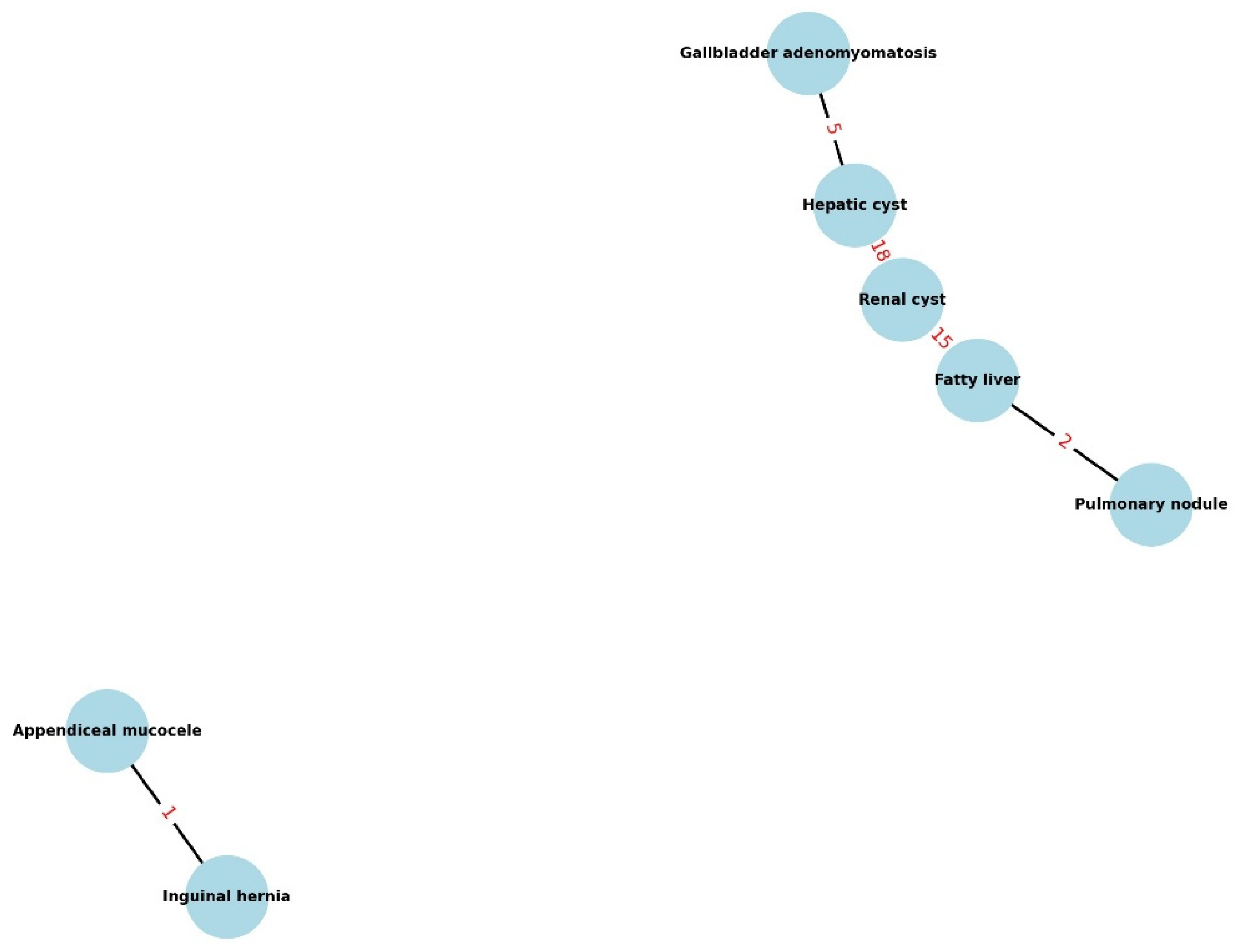
3.1.3. Co-Occurrence of Incidental Findings (Cluster Analysis)
4. Discussion
4.1. Clinical Implications of Incidental Findings
4.2. Co-Occurrence of Incidental Findings
4.3. Military Healthcare Implications
- A standardized IF section in radiology reports with guideline-linked next steps;
- EHR-embedded alerts (size/feature-triggered reminders with default due dates);
- A lightweight IF registry that persists across transfers to preserve follow-up tasks;
- Standardized handoff notes at discharge/transfer listing IFs and due dates;
- Periodic quality dashboards (completion rates, time-to-follow-up) [24].
