Reduction in Severe, Chronic Mid-Back Pain Following Correction of Sagittal Thoracic Spinal Alignment Using Chiropractic BioPhysics® Spinal Rehabilitation Program Following Prior Failed Treatment: A Case Report with 9-Month Follow-Up
Abstract
1. Introduction
2. Methods
2.1. Ethical Considerations and Declarations
2.2. Patient History, Examination Results, and Subjective and Objective Findings
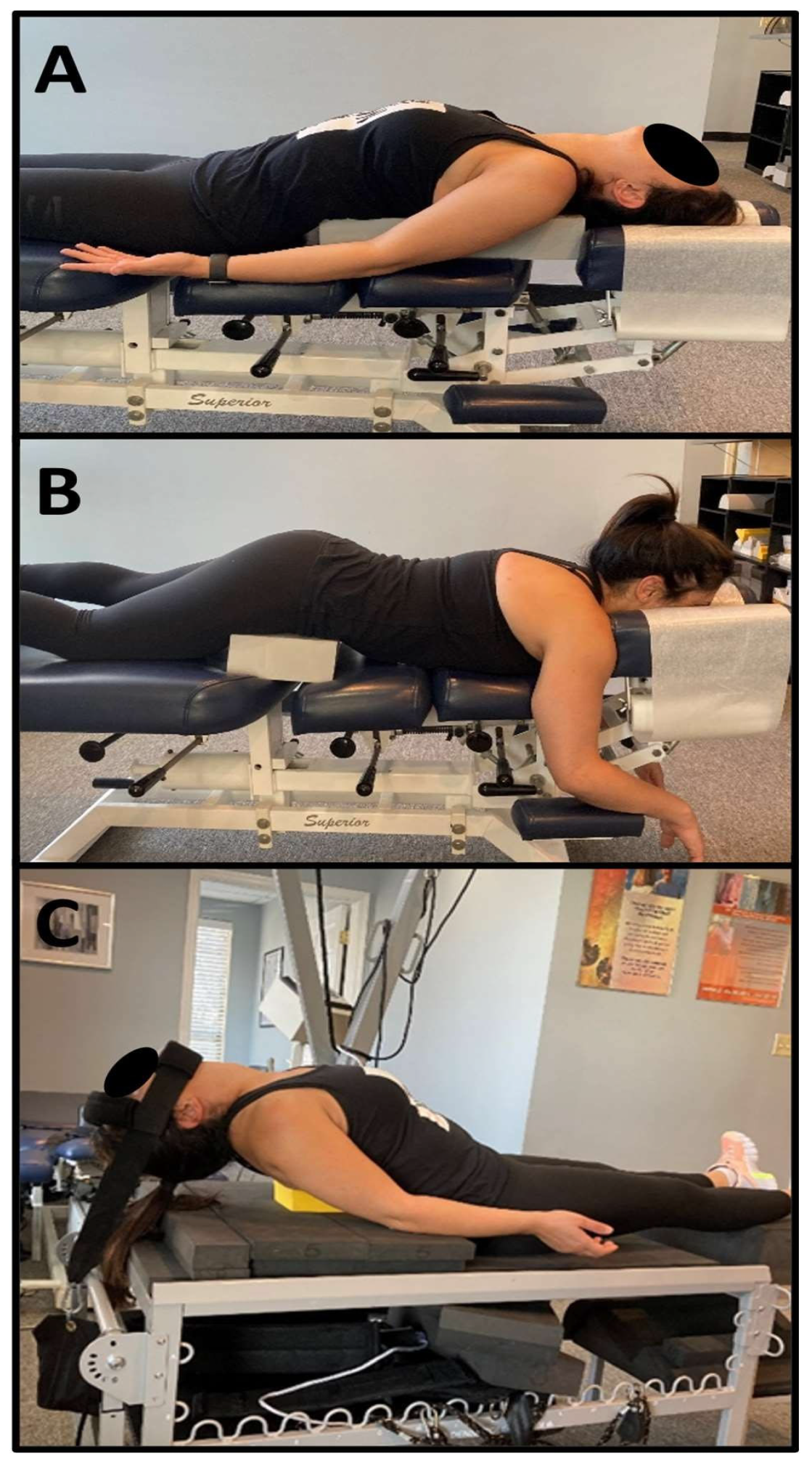
2.3. Treatment Protocol
3. Results
3.1. Post-Treatment Subjective and Objective Findings
3.2. Post-Treatment Radiographic Findings and Home Care Recommendations
3.3. Nine-Month Post-Treatment Long-Term Follow-Up
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hoy, D.; Bain, C.; Williams, G.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Vos, T.; Buchbinder, R. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012, 64, 2028–2037. [Google Scholar] [CrossRef] [PubMed]
- Schneider, S.; Randoll, D.; Buchner, M. Why do women have back pain more than men? A representative prevalence study in the federal republic of Germany. Clin. J. Pain 2006, 22, 738–747. [Google Scholar] [CrossRef]
- Freburger, J.K.; Holmes, G.M.; Agans, R.P.; Jackman, A.M.; Darter, J.D.; Wallace, A.S.; Castel, L.D.; Kalsbeek, W.D.; Carey, T.S. The rising prevalence of chronic low back pain. Arch. Intern. Med. 2009, 169, 251–258. [Google Scholar] [CrossRef]
- Oakley, P.A.; Harrison, D.D.; Harrison, D.E.; Haas, J.W. Evidence-based protocol for structural rehabilitation of the spine and posture: Review of clinical biomechanics of posture (CBP) publications. J. Can. Chiropr. Assoc. 2005, 49, 270–296. [Google Scholar]
- Harrison, D.E.; Cailliet, R.; Harrison, D.D.; Janik, T.J.; Holland, B. Changes in sagittal lumbar configuration with a new method of extension traction: Nonrandomized clinical controlled trial. Arch. Phys. Med. Rehabil. 2002, 83, 1585–1591. [Google Scholar] [CrossRef]
- Moustafa, I.M.; Diab, A.A.; Harrison, D.E. The effect of normalizing the sagittal cervical configuration on dizziness, neck pain, and cervicocephalic kinesthetic sensibility: A 1-year randomized controlled study. Eur. J. Phys. Rehabil. Med. 2017, 53, 57–71. [Google Scholar] [CrossRef]
- Gong, W. The effects of cervical joint manipulation, based on passive motion analysis, on cervical lordosis, forward head posture, and cervical ROM in university students with abnormal posture of the cervical spine. J. Phys. Ther. Sci. 2015, 27, 1609–1611. [Google Scholar] [CrossRef]
- Vos, T.; Flaxman, A.D.; Naghavi, M.; Lozano, R.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; Aboyans, V.; et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2163–2196. [Google Scholar] [CrossRef]
