Nurse-Led Microsurgical Free Flap Monitoring: A Scoping Review and Evidence-Based Framework
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Research Question
- Population: Patients undergoing free flap reconstruction
- Concept: Nurse involvement in postoperative monitoring
- Context: All surgical specialties and healthcare settings
2.3. Search Strategy
2.4. Eligibility Criteria
2.4.1. Inclusion Criteria
- Studies involving any form of nurse participation in the postoperative monitoring of free flaps;
- All study designs (e.g., experimental, observational, qualitative, mixed methods);
- All publication types (e.g., peer-reviewed articles, gray literature);
- No restrictions on language or publication year.
2.4.2. Exclusion Criteria
- Studies focusing solely on surgical techniques without nursing components;
- Studies where nursing involvement could not be distinguished from other healthcare professionals;
- Conference abstracts without available full text;
- Editorials and opinion pieces without empirical data.
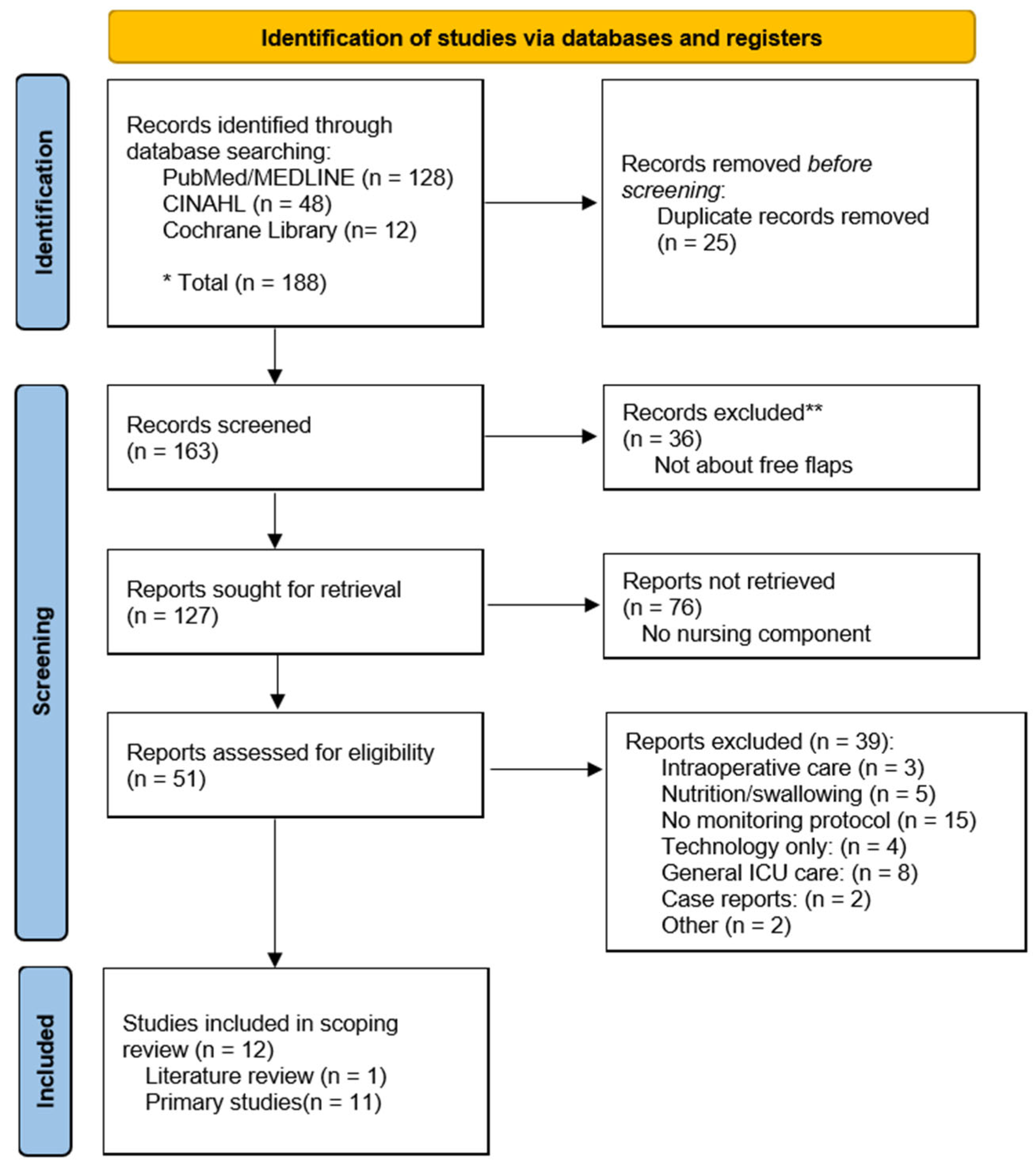
2.5. Study Selection
2.6. Data Extraction
Extracted Data Included
- Study characteristics: Author(s), year, country, study design, sample size, setting
- Monitoring protocols: Personnel involved, monitoring frequency, nurse-to-patient ratios, assessment methods
- Clinical outcomes: Flap success rates, salvage rates, complications
- Educational components: Training programs, knowledge assessments, confidence measures
- Key findings relevant to nurse involvement
2.7. Data Charting and Synthesis
2.8. Ethical Considerations
3. Results
3.1. Study Selection Results
3.2. Characteristics of Included Studies
3.3. Monitoring Protocols and Implementation
3.4. Clinical Outcomes
3.5. Educational Interventions and Nurse Competency
3.6. Emerging Themes
- Equivalence of Outcomes: Nurse-led monitoring consistently achieved outcomes comparable to traditional physician-led systems across diverse settings.
- Technology as Enabler: Objective monitoring devices (tissue oximetry, implantable Doppler) reduced nurse anxiety and improved confidence while maintaining high success rates.
- Standardization Gap: Despite successful outcomes, substantial variation existed in protocols, training approaches, and documentation methods across institutions.
4. Discussion
4.1. Principal Findings
4.2. Bridging the Gap in Venous Congestion Management: From Knowledge to Authorized Practice
- Developing explicit protocols that authorize trained nurses to perform pinprick testing.
- Providing hands-on training in both the technique and interpretation of results.
- Establishing clear escalation pathways for abnormal findings.
- Ensuring legal and institutional protection for nurses performing this expanded role.