4.4. External Validity
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| APCT | Abdominopelvic computed tomography |
| IF | Incidental finding |
| ED | Emergency department |
| IPMN | Intraductal papillary mucinous neoplasm |
| ADPKD | Autosomal dominant polycystic kidney disease |
| MCKD | Medullary cystic kidney disease |
| IQR | Interquartile range |
| IRB | Institutional Review Board |
| CT | Computed tomography |
| SPSS | Statistical Package for the Social Sciences |
References
- Samim, M.; Goss, S.; Luty, S.; Weinreb, J.; Moore, C. Incidental findings on CT for suspected renal colic in emergency department patients: Prevalence and types in 5,383 consecutive examinations. J. Am. Coll. Radiol. 2015, 12, 63–69. [Google Scholar] [CrossRef]
- Evans, C.S.; Arthur, R.; Kane, M.; Omofoye, F.; Chung, A.E.; Moreton, E.; Moore, C. Incidental Radiology Findings on Computed Tomography Studies in Emergency Department Patients: A Systematic Review and Meta-Analysis. Ann. Emerg. Med. 2022, 80, 243–256. [Google Scholar] [CrossRef] [PubMed]
- Thompson, R.J.; Wojcik, S.M.; Grant, W.D.; Ko, P.Y. Incidental Findings on CT Scans in the Emergency Department. Emerg. Med. Int. 2011, 2011, 624847. [Google Scholar] [CrossRef] [PubMed]
- Moore, C.L.; Baskin, A.; Chang, A.M.; Cheung, D.; Davis, M.A.; Fertel, B.S.; Hans, K.; Kang, S.K.; Larson, D.M.; Lee, R.K.; et al. White Paper: Best Practices in the Communication and Management of Actionable Incidental Findings in Emergency Department Imaging. J. Am. Coll. Radiol. 2023, 20, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Orme, N.M.; Fletcher, J.G.; Siddiki, H.A.; Harmsen, W.S.; O’Byrne, M.M.; Port, J.D.; Tremaine, W.J.; Pitot, H.C.; McFarland, E.G.; Robinson, M.E.; et al. Incidental findings in imaging research: Evaluating incidence, benefit, and burden. Arch. Intern. Med. 2010, 170, 1525–1532. [Google Scholar] [CrossRef]
- Bae, E.; Park, J.; Jung, E. Unmet Healthcare Needs and Associated Factors Among Korean Enlisted Soldiers. Mil. Med. 2021, 186, e186–e193. [Google Scholar] [CrossRef]
- Lim, A.Y.; Park, S.M.; Shin, E.; Lee, J.-Y.; Choi, J.-S.; Jung, H.-Y. Clinical and Psychological Characteristics of Young Men with Military Adaptation Issues Referred for a Psychiatric Evaluation in South Korea: Latent Profile Analysis of Minnesota Multiphasic Personality Inventory-2 and Temperament and Character Inventory. Psychiatry Investig. 2021, 18, 19–30. [Google Scholar] [CrossRef]
- Reisinger, H.S.; Hunt, S.; Burgo-Black, A.; Agarwal, M. A population approach to mitigating the long-term health effects of combat deployments. Prev. Chronic Dis. 2012, 9, E54. [Google Scholar] [CrossRef]
- Chalasani, N.; Younossi, Z.; LaVine, J.E.; Charlton, M.; Cusi, K.; Rinella, M.; Harrison, S.A.; Brunt, E.M.; Sanyal, A.J. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology 2018, 67, 328–357. [Google Scholar] [CrossRef]