- Murray, C.J.; Vos, T.; Lozano, R.; Naghavi, M.; Flaxman, A.D.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2197–2223. [Google Scholar] [CrossRef] [PubMed]
- Koes, B.W.; van Tulder, M.; Lin, C.W.; Macedo, L.G.; McAuley, J.; Maher, C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur. Spine J. 2010, 19, 2075–2094. [Google Scholar] [CrossRef] [PubMed]
- Chou, R.; Qaseem, A.; Snow, V.; Casey, D.; Cross, J.T., Jr.; Shekelle, P.; Owens, D.K.; Clinical Efficacy Assessment Subcommittee of the American College of Physicians; American College of Physicians; American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: A joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann. Intern. Med. 2007, 147, 478–491. [Google Scholar] [CrossRef]
- GBD 2021 Low Back Pain Collaborators. Global, regional, and national burden of low back pain, 1990–2020, its attributable risk factors, and projections to 2050: A systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023, 5, e316–e329. [Google Scholar] [CrossRef]
- Harrison, D.E.; Colloca, C.J.; Harrison, D.D.; Janik, T.J.; Haas, J.W.; Keller, T.S. Anterior thoracic posture increases thoracolumbar disc loading. Eur. Spine J. 2005, 14, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Ghezelbash, F.; Shirazi-Adl, A.; El Ouaaid, Z.; Plamondon, A.; Arjmand, N. Subject-specific regression equations to estimate lower spinal loads during symmetric and asymmetric static lifting. J. Biomech. 2020, 102, 109550. [Google Scholar] [CrossRef]
- Jensen, M.P.; Karoly, P.; Braver, S. The measurement of clinical pain intensity: A comparison of six methods. Pain 1986, 27, 117–126. [Google Scholar] [CrossRef]
- Divi, S.N.; Eleswarapu, A.S.; Stout, C.E.; Lee, M.J. Real-World Effectiveness of Physical Therapy for Common Neck Pain Diagnoses: A Multivariate Analysis of 1554 Patients. Clin. Spine Surg. 2018, 31, 395–399. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, M.M.; Mahoor, M.H.; Haas, J.W.; Ferrantelli, J.R.; Dupuis, A.-L.; Jaeger, J.O.; Harrison, D.E. Intra-Examiner Reliability and Validity of Sagittal Cervical Spine Mensuration Methods Using Deep Convolutional Neural Networks. J. Clin. Med. 2024, 13, 2573. [Google Scholar] [CrossRef]
- Russell, B.S.; Muhlenkamp-Wermert, K.A.; Hoiriis, K.T. Measurement of Lumbar Lordosis: A Comparison of 2 Alternatives to the Cobb Angle. J. Manip. Physiol. Ther. 2020, 43, 760–767. [Google Scholar] [CrossRef]
- Glassman, S.D.; Bridwell, K.; Dimar, J.R.; Horton, W.; Berven, S.; Schwab, F. The impact of positive sagittal balance in adult spinal deformity. Spine 2005, 30, 2024–2029. [Google Scholar] [CrossRef]