4.3. Technology as a Tool for Objective Assessment
- Implantable Doppler: Real-time audible feedback on flow
- Tissue oximetry: Continuous StO2 values with clear thresholds
4.4. Closing the Standardization Gap: A Framework for Implementation
4.4.1. Standardized Education
4.4.2. Standardized Protocols and Tools
4.4.3. Standardized Integration of Technology
4.5. Strengths, Limitations, and Contributions to the Field
5. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Escandon, J.M.; Ciudad, P.; Mayer, H.F.; Pencek, M.; Mantilla-Rivas, E.; Mohammad, A.; Langstein, H.N.; Manrique, O.J. Free flap transfer with supermicrosurgical technique for soft tissue reconstruction: A systematic review and meta-analysis. Microsurgery 2023, 43, 171–184. [Google Scholar] [CrossRef]
- Shen, A.Y.; Lonie, S.; Lim, K.; Farthing, H.; Hunter-Smith, D.J.; Rozen, W.M. Free Flap Monitoring, Salvage, and Failure Timing: A Systematic Review. J. Reconstr. Microsurg. 2021, 37, 300–308. [Google Scholar] [CrossRef]
- Kohlert, S.; Quimby, A.E.; Saman, M.; Ducic, Y. Postoperative Free-Flap Monitoring Techniques. Semin. Plast. Surg. 2019, 33, 13–16. [Google Scholar] [CrossRef]
- Salgado, C.J.; Chim, H.; Schoenoff, S.; Mardini, S. Postoperative care and monitoring of the reconstructed head and neck patient. Semin. Plast. Surg. 2010, 24, 281–287. [Google Scholar] [CrossRef]
- Accreditation Council for Graduate Medical Education. The ACGME’s Approach to Limit Resident Duty Hours 12 Months After Implementation: A Summary of Achievements; Accreditation Council for Graduate Medical Education: Chicago, IL, USA, 2004. [Google Scholar]
- British Medical Association. Doctors and the European Working Time Directive; British Medical Association: London, UK, 2021. [Google Scholar]
- Khoushhal, Z.; Hussain, M.A.; Greco, E.; Mamdani, M.; Verma, S.; Rotstein, O.; Tricco, A.C.; Al-Omran, M. Prevalence and causes of attrition among surgical residents: A systematic review and meta-analysis. JAMA Surg. 2017, 152, 265–272. [Google Scholar] [CrossRef]
- Kang, D. Challenges in Pediatric Facial Laceration Management Amid the Health Care Crisis in South Korea. J. Craniofacial Surg. 2025. [Google Scholar] [CrossRef]
- Kleban, S.R.; Ogley, S.C.; MacDavid, J.C.; Goldman, J.J.; Francis, A.; Colombini, C.J.; Baynosa, R.C. Nursing monitoring of microsurgical free flaps: Identifying and addressing knowledge gaps. J. Reconstr. Microsurg. 2020, 36, 673–679. [Google Scholar] [CrossRef] [PubMed]
- Tsuge, I.; Yamanaka, H.; Katsube, M.; Sakamoto, M.; Saito, S.; Morimoto, N. Fingerstall-type tissue oximetry reduced anxiety of nurses in postoperative nursing monitoring of free flaps. Plast. Reconstr. Surg.–Glob. Open 2021, 9, e3991. [Google Scholar] [CrossRef] [PubMed]