- Fassnacht, M.; Tsagarakis, S.; Terzolo, M.; Tabarin, A.; Sahdev, A.; Newell-Price, J.; Pelsma, I.; Marina, L.; Lorenz, K.; Bancos, I.; et al. European Society of Endocrinology clinical practice guidelines on the management of adrenal incidentalomas, in collaboration with the European Network for the Study of Adrenal Tumors. Eur. J. Endocrinol. 2023, 189, G1–G42. [Google Scholar] [CrossRef]
- Hamada, T.; Oyama, H.; Tange, S.; Hakuta, R.; Ishigaki, K.; Kanai, S.; Kawaguchi, Y.; Noguchi, K.; Saito, T.; Sato, T.; et al. The Revised Kyoto Criteria and Risk of Malignancy Among Patients with Intraductal Papillary Mucinous Neoplasms. Clin. Gastroenterol. Hepatol. 2024, 22, 2413–2423.e18. [Google Scholar] [CrossRef]
- MacMahon, H.; Naidich, D.P.; Goo, J.M.; Lee, K.S.; Leung, A.N.C.; Mayo, J.R.; Mehta, A.C.; Ohno, Y.; Powell, C.A.; Prokop, M.; et al. Guidelines for Management of Incidental Pulmonary Nodules Detected on CT Images: From the Fleischner Society 2017. Radiology 2017, 284, 228–243. [Google Scholar] [CrossRef]
- McGrath, T.A.; Davenport, M.S.; Silverman, S.G.; Lim, C.S.; Almalki, Y.E.; Arita, Y.; Bai, X.; Basha, M.A.A.; Dana, J.; Elbanna, K.Y.; et al. Bosniak Classification of Cystic Renal Masses Version 2019: Proportion of Malignancy by Class and Subclass-Systematic Review and Meta-Analysis. AJR Am. J. Roentgenol. 2025, 224, e2432342. [Google Scholar] [CrossRef]
- Silverman, S.G.; Pedrosa, I.; Ellis, J.H.; Hindman, N.M.; Schieda, N.; Smith, A.D.; Remer, E.M.; Shinagare, A.B.; Curci, N.E.; Raman, S.S.; et al. Bosniak Classification of Cystic Renal Masses, Version 2019: An Update Proposal and Needs Assessment. Radiology 2019, 292, 475–488. [Google Scholar] [CrossRef]
- Tanaka, M.; Fernández-del Castillo, C.; Kamisawa, T.; Jang, J.Y.; Levy, P.; Ohtsuka, T.; Salvia, R.; Shimizu, Y.; Tada, M.; Wolfgang, C.L. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology 2017, 17, 738–753. [Google Scholar] [CrossRef] [PubMed]
- Golse, N.; Lewin, M.; Rode, A.; Sebagh, M.; Mabrut, J.-Y. Gallbladder adenomyomatosis: Diagnosis and management. J. Visc. Surg. 2017, 154, 345–353. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; AlSubaie, R.S.; Saleh, A.A.A. Mucocele of the Appendix: A Case Report and Review of Literature. Cureus 2023, 15, e40168. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Fernández-del Castillo, C.; Adsay, V.; Chari, S.; Falconi, M.; Jang, J.-Y.; Kimura, W.; Levy, P.; Pitman, M.B.; Schmidt, C.M.; et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology 2012, 12, 183–197. [Google Scholar] [CrossRef]
- Fassnacht, M.; Arlt, W.; Bancos, I.; Dralle, H.; Newell-Price, J.; Sahdev, A.; Tabarin, A.; Terzolo, M.; Tsagarakis, S.; Dekkers, O.M. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur. J. Endocrinol. 2016, 175, G1–G34. [Google Scholar] [CrossRef]
- Safari, S.; Dizaji, S.R.; Yousefifard, M.; Taheri, M.S.; Sharifi, A. Prevalence and clinical significance of incidental findings in chest and abdominopelvic CT scans of trauma patients; A cross-sectional study. Am. J. Emerg. Med. 2024, 82, 117–124. [Google Scholar] [CrossRef]
- Paluska, T.R.; Sise, M.J.M.; Sack, D.I.B.; Sise, C.B.J.; Egan, M.C.M.; Biondi, M. Incidental CT findings in trauma patients: Incidence and implications for care of the injured. J. Trauma 2007, 62, 157–161. [Google Scholar] [CrossRef]