- Plais, N.; Bao, H.; Lafage, R.; Gupta, M.; Smith, J.S.; Shaffrey, C.; Mundis, G.; Burton, D.; Ames, C.; Klineberg, E.; et al. The clinical impact of global coronal malalignment is underestimated in adult patients with thoracolumbar scoliosis. Spine Deform. 2020, 8, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Diebo, B.G.; Alsoof, D.; Lafage, R.; Daher, M.; Balmaceno-Criss, M.; Passias, P.G.; Ames, C.P.; Shaffrey, C.I.; Burton, D.C.; Deviren, V.; et al. Impact of Self-Reported Loss of Balance and Gait Disturbance on Outcomes following Adult Spinal Deformity Surgery. J. Clin. Med. 2024, 13, 2202. [Google Scholar] [CrossRef]
- Bridwell, K.H.; Baldus, C.; Berven, S.; Edwards, C., 2nd; Glassman, S.; Hamill, C.; Horton, W.; Lenke, L.G.; Ondra, S.; Schwab, F.; et al. Changes in radiographic and clinical outcomes with primary treatment adult spinal deformity surgeries from two years to three- to five-years follow-up. Spine 2010, 35, 1849–1854. [Google Scholar] [CrossRef]
- Acaroglu, E.; Yavuz, A.C.; Guler, U.O.; Yuksel, S.; Yavuz, Y.; Domingo-Sabat, M.; Pellise, F.; Alanay, A.; Perez Grueso, F.S.; Kleinstück, F.; et al. A decision analysis to identify the ideal treatment for adult spinal deformity: Is surgery better than non-surgical treatment in improving health-related quality of life and decreasing the disease burden? Eur. Spine J. 2016, 25, 2390–2400. [Google Scholar] [CrossRef]
- McCarthy, I.; O’Brien, M.; Ames, C.; Robinson, C.; Errico, T.; Polly, D.W., Jr.; Hostin, R.; International Spine Study Group. Incremental cost-effectiveness of adult spinal deformity surgery: Observed quality-adjusted life years with surgery compared with predicted quality-adjusted life years without surgery. Neurosurg. Focus 2014, 36, E3. [Google Scholar] [CrossRef]
- Al-Mohrej, O.A.; Aldakhil, S.S.; Al-Rabiah, M.A.; Al-Rabiah, A.M. Surgical treatment of adolescent idiopathic scoliosis: Complications. Ann. Med. Surg. 2020, 52, 19–23. [Google Scholar] [CrossRef]
- Kim, Y.J.; Bridwell, K.H.; Lenke, L.G.; Cheh, G.; Baldus, C. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: A minimum 5-year follow-up study. Spine 2007, 32, 2189–2197. [Google Scholar] [CrossRef] [PubMed]
- Ailon, T.; Smith, J.S.; Shaffrey, C.I.; Lenke, L.G.; Brodke, D.; Harrop, J.S.; Fehlings, M.; Ames, C.P. Degenerative Spinal Deformity. Neurosurgery 2015, 77, S75–S91. [Google Scholar] [CrossRef] [PubMed]
- Debrosse, M.; Shergill, S.; Shah, A.; Patel, K.; Gulati, A.; Rajput, K. Trigger point injection therapies for chronic myofascial neck and back pain: A systematic review. Interv. Pain Med. 2022, 1, 100076. [Google Scholar] [CrossRef]