- Anagnos, V.J.; Brody, R.M.; Carey, R.M.; De Ravin, E.; Tasche, K.K.; Newman, J.G.; Shanti, R.M.; Chalian, A.A.; Rassekh, C.H.; Weinstein, G.S. Post-operative monitoring for head and neck microvascular reconstruction in the era of resident duty hour restrictions: A Retrospective Cohort Study Comparing 2 Monitoring Protocols. Ann. Otol. Rhinol. Laryngol. 2023, 132, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Park, R.C.W.; Bresler, A.Y.; Bansal, A.P.; Baredes, S. Outcomes in microvascular head and neck reconstruction in the setting of restricted residency hours. Am. J. Otolaryngol. 2018, 39, 522–526. [Google Scholar] [CrossRef]
- Patel, U.A.; Hernandez, D.; Shnayder, Y.; Wax, M.K.; Hanasono, M.M.; Hornig, J.; Ghanem, T.A.; Old, M.; Jackson, R.S.; Ledgerwood, L.G. Free flap reconstruction monitoring techniques and frequency in the era of restricted resident work hours. JAMA Otolaryngol.–Head Neck Surg. 2017, 143, 803–809. [Google Scholar] [CrossRef]
- Varadarajan, V.V.; Arshad, H.; Dziegielewski, P.T. Head and neck free flap reconstruction: What is the appropriate post-operative level of care? Oral Oncol. 2017, 75, 61–66. [Google Scholar] [CrossRef]
- Hadie, S.N.H. ABC of a scoping review: A simplified JBI scoping review guideline. Educ. Med. J. 2024, 16, 185–197. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Westphaln, K.K.; Regoeczi, W.; Masotya, M.; Vazquez-Westphaln, B.; Lounsbury, K.; McDavid, L.; Lee, H.; Johnson, J.; Ronis, S.D. From Arksey and O’Malley and Beyond: Customizations to enhance a team-based, mixed approach to scoping review methodology. MethodsX 2021, 8, 101375. [Google Scholar] [CrossRef]
- Stevens, M.N.; Prasad, K.; Sharma, R.K.; Gallant, J.N.; Habib, D.R.; Langerman, A.; Mannion, K.; Rosenthal, E.; Topf, M.C.; Rohde, S.L. Comparative Outcomes for Microvascular Free Flap Monitoring Outside the Intensive Care Unit. Otolaryngol.–Head Neck Surg. 2024, 171, 381–386. [Google Scholar] [CrossRef]
- Yu, P.K.; Sethi, R.K.; Rathi, V.; Puram, S.V.; Lin, D.T.; Emerick, K.S.; Durand, M.L.; Deschler, D.G. Postoperative care in an intermediate-level medical unit after head and neck microvascular free flap reconstruction. Laryngoscope Investig. Otolaryngol. 2019, 4, 39–42. [Google Scholar] [CrossRef] [PubMed]
- Jackson, R.S.; Walker, R.J.; Varvares, M.A.; Odell, M.J. Postoperative monitoring in free tissue transfer patients: Effective use of nursing and resident staff. Otolaryngol.-Head Neck Surg. 2009, 141, 621–625. [Google Scholar] [CrossRef]
- Devine, J.; Potter, L.; Magennis, P.; Brown, J.; Vaughan, E. Flap monitoring after head and neck reconstruction: Evaluating an observation protocol. J. Wound Care 2001, 10, 525–529. [Google Scholar] [CrossRef] [PubMed]