- Lee, J.; Jung, J.H.; Choi, S.J.; Ha, B.; Yang, H.; Sung, P.S.; Bae, S.H.; Yu, J.-A. Impact of Korean Military Service on the Prevalence of Steatotic Liver Disease: A Longitudinal Study of Pre-enlistment and In-Service Health Check-Ups. Gut Liver 2024, 18, 888–896. [Google Scholar] [CrossRef] [PubMed]
- Hélénon, O.; Crosnier, A.; Verkarre, V.; Merran, S.; Méjean, A.; Correas, J.-M. Simple and complex renal cysts in adults: Classification system for renal cystic masses. Diagn. Interv. Imaging 2018, 99, 189–218. [Google Scholar] [CrossRef]
- Bunck, A.C.; Baeßler, B.; Ritter, C.; Kröger, J.R.; Persigehl, T.; Santos, D.P.; Steinmetz, M.; Niehaus, A.; Bamberg, F.; Beer, M.; et al. Structured Reporting in Cross-Sectional Imaging of the Heart: Reporting Templates for CMR Imaging of Cardiomyopathies (Myocarditis, Dilated Cardiomyopathy, Hypertrophic Cardiomyopathy, Arrhythmogenic Right Ventricular Cardiomyopathy and Siderosis). Fortschr Röntgenstrahlen 2020, 192, 27–37. [Google Scholar] [CrossRef]
- Zaki-Metias, K.M.; MacLean, J.J.; Satei, A.M.; Medvedev, S.; Wang, H.; Zarour, C.C.; Arpasi, P.J. The FIND Program: Improving Follow-up of Incidental Imaging Findings. J. Digit. Imaging 2023, 36, 804–811. [Google Scholar] [CrossRef]
| Characteristic * | With IFs (n = 218) | Without IFs (n = 844) | p-Value |
|---|---|---|---|
| Age (years), median (IQR) | 21 (20–22) | 21 (20–22) | 0.14 |
| Current smoker, n (%) | 80 (36.7) | 280 (33.2) | 0.39 |
| BMI (kg/m2), median (IQR] | 24 (22–26) | 23 (21–25) | 0.08 |
| Any previous medical history, n (%) | 20 (9.2) | 60 (7.1) | 0.37 |
| Location | Incidental Finding | IF (n = 218), n (%) | All APCT Scans (n = 1062), n (%) |
|---|---|---|---|
| Liver and Spleen | Hemangioma | 9 (4.1%) | 9 (0.8%) |
| Cyst | 28 (12.8%) | 28 (2.6%) | |
| Symptomatic or >4 cm cyst | 0 (0%) | 0 (0%) | |
| Polycystic liver disease (with multiple renal cysts) | 1 (0.5%) | 1 (0.1%) | |
| Fatty liver | 43 (19.7%) | 43 (4.0%) | |
| Hepatomegaly | 5 (2.3%) | 5 (0.5%) | |
| Splenomegaly | 11 (5.0%) | 11 (1.0%) | |
| Hepatosplenomegaly | 2 (0.9%) | 2 (0.2%) | |
| Gallbladder | Asymptomatic stone | 9 (4.1%) | 9 (0.8%) |
| Adenomyomatosis | 7 (3.2%) | 7 (0.7%) | |
| Pancreas | Intraductal papillary mucinous neoplasm | 1 (0.5%) | 1 (0.1%) |
| Cyst | 1 (0.5%) | 1 (0.1%) | |
| Adrenal gland | Hyperplasia | 2 (0.9%) | 2 (0.2%) |
| Adenoma | 2 (0.9%) | 2 (0.2%) | |
| Large adenoma (>2 cm) | 1 (0.5%) | 1 (0.1%) | |
| Kidney | Cyst (any) | 66 (30.3%) | 66 (6.2%) |
| – Single cyst | 49 (22.5%) | 49 (4.6%) | |
| >1 cm (subset of single cysts) | 20 (9.2%) | 20 (1.9%) | |
| – Multiple cysts | 17 (7.8%) | 17 (1.6%) | |
| • Largest > 1 cm | 9 (4.1%) | 9 (0.8%) | |
| – Cysts in both kidneys | 7 (3.2%) | 7 (0.7%) | |
| Bosniak classification: | |||
| • I | 56 (25.7%) | 56 (5.3%) | |
| • II | 5 (2.3%) | 5 (0.5%) | |
| • IIF | 3 (1.4%) | 3 (0.3%) | |
| • III/IV | 0 (0%) | 0 (0%) | |
| ADPKD (polycystic kidney disease) | 1 (0.5%) | 1 (0.1%) | |
| MCKD (medullary cystic kidney disease) | 1 (0.5%) | 1 (0.1%) | |