- Fard, A.P.; Ferrantelli, J.R.; Dupuis, A.L.; Mahoor, M.H. Sagittal Cervical Spine Landmark Point Detection in X-Ray Using Deep Convolutional Neural Networks. IEEE Access 2022, 10, 59413–59427. [Google Scholar] [CrossRef]
- Betz, J.W.; Lightstone, D.F.; Oakley, P.A.; Haas, J.W.; Moustafa, I.M.; Harrison, D.E. Reliability of the Biomechanical Assessment of the Sagittal Lumbar Spine and Pelvis on Radiographs Used in Clinical Practice: A Systematic Review of the Literature. J. Clin. Med. 2024, 13, 4650. [Google Scholar] [CrossRef]
- Vaiserman, A.; Cuttler, J.M.; Socol, Y. Low-dose ionizing radiation as a hormetin: Experimental observations and therapeutic perspective for age-related disorders. Biogerontology 2021, 22, 145–164. [Google Scholar] [CrossRef]
- Suwaidi, A.S.A.; Moustafa, I.M.; Kim, M.; Oakley, P.A.; Harrison, D.E. A Comparison of Two Forward Head Posture Corrective Approaches in Elderly with Chronic Non-Specific Neck Pain: A Randomized Controlled Study. J. Clin. Med. 2023, 12, 542. [Google Scholar] [CrossRef]
- Katzman, W.B.; Parimi, N.; Gladin, A.; Fan, B.; Wong, S.S.; Mergenthaler, J.; Lane, N.E. Reliability of sagittal vertical axis measurement and association with measures of age-related hyperkyphosis. J. Phys. Ther. Sci. 2018, 30, 1417–1423. [Google Scholar] [CrossRef]
- Tan, L.X.; Du, X.K.; Tang, R.M.; Rong, L.M.; Zhang, L.M. Effect of spinal-pelvic sagittal balance on the clinical outcomes after lumbar fusion surgery. BMC Surg. 2023, 23, 334. [Google Scholar] [CrossRef]
- Calabrese, E.J.; Blain, R. The Occurrence of Hormetic dose Responses in the Toxicological Literature, the Hormesis Database: An Overview. Toxicol. Appl. Pharmacol. 2005, 202, 289–301. [Google Scholar] [CrossRef] [PubMed]
- Jargin, S.V. Radiation safety and hormesis. Front. Public Health 2020, 8, 278. [Google Scholar] [CrossRef] [PubMed]
- Calabrese, E.J.; Baldwin, L.A. Hormesis as a biological hypothesis. Environ. Health Perspect. 1998, 106, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Arnone, P.A.; McCanse, A.E.; Farmen, D.S.; Alano, M.V.; Weber, N.J.; Thomas, S.P.; Webster, A.H. Plain Radiography: A unique component of spinal assessment and predictive health. Healthcare 2024, 12, 633–661. [Google Scholar] [CrossRef]
- Robertson, D.; Willardson, R.; Parajuli, D.; Cannon, A.; Bowden, A.E. The lumbar supraspinous ligament demonstrates increased material stiffness and strength on its ventral aspect. J. Mech. Behav. Biomed. Mater. 2013, 17, 34–43. [Google Scholar] [CrossRef]