- Barrera, J.M.; Faz, M.G.; García, M.A.; Garcia, A.C.; Piñero, M.N. Implementation of an easy-to-follow standardized chart for free flaps clinical monitoring during the start of a head and neck microsurgery unit in a tertiary hospital. J. Stomatol. Oral Maxillofac. Surg. 2019, 120, 474–475. [Google Scholar] [CrossRef]
- Lin, T.-R.; Yang, C.-I.; Wu, C.-Y.; Liao, Y.-M. Project to improve the free flap survival rate in oral cancer microreconstruction free flap surgery. Hu Li Za Zhi 2013, 60, 68. [Google Scholar] [PubMed]
- Kim, J.H.; Yoon, S.; Kwon, H.; Oh, D.Y.; Jun, Y.-J.; Moon, S.-H. Safe and effective thrombolysis in free flap salvage: Intra-arterial urokinase infusion. PLoS ONE 2023, 18, e0282908. [Google Scholar] [CrossRef] [PubMed]
- Boissiere, F.; Gandolfi, S.; Riot, S.; Kerfant, N.; Jenzeri, A.; Hendriks, S.; Grolleau, J.-L.; Khechimi, M.; Herlin, C.; Chaput, B. Flap venous congestion and salvage techniques: A systematic literature review. Plast. Reconstr. Surg.–Glob. Open 2021, 9, e3327. [Google Scholar] [CrossRef] [PubMed]
| Author (Year) | Country | Study Design | Sample Size | Setting | Primary Focus |
|---|---|---|---|---|---|
| Kleban (2020) [9] | USA | Retrospective | 150 patients | Single center | ICU vs. ward |
| Tsuge (2021) [10] | Japan | Pre-post intervention | 10 flaps | Single center | Nurse anxiety with oximetry |
| Anagnos (2023) [11] | USA | Prospective educational intervention | 72 nurses | Single center | Nursing education |
| Park (2018) [12] | USA | Retrospective | 122 flaps | Single center | Protocol comparison |
| Patel (2017) [13] | USA | Prospective cohort | 1085 flaps | 34 institutions | Monitoring frequency |
| Varadarajan (2017) [14] | USA | Literature review | 17 studies | Multiple studies | Nurse vs. Physician monitoring |
| Stevens (2024) [18] | USA | Retrospective | 803 flaps | 2 hospitals | Resident monitoring frequency |
| Yu (2018) [19] | USA | Retrospective | 512 flaps | Single center | Intermediate care unit |
| Jackson (2009) [20] | USA | Retrospective | 94 patients | Single center | Nurse vs. resident monitoring |
| Devine et al., (2001) [21] | UK | Retrospective | 370 flaps | Single center | Monitoring frequency |
| Megías Barrera (2019) [22] | Spain | Implementation study | NS | Single center | Monitoring chart |
| Lin (2013) [23] | Taiwan | QI project | 53 patients | Single center | Protocol improvement |
| Author (Year) | Monitoring Protocol | Flap Success Rate | Salvage Rate | Key Findings/Other Outcomes |
|---|---|---|---|---|
| (Personnel, Frequency, Tools) | ||||
| Kleban (2020) [9] | Educational Intervention | N/A | N/A | Structured education improved nurse knowledge (61.9% → 89.3%) |
| (Not a clinical protocol) | ||||