| Asymptomatic stone (kidney or ureter) | 20 (9.2%) | 20 (1.9%) | |
| Congenital anomalies: | |||
| • Horseshoe kidney | 2 (0.9%) | 2 (0.2%) | |
| • Incomplete kidney malrotation | 1 (0.5%) | 1 (0.1%) | |
| • Mal-rotated (downward) kidney | 1 (0.5%) | 1 (0.1%) | |
| Gastrointestinal | Diverticulosis (colonic) | 8 (3.7%) | 8 (0.8%) |
| Appendiceal mucocele | 2 (0.9%) | 2 (0.2%) | |
| Internal hemorrhoid | 2 (0.9%) | 2 (0.2%) | |
| Perineal region | Inguinal hernia | 3 (1.4%) | 3 (0.3%) |
| Prostatic cyst | 5 (2.3%) | 5 (0.5%) | |
| Urethral diverticulum | 1 (0.5%) | 1 (0.1%) | |
| Spine/Pelvis | Scoliosis | 4 (1.8%) | 4 (0.4%) |
| (musculoskeletal) | Spondylosis (with spondylolisthesis) | 8 (3.7%) | 8 (0.8%) |
| Lumbarization of S1 | 2 (0.9%) | 2 (0.2%) | |
| Sacroiliitis | 4 (1.8%) | 4 (0.4%) | |
| Lung | Pulmonary nodule | 8 (3.7%) | 8 (0.8%) |
| Other | Urachal remnant | 2 (0.9%) | 2 (0.2%) |
| Abdominal wall hemangioma | 1 (0.5%) | 1 (0.1%) | |
| SMA with acute angle | 1 (0.5%) | 1 (0.1%) |
| Incidental Finding | Patients (%) | Clinical Implication | Recommended Management |
|---|---|---|---|
| Gallbladder adenomyomatosis | 7 (3.2%) | Potential malignancy risk | Periodic follow-up imaging |
| Bosniak IIF renal cyst | 3 (1.4%) | Uncertain malignancy potential | Scheduled follow-up CT |
| Appendiceal mucocele | 2 (0.9%) | Malignant potential | Surgical resection |
| ADPKD | 1 (0.5%) | Renal dysfunction | Referral to specialist |
| Adrenal adenoma (>2 cm) | 1 (0.5%) | Endocrine evaluation | Specialist follow-up |
| Primary IF | Co-Occurring IF | Patients, n (%) | Odds Ratio (95% CI) | p-Value | q-Value |
|---|---|---|---|---|---|
| Renal cyst | Hepatic cyst | 18 (27.3%) | 2.3 (1.3–4.1) | 0.008 | 0.016 |
| Renal cyst | Fatty liver | 15 (22.7%) | 1.8 (1.0–3.3) | 0.045 | 0.045 |
| Hepatic cyst | Gallbladder adenomyomatosis | 5 (17.9%) | 3.1 (1.2–8.0) | 0.032 | 0.043 |
| Appendiceal mucocele | Inguinal hernia | 1 (50.0%) | 11.2 (1.5–85.0) | 0.004 | 0.016 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, K.; Jung, K.U.; Lee, C.; Lee, D. Incidental Findings on Abdominopelvic CT in Young Korean Soldiers: Prevalence, Clinical Relevance, and Healthcare System Implications. Healthcare 2025, 13, 2736. https://doi.org/10.3390/healthcare13212736
Lee K, Jung KU, Lee C, Lee D. Incidental Findings on Abdominopelvic CT in Young Korean Soldiers: Prevalence, Clinical Relevance, and Healthcare System Implications. Healthcare. 2025; 13(21):2736. https://doi.org/10.3390/healthcare13212736
Chicago/Turabian StyleLee, Kyungwon, Kyung Uk Jung, Changsin Lee, and Donghyoun Lee. 2025. "Incidental Findings on Abdominopelvic CT in Young Korean Soldiers: Prevalence, Clinical Relevance, and Healthcare System Implications" Healthcare 13, no. 21: 2736. https://doi.org/10.3390/healthcare13212736
APA StyleLee, K., Jung, K. U., Lee, C., & Lee, D. (2025). Incidental Findings on Abdominopelvic CT in Young Korean Soldiers: Prevalence, Clinical Relevance, and Healthcare System Implications. Healthcare, 13(21), 2736. https://doi.org/10.3390/healthcare13212736