- Merter, A.; Karaca, M.O.; Yazar, T. Biomechanical effects of sequential resection of the posterior ligamentous complex on intradiscal pressure and resistance to compression forces. Acta Orthop. Traumatol. Turc. 2019, 53, 502–506. [Google Scholar] [CrossRef]
- Little, J.S.; Khalsa, P.S. Human lumbar spine creep during cyclic and static flexion: Creep rate, biomechanics, and facet joint capsule strain. Ann. Biomed. Eng. 2005, 33, 391–401. [Google Scholar] [CrossRef] [PubMed]
- Panjabi, M.M.; Crisco, J., 3rd; Lydon, C.; Dvorak, J. The mechanical properties of human alar and transverse ligaments at slow and fast extension rates. Clin. Biomech. 1998, 13, 112–120. [Google Scholar] [CrossRef]
- Mattucci, S.F.; Moulton, J.A.; Chandrashekar, N.; Cronin, D.S. Strain rate dependent properties of human craniovertebral ligaments. J. Mech. Behav. Biomed. Mater. 2013, 23, 71–79. [Google Scholar] [CrossRef]
- Widmer, J.; Cornaz, F.; Scheibler, G.; Spirig, J.M.; Snedeker, J.G.; Farshad, M. Biomechanical Contribution of Spinal Structures to Stability of the Lumbar Spine—Novel Biomechanical Insights. Spine J. 2020, 20, 1705–1716. [Google Scholar] [CrossRef]
- Freyler, K.; Gollhofer, A.; Colin, R.; Brüderlin, U.; Ritzmann, R. Reactive Balance Control in Response to Perturbation in Unilateral Stance: Interaction Effects of Direction, Displacement and Velocity on Compensatory Neuromuscular and Kinematic Responses. PLoS ONE 2015, 10, e0144529. [Google Scholar] [CrossRef]
- Mohapatra, S.; Krishnan, V.; Aruin, A.S. Postural control in response to an external perturbation: Effect of altered proprioceptive information. Exp. Brain Res. 2012, 217, 197–208. [Google Scholar] [CrossRef]
- Diener, H.C.; Dichgans, J.; Bootz, F.; Bacher, M. Early stabilization of human posture after a sudden disturbance: Influence of rate and amplitude of displacement. Exp. Brain Res. 1984, 56, 126–134. [Google Scholar] [CrossRef]
- Beckley, D.J.; Bloem, B.R.; Remler, M.P. Impaired scaling of long latency postural reflexes in patients with Parkinson’s disease. Electroencephalogr. Clin. Neurophysiol. 1993, 89, 22–28. [Google Scholar] [CrossRef]
- Jung, J.Y.; Kang, C.K.; Kim, Y.B. Postural supporting cervical traction workstation to improve resting state brain activity in digital device users: EEG study. Digit. Health 2024, 10, 20552076241282244. [Google Scholar] [CrossRef]
- Jung, J.Y.; Lee, Y.B.; Kang, C.K. Effect of forward head posture on resting state brain function. Healthcare 2024, 12, 1162. [Google Scholar] [CrossRef] [PubMed]
- Katzman, W.B.; Parimi, N.; Gladin, A.; Wong, S.; Lane, N.E. Long-Term Efficacy of Treatment Effects After a Kyphosis Exercise and Posture Training Intervention in Older Community-Dwelling Adults: A Cohort Study. J. Geriatr. Phys. Ther. 2021, 44, 127–138. [Google Scholar] [CrossRef] [PubMed]