| Tsuge (2021) [10] | Nurses, q4h (24–100 h), Tissue oximetry | 100% | N/A | Toccare® device reduced nurse anxiety (41% → 7%) |
| Anagnos (2023) [11] | Nurses/Residents, q1h (Nurses), | 95.60% | 75.5%/74.4% | No difference in failure rates with less frequent resident checks (p = 0.27) |
| q4h vs. q12h (Residents) | ||||
| Implantable Doppler | ||||
| Park (2018) [12] | Nurses/Residents, q1h (Nurses), q12h (Residents) | 96% | 64.30% | Nurse-led protocol with limited resident checks is effective and safe |
| Implantable Doppler | ||||
| Patel (2017) [13] | Nurses/Residents, q1h (Nurses), | 95.20% | 65% | Increased frequency of resident checks does not improve outcomes |
| Variable (Residents) | ||||
| Handheld Doppler (68%) | ||||
| Implanted Doppler (31%) | ||||
| Varadarajan (2017) [14] | Literature Review (17 studies) | 95.70% | 65.5% (mean) | Nurse monitoring is non-inferior to physician monitoring |
| Stevens (2024) [18] | Nurses, q1h, 1:4 ratio | 96.70% | 60% | No difference in flap loss between ICU vs. ward (p = 0.82) |
| Clinical assessment | ||||
| Yu (2018) [19] | Nurses, q1h, 1:3 ratio | 97.10% | 67% | Intermediate monitoring unit is a cost-effective alternative to ICU |
| Implantable Doppler | ||||
| Jackson (2009) [20] | Nurses/Residents, | 94.70% | 60% | Nurse-led monitoring is as effective as resident-led protocol |
| q1h (Nurses), q2h (Residents) | ||||
| Devine et al., (2001) [21] | Nurses, q1h for 72 h | 94% | 76% | Early detection of flap compromise (avg. 17.5 h) is critical for successful salvage. |
| Clinical assessment | Recommended hourly monitoring for the first 72 h. | |||
| Doppler for buried flaps | ||||
| Megías Barrera (2019) [22] | Nurses, q1h, Standardized chart | NR | NR | Standardized chart improved communication and early detection |
| Lin (2013) [23] | Nurses, q1h → q4h, Clinical assessment | 96.20% | 50% | Protocol improvement reduced detection-to-intervention time |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, D. Nurse-Led Microsurgical Free Flap Monitoring: A Scoping Review and Evidence-Based Framework. Healthcare 2025, 13, 2703. https://doi.org/10.3390/healthcare13212703
Kang D. Nurse-Led Microsurgical Free Flap Monitoring: A Scoping Review and Evidence-Based Framework. Healthcare. 2025; 13(21):2703. https://doi.org/10.3390/healthcare13212703
Chicago/Turabian StyleKang, Daihun. 2025. "Nurse-Led Microsurgical Free Flap Monitoring: A Scoping Review and Evidence-Based Framework" Healthcare 13, no. 21: 2703. https://doi.org/10.3390/healthcare13212703
APA StyleKang, D. (2025). Nurse-Led Microsurgical Free Flap Monitoring: A Scoping Review and Evidence-Based Framework. Healthcare, 13(21), 2703. https://doi.org/10.3390/healthcare13212703