- de Groot, M.H.; van der Jagt-Willems, H.C.; van Campen, J.P.; Lems, W.F.; Beijnen, J.H.; Lamoth, C.J. A flexed posture in elderly patients is associated with impairments in postural control during walking. Gait Posture 2014, 39, 767–772. [Google Scholar] [CrossRef] [PubMed]
- Oakley, P.A.; Jaeger, J.O.; Brown, J.E.; Polatis, T.A.; Clarke, J.G.; Whittler, C.D.; Harrison, D.E. The CBP® mirror image® approach to reducing thoracic hyperkyphosis: A retrospective case series of 10 patients. J. Phys. Ther. Sci. 2018, 30, 1039–1045. [Google Scholar] [CrossRef] [PubMed]
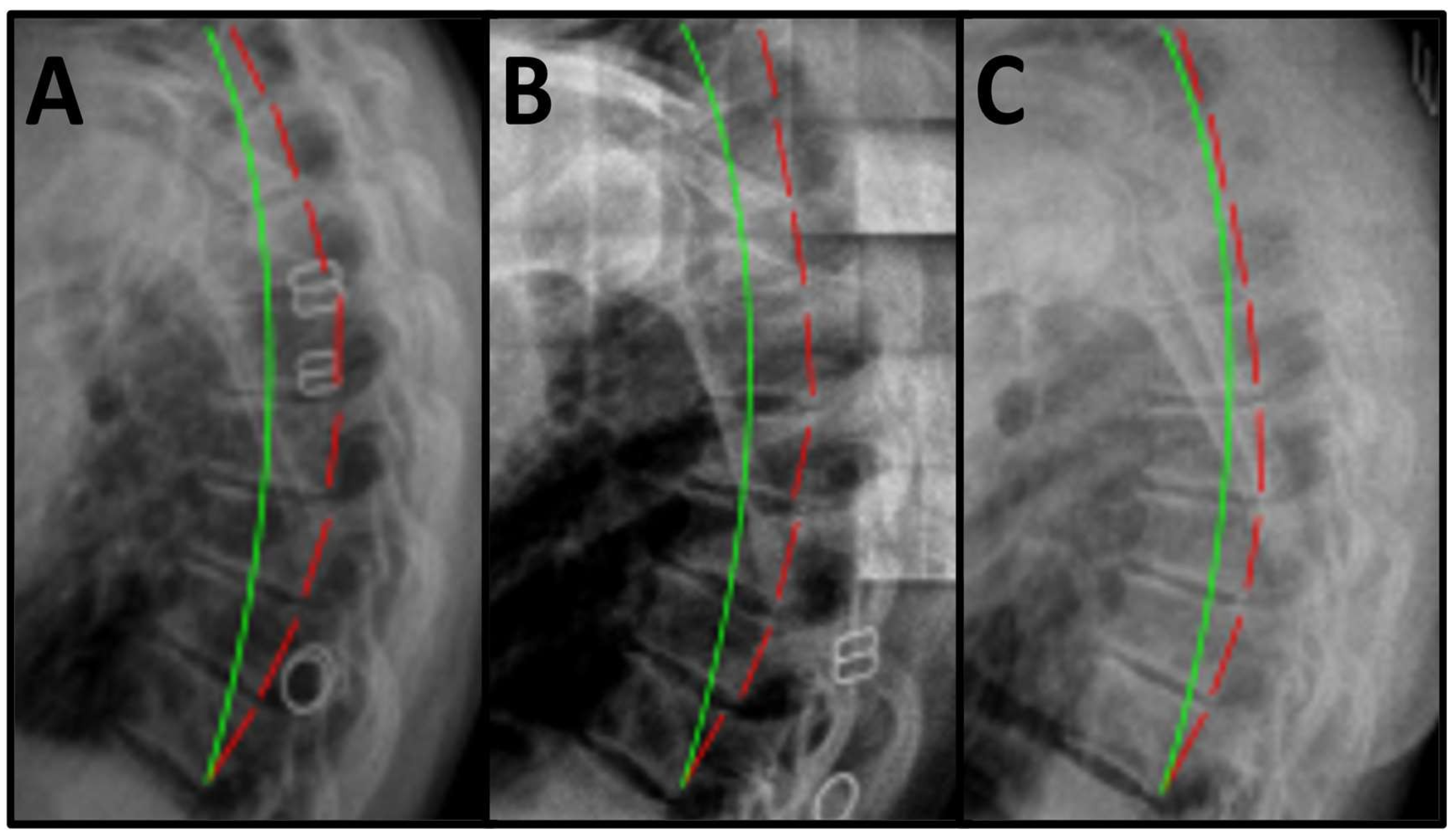
| Radiographic Findings | T1–T12 ARA (Ideal is 44°) |
|---|---|
| Pre-Treatment | 66.2° |
| Post-Treatment | 45.2° |
| Long-Term Follow-up | 47.7° |
| Evaluation | VAS | VAS |
|---|---|---|
| Date | Pain at Worst | Average Pain |
| 28 August 2022 | 8\10 | 6\10 |
| 1 December 2022 | 4\10 | 2\10 |
| 11 August 2023 | 2\10 | 0\10 |
| Overall Change | 6\10 | 6\10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Longo, K.; Haas, J.W.; Oakley, P.A.; Harrison, D.E. Reduction in Severe, Chronic Mid-Back Pain Following Correction of Sagittal Thoracic Spinal Alignment Using Chiropractic BioPhysics® Spinal Rehabilitation Program Following Prior Failed Treatment: A Case Report with 9-Month Follow-Up. Healthcare 2025, 13, 2587. https://doi.org/10.3390/healthcare13202587
Longo K, Haas JW, Oakley PA, Harrison DE. Reduction in Severe, Chronic Mid-Back Pain Following Correction of Sagittal Thoracic Spinal Alignment Using Chiropractic BioPhysics® Spinal Rehabilitation Program Following Prior Failed Treatment: A Case Report with 9-Month Follow-Up. Healthcare. 2025; 13(20):2587. https://doi.org/10.3390/healthcare13202587
Chicago/Turabian StyleLongo, Kyle, Jason W. Haas, Paul A. Oakley, and Deed E. Harrison. 2025. "Reduction in Severe, Chronic Mid-Back Pain Following Correction of Sagittal Thoracic Spinal Alignment Using Chiropractic BioPhysics® Spinal Rehabilitation Program Following Prior Failed Treatment: A Case Report with 9-Month Follow-Up" Healthcare 13, no. 20: 2587. https://doi.org/10.3390/healthcare13202587
APA StyleLongo, K., Haas, J. W., Oakley, P. A., & Harrison, D. E. (2025). Reduction in Severe, Chronic Mid-Back Pain Following Correction of Sagittal Thoracic Spinal Alignment Using Chiropractic BioPhysics® Spinal Rehabilitation Program Following Prior Failed Treatment: A Case Report with 9-Month Follow-Up. Healthcare, 13(20), 2587. https://doi.org/10.3390/healthcare13202587








